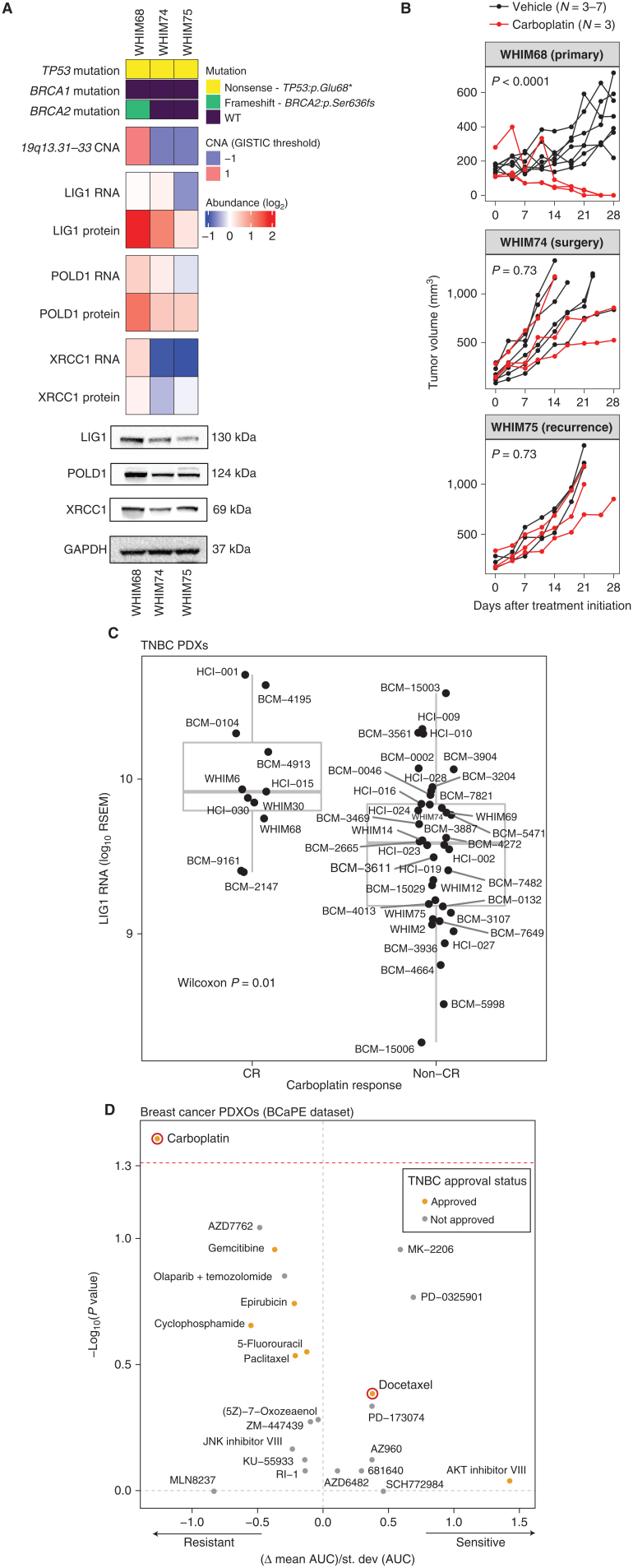
Figure 6.
LIG1 association with advanced TNBC disease in preclinical models. A, Proteogenomic status of LIG1, POLD1, and XRCC1 in three PDX models derived from longitudinal biopsies from the same patient with TNBC prior to any treatment (WHIM68), at the time of surgery after completing 5 months of neoadjuvant carboplatin and docetaxel (WHIM74), and from a liver metastasis 1 year after treatment initiation (WHIM75). Mutation and copy-number data were derived from WES and RNA from RNA-seq, and protein data were obtained from TMT proteomics generated by this current study. Bottom, representative western blots from three biological repeats for LIG1, POLD1, and XRCC1 protein levels. GAPDH was used as a loading control. WT, wild-type. *, stop codon. B, Tumor volume was measured in three PDX models. Black and red lines indicate changes in tumor volume in PDXs treated with vehicle and carboplatin, respectively. WHIM68, with the highest LIG1 protein levels, was most sensitive to carboplatin, whereas WHIM74 and 75, which displayed progressive LIG1 loss at the copy-number, mRNA, and protein levels, were insensitive to carboplatin treatment. P values derived from a general linear model within each PDX were computed using estimated mean log2 fold changes in tumor volume at day 28 versus day 0 for each treatment arm.C, Box plots showing LIG1 mRNA levels in TNBC PDXs categorized into CR and non-CR groups. After 4 weeks of carboplatin treatment, CR was defined as PDXs with nonpalpable tumors, and non-CR was defined as PDXs with residual tumors with measurable dimensions. The Wilcoxon rank sum test was used to compare the two groups. RSEM, expected counts from RNA-seq by expectation-maximization. D, Association between LIG1 copy-number loss and treatment response in PDX organoids (PDXO) obtained from the BCaPE database. Carboplatin and docetaxel are highlighted in red.