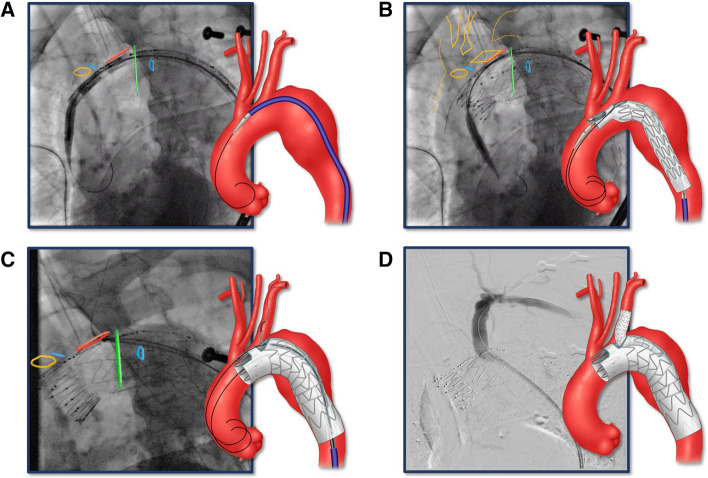
Fig. 2.
Bilateral percutaneous femoral approach using pre-closure technique was established using duplex ultrasound guidance. Systemic heparinization was performed to achieve an activated clotting time (ACT) > 250 s. A 0.035-inch double curve Lunderquist wire (Cook Medical, Bloomington, Indiana, USA) was positioned in the proximal ascending aorta. Angiography was performed to identify the supra-aortic trunks and calibrate the on-lay fusion. The arch branch stent graft was flushed with carbon dioxide and subsequently with heparinized saline [19]. The stent graft was introduced over the Lunderquist wire and advanced into position. Systolic blood pressure was decreased to approximately 90 mmHg prior to device deployment. A Stent graft was introduced over Lunderquist wire and advanced into position using radiopaque markers and on-lay fusion. B Arch branch stent graft was deployed. C A second Lunderquist wire was advanced via the pre-loaded catheter through the retrograde LSA branch up to the ascending aorta. The aortic stent graft delivery system and the main aortic Lunderquist wire were removed and a 22 to 24 Fr Dryseal sheath (WL Gore, Flagstaff AZ) was introduced over the second LSA inner branch Lunderquist wire. A 10-Fr 80 cm long Flexor® Ansel sheath (Cook Medical, Bloomington, Indiana, the USA) was advanced into the LSA branch. Using a “buddy” 5Fr VanSchie 3 catheter (Cook Medical Inc., Bloomington IN), the LSA was selectively anterogradely catheterized with a glidewire, which was exchanged for a 1-cm tip Amplatz wire (Cook Medical, Bloomington, IN). Limited angiography was performed via the sheath to identify the origin of the LSA. The repair was extended into the LSA by placement of self-expandable or balloon-expandable Viabahn stent graft (WL Gore, Flagstaff AZ). D Completion LSA angiography was performed to demonstrate patency and the absence of dissection, endoleak or embolization. Final rotational digital subtraction angiography and high-definition CBCT were performed to evaluate technical success, vessel patency and the absence of endoleaks, dissections or embolization