Abstract
Background:
Pediatric overweight/obesity is a major health problem worldwide. Accurate parental perception of children’s weight status is crucial in preventing and tackling this issue. Despite the consistent increase in prevalence of the childhood obesity in Saudi Arabia, the role of the parents is not well described. This study aims to explore Saudi parents’ readiness to change the lifestyle of their overweight/obese children and the barriers facing it.
Individuals and Methods:
Through a cross-sectional design, 362 parents of overweight/obese children attending King Abdulla Specialized Children’s Hospital were selected and requested to fill a predesigned questionnaire reflecting their perception about their children’s weight status and their preparedness to change their lifestyle. A Chi-square test was used to verify significance. A P value of <0.05 was considered an indication of significance.
Results:
Among all overweight/obese children (n = 362), obese children formed 39.5 and 22.7% had morbid obesity. Only one half of the parents (49.7%) had correct perception about their children’s weight. Correct perception increases significantly with an increase age of the child and in the presence of family history of diabetes, P < 0.05. Only 68.9% were worried about body weight of their children, the percentage was significantly higher in younger parents; parents with obese children and with a positive family history of hypertension P < 0.05. In total, 83.1% of the worried parents proceeded to preparation and action stages; the percentage was significantly higher among parents whom their children were free from identified comorbidities, P < 0.05.
Conclusion:
Misconception about real weight status of overweight/obese children is common in Saudi parents. Parents who have correct perception and worried about health status of their children are more likely to take actions. The first step in controlling children’s obesity is to educate parents about how to recognize the real weight status of their children and to be aware about the health-related problems of obesity.
Keywords: Overweight, parental perception, pediatric obesity, readiness to change
Introduction
Pediatric overweight/obesity is a serious health problem worldwide, which is associated with developmental, mental, and physical health consequences.[1] The most serious consequences are cardiovascular diseases, hypertension, type 2 diabetes, depression, and low self-esteem which may lead to serious morbidities.[2,3] Research revealed that childhood overweight is a key predictor of obesity in adulthood.[4] Globally, WHO stated in 2016 that the number of preschool overweight children is estimated to be over 41 million, half of them live in Asia and one-quarter in Africa.[5] Regionally, in UAE, 28.2% of children are obese or overweight.[6] In Saudi Arabia, the prevalence of overweight and obesity in school age children was 13.4 and 18.2%, respectively.[7]
Parents are responsible for their children’s weight, by shaping and controlling their eating habits and physical activity.[8] Studies showed that parents who can recognize their child’s obesity seem to be more concerned to modify their lifestyle.[9,10] Unfortunately, most parents cannot interpret the weight status of their children correctly, which is considered a barrier for early intervention and prevention of obesity.[11] In United Kingdom, 62.4% of parents misinterpret their child’s weight status,[12] while in a Saudi study, 90% of 76 overweight children were perceived as normal weight and 64% of obese children were weight-misperceived by their parents.[13] Factors that were found to contribute to misperception of children’s weight status include child related factors (gender, young age) and parental factors (lower education, overweight parents),[14] as well as maternal health.[15] Parents’ readiness to change is crucial to help overweight and obese children lose weight and make better choices regarding their health.[16] Considering that, parental readiness to change does not necessarily indicate that they are ready to modify their overweight/obese child’s lifestyle[17], as it was found that parents could be ready to change dietary habits but reluctant to take active steps in increasing physical activity.[18] In this regard, Al Khashan et al. (2021)[19] asserted that primary health care physicians, being in the front line of health systems, are responsible for early detection of childhood obesity and increasing awareness of parents about the risks of obesity and how to prevent it.
The aim of this study is to explore the parental perception of children’s weight status and verify their readiness to change based on the transtheoretical model (TTM),[20] in addition to determine variables that influence their readiness to change.
Methods
This is a cross-sectional study that was conducted at outpatient clinics in King Abdulla Specialized Children’s Hospital (KASCH), Riyadh, KSA. KASCH is a part of King Abdulaziz Medical City complex which is the first medical referral institute that serves children. All obese/overweight children ages ranging from 2 to 14 coming to the outpatient clinic for regular appointments were considered eligible for inclusion in the study. The exclusion criteria included physically or mentally disabled, gastric-tube feeding, and chronic medical conditions that affect his/her weight or ability to eat independently, being treated with steroids, chemotherapy, or immune suppressants, and children not accompanied by the primary caregiver. The sample size was calculated using www.raosoft.com; the required sample size was 377 with a confidence level of 95%. The sample was collected from April 2021 to August 2021 using a convenience sampling technique. For data collection, first, the anthropometric measures were taken from the medical records on the same date of the appointment. According to CDC classification, the body mass index (BMI) of each child was calculated and marked on the chart appropriate to gender and age. Overweight was considered for children of the same age and sex with BMI at ≥ 85–<95th percentile and obesity at ≥ 95th percentile. Next, an electronic survey was filled by the obese/overweight children’s parents via an interview or a phone call after attaining the consent. After completing the survey, the participants were categorized according to the TTM,[20] into the four stages of change: precontemplation (unlikely to make a change in the near future), contemplation (likely to make a change in the next 6 month), preparation (very likely to make a change but not started yet), and action stage (already actively making changes). Data were coded and analyzed using SAS version 9.4 (SAS Institute Inc.). Qualitative variables are summarized and presented as frequency distribution, while quantitative normally distributed variables are presented in mean and standard deviation. Chi-square test was used to verify significance, P value less than 0.05 was considered a level of significance.
Results
Among the studied overweight/obese children (n = 362), there was a slight dominance of males (54.4%), with a mean age of 10.4 ± 3.2 years. The great majority (89%) were living with both parents. Obese children formed 39.5 and 22.7% had morbid obesity. In two-thirds of the children (67.7%), the father was interviewed. The caregivers were mainly (44.8%) in the age group 40–50 years, with an intermediate level of education (41.2%) or university qualifications (35.9%). In total, 34.8 and 14.9% of the caregivers described themselves as overweight or obese, respectively [Table 1].
Table 1.
Sociodemographic and clinical characteristics of the overweight/obese children and their parents (n=362)
| Characteristics | No. | Percentage |
|---|---|---|
| Characteristics of the children | ||
| Gender | ||
| Male | 197 | 54.4 |
| Female | 165 | 45.6 |
| Age at presentation | ||
| 2-<6 years | 43 | 11.9 |
| 6-<12 years | 171 | 47.2 |
| ≥12 years | 148 | 40.9 |
| Mean±SD | 10.4±3.2 years | |
| Live with whom | ||
| Both parents | 322 | 89.0 |
| One parent | 40 | 11.0 |
| BMI categories | ||
| Overweight | 137 | 37.8 |
| Obese | 143 | 39.5 |
| Morbid obesity | 82 | 22.7 |
| Comorbidities | ||
| Respiratory | 36 | 9.9 |
| Mobility | 24 | 6.6 |
| Metabolic | 74 | 20.4 |
| Characteristics of the presenting parents | ||
| Relation to the child | ||
| Mother | 117 | 32.3 |
| Father | 245 | 67.7 |
| Age | ||
| <40 years | 127 | 35.1 |
| 40-<50 years | 162 | 44.8 |
| 50+ years | 73 | 20.2 |
| Education level | ||
| Elementary | 83 | 22.9 |
| Intermediate | 149 | 41.2 |
| University/postgraduate | 130 | 35.9 |
| Employment: | ||
| Employed | 232 | 64.1 |
| Not employed | 130 | 35.9 |
| Household monthly income in SR | ||
| <5,000 | 70 | 19.3 |
| 5,000-<10,000 | 153 | 42.3 |
| 10,000-<20,000 | 101 | 27.9 |
| ≥20,000 | 38 | 10.5 |
| Self-recognition of body mass | ||
| Underweight | 10 | 2.8 |
| Normal weight | 172 | 47.5 |
| Overweight | 126 | 34.8 |
| Obese | 54 | 14.9 |
Diagram 1 summarizes parents’ perception about the weight status of their children, the consequent worry about their health status, and the progress in their intention to change the lifestyle of their children. It showed that only one-half of the parents (49.7%) had correct perception. Despite their correct perception, one-third of them were not worried about the health of their children. The majority of worried parents (83%) expressed that future weight-related health problems were their main concern, while current health, interference with physical activity, bullying, and low self-esteem concerns were reported with the following percentage 46, 42, 36, and 40%, respectively, by the worried caregivers.
Diagram 1.
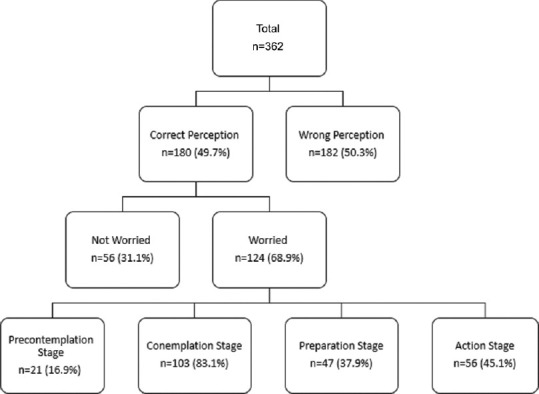
Distribution of parents according to their perception about weight status of their children, worry about their health, and progress in their readiness to change
The worried parents (68.9%) were further classified (according to TTM) into the four stages of readiness to change. Those in the precontemplation stage (7%) were worried but were not thinking of lifestyle changes. Those in the contemplation stage (10%) were considering making lifestyle changes in the next 6 months. In the preparation stage (38%), they have started some lifestyle changes but succeeded less than 50% of the time, while in the action stage (45%), they did succeed more than 50% of the time to make those changes.
A Sedentary lifestyle was the top selection by parents as a cause of their children overweight and obesity (70%), whereas too much food and unhealthy food choice received an equal percentage of ~57% [Figure 1].
Figure 1.
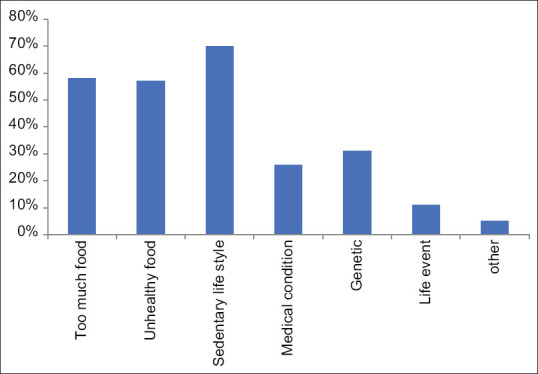
Caregivers’ perception of possible causes of their children’s obesity (n = 132)
When, those worried parents, were asked about what healthy lifestyle changes they are planning to introduce, limiting fast food intake and increasing physical activity received the highest vote (~70% each) followed by limiting screen time and changing family diet by 50%. Specific diet changes like reducing sugary drinks and increasing fruits and vegetables portions were lower on the list of planned changes [Figure 2].
Figure 2.
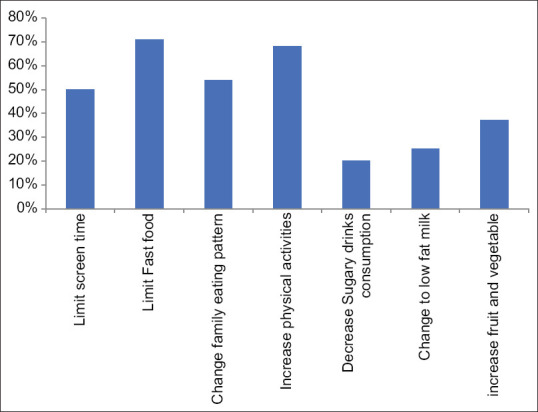
Contemplated healthy lifestyle changes’ options chosen by caregivers (n = 124)
Table 2 demonstrates that correct perception increases significantly with an increasing age of the child, P < 0.05, and was higher among parents who declared that there was a family history of diabetes (56.4%), while the lowest percentage was in parents who recognized themselves as being of normal weight (38.4%), P < 0.05. Otherwise, no statistically significant difference in correct perception was detected regarding other factors, P > 0.05.
Table 2.
Factors associated with correct perception of the parents about the actual weight of their children
| Factors/variables | Perception about actual weight | χ 2 | P* | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Correct | Wrong | |||||
|
|
|
|||||
| No | % | No | % | |||
| Gender of the child | ||||||
| Male | 107 | 54.3 | 90 | 45.7 | 3.644 | 0.056 |
| Female | 73 | 44.2 | 92 | 55.8 | ||
| Age of the child | ||||||
| 2 to<6 years | 9 | 20.9 | 34 | 79.1 | 21.917 | <0.001** |
| 6 to<12 years | 81 | 47.4 | 90 | 52.6 | ||
| ≥12 years | 90 | 60.8 | 58 | 39.2 | ||
| The child lives with | ||||||
| Both parents | 160 | 49.7 | 162 | 50.3 | 0.001 | 0.970 |
| One parent | 20 | 50.0 | 20 | 50.0 | ||
| Daily contact with an extended family member | ||||||
| Yes | 161 | 48.3 | 172 | 51.7 | 3.146 | 0.076 |
| No | 19 | 65.5 | 10 | 34.5 | ||
| Age of the parent | ||||||
| <40 years | 60 | 47.2 | 67 | 52.8 | 0.893 | 0.640 |
| 40-<50 years | 85 | 52.5 | 77 | 47.5 | ||
| ≥50 years | 35 | 47.9 | 38 | 52.1 | ||
| Education level of the presenting parent | ||||||
| Elementary | 40 | 48.2 | 43 | 51.8 | 0.919 | 0.832 |
| Intermediate | 71 | 47.7 | 78 | 52.3 | ||
| University | 69 | 53.1 | 61 | 46.9 | ||
| Employment | ||||||
| Employed | 113 | 48.7 | 119 | 51.3 | 0.267 | 0.605 |
| Not employed | 67 | 51.5 | 63 | 48.5 | ||
| Household monthly income | ||||||
| <5,000 | 30 | 42.9 | 40 | 57.1 | 5.783 | 0.123 |
| 5,000-<10,000 | 71 | 46.4 | 82 | 53.6 | ||
| 10,000-<20,000 | 60 | 59.4 | 41 | 40.6 | ||
| ≥20,000 | 19 | 50.0 | 19 | 50.0 | ||
| Self-recognition of body mass | 17.501 | 0.001** | ||||
| Underweight | 6 | 60.0 | 4 | 40.0 | ||
| Normal weight | 66 | 38.4 | 106 | 61.6 | ||
| Overweight | 78 | 61.9 | 48 | 38.1 | ||
| Obese | 30 | 55.6 | 24 | 44.4 | ||
| Family history of diabetes mellitus | 5.353 | 0.021* | ||||
| Yes | 92 | 56.4% | 71 | 43.6% | ||
| No | 88 | 44.2% | 111 | 55.8% | ||
*Based on Chi-square; **Statistically significant
Table 3 shows that the percentage of worried parents was significantly higher in younger parents than older ones, and parents with obese children (91.5%) rather than parents with overweight children (57.9%). The percentage was also significantly higher among parents who denoted that there is a positive family history of hypertension (80.3%), P < 0.05.
Table 3.
Factors associated with the worry of the parents who had correct perception about child’s weight regarding their health issues (n=180)
| Factors/variables | Worry of the parents | χ 2 | P* | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Worried |
Not worries |
|||||
| No | % | No | % | |||
| Gender of the child | ||||||
| Male | 73 | 68.2 | 34 | 31.8 | 0.054 | 0.816 |
| Female | 51 | 69.9 | 22 | 30.1 | ||
| Age of the child | ||||||
| 2-<6 years | 6 | 66.7 | 3 | 33.3 | 0.023 | 0.989 |
| 6-<12 years | 56 | 69.1 | 25 | 30.9 | ||
| ≥12 years | 62 | 68.9 | 28 | 31.1 | ||
| Age of the parent | ||||||
| <40 years | 45 | 75.0 | 15 | 25.0 | 6.352 | 0.042** |
| 40-<50 years | 61 | 71.8 | 24 | 28.2 | ||
| ≥50 years | 18 | 51.4 | 17 | 48.6 | ||
| Correct perceived weight category of the child | ||||||
| Overweight | 70 | 57.9 | 51 | 42.1 | 20.984 | <0.001** |
| Obese | 54 | 91.5 | 5 | 8.5 | ||
| Family history of hypertension | ||||||
| Yes | 49 | 80.3 | 12 | 19.7 | 5.633 | 0.018** |
| No | 75 | 63.0 | 44 | 37.0 | ||
| Family history of diabetes mellitus | ||||||
| Yes | 67 | 72.8 | 25 | 27.2 | 1.361 | 0.243 |
| No | 57 | 64.8 | 31 | 35.2 | ||
| Family history of dyslipidemia | ||||||
| Yes | 39 | 75.0 | 13 | 25.0 | 1.274 | 0.259 |
| No | 85 | 66.4 | 43 | 33.6 | ||
| Family history of IHD | Fisher | 0.204 | ||||
| Yes | 11 | 84.6 | 2 | 15.4 | ||
| No | 113 | 67.7 | 54 | 32.3 | ||
*Based on Chi-square; **Statistically significant
Table 4 demonstrates that the percentage of the worried parents who proceeded to the preparation/action stages was significantly higher among those whose children were free from identified comorbidities, P < 0.05. On the other side, adopting changes to reduce the weight of the child was higher among parents of male children (83.6%), parents of obese children (85.2%), younger parents aged < 40 years (86.7%), parents in families with a positive family history of hypertension (85.7%), diabetes mellitus (85.1%), and/or dyslipidemia (84.6%); however, these differences are not statistically significant, P > 0.05, but it could be of clinical importance.
Table 4.
Factors associated with reaching the stage of adopting changes to reduce the weight of the child among parents worried about health issues related to weight (n=124)
| Factors/variables | Likeliness to make changes | χ 2 | P* | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Likely | Unlikely | |||||
|
|
|
|||||
| No | % | No | % | |||
| Gender of the child | ||||||
| Male | 61 | 83.6 | 12 | 16.4 | 0.031 | 0.860 |
| Female | 42 | 82.4 | 9 | 17.6 | ||
| Comorbidities of the child | ||||||
| Yes | 32 | 71.1 | 13 | 28.9 | 7.174 | 0.007** |
| No | 71 | 89.9 | 8 | 10.1 | ||
| Correct perceived weight category of the child | ||||||
| Overweight | 57 | 81.4 | 13 | 18.6 | 0.306 | 0.580 |
| Obese | 46 | 85.2 | 8 | 14.8 | ||
| Age of the parent | ||||||
| <40 years | 39 | 86.7 | 6 | 13.3 | 0.825 | 0.662 |
| 40-<50 years | 50 | 82.0 | 11 | 18.0 | ||
| ≥50 years | 14 | 77.8 | 4 | 22.2 | ||
| Education level of the presenting parent | ||||||
| Elementary | 23 | 88.5 | 3 | 11.5 | 3.623 | 0.163 |
| Intermediate | 36 | 75.0 | 12 | 25.0 | ||
| University | 44 | 88.0 | 6 | 12.0 | ||
| Family history of hypertension | ||||||
| Yes | 42 | 85.7 | 7 | 14.3 | 0.404 | 0.525 |
| No | 61 | 81.3 | 14 | 18.7 | ||
| Family history of diabetes mellitus | ||||||
| Yes | 57 | 85.1 | 10 | 14.9 | 0.419 | 0.518 |
| No | 46 | 80.7 | 11 | 19.3 | ||
| Family history of dyslipidemia | ||||||
| Yes | 33 | 84.6 | 6 | 15.4 | 0.097 | 0.755 |
| No | 70 | 82.4 | 15 | 17.6 | ||
| Family history of IHD | ||||||
| Yes | 9 | 81.8 | 2 | 18.2 | Fisher | 0.589 |
| No | 94 | 83.2 | 19 | 16.8 | ||
*Based on Chi-square; **Statistically significant
Out of all parents who could declare the barriers they are facing for change (n = 116), almost one half (48.3%) indicated that their physicians are not drawing attention to weight issues, and almost equal percentage (45.7%) claimed that they do not know how to get help, and one-third (32.8%) expressed that family members do not see weight as a problem [Figure 3].
Figure 3.

Barriers facing parents to take action for changing the lifestyle of their obese/overweight children (n = 116)
Discussion
Pediatric obesity has been recognized as a growing problem in Saudi Arabia like in many other countries worldwide.[7,21,22] Given the risk of the consequent severe health problems and heavy burden on the health care system, effective efforts of controlling obesity in children through parents is the key to combat this health problem.[5,8,21,23] The aim of the current study was to explore the readiness of parents of overweight/obese children to make healthy lifestyle changes. First, the study examined the parental perception about the actual weight status of their children, whether they are worried about it, and their readiness to change. One-half of the parents had a misconception about the real status of their overweight/obese children, which comes in accordance with several pieces of research which indicated that parental misconception about the weight of their children is a common worldwide problem.[1,3,12,15,23] In attempts to explain the roots of the problem of this misconception, Puhl and Heur suggested that parents might be reluctant to label their children as obese or overweight for societal factors, for example, considering obesity as a stigma,[24] or preferring children to be overweight or obese rather than being thin or underweight as they consider that overweight and obese as healthy children.[8] Campbell et al. accused the media to be responsible for distorting perception about what qualifies as being overweight by depicting obesity only in its extreme.[25] Even more, Queally et al. pointed to the role of some health clinicians who unintentionally send wrong messages to the parents by overlooking the problem of childhood obesity during clinical visits,[26] which had been asserted by Al Khashan et al. (2021) about the crucial role and responsibility of the primary health care physicians in modifying parental perception about childhood obesity.[19] The current study showed that the percentage of parents who had correct perception about the weight status of their children was significantly lowest among the parents of preschool children than older children, which could be attributed to what had been stated by Almoosawi et al.[12] who argued that the parents of toddlers and young children “might not consider their child to be overweight because he/she engages in physical activity, and they are not teased about his/her size, as long as there are no obvious health issues.” This argument was emphasized later by Ruiter et al.[3] who stated that “the accuracy of parents’ estimating their child’s weight status increases with the age of the child”, which support the findings of the current study.
The misconception of the children overweight/obesity children was significantly higher among parents who perceive their own body weight as normal, which draws attention toward an important issue regarding the cultural norms regarding “what is normal weight?” as shown in the current study, where parents indicated that the denial of the family members that overweight is a problem represents one of the barriers to change. In this regard, Opie and his colleagues (2017) pointed out that “In a society where more people exhibit unhealthy weight, social perception of a healthy weight is at risk of becoming obscured, leading to people with overweight and/or obesity perceiving their weight as healthy or normal,”[27]
Not all the parents who had correct perception felt worried about it. The results showed that the unworried parents were mostly the older parents and those who perceived their children as overweight rather than obese, while worried parents were mostly who indicated that there is a family history of hypertension. In this regard, Nsiah-Kumi et al. (2009)[28] argued that a positive family history of diabetes and cardiovascular diseases is significantly associated with parental perception of overweight children and its related risk factors; they suggested that strategies should be adapted to use family history to motivate families with overweight children toward behavior changes.
The importance of stratifying patients according to their stage of readiness to change lies in correctly approaching each stage with a proposed action. The results showed that once the parents became worried about possible obesity-related health problems in their children, they often proceed to initiate lifestyle changes which put them into the preparation and action stages (83.1%) collectively, while the remaining were in the precontemplation stage who, by definition of TTM, represent those who acknowledge the problem but are “uncertain if the problem behavior is worthy of correcting.”[29] The percentage of parents who proceeded to the preparation and action stages was higher among parents who indicated a family history of chronic diseases (diabetes, hypertension, IHD, dyslipidemia), although that was not statistically significant, it could be of clinical importance for motivating families to behavioral changes.[28]
Within our population, there seems to be a good understanding of the common causes of childhood obesity with a clear emphasis on sedentary lifestyle and junk food avoidance. However, they lack knowledge of more specific common health campaigns-promoted changes like increasing fruits/vegetable portions, reducing sugary drinks. Limitations of the study were as follows: responses were skewed toward fathers filling the survey more than mothers, due to the implementation of virtual clinics during the COVID-19 pandemic in which the fathers contact information was available in the patients’ files more so than the mothers. In addition, another limit was to not achieving the ideal target sample size due to exclusion criteria discovered during data analysis.
Conclusion
Misconception about the real weight status of overweight/obese children is common among Saudi parents. However, once having the correct perception, they are likely to be worried about their children’s health. Worry was the main trigger for contemplation, preparation, and action. A family history of chronic diseases is a significant predictor of the preparedness of the parents to adopt changes to overcome overweight and obesity in their children.
Recommendations
Parental education about how to recognize the real weight status of their children and the health-related problems of obesity via family physicians and public health prevention campaigns.
Interventions targeting younger age groups (preschoolers) parents and the overweight group before reaching late childhood with obesity.
Local studies are needed to explore barriers facing health care professional when discussing weight issues with caregivers.
To exploit a family history of chronic diseases related to obesity can help to motivate parents into making a change.
Healthy lifestyle campaign with simplified messages to promote more specific diet/exercise changes within our population is needed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Ethical approval
IRBC/0502/21.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors would like to acknowledge Mohammed Almutairi, Mohammed Alharbi, Abdullah Alanazi, Rakan Almokhlef, Norah Alkeneetir, Maha Binsaqer, Ziad Khalil, Khaled Alanazi, Hisham Aljeraisi, Nawaf Alhamied, and Abdulrahman Alajlan for their participation in the data extraction and collection part of this research.
References
- 1.Merema MR, Sullivan DL, Pollard CM, Abraham JA, Tomlin SM, Radomiljac AL. Parents’ perception of their child's weight status and intention to intervene: A Western Australian cross-sectional population survey 2009–12. Aust N Z J Public Health. 2016;40:68–70. doi: 10.1111/1753-6405.12483. [DOI] [PubMed] [Google Scholar]
- 2.Ribeiro RC, Coutinho M, Bramorski MA, Giuliano IC, Pavan J. Association of the waist-to-height ratio with cardiovascular risk factors in children and adolescents: The three cities heart study. Int J Prev Med. 2010;1:39–49. [PMC free article] [PubMed] [Google Scholar]
- 3.Ruiter ELM, Saat JJEH, Molleman GRM, Fransen GAJ, Velden K van der, Jaarsveld CHM van, et al. Parents’ underestimation of their child's weight status. Moderating factors and change over time: A cross-sectional study. PLoS One. 2020;15:0227761. doi: 10.1371/journal.pone.0227761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rapuano KM, Laurent JS, Hagler DJ, Hatton SN, Thompson WK, Jernigan TL, et al. Nucleus accumbens cytoarchitecture predicts weight gain in children. Proc Natl Acad Sci. 2020;117:26977–84. doi: 10.1073/pnas.2007918117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Noncommunicable diseases: Childhood overweight and obesity. 2020. [Last accessed on2021 Sep 15]. Available from: https://www.who.int/news-room/q-a-detail/noncommunicable-diseases-childhood-overweight-and-obesity .
- 6.Abduelkarem AR, Sharif SI, Bankessli FG, Kamal SA, Kulhasan NM, Hamrouni AM. Obesity and its associated risk factors among school-aged children in Sharjah, UAE. PLoS One. 2020;15:0234244. doi: 10.1371/journal.pone.0234244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Hussaini A, Bashir MS, Khormi M, AlTuraiki M, Alkhamis W, Alrajhi M, et al. Overweight and obesity among Saudi children and adolescents: Where do we stand today? Saudi J Gastroenterol Off J Saudi Gastroenterol Assoc. 2019;25:229–35. doi: 10.4103/sjg.SJG_617_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hashim MS, Abaid SS, Al-Saadi AMMA, Abutiheen AAK. Perceptions and attitudes of parents towards overweight and obesity among their preschool-aged children in Karbala. Karbala J Med. 2020;13:2326–34. [Google Scholar]
- 9.Alexander DS, Alfonso ML, Cao C, Wright AR. Do maternal caregiver perceptions of childhood obesity risk factors and obesity complications predict support for prevention initiatives among African Americans? Matern Child Health J. 2017;21:1522–30. doi: 10.1007/s10995-017-2277-0. [DOI] [PubMed] [Google Scholar]
- 10.Swyden K, Sisson S, Lora K, Weedn A, A S, Degrace B, et al. Relationship between parental perception and concern for child weight and influence on obesogenic parenting practices. Adv Neonatal Care. 2015;2 doi: 10.12715/apr.2015.2.12. [Google Scholar]
- 11.Messiah SE, Weerakoon S, Atem F, Schulte M, Lebron C, Kambali S, et al. Determinants of accurate visual perception of child anthropometric phenotype among ethnically diverse preschool parents in the United States. Health Soc Care Community. 2020;28:2095–104. doi: 10.1111/hsc.13020. [DOI] [PubMed] [Google Scholar]
- 12.Almoosawi S, Jones AR, Parkinson KN, Pearce MS, Collins H, Adamson AJ. Parental perception of weight status: Influence on children's diet in the Gateshead Millennium Study. PLoS One. 2016;11:0144931. doi: 10.1371/journal.pone.0144931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Mohaimeed AA. Parents’ perception of children's obesity, in Al-Qassim, Saudi Arabia. J Fam Community Med. 2016;23:179–83. doi: 10.4103/2230-8229.189134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giannisi F, Pervanidou P, Michalaki E, Papanikolaou K, Chrousos G, Yannakoulia M. Parental readiness to implement life-style behaviour changes in relation to children's excess weight. J Paediatr Child Health. 2014;50:476–81. doi: 10.1111/jpc.12500. [DOI] [PubMed] [Google Scholar]
- 15.Gerards SM, Gubbels JS, Dagnelie PC, Kremers SP, Stafleu A, de Vries NK, et al. Parental perception of child's weight status and subsequent BMIz change: The KOALA birth cohort study. BMC Public Health. 2014;14:291. doi: 10.1186/1471-2458-14-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pasch LA, Penilla C, Tschann JM, Martinez SM, Deardorff J, de Groat CL, et al. Preferred child body size and parental underestimation of child weight in Mexican-American families. Matern Child Health J. 2016;20:1842–8. doi: 10.1007/s10995-016-1987-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cobb J. Child and parent readiness to change in a clinical sample of obese youth. Psychol Diss. 2011. Available from: https://scholarworks.gsu.edu/psych_diss/76 .
- 18.Rhee KE, McEachern R, Jelalian E. Parent readiness to change differs for overweight child dietary and physical activity behaviors. J Acad Nutr Diet. 2014;114:1601–10. doi: 10.1016/j.jand.2014.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al Khashan H, Abogazalah F, Alomary S, Nahhas M, Alwadey A, Al-Khudhair B, et al. Primary health care reform in Saudi Arabia: Progress, challenges and prospects. East Mediterr Health J. 2021;27:1016–26. doi: 10.26719/emhj.21.042. [DOI] [PubMed] [Google Scholar]
- 20.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization. Childhood overweight and obesity. 2017. [Last accessed on2021 Sep 22]. Available from: https://www.who.int/dietphysicalactivity/childhood/en/
- 22.Aljaadi A, Alharbi M. Overweight and Obesity Among Saudi Children: Prevalence, Lifestyle Factors, and Health Impacts. Handbook of Healthcare in the Arab World. 2020 DOI: 10.1007/978-3-319-74365-3_187-1. [Google Scholar]
- 23.Howe CJ, Alexander G, Stevenson J. Parents’ underestimations of child weight: Implications for obesity prevention. J Pediatr Nurs 2017 Nov 1. 37:57–61. doi: 10.1016/j.pedn.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 24.Puhl RM, Heuer CA. The stigma of obesity: A review and update. Obesity. 2009;17:941–64. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 25.Campbell MW-C, Williams J, Hampton A, Wake M. Maternal concern and perceptions of overweight in Australian preschool-aged children. Med J Aust. 2006;184:274–7. doi: 10.5694/j.1326-5377.2006.tb00236.x. [DOI] [PubMed] [Google Scholar]
- 26.Queally M, Doherty E, Matvienko-Sikar K, Toomey E, Cullinan J, Harrington JM, et al. Do mothers accurately identify their child's overweight/obesity status during early childhood?Evidence from a nationally representative cohort study. Int J Behav Nutr Phys Act. 2018;15:56. doi: 10.1186/s12966-018-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Opie CA, Glenister K, Wright J. Is social exposure to obesity associated with weight status misperception?Assessing Australians ability to identify overweight and obesity. BMC Public Health. 2019;19:1222. doi: 10.1186/s12889-019-7556-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nsiah-Kumi PA, Ariza AJ, Mikhail LM, Feinglass J, Binns HJ. Pediatric Practice Research Group. Family history and parents’ beliefs about consequences of childhood overweight and their influence on children's health behaviors. Acad Pediatr. 2009;9:53–9. doi: 10.1016/j.acap.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 29.Raihan N, Cogburn M. Treasure Island (FL): StatPearls Publishing; 2021. [Last accessed on2021 Oct 06]. Stages of Change Theory. In: StatPearls [Internet] Available from: http://www.ncbi.nlm.nih.gov/books/NBK556005/ [PubMed] [Google Scholar]


