Abstract
Postnatal follow-up care is reported to be the ‘underutilised’ aspect of the maternity care continuum. This review explores women’s utilisation of early and late postnatal follow-up and their experiences and satisfaction with it. Five online databases were searched for English or Arabic articles published between 2011 and 2021. Methodological quality of included studies was assessed using the Mixed Methods Appraisal Tool; the Andersen healthcare utilisation model was the framework for data analysis. A total of 19 articles met all inclusion criteria. Utilisation facilitators included complications, travel distance, knowledge of the importance for attending and being offered a telephone call and home visit or clinic visit as options for follow-up. Impediments included lack of perceived need and not being provided with information about postnatal care. Comprehensive discussions with and examination by health providers were reported as positive experiences and influenced repeat utilisation. Dissatisfaction was associated with inconsistent information provided by health providers.
Keywords: Postpartum Period, Postnatal Care, Women, Literature Review
The maternity continuum includes postpartum care, which is delivered following childbirth, most commonly over a six-week period and comprises three stages: the immediate stage (0–24 hours after birth), the early stage (days 2–7) and the late stage (days 8–42).1 Care during the immediate stage is mostly administered in birth facilities, whereas early- and late-stage care is community-based. Care during the postnatal period is as important as antenatal and intrapartum care as complications can arise, resulting in adverse outcomes and leading to increased morbidity and mortality for the mother and/or newborn.1 Moreover, determining women’s satisfaction with postnatal care is essential as it has a direct influence on the utilisation of the postnatal follow-up care.2 Utilisation of healthcare services is crucial for not only women’s physical health but also their mental health. Early detection and management of postnatal mental health conditions such as anxiety and depression are vital, as such conditions have a significant impact not only on the woman but also upon the well-being of the newborn and the entire family.3
The World Health Organization (WHO) recommends that mothers and newborns receive postnatal care at the birthing facility for at least 24 hours.4 However, birthing facilities (e.g. hospitals) in many countries discharge women and their newborns before that time.5 A systematic review by Campbell et al. reported that the length of stay in birthing facilities has decreased, with women staying less than 24 hours following vaginal birth and less than 72 hours following a caesarean section.6 Kumar and Dhillon reported that early discharge underpins the lack of early detection and management of complications for both the mother and the newborn, which increases the risk of morbidity and mortality.7 Early discharge is also associated with increased neonatal readmission within 28 days of birth and increased risks of maternal postpartum depression.5,8
Immediate postnatal care is focused on the immediate general well-being of the mother and newborn following childbirth and involves treating complications, such as infections, perineal pain, vaginal discharge and excessive bleeding and supporting breastfeeding.7,9 Early and late postnatal care tends to focus on maximising maternal and newborn health and well-being through health monitoring and health promotion during postnatal follow-up care.10 This may include screening for maternal postpartum depression, checking and treating childbirth-related complications and having discussions on parenting and family planning.4,11 For the newborn, this covers breastfeeding support, monitoring of the newborn’s growth, development and overall health and referrals for specialised care, if required.1 Additionally, while becoming a new parent is exciting, it can also be a stressful time, particularly for first-time parents and those without strong social support and role models.12 Thus, early and late postnatal periods are important periods during which education from health professionals has the potential to influence positive parenting experiences and healthy child development.12
Forster et al. found that the majority of mothers (90%) viewed their experiences of a flexible model of care, which included early hospital discharge (within 12 hours) and four planned home visits, as positive; the majority (88%) of mothers indicated their willingness to participate in this model of care again.13 Additionally, Yonemoto et al.’s Cochrane systematic review found that home visits were associated with reduced newborn re-admissions in the weeks following birth, continued and exclusive breastfeeding and increased maternal satisfaction with postnatal care.14 The importance of postnatal contacts by healthcare professionals has been further emphasised by the WHO via the recommendation of three contacts following discharge from a health facility or home birth, in line with target three of the Sustainable Development Goals (SDGs).4,15 Thus, scheduled contacts and home visits during the postnatal period are essential to ensuring the ongoing monitoring of maternal and newborn health and well-being.
National and international guidelines and recommendations for immediate, early and late postnatal care following birth at a health facility or at home have been developed by many countries, professional organisations and professional groups.4,11,16–19 Postnatal follow-up is provided in the early and late stages and it appears to vary from two postnatal visits around two and six weeks after birth to three visits starting at day three (47–72 hours), between days seven and 14 and at 42 days after birth.4,16 Additionally, there are reports in the literature that postnatal follow-up care is the “neglected”, under offered and/or underutilised aspect of the maternity care continuum.3,4,20 This may result in lost opportunities for health promotion and monitoring of mothers and their newborns. Promoting postnatal follow-up care is important to the whole family unit as mothers often have the role and responsibility of overseeing the family’s health in both health promotion and illness prevention and of managing ill health.21
Although there are many studies reporting on satisfaction and experiences of immediate postnatal care, less is known about the factors that influence women’s decisions with regard to utilising early and late postnatal follow-up and their experiences and satisfaction with care received. Thus, this review aimed to explore women’s utilisation of early and late postnatal follow-up and their experiences and satisfaction with it.
Methods
This systematic review used the population, exposure and outcome framework to guide the search strategy instead of the population, intervention, comparison and outcome, as the purpose of this review was not to investigate or compare exclusive interventions. Several preliminary searches were performed to identify commonly used keywords and the final search strategy was developed in collaboration with a senior librarian. Wildcard symbols were used in line with database requirements and Medical Subject Headings (MeSH; US National Library of Medicine, Bethesda, Maryland, USA) for PubMed (US National Library of Medicine) and Cumulative Index to Nursing and Allied Health Literature (CINAHL; EBSCO Information Services, Ipswich, Massachusetts, USA) databases, where appropriate. For example, the question mark symbol “?” was used when searching for words that can be spelt with both an ‘s’ or a ‘z’ (utilisation/utilization) or for words with singular and plural forms (woman/women). Between March and April 2021, PubMed (US National Library of Medicine), CINAHL (EBSCO Information Services), Scopus (Elsevier, Amsterdam, the Netherlands), Web of Science (Clarivate Analytics, Philadelphia, Pennsylvania, USA) and Google Scholar (Google LLC, Mountain View, California, USA) electronic databases were systematically searched using the English search terms “wom?n”, “maternal”, “post-partum period”, “post-partum care”, “postnatal care”, “postnatal follow-up”, “home-based”, “utili?ation”, “experience” and “satisfaction”. The language filter was not applied.
Primary studies of any study design that reported one or more of the outcomes of women’s utilisation of or experience or satisfaction with early (2–7 days) or late (8–42 days) postnatal care, irrespective of birth setting (e.g. hospital, health centre, home), were eligible for inclusion. Full text publications in English or Arabic were eligible for inclusion; however, no studies published in Arabic were retrieved. Publications in which data collection occurred within the last 10 years (between January 2011 and July 2021) and within one year of childbirth were eligible. The search parameter was limited to articles published with data collected within the last 10 years to capture recent perspectives from women on postnatal service utilisation, experiences and satisfaction and to limit potential variation in practice change that may have occurred along with changes that have occurred around antenatal and intrapartum care. Studies were excluded if the data included immediate postnatal care and if the data specifically for early and/or late follow-up could not be extracted. Likewise, studies in which the views and experiences of women and their support network (partners or other family members) were presented collaboratively and wherein women’s responses could not be extracted were excluded. Abstracts, thesis, conference proceedings and secondary studies were also excluded.
Search results were uploaded into Zotero reference management software, Version 5.0.96.2. Following the removal of duplicates, title and abstract screening was undertaken independently by three reviewers (AH, JD and MP) and arbitrated by a fourth reviewer (KN), if needed. Review of full texts was undertaken independently by three reviewers (AH, JD and MP) and the opinion of a fourth reviewer (KN) was sought to reach a final decision regarding eligibility when needed.
A data extraction spreadsheet was developed by the review team. Data were extracted by one reviewer (AH) and verified by two others (MP and KN). Any disagreements were discussed to reach consensus. The review team continuously discussed and validated decisions made during all stages of the review process.
The Mixed Methods Appraisal Tool (MMAT) 2018 was used to appraise the included studies as this tool permits the appraisal of qualitative, quantitative descriptive, mixed methods and non-randomised studies and randomised controlled trials.22 Quality assessment is undertaken by answering ‘yes’, ‘no’ or ‘can’t tell’ for five methodological quality criteria specific to each study design. For this review, a quality rating was assigned using a star (*) rating system from one star (20% of quality criteria met = one criterion received yes) to five stars (100% of quality criteria met = five criteria received yes).23 Two reviewers (AH and MP) independently assessed the quality of the included studies and discrepancies were resolved via discussions or the involvement of a third reviewer.24
The data analysis framework was based on the Andersen healthcare utilisation model of predisposing factors, enabling (and impeding) factors and need factors.25 As the review contained quantitative and qualitative studies, numerical data on utilisation and factors reported qualitatively that facilitated or impeded utilisation, influenced experiences positively or negatively and resulted in satisfaction or dissatisfaction with care received were summarised.
Results
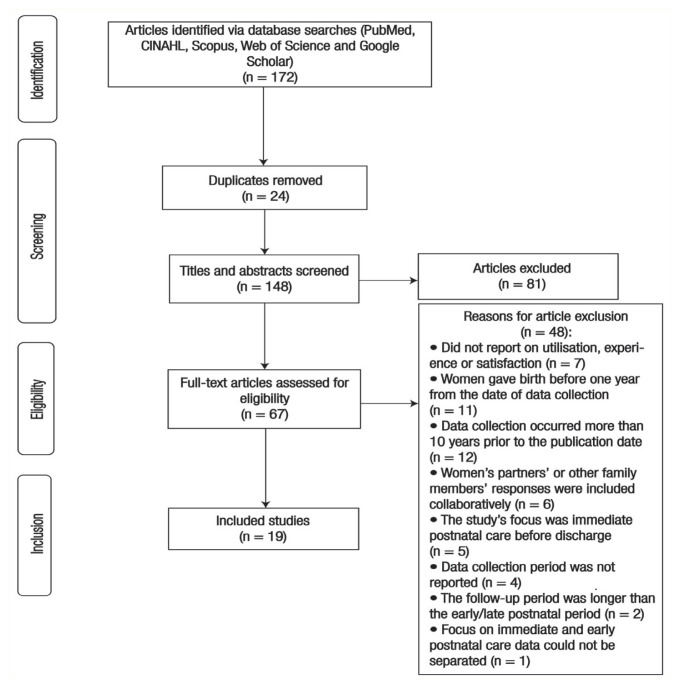
A total of 172 articles were identified as potentially eligible. Following the removal of duplicates and the screening and data extraction processes, a total of 19 studies met the eligibility criteria for inclusion in this review [Figure 1].
Figure 1.
Flowchart showing the article selection process.
CINAHL = Cumulative Index to Nursing and Allied Health Literature.
CHARACTERISTICS OF INCLUDED STUDIES
Included studies were conducted in low-, middle- and high-income countries, with the majority from Africa (n = 9), followed by Asia (n = 5) and Australia (n = 2).26–41 There was one study each from Europe, North America and the Middle East.42–44 The majority of included studies were quantitative and descriptive (n = 11), with participant response rates ranging from 11.4–80.7%.26–29,31,32,34,36,38,39,44 Five studies were qualitative, two were mixed methods and one was an experimental study.30,33,35,37,40–43
Based on the quality assessment of the studies using the MMAT tool, two studies were rated one star because of concerns regarding the clarity on sampling strategies, sample representative of the target population, measurements used, the risk of nonresponse bias and the appropriateness of the statistical analyses.27,39 Most studies (n = 17) were assigned a rating of three or more stars [Table 1].
Table 1.
Characteristics of included studies and the Mixed Methods Appraisal Tool 2018 quality rating
| Author and year of publication | Country | Participants | Methodological characteristics | Postnatal follow-up findings | MMAT quality rating | ||
|---|---|---|---|---|---|---|---|
| Utilisation | Experiences | Satisfaction | |||||
| Abuka Abebo and Jember Tesfaye26 (2018) | Ethiopia | N = 401 women aged 15–49 years who had a live birth within one year prior to the survey |
Study design: Community-based cross-sectional study Data collection: Structured, closed-ended, interviewer-administered, pre-tested questionnaire conducted in 2016 Sampling: Stratified random |
PNC was utilised by 191 (47.6%) women between one and 42 days after birth. Factors that facilitated utilisation: - Maternal education, occupation, household monthly income and joint decision-making (husband/wife dyad) - The greater number of ANC visits was associated with increased postnatal utilisation. Awareness of at least one postpartum danger sign was also associated with increased utilisation. Factors that impeded utilisation: Birthing at home was associated with decreased utilisation. |
Not reported | Not reported | ***** |
| Almalik44 (2017) | Jordan | N = 150 women, aged 17–46 years, recruited on the day of hospital discharge with a follow-up at 6–8 weeks postnatally | Study design: Prospective cohort study Data collection: Self-administrated postpartum learning needs on a 50-item scale completed on the day of discharge; at 6–8 weeks after giving birth, women were asked to complete the postpartum perceived met learning needs scale following a postpartum check-up at a health centre. Data collection occurred in 2015. Sampling: Convenience sampling |
117 (78%) women attended the health centre for a postpartum check-up between 6 and 8 weeks. | - Women who were older, were employed, had a higher level of education, had regular attendance at ANC visits, had a caesarean section and wanted more information, “had higher learning needs”. - Primary unmet learning needs were danger signs post-caesarean section, physical changes, breastfeeding and newborn care. |
Not reported | **** |
| Belihu and Deressa27 (2020) | Ethiopia | N = 332 women with a mean age of 27.8 years who had given birth within six weeks and attended one of four health centres for early postnatal follow-up care (within one week) | Study design: Institution-based cross-sectional study Data collection: Structured interviewer-administered questionnaire designed for the study based on ‘different literatures and modified for the objective of the study’ to assess PNC utilisation at one week after delivery. Data collection occurred in 2018. Sampling: Systematic sampling |
PNC was utilised by only 84 (25.3%) women within the first week. Factors that facilitated early utilisation: Complications during labour and delivery, living within 30 minutes of a health centre, being aware that they should attend for PNC within one week. Factors that impeded early utilisation: Being uninformed and/or not given an appointment for attending care in one week, but for six weeks, living more than a 30-minute walk away from the health centre, partner self-employed (e.g., farmer) and cultural reasons (not specified) |
-The majority of women reported the need for advice on maternal and neonatal postpartum complications. | Not reported | * |
| Brodribb et al.40 (2013) | Australia | N = 88 women, including 18 women aged 21–41 years, involved in the pilot study, recruited in hospital after childbirth and followed-up approximately 10 weeks after birth; 70 women, aged 21–39 years, who had given birth less than two years prior and participated in an evaluation study | Study design: Qualitative studies. -The pilot study investigated primary care services women accessed during the eight-week postpartum period. -The second study evaluated a universal postnatal contact service (including phone contact or a home visit within 10 days of discharge post-birth). -Data were analysed together because both studies asked similar questions regarding postpartum care in the community. Data collection: Data were collected using semi-structured, face-to-face interviews conducted between 2010 and 2012 (study 1) and in 2011 (study 2). Sampling: Not reported |
-Women did not appear to be given consistent information about when they should visit their GP for maternal and newborn postpartum check-ups. -First postpartum visit ranged from five days to 2.5 months, with most visits around six weeks, commonly for the newborn immunisations. -Some women followed instructions given in the newborn personal health record book (recommendation: attend GP within the first four weeks). Factors that facilitated utilisation: Explicit information/instructions (Women who birthed in the public sector compared to the private sector reported having received explicit instructions from a midwife to attend their GP in the first two weeks after childbirth, especially if they were discharged within 48 hours of birth.)Factors that impeded utilisation: Lack of knowledge regarding the reasons for follow-up post-birth, no problems were evident, were multiparous, experienced a sense of abandonment by the hospital and their specialists |
Women reported that GPs were seen for any maternal or infant health issues, whereas knowledge on infant behaviour problems and parenting advice was sought from child and family health centres, telephone advice lines or mothers’ groups. Positive experience factors: Comprehensive discussion of their social situation, how the family was managing, specific questions about problem areas either physical or mental and a comprehensive examination of themselves and their newborn Negative experience factors: Cursory examination with little discussion | Dissatisfaction was associated with the divergence of information given around check-ups: six weeks for mother/newborn; four weeks for baby and six weeks for mother; around five weeks for newborn, mother did not need any check-ups; first 5–10 days for mother/newborn and again at six weeks for mother and eight weeks for newborn or advised at one, two and then four months. | ***** |
| Creanga et al.34 (2017) | Malawi | N = 1,301 women aged 15–49 years who had a live birth within the last 12 months | Study design: Baseline, two-stage cluster sampling household survey Data collection: -self-reported survey with data collected in 2012, prior to implementation of an intervention to improve utilisation and quality of perinatal health services. The questions to assess quality of care were developed separately for each type of PNC using the Hulton framework on quality of maternity care as guide. Sampling: Two-stage cluster sampling |
1,009 (77.5%) postpartum women had at least one postnatal check. Timing of the first postnatal visit for maternal and/or newborn was on average 3.1 weeks and average number of postnatal checks within eight-week postpartum period was 3.1. Factors that facilitated utilisation: Lived close to a health facility (<30 minutes) and history of family planning Factors that impeded utilisation: Lived >1 hour from a health facility | Of the women who answered quality of PNC questions, 90.4% reported they were advised on danger signs to watch for in both themselves and their newborn, 95.4% received breastfeeding support and counselling and 97.9% received counselling on methods to avoid or delay another pregnancy. | Not reported | **** |
| Darega et al.28 (2016) | Ethiopia | N = 703 women, aged ≥18 years, who gave birth within past 12 months | Study design: Community-based cross-sectional study Data collection: Interviewer-administered, structured questionnaires designed for the study, adapted from pertinent literature and pre-tested on 5% of target population not included in the study. Data were collected in 2013. Sampling: Random | Of the total respondents, 556 (79.1%) had heard about PNC services but only 223 (31.7 %) utilised PNC services over a period of up to six weeks. The majority used health extension workers at health aid posts (91.5%) and had home birthed (n = 212, 30.2%). Factors that facilitated utilisation: Utilised ANC services, able to decide for themselves, lived less than 5 km from a health facility | Not reported | Not reported | ***** |
| Gebrehiwot et al.29 (2018) | Ethiopia | N = 367 women, aged >15 years, who had a child aged 45 days up to six months | Study design: Facility-based, cross-sectional study Data collection: Structured questionnaire adapted by reviewing relevant literature and questionnaire such as EDHS 2011 and WHO Guideline for Postnatal Care; pre-tested among 5% of total sample population not selected for the study. Data collection period occurred in 2014. Sampling: Random | 170 (46.3%) knew about the availability of PNC at health facilities; of these, 73 (42.9%) knew the frequency of visits. Only 118 (32.2%) had utilised postnatal follow-up at least once within 42 days of delivery. The majority (51.7%) had first visit between days 15 and 42, 28.8% between days seven and 14 and 19.4% within three days. Of those who utilised follow-up, 38.1% attended for PNC visit, 28% for care of sick mother, 20.3% care of sick baby and 13.6% for baby immunisation. Factors that facilitated utilisation: Had attended ANC at least once, knew about PNC and timing of visits, had attended PNC after previous pregnancy and had complications during delivery, lived within walking distance to the health centre. Women’s occupation (private employees and businesswomen) and education level, husband’s occupation and education level influenced attendance. Factors that impeded utilisation: No knowledge about the availability of PNC services (n = 184, 73.9%), four or more previous children, healthy and high workload in their house | Of the women who had visited a PNC clinic (n = 118), most (n = 103, 87.3%) had experienced receiving less than six elements of postnatal follow-up care, the lowest elements were on personal hygiene, measuring body temperature of the baby, counselling on HIV transmission, baby care and exclusive breast feeding. | Not reported | **** |
| Izudi et al.32 (2017) | Sudan | N = 385 women with a mean age of 27.9 years who attended a postnatal follow-up visit within 2–7 days after birth | Study design: Analytical cross-sectional study Data collection: Data were collected in 2016 via interviews using structured questionnaires at 13 locations (one regional referral hospital, two county hospitals and 10 primary healthcare centres). Sampling: Systematic random and convenience | Only 44 (11.4%) women utilised early PNC (within 2–7 days)Factors that facilitated early utilisation: Secondary level of education or beyond, attended ANC visits, birthed in health facility, had health education on PNC visits, informed about PNC check-ups after birth, knew postpartum complications, had friendly health workers and witnessed presence of health workers at health facilities Factors that impeded early utilisation: Had home birth, accessed health services at government health facilities, reported more than 1 hour to reach the nearest health facility, lived more than 5 km from the nearest health facility | Not reported | Not reported | **** |
| Izudi and Amongin31 (2015) | Uganda | N = 357 women aged 15–49 years who had given birth between one week and one year | Study design: Cross-sectional study Data collection: Structured questionnaire consisting of both open- and closed-ended questions, pretested to assess its acceptability, validity, reliability and appropriateness. Data were collected in 2014. Sampling: Systematic random and convenience. | A total of 288 (80.7%) women had full knowledge of the available PNC services at the nearest health facility. Early PNC (between 2–7 days post-birth) was only utilised by 55 (15.4%) women; 191 women (53.5%) utilised PNC within 42 days post-delivery. Factors that facilitated early utilisation: Formal employment, education about PNC schedules and complications, attendance at private health facility. Factors that impeded early utilisation: PNC at public health facility, not given education on postpartum complications before discharge, self-employed mothers, a long or very long queuing time at the health facility, encountered rude health workers. | Not reported | Not reported | **** |
| Johansson et al.42 (2019) | Sweden | N = 180 healthy women, mostly aged 25 years, of Swedish origin, who had a high level of education, lived with their partner, had an uncomplicated pregnancy and birth and were one week postpartum | Study design: Cross-sectional study using quantitative and qualitative data with a concurrent mixed methods design Data collection: Via an online questionnaire administered one week post-birth. The questionnaire consisted of 22 closed-ended and four open-ended questions. The questionnaire was pilot tested by four parents (both mothers and their partners) who had received similar PNC just before the start of data collection, which took place between 2017 and 2018. Sampling: Purposive (all women who participated in a home-based model of midwifery care over 12 months were invited to participate [n = 247].) | -Early discharge and utilisation of optional postnatal follow-ups by telephone, home visits and hospital visits. -100% utilised telephone contact (mean: 2.06 ± 1.087), 93.9% (n = 169) home visit(s) and 98.3% (n = 177) hospital visit(s) |
152 (84.4%) reported positive PNC experiences. Having the opportunity to receive breastfeeding support and to ask midwives questions contributed to this experience. Positive experience factors: Early discharge followed by home visits (was experienced as personal, calming, comfortable and harmonious), telephone contacts, organised and effective hospital visits as well as having enough time for check-up. Negative experience factors: -Some mothers wanted a longer hospital stay when needing more breastfeeding or informational support before discharge, lack of co-ordination of care when extra check- ups were needed for the infant, being unable to choose the day for the hospital visit or chose either hospital or home visits, stressed professionals, professionals who gave contradicting advice and the father or the family not being involved in the visit. -Also, few mothers had a less positive experience of the home visit, as they perceived that the midwife was unskilled. |
Telephone contact follow-up: 172 (97.2%) women reported being very satisfied or satisfied Home visit follow-up: 163 (96.5%) women reported being very satisfied or satisfied Hospital visit follow-up: 157 (91.3%) women reported being very satisfied or satisfied | **** |
| Laliberté et al.43 (2016) | Canada | N = 472 women aged 18 years and older who had delivered a healthy term singleton infant | Study design: Randomised controlled trial using a 1:2 ratio to randomise mothers to either standard care (control group, n = 157) or mandatory attendance of one visit to a newly established integrative postpartum community-based clinic (intervention group, n = 315) Data collection: Undertaken in 2014; follow-up data were collected from mothers at two, four, 12 and 24 weeks postnatally via a self-report web-based survey (REDCap) or a telephone interview Sampling: stratified random | Intervention group: Could attend the clinic as many times as they desired up to six weeks after birth. A total of 34 (10.8%) did not attend the clinic at all, 56 (17.8%) visited once, 62 (19.7%) visited twice, 64 (20.3%) had three visits and 99 (31.4%) visited four or more times. Control group: Four women withdrew from the study. Data on clinic attendance were not reported. | The experiences of women attending an integrated community-based clinic did not result in significant differences in breastfeeding outcomes (exclusively, partially or any) at two, four or 12 weeks. Similarly, there were no significant differences between the groups for depression scores at three weeks, mean self-efficacy scores at two, four and 12 weeks. | The intervention group was significantly more satisfied with the breastfeeding support they received compared to the control group. They were also satisfied with the breastfeeding clinic in terms of location, physical environment, opening hours and easiness to get an appointment at a convenient time. | **** |
| Ong et al.35 (2014) | Singapore | N = 13 first-time mothers aged 21–39 years were interviewed between 7–11 days post hospital discharge | Study design: Descriptive qualitative study Data collection: One semi-structured interview was conducted with each mother at her home/or at the hospital after early (first) postnatal consultation. An interview guide was developed with the consultation of two experts in qualitative research. Data were collected in 2011–2012. Sampling: Purposive | Not reported | -Information given prior to discharge did not prepare mothers for the postnatal period at home resulting in a perceived lack of knowledge in various aspects of infant and maternal care, including bathing and swaddling, as well as factual information on common normal and abnormal symptoms. -Participant’s experience was that more guidance and support is needed in the early postnatal period and that home visits were needed. -Not all of the women received information of contact details for a ‘hotline’ phone number to contact a health professional when advice is needed post discharge (a standard practice wherein all women should be provided this information). |
Dissatisfaction was expressed around advice given by lactation consultants over the phone regarding breastfeeding (‘impractical advice’) | ***** |
| Sacks et al.33 (2017) | Uganda and Zambia | N = 393 women with a mean age of 26.3 years who had given birth within one year of the data collection period | Study design: Descriptive qualitative nested study (within a larger evaluation study) Data collection: Focus groups (n = 48) were held across four rural contiguous districts in Uganda and four rural non-contiguous districts in Zambia. -Semi-structured interview guides were translated and back translated for accuracy. Data collection took place in 2012–2013. Sampling: Not reported- |
The majority of participants reported not seeking PNC. Factors that facilitated utilisation: Both countries’ community health workers and nurses taught women the importance of PNC Factors that impeded utilisation: Lack of importance in both countries, a healthy mother and baby means no need to seek PNC, cost (for transport and under five card) and distance (reported more in Zambia), fear of mistreatment at health facilities and previous negative experience (being made to wait, yelled at, criticised, physically abused; reported more in Uganda) | In approximately half of the focus groups in both countries, women experienced direct denial of care, discouragement from seeking care or fear of being turned away (predominantly related to having given birth at home). Zambia: Most focus groups reported positive experiences with PNC. Mothers stated that they were ‘received well’ and examined for possible complications and that the nurses’ attitudes were generally positive and ‘welcoming’. Uganda: Most focus groups reported negative experiences with PNC (mostly related to giving birth at home). | In both countries: Women reported being satisfied with PNC given to their newborn when examined, treated for complications, immunised and given an under five card. Zambia: Many women were pleased with the manner in which the nurses attended to them and their newborns. They were also satisfied with the care they received when they developed complications, such as excessive bleeding. | *** |
| Selvaraj et al.36 (2021) | India | N = 227 postnatal mothers aged 19–42 years, between 6–10 weeks post-birth | Study design: Community-based cross-sectional study Data collection: Data were collected using pretested semi-structured proforma was developed based on the PNC assessment as per IPHS guidelines. Data were collected up to four weeks after the completion of the postpartum period (six weeks) in 2015–2016. Sampling: Simple random | Home visits: Only 47 (20.7%) had received at least one home visit by any health worker, with 36 (76.6%) occurring between days 29–42. Seven (14.9%) occurred within first seven days and the remaining four (8.5%) between days 14–28. During these visits, neither the mother nor newborn were assessed for any health problems. None of the mothers had received ‘adequate’ visits (at least three per the IPHS guidelines). Health facility visits: 98 (43.2%) women visited the hospital for themselves (n = 20, 9%) or their newborn (n = 78, 34.4%) during the postnatal period (most frequently for mother: lower back ache, prolonged bleeding, inadequate milk secretion; for newborn: upper respiratory infection, jaundice, physiological issues). | Not reported | Not reported | *** |
| Shahjahan et al.38 (2017) | Bangladesh | N = 360 postnatal mothers, aged >16 years who attended for PNC within 42 days of delivery. | Study design: Community-based cross-sectional study Data collection: Face-to-face interview using a structured questionnaire, which was developed in a simple, accessible language and compiled by adapting questions from published studies with appropriate modifications and/or improvement. The questionnaire was piloted with 20 women prior to use in this study. Data were collected in 2012. Sampling: Recruitment units (Family Welfare Assistant Health Workers) were randomly selected (n = 12) and then 30 women from each health worker catchment area were ‘systematically identified’ for inclusion as the sample. | 64 (17.8%) women utilised PNC services within the first 42 days postnatally (80% of births were home births). 135 (37.5%) women reported they knew that regular PNC was necessary. Factors that facilitated utilisation: High income, higher maternal education (more than nine years schooling), reading newspaper/magazines, watching TV, having mobile phone and those who could walk to the health facility Factors that impeded utilisation: no Education or having 1–5 years of schooling, high transportation cost to the nearest health facility and maternal age | Not reported | Not reported | **** |
| Tesfahun et al.30 (2014) | Ethiopia | N = 820 mothers aged >15 years who had given birth within the past year completed the survey. N = 16 mothers participated in one of three focus groups | Study design: Mixed methods study Data collection: Quantitative data were collected by interview using a structured pre-tested questionnaire. It was developed through review of related Ethiopian and international literature. For the qualitative data, guiding questions for the focus groups were developed in English and translated to Amharic and then checked for validity. Data were collected in 2011. Sampling: Multistage sampling technique was undertaken for the questionnaire, followed by stratified random sampling of wards proportioned for rural and urban, then random sampling of households. If one household hold had more than one eligible mother, then random lottery method undertaken to select the mother. Focus groups: purposive | Questionnaire: -692 (84.4%) women were aware they should attend, and 609 (74.3%) stated it was necessary for women and newborns, but only 548 (66.8 %) utilised PNC services. 371 (67.7%) women attended once, 153 (27.9%) twice and just 24 (4.4%) visited three or more times within six weeks after delivery. Half (52.2%) utilise services from health extension workers and community health outreach services, 49.9% attended a health institution and 0.9% used trained birth attendants. -Reasons for utilising included: newborn immunisation (n = 496, 60.5%), family planning (n = 175, 21.3%), counselling on PNC (n = 129, 15.7%), counselling on breastfeeding (n = 29, 3.5%) and physical examination (n = 15, 1.8%) Factors that facilitated utilisation: Knowing about the PNC service (90.7% who attended knew about the service), being provided with information post-birth about PNC by health extension workers (85.5%), nurses (17.8%), family (8.2%) and doctors (1.1%), maternal age (over 25 years), married, lived in urban area, lived less than two hours from a health facility, had attended ANC, support of a health extension worker Factors that impeded utilisation: Lack of time (30.5%), long distance to provider (19.3%), lack of guardians for children care (16.1%), lack of awareness (12.7%), cultural barriers (8.6%), lack of service (8.6%) and costly transportation (3.4%). A total of 352 (64.2%) women who did not utilise PNC reported not having the ability to make decisions for utilisation. |
Questionnaire: 420 (76.6%) women who utilised PNC had a positive perception towards PNC. Focus Groups: Most mothers assumed that PNC services were only available 45 days after birth (only for newborn vaccinations). Most mothers experienced a positive perception towards PNC, and they encourage others to use PNC. | Not reported | *** |
| Upadhyai and Gupta39 (2019) | India | N = 488 women, <20 to >35 years, who delivered within the past three months | Study design: Cross-sectional community-based study Data collection: Interviews of mothers were conducted in their house using a pretested and predesigned questionnaire. Data were collected for a period from 2014 to 2015. Sampling: Unclear (two-stage systematic random sampling. First stage: slums were identified randomly, and 30 slums were identified. Second stage: proportionate to size, sampling was done in the selected slums to cover the desired sample size of 488 by house-to-house visits. | 159 (32.6%) women received no PNC post-birth and 256 (52.5%) had a postnatal visit within 48 hours of delivery and only 76 (15.6%) received all recommended three or more visits Factors that facilitated utilisation: Age (20–35 years), higher socio-economic class, education level (women and husband), received four or more antenatal check-ups, belongs to joint family, had caesarean delivery, had institutional birth and had complications or perceived health problems after delivery Factors that impeded utilisation: Age (<20 or >35 years), literacy, nuclear family and had a home birth | Not reported | Not reported | * |
| *Woodward et al.41 (2016) | Australia | N = 15 mothers, aged 25–43 years who had an infant aged under 12 months | Study design: Qualitative descriptive Data collection: Semi-structured, face-to-face interview. Data were collected in 2012. Sampling: Purposive | -The majority of women who received private obstetrician care (n = 8) were discharged with a six-week check-up appointment. -Women who birthed in public institutions (n = 4) all received a home visit or a phone call within 10 days of going home. -Community post-birth care utilised included pharmacy nurse (n = 10), child and family health clinic (n = 10) and GP (n = 9). A private midwife was utilised by three women for all postpartum care. |
-The women who received a home visit or phone call experienced reassurance and support through the communication as they could seek and obtain reliable information; this eased their transition to parenting and gave them confidence. -The women who received private obstetrician care experienced receiving a lack of information about where or how to access PNC. -Women experienced psychosocial support by the pharmacy nurses with a focus of positive parenting validation. -Women did not report experiencing psychosocial support and reassurance from GPs or the child and family health clinics. Their experience with GPs was limited to medial issues, health problems or routine vaccinations. |
Satisfaction: The highest levels of satisfaction were reported by women who had a home birth (n = 3) as they received continuous home care by a privately paid for midwife. Women were generally satisfied with PNC provided by the pharmacy nurses as it was accessible and provided continuity of care. Dissatisfaction: -Women expressed dissatisfaction at child and family health clinics around a lack of a ‘women-centred’ approach, continuity of carer and to focused on surveillance rather than support, with the information about where and how to access post-birth care in the community, with PNC at large as they described it as ‘regimented care’ as it focused on infant surveillance rather than support for mothers. -At pharmacies, women were dissatisfied with the physical environment (PNC was provided in an open area of the pharmacy, and it was available for limited hours). |
**** |
| Xiao et al.37 (2020) | China | N = 22 women aged between 22–43 years who had given birth to a healthy term baby within six weeks, without complications, returned to the health centre for a check-up on the 30th or 42nd day after birth | Study design: Qualitative exploratory study Data collection: -In-depth, semi-structured, face-to-face interviews -The demographic information sheet and the interview guide were developed based on the researcher’s experience in working with postpartum women, and discussed with two academics in obstetric nursing and family nursing. Data were collected in 2018. Sampling: Purposive |
All women had received a home visit by a nurse within two days of discharge (standard practice at study site hospital) and additional home visits (not stated/reported for each participant). Also they attended either 30- or 42-day PNC check-up at the hospital. | Home visit nurses were warm and provided continuous care instead of ‘task-oriented’ fragmented care. | Satisfaction: Most women were satisfied with the postpartum home visit but suggested the need for a more comprehensive postpartum care program that catered to their needs. Dissatisfaction: Not receiving timely information from health professionals, suggested need for internet-based or hotline phone support; needing to take their baby to a clinic for examination within the first month (due to cultural beliefs that mothers need to rest and stay at home for a month to regain strength); breastfeeding consultations not part of postpartum home visits | *** |
MMAT = Mixed Methods Appraisal Tool; PNC = postnatal care; ANC = antenatal care; GP = general practitioner; EDHS = Ethiopian Demographic and Health Surveys; WHO = World Health Organization; IPHS = Indian Public Health Standards.
UTILISATION
Overall utilisation rates of 11.4–100% were reported in 15 studies.26–34,36,38,39,42–44 The remaining four studies did not report utilisation rates. Several studies reported that while women were aware of the need for regular postnatal visits or the importance of attending, they did not utilise postnatal follow-up care.30,38
Factors that influenced greater utilisation during early and/or late postnatal periods were complications during labour, birth and after birth, distance from a health centre and knowledge on the importance of postnatal review.27–32,34,38,39 Additionally, women who had completed advanced education (secondary and above), and thus who had higher monthly incomes, were reported as having higher utilisation of postnatal care services.26,29,32,38,39 Several studies reported increased use of postnatal care if women’s husbands had completed advanced education from college and above.29,30,39 Women who were 18–48 years and had attended an antenatal review during pregnancy were more likely to utilise postnatal care.26,28–30,32,39 Women who identified that they were able to decide for themselves or were involved in joint decision-making (husband–wife dyad) were more likely to attend postnatal visits.26,28 Other factors that were reported to increase utilisation of postnatal follow-up care included awareness of at least one postpartum danger sign, attendance at family planning services and use of postnatal care after a previous pregnancy.26,29,34
Major factors reported by women that impeded the utilisation of postnatal services included a lack of knowledge about postnatal services, beliefs that there was no need for postnatal review if one was feeling well, not being given information regarding postnatal complications before discharge, long distance to health facilities, high transportation costs, home birth, cultural barriers and lack of education, long queues at health facilities, experiences of abandonment by healthcare providers and fears of mistreatment by health professionals.26,27,29–34,38–40 There were also additional impediments [Table 1].
EXPERIENCES
A total of 12 studies reported women’s experiences, with most reporting positive and negative factors that influenced their experiences.27,29,30,33–35,37,40–44 Several studies reported that women felt they were not provided with enough information on maternal and newborn postpartum complications or ‘danger signs’, physical changes, breastfeeding and general maternal and newborn care [Table 1].27,35,44
Gebrehiwot et al. found that women had experienced receiving advice or information on fewer than six elements of postnatal care at postnatal follow-up visits.29 The least discussed elements included exclusive breastfeeding, baby care and personal hygiene. Ong et al. reported that women felt that more guidance and support was needed during the early postnatal period, particularly with regard to breastfeeding and also expressed the need for more home visits due to expectations around cultural postnatal confinement practices.35
Women’s positive experiences were predominantly related to quality time with and comprehensive information provided by the healthcare provider.34,37,40 Three women who received early contact after discharge (home visit, telephone contact) reported feeling reassured and supported.41,42 Postnatal follow-up care that was organised and effective and allowed sufficient time for check-up of both the mother and infant was viewed positively.
Negative experiences were more commonly reported by women and were related to cursory examinations or unfulfilling discussions with health professionals, conflicting information given by health professionals and not receiving adequate or enough information from health professionals.29,30,35,40–42 In some countries, women reported experiencing a direct denial of care, discouragement from seeking care or fear of being turned away, particularly if they had given birth at home [Table 1].33
SATISFACTION
The majority of studies (n = 12) did not report on women’s satisfaction with postnatal follow-up care. Satisfaction or dissatisfaction when reported was mostly associated with consistency of advice received and continuity of care.33,37,40–43
Johansson et al. reported that women were satisfied with telephone follow-up (97.2%), home visit (96.5%) and hospital follow-up (91.3%).42 Woodward et al. found that women who had home births were satisfied with follow-up when they received continuity of care.41 Women who attended an integrated community-based clinic providing comprehensive support for postpartum women reported that they were satisfied with the breastfeeding support they received.43
Women reported dissatisfaction with divergent information and impractical advice as well as with a lack of timely advice and a ‘women-centred’ approach and continuity of care [Table 1].35,37,40,41
Discussion
This review aimed to explore women’s utilisation of early and late postnatal follow-up and their experiences and satisfaction with it. Overall, the majority of the included studies when appraised using the MMAT tool were assessed as meeting three or more of the five quality criteria.26,28–38,40–44
Low utilisation was mostly reported from low- and middle-income countries (LMICs).26–29,31–33 This finding could be attributed to limited postnatal follow-up care options offered to women and newborns in LMICs, such as lack of home visits and telephone contact, compared to high-income countries. A number of studies reported the use of mobile technology such as short message service as being a cost-effective method in enhancing maternal and newborn outcomes in early postnatal period in both low- and high-income settings.45,46 Furthermore, Perrenoud et al. reported that immediate messaging application from ‘Whatsapping’ contributes to women-centred care and enhances continuity of care.47 This aligns with the recommendations of the American College of Obstetrics and Gynecologists on optimising women’s and newborns’ health through offering various services to meet individualised needs.17
The limited services reflect the distinctive distribution of maternal and newborn deaths globally. International organisations reported that approximately 295,000 maternal deaths occurred globally in 2017, and 86% of these occurred in Sub-Saharan Africa and South Asia.48 In addition, it is estimated that 2.4 million neonatal deaths occurred globally in 2019.49 As such, improving maternal health and putting an end to preventable maternal deaths have been the focus of various organisations, such as the WHO through its launch of the SDGs.
An examination of utilisation is needed to identify potential target areas to improve the quality and use of healthcare services provided during the postnatal period. Many of the included studies undertaken in LMICs focused on the utilisation of postnatal care and reported low overall rates, which appeared to be associated with transport costs, distances to health centres and the importance of postnatal follow-up care not being conveyed by healthcare professionals around the time of discharge from hospitals.26–32,34,36,38,39,43,44 Comparatively, the studies conducted in high-income countries reported high rates of utilisation, and the focus was on experiences and satisfaction with postnatal services.35,37,40–43
While some women reported a lack of awareness of the need or availability of services, others who were aware still did not use these services or were likely to use them only once.26,27,29,30,34,36,38–41,44 It appears that women were most likely to utilise postnatal care services during the late postnatal period, despite the fact that the WHO recommends at least three contacts following childbirth: on day three, between days seven and 14 and at six weeks.26,29,31,32,34,36,40,41,44 Women seem to have fewer than the recommended number of contacts during the postnatal period. A lack of knowledge regarding the accessibility and importance of postnatal care services was reported in a number of studies.27,29,33,40 While the study by Angore et al. could not be included in this review as it reported on women using postnatal follow-up care over one year, it is crucial to note that the authors found that women who were informed about the importance of attending postnatal care services after birth had high utilisation rates.50
Cultural practices surrounding non-utilisation did not feature strongly in the studies undertaken in Africa or India. In contrast, the study by Ong et al. with Singaporean mothers in Asian countries revealed that traditional practices, such as ‘seclusion’, may account for the lack of use of care services within the first two weeks postpartum.35 A study conducted by Almalik in Jordan reported that 78% of women attended postnatal follow-up between six and eight weeks, with a focus on whether attendance met their perceived requirements.44 To the best of the authors’ knowledge, no data has been published on either the early postnatal period or the influence of cultural practices such as seclusion, which is practiced in the Middle East. The practice of seclusion is well known in Middle Eastern countries, such as Oman, where women are expected to be confined to their homes for 40 days, to rest and eat traditional foods (e.g. honey) to regain strength and be healthy to take care of their newborn.51 During this period, the mother and newborn are viewed as vulnerable and at high risk for illness and death as well as the ‘evil eye’.52 The women in Ong et al.’s study reported the need for more home visits during this early period when they cannot leave the house.35
Access to detailed information about the postnatal period was reported to have a positive influence on maternal experience.34,37,40,42 In contrast, the scarcity of information was associated with maternal dissatisfaction and increased breastfeeding problems, especially at 3–6 weeks after birth.30,35,41
Women’s satisfaction with the care provided during the postnatal period was explored in a number of studies.33,37,40–43 Women appeared to be dissatisfied when there was a lack of consistent information provided and satisfied when there was continuity of care provided.40,41 Interestingly, two Australian studies reported a lack, or inconsistency, of information.40,41 This may be due to the lack of clarity in the Royal Australian College of General Practice guidelines, which do not make any recommendations regarding the timing and number of postnatal contacts.19
Women reported that information provided by health providers was not practical or helpful and that there was a need for more targeted education, especially related to breastfeeding, physical changes and newborn care.27,35,44 Interestingly, however, Laliberté et al. found that the provision of a community-based clinic with a focus on providing breastfeeding support did not result in significant differences in breastfeeding outcomes or depression scores up to 12 weeks postnatally when comparing women who visited the clinic and those who did not.43 That study concluded that the reason for the lack of significant differences between the two groups could be that the majority of the women were over 29 years old and had a high educational level, hypothesising that this group of well-educated women sought advice from other sources.
Health providers’ provision of information and the way in which information is provided are important to women. Almalik stated that women reported unmet needs at 6–8 weeks and emphasised the need to change policymakers’ focus from reducing maternal mortality rates to providing more women-centred approaches that address their needs and concerns.44 Similarly, in Woodward et al.’s Australian study, women attending a community-based child and family health clinic felt that the nurses/midwives were more interested in collecting data and undertaking surveillance than providing support and positive parenting advice.41 Women in that study found nurses/midwives located in pharmacies to be much more supportive. Thus, the attitudes of health professionals play an important role in whether women seek follow-up care.30,53 This was evident in low-income country settings where women reported they were reluctant to attend postnatal follow-up care because of health workers’ attitudes and fear of mistreatment.31,33
The findings of this review should be considered in light of its strengths and potential limitations. A strength of this review was that the systematic search was developed in conjunction with a senior librarian and was not limited by study design, country context or postnatal follow-up setting. The English language filter was not applied; however, searching with MeSH terms and keywords was undertaken in English only. Therefore, it was unlikely for articles published in Arabic but without an English-translated abstract and keywords to have appeared in the search results. The selection of studies was restricted to data collection taken place within the last 10 years and from women who had given birth within 12 months of the study period, to ensure that the information was contemporary and to limit potential variation in practice change that may have occurred along with changes in and around antenatal and intrapartum care. Additionally, while women’s recall has been shown to be consistent around antenatal and childbirth events, this is not the case for the postnatal period, with sensitivity of reporting lower at six weeks and six months than at one week postnatally.54 Only studies that collected data up to 12 months following childbirth were included in this review; therefore, future reviews should consider studies in which participants are interviewed or surveyed within a shorter time frame following the six-week follow-up appointment. This may provide additional insights due to increased clarity of recall.
Conclusion
This systematic review highlights the need for increasing women’s awareness of the importance of postnatal follow-up care. This includes discussing postnatal anxiety and depression, providing more individualised options for receiving postnatal follow-up care such as telephone call, home visit or health facility visit and improving conformity of information provided to women by healthcare providers. These could be facilitated by providing written/electronic resources to women around the time of discharge after childbirth, mandating annual training for healthcare providers and ensuring that local policies are aligned with national policies and guidelines. Future research should explore the influence of social and cultural practices on the utilisation of postnatal follow-up care and alignment of postnatal follow-up services and policies such that they are women-centred and culturally acceptable.
ACKNOWLEDGEMENT
The authors would like to thank Mr Michael Fagg, the expert senior librarian at the University of Queensland, for his support during the systematic search for relevant studies.
Footnotes
AUTHORS’ CONTRIBUTIONS
AH, MP, JD, KW and KN conceptualised and designed the study. AH administered the study, while MP, JD, KW and KN supervised the work. AH, MP and KN analysed the data. All authors drafted, reviewed and edited the manuscript. All authors approved the final version of the manuscript.
References
- 1.World Health Organization. WHO Technical Consultation on Postpartum and Postnatal Care. Geneva: World Health Organization WHO/MPS/1003; p. 12. [PubMed] [Google Scholar]
- 2.Odetola TD, Fakorede EO. Assessment of perinatal care satisfaction amongst mothers attending postnatal care in Ibadan, Nigeria. Ann Glob Health. 2018;84:36–46. doi: 10.29024/aogh.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McLellan J, Laidlaw A. Perceptions of postnatal care: Factors associated with primiparous mothers perceptions of postnatal communication and care. BMC Pregnancy Childbirth. 2013;13:227. doi: 10.1186/1471-2393-13-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. WHO Recommendations on Postnatal Care of the Mother and Newborn. [Accessed: Jan 2022]. From https://www.ncbi.nlm.nih.gov/books/NBK190086/pdf/Bookshelf_NBK190086.pdf. [PubMed]
- 5.Jones E, Stewart F, Taylor B, Davis PG, Brown SJ. Early postnatal discharge from hospital for healthy mothers and term infants. Cochrance Database of Syst Rev. 2021;6:CD002958. doi: 10.1002/14651858.CD002958.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Campbell OM, Cegolon L, Macleod D, Benova L. Length of stay after childbirth in 92 countries and associated factors in 30 low- and middle-income countries: Compilation of reported data and a cross-sectional analysis from nationally representative surveys. PLoS Med. 2016;13:e1001972. doi: 10.1371/journal.pmed.1001972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumar P, Dhillon P. Length of stay after childbirth in India: A comparative study of public and private health institutions. BMC Pregnancy Childbirth. 2020;20:181. doi: 10.1186/s12884-020-2839-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bravo P, Uribe C, Contreras A. Early postnatal hospital discharge: The consequences of reducing length of stay for women and newborns. Rev Esc Enferm USP. 2011;45:758–63. doi: 10.1590/S0080-62342011000300030. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Improving Early Childhood Development: WHO Guideline. Geneva: World Health Organization; p. 29. [PubMed] [Google Scholar]
- 10.Finlayson K, Crossland N, Bonet M, Downe S. What matters to women in the postnatal period: A meta-synthesis of qualitative studies. PLoS One. 2020;15:e0231415. doi: 10.1371/journal.pone.0231415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Institute for Health and Care Excellence. Postnatal Care up to 8 Weeks After Birth. London: National Institute for Health and Care Excellence; [Accessed: Jan 2022]. From: https://www.nice.org.uk/guidance/ng194/resources/postnatal-care-pdf-66142082148037. [Google Scholar]
- 12.Bryanton J, Beck CT, Montelpare W. Postnatal parental education for optimizing infant general health and parent-infant relationships. Cochrane Database Syst Rev. 2013:CD004068. doi: 10.1002/14651858.CD004068.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Forster DA, Savage TL, McLachlan HL, Gold L, Farrell T, Rayner J, et al. Individualised, flexible postnatal care: A feasibility study for a randomised controlled trial. BMC Health Serv Res. 2014;14:569. doi: 10.1186/s12913-014-0569-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yonemoto N, Dowswell T, Nagai S, Mori R. Schedules for home visits in the early postpartum period. Cochrane Database Syst Rev. 2017;8:CD009326. doi: 10.1002/14651858.CD009326.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.United Nations. Transforming our World: The 2030 Agenda for Sustainable Development. [Accessed: Jan 2022]. From https://sustainabledevelopment.un.org/content/documents/21252030%20Agenda%20for%20Sustainable%20Development%20web.pdf.
- 16.Sultanate of Oman Ministry of Health. Pregnancy and Childbirth Management Guidelines. ML-60. Muscat: Sultanate of Oman Ministry of Health; 2016. pp. 105–8. [Google Scholar]
- 17.McKinney J, Keyser L, Clinton S, Pagliano C. ACOG Committee Opinion No. 736: Optimizing postpartum care. Obstet Gynecol. 2018;132:784–5. doi: 10.1097/AOG.0000000000002849. [DOI] [PubMed] [Google Scholar]
- 18.International Confederation of Midwives. Essential Competencies for Midwifery Practice. London: International Confederation of Midwives; pp. 19–21. [Google Scholar]
- 19.Royal Australian College of General Practitioners. Guidelines for Preventive Activities in General Practice. Victoria: Royal Australian College of General Practitioners; pp. 127–38. [Google Scholar]
- 20.Langlois ÉV, Miszkurka M, Zunzunegui MV, Ghaffar A, Ziegler D, Karp I. Inequities in postnatal care in low-and middle-income countries: A systematic review and meta-analysis. Bull World Health Organ. 2015;93:259–70. doi: 10.2471/BLT.14.140996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McGuigan K. Master’s Thesis. Massey University; Albany, New Zealand: 2012. The Role of Mothers in Family Health: A Thesis Presented in Partial Fulfilment of the Requirements for the Degree of Masters of Science in Psychology at Massey University, Albany, New Zealand. [Google Scholar]
- 22.Pluye P, Robert E, Cargo M, Bartlett G, O’Cathain A, Griffiths F, et al. Mixed Methods Appraisal Tool (MMAT) – Version 2011. [Accessed: Jul 2021]. From: http://mixedmethodsappraisaltoolpublic.pbworks.com.
- 23.Reporting the results of the MMAT (version 2018) [Accessed: Jul 2021]. From: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/140056890/Reporting%20the%20results%20of%20the%20MMAT.pdf.
- 24.Elshafay A, Omran ES, Abdelkhalek M, El-Badry MO, Eisa HG, Fala SY, et al. Reporting quality in systematic reviews of in vitro studies: A systematic review. Curr Med Res Opin. 2019;35:1631–41. doi: 10.1080/03007995.2019.1607270. [DOI] [PubMed] [Google Scholar]
- 25.Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav. 1995;36:1–10. doi: 10.2307/2137284. [DOI] [PubMed] [Google Scholar]
- 26.Abuka Abebo T, Jember Tesfaye D. Postnatal care utilization and associated factors among women of reproductive age group in Halaba Kulito Town, Southern Ethiopia. Arch Public Health. 2018;76:9. doi: 10.1186/s13690-018-0256-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Belihu TM, Deressa AT. Postnatal care within one week and associated factors among women who gave birth in Ameya District, Oromia Regional State, Ethiopia, 2018: Cross sectional study. Ethiop J Health Sci. 2020;30:329–36. doi: 10.4314/ejhs.v30i3.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Darega B, Dida N, Tafese F, Ololo S. Institutional delivery and postnatal care services utilizations in Abuna Gindeberet District, West Shewa, Oromiya Region, Central Ethiopia: A community-based cross sectional study. BMC Pregnancy Childbirth. 2016;16:149. doi: 10.1186/s12884-016-0940-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gebrehiwot G, Medhanyie AA, Gidey G, Abrha K. Postnatal care utilization among urban women in Northern Ethiopia: Cross-sectional survey. BMC Womens Health. 2018;18:78. doi: 10.1186/s12905-018-0557-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tesfahun F, Worku W, Mazengiya F, Kifle M. Knowledge, perception and utilization of postnatal care of mothers in Gondar Zuria District, Ethiopia: A cross-sectional study. Matern Child Health J. 2014;18:2341–51. doi: 10.1007/s10995-014-1474-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Izudi J, Amongin D. Use of early postnatal care among postpartum women in Eastern Uganda. Int J Gynaecol Obstet. 2015;129:161–4. doi: 10.1016/j.ijgo.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 32.Izudi J, Akwang GD, Amongin D. Early postnatal care use by postpartum mothers in Mundri East County, South Sudan. BMC Health Serv Res. 2017;17:442. doi: 10.1186/s12913-017-2402-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sacks E, Masvawure TB, Atuyambe LM, Neema S, Macwan’gi M, Simbaya J, et al. Postnatal care experiences and barriers to care utilization for home- and facility-delivered newborns in Uganda and Zambia. Matern Child Health J. 2017;21:599–606. doi: 10.1007/s10995-016-2144-4. [DOI] [PubMed] [Google Scholar]
- 34.Creanga AA, Gullo S, Kuhlmann AKS, Msiska TW, Galavotti C. Is quality of care a key predictor of perinatal health care utilization and patient satisfaction in Malawi? BMC Pregnancy Childbirth. 2017;17:150. doi: 10.1186/s12884-017-1331-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ong SF, Chan WC, Shorey S, Chong YS, Klainin-Yobas P, He HG. Postnatal experiences and support needs of first-time mothers in Singapore: A descriptive qualitative study. Midwifery. 2014;30:772–8. doi: 10.1016/j.midw.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 36.Selvaraj R, Ramakrishnan J, Sahu SK, Kar SS, Roy G. Community-based assessment of postnatal care in Puducherry—A cross-sectional study. J Family Med Prim Care. 2021;10:798–803. doi: 10.4103/jfmpc.jfmpc_1083_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xiao X, Ngai FW, Zhu SN, Loke AY. The experiences of early postpartum Shenzhen mothers and their need for home visit services: A qualitative exploratory study. BMC Pregnancy Childbirth. 2019;20:5. doi: 10.1186/s12884-019-2686-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shahjahan M, Chowdhury HA, Al-Hadhrami AY, Harun GD. Antenatal and postnatal care practices among mothers in rural Bangladesh: A community based cross-sectional study. Midwifery. 2017;52:42–8. doi: 10.1016/j.midw.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 39.Upadhyai N, Gupta SK. Utilization of postnatal care services and factors affecting it among women of urban slums in Dehradun, Uttarakhand. Indian J Community Health. 2019;31:470–6. doi: 10.47203/IJCH.2019.v31i04.009. [DOI] [Google Scholar]
- 40.Brodribb W, Zadoroznyj M, Dane A. The views of mothers and GPs about postpartum care in Australian general practice. BMC Fam Pract. 2013;14:139. doi: 10.1186/1471-2296-14-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Woodward BM, Zadoroznyj M, Benoit C. Beyond birth: Women’s concerns about post-birth care in an Australian urban community. Women Birth. 2016;29:153–9. doi: 10.1016/j.wombi.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 42.Johansson M, Thies-Lagergren L, Wells MB. Mothers’ experiences in relation to a new Swedish postnatal home-based model of midwifery care–A cross-sectional study. Midwifery. 2019;78:140–9. doi: 10.1016/j.midw.2019.07.010. [DOI] [PubMed] [Google Scholar]
- 43.Laliberté C, Dunn S, Pound C, Sourial N, Yasseen AS, 3rd, Millar D, et al. A randomized controlled trial of innovative postpartum care model for mother-baby dyads. PLoS One. 2016;11:e0148520. doi: 10.1371/journal.pone.0148520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Almalik MM. Understanding maternal postpartum needs: A descriptive survey of current maternal health services. J Clin Nurs. 2017;26:4654–63. doi: 10.1111/jocn.13812. [DOI] [PubMed] [Google Scholar]
- 45.Jones RM, Kimenju G, Subbiah S, Styles A, Pearson N, Rajasekharan S. A short message service (SMS) increases postpartum care-seeking behavior and uptake of family planning of mothers in peri-urban public facilities in Kenya. PLoS One. 2020;15:0239213. doi: 10.1371/journal.pone.0239213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Patel A, Kuhite P, Puranik A, Khan SS, Borkar J, Dhande L. Effectiveness of weekly cell phone counselling calls and daily text messages to improve breastfeeding indicators. BMC Pediatr. 2018;18:337. doi: 10.1186/s12887-018-1308-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Perrenoud P, Chautems C, Kaech C. “Whatsapping” the continuity of postpartum care in Switzerland: A socio-anthropological study”. Women Birth. 2022;35:e263–74. doi: 10.1016/j.wombi.2021.06.009. [DOI] [PubMed] [Google Scholar]
- 48.World Health Organization United Nations Population Fund, World Bank Group and the United Nations Population Division. Trends in Maternal Mortality 2000 to 2017. [Accessed: Jan 2022]. From https://www.unfpa.org/sites/default/files/pub-pdf/Maternal_mortality_report.pdf.
- 49.World Health Organization. Newborns: Improving Survival and Well-being. [Accessed: Jan 2022]. From https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality.
- 50.Angore BN, Tufa EG, Bisetegen FS. Determinants of postnatal care utilization in urban community among women in Debre Birhan Town, Northern Shewa, Ethiopia. J Health Popul Nutr. 2018;37:10. doi: 10.1186/s41043-018-0140-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Missal B. Gulf Arab women’s transition to motherhood. J Cult Divers. 2013;20:170–6. [PubMed] [Google Scholar]
- 52.Hundt GL, Beckerleg S, Kassem F, Abu Jafar AM, Belmaker I, Abu Saad K, et al. Women’s health custom made: Building on the 40 days postpartum for Arab women. Health Care Women Int. 2000;21:529–42. doi: 10.1080/07399330050130313. [DOI] [PubMed] [Google Scholar]
- 53.Adams Y. PhD Thesis. Michigan State University; Michigan, USA: 2016. Use of postpartum care services in rural central Malaw; pp. 55–63. [Google Scholar]
- 54.Zimmerman LA, Shiferaw S, Seme A, Yi Y, Grove J, Mershon CH, et al. Evaluating consistency of recall of maternal and newborn care complications and intervention coverage using PMA panel data in SNNPR, Ethiopia. PLoS One. 2019;14:e0216612. doi: 10.1371/journal.pone.0216612. [DOI] [PMC free article] [PubMed] [Google Scholar]