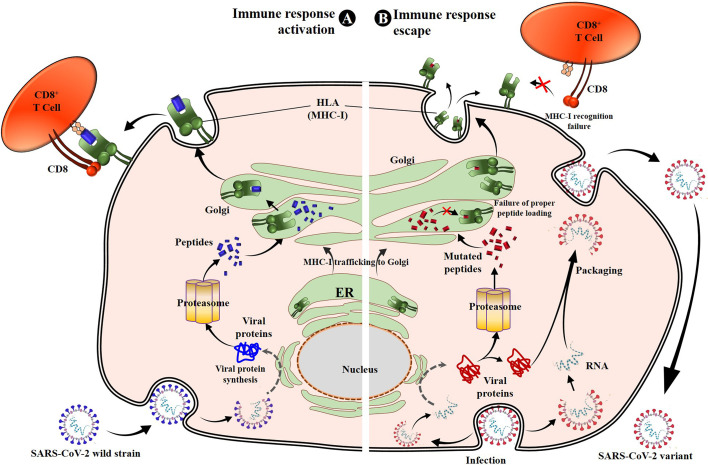
Figure 4.
SARS-CoV-2 S protein mutations prevent cellular immunity activation. Once entered into the target cell, SARS-CoV-2 releases its genomic RNA, which serves to produce the viral proteins, including structural and nonstructural proteins. Recognized as non-self-molecules, antigen processing and presentation pathways occur for viral protein lysis into peptides that are then loaded onto the MHC-I or HLA molecules and presented to CD8+ CTLs, activating the cell cytotoxic response. The CD8+ T cells produce numerous toxic substances (perforins, granzyme, and FasL) and cytokines (IFN-γ, TNF-α, and IL-2) directly involved in SARS-CoV-2–infected cell death (A) (30, 32). However, because of the mutations in specific antigen peptides (such as spike-mutated derived antigens), these later lose their binding affinity to HLA-I. Consequently, the peptides are either not loaded or unstably loaded onto the corresponding HLA molecules. This leads to the reduction or non-activation of the CD8+ T cells through low affinity or absence of HLA-I-peptide recognition by TCR, resulting in cellular immune escape and infection maintenance by SARS-CoV-2 variants (B). MHC-I, major histocompatibility complex type I; CTL, cytotoxic T lymphocyte.