Abstract
Background: The number of adults requiring prolonged mechanical ventilation (PMV) including those with cognitive impairment or disorders of consciousness is escalating. We aimed to compare in a long-term acute care hospital (LTACH) mortality and length of stay (LOS) among three age groups (40-59y, 60-79y, ≥80y) of hospitalized PMV patients, and according to consciousness and cognitive state at admission. Methods: We obtained data from the health records of 308 adults aged ≥40 years requiring PMV hospitalized at a Chronic Ventilator Dependent Unit in a LTACH between 01/01/2015 to 06/30/2019 and followed-up until discharge or death or until 12/31/2019. Results: At admission to LTACH, 42.2% of PMV patients were in a vegetative state/ minimally conscious state (VS/MCS); 32.5% were severely cognitively impaired, 11.0% were mildly to moderately cognitively impaired, 12.3% had no cognitive impairment, and 1.9% had intellectual disability/psychiatric disorder. In-LTACH LOS (months) decreased from 34.6 ± 42.6 at age 40–59y, 19.1 ± 22.3 at 60–79y to 14.4 ± 19.3 at age ≥80y (p = .006). In-LTACH mortality was 30.6% for 40–59y, 41.1% for 60–79y and 54.8% for age ≥80y. In-LTACH LOS (months) was 23.8 ± 30.7 for VS/MCS, 15.1 ± 19.5 for the severely cognitively impaired, 10.0 ± 12.8 for mild to moderate cognitive impairment and 18.9 ± 21.9 for those without cognitive impairment (p = .02). In-LTACH mortality was 50.8% for VS/MCS, 58.0% for the severely cognitively impaired, 26.5% for mild to moderate cognitive impairment and 13.2% for those without cognitive impairment (p < .001). Conclusion: In this population requiring PMV, mortality and in-LTACH LOS worsened with age. In-LTACH LOS was longest for VS/MCS patients, who had a mean survival of about two years, followed by those without cognitive impairment and then those with severe cognitive impairment. Mortality was associated with worse consciousness and cognitive state. These findings highlight the importance of discussing end-of-life decisions with patients and family members regarding resuscitation/intubation and the long-term management of these patients.
Keywords: age, cognitive impairment, disorders of consciousness, long-term ventilation facility, outcome, prognosis, prolonged mechanical ventilation
Introduction
Acute and chronic illnesses associated with high mortality, eg respiratory failure, have seen improved survival due to the current advances in critical care. Much of the current literature on patients with respiratory failure has focused on short-term outcomes including hospital mortality and short-term ventilator weaning.1–3 However, survival for many of these patients described as the "chronically critically ill" is contingent upon continued intensive support beyond their acute hospital stay.2,3 For that reason, attention needs to focus on their long-term outcomes.4,5 Not only is the latter bleak, with a high degree of morbidity and mortality,3,6,7 the enduring cost of this ever-growing population is significant and has increased exponentially. Costs are approximately $35 billion annually in the United States alone in 20158 up from $20 billion in 2010.3 In order to free hospital beds of patients receiving prolonged mechanical ventilation (PMV), long-term acute-care hospitals (LTACH) have begun to receive this growing patient population. However, evidence is scarce relating to survival and functional outcomes as well as relating to quality of life for patients,families, and caregivers. In a study of chronically ventilated patients treated either in an acute-care hospital or transferred to a LTACH, there was no statistically significant difference in the six-month mortality rate, but admission to the LTACH was associated with a longer mean survival time. Moreover, hospital cost of care when referred to a LTACH was approximately one quarter less than treatment exclusively at an acute care hospital (ACH).9
Few studies have investigated the characteristics of survivors of critical illness in need of continued mechanical ventilation. Some patients require prolonged respiratory support due to neurological or neurodegenerative diseases eg, amyotrophic lateral sclerosis or Duchenne muscular dystrophy or due to end-stage heart and lung diseases. Another growing group of patients comprises survivors of cardio-pulmonary resuscitation with severe anoxic brain damage, who are in vegetative or minimally conscious state (VS/MCS). In a recent meta-analysis of critically ill adults treated with prolonged ventilation for 14 days or more, mortality was associated with age, vasopressor requirement, thrombocytopenia and kidney disease.10 Frengley et al11 studied a public LTACH in New York City with an active program for ventilator weaning from PMV. They found that meeting weaning criteria and successful weaning decreased with increasing age. However, age was not the dominant factor in predicting outcomes; thus individuals with PMV with better respiratory physiology and lower comorbidity burdens were more likely to be weaned successfully and to have longer survival, regardless of their age. Of interest, only 20 of the 540 patients (4%) were discharged to their home.11 Of note, even after discharge from LTACH, outcomes remain bleak. In an early study of Schönhofer et al, the five year survival rate after discharge from LTACH estimated from 21 at-risk patients was 33%, and the survival rate declined steeply from three months post-hospital discharge (67%) to three years (38%).12
In Israel, the Dying Patient Act of 2005 enables patients with end-stage diseases to formulate advance directives determining whether they want aggressive treatments near the end of life. Contrary to most countries, it is illegal to withdraw continuous life-sustaining treatment such as mechanical ventilation, or to disconnect ventilator dependent patients, or to hasten death actively. Thus, these patients, who cannot be weaned, are ventilated indefinitely until their disease progresses, or until complications develop.4,13 Hence, a patient may arrive ventilated to the emergency room (ER) after out of hospital resuscitation; in cases where prognosis appears poor, terminal weaning is prohibited, consequently the patient stays ventilated in ACH until being transferred to LTACH. Furthermore, due to the lack of advance directives and cultural and religious factors in Israel, people suffering from end stage diseases, even those with severe physical and cognitive impairment, are often intubated and mechanically ventilated for prolonged periods. Relatives of these chronically ventilated patients sometimes find it difficult to make end-of-life decisions for their loved ones, thus choose to continue life-sustaining treatments indefinitely,13 which poses a substantial administrative, financial, ethical, and emotional burden for caretakers, policy makers, patients, and relatives. The unique situation in Israel allows us to describe the natural history of this patient population and their outcomes over time, including physical and cognitive functions, in order to improve prognostication and future planning of chronic care facilities required to take care of this increasing population.
To better understand this patient population, we describe and analyze clinical characteristics and long-term functional and cognitive outcomes in a group of 308 adult patients undergoing PMV at a single center in Jerusalem. We divided and compared them according to three age groups and five consciousness and cognitive states, expecting to find worse outcomes for the oldest age group and for those with worse cognitive impairments.
Methods
Setting
The study was conducted at the 110-bed Chronic Ventilator Dependent Unit at Herzog Medical Center, a university affiliated geriatric LTACH in Jerusalem, Israel. All patients admitted were ventilated in the three acute hospitals of the Greater Jerusalem area, but failed weaning attempts and underwent tracheostomy. Criteria for admission together with the latter was hemodynamic stability. Poor weaning potential and prognosis were not exclusion criteria. Patients were discharged either to home mechanical ventilation, or after weaning, to other chronic care departments or home. Some were transferred to ACH for treatment due to acute deterioration.
Study Design
All data were retrospectively obtained from the electronic health records (EHR) of 308 adults aged ≥40 years at admission to LTACH, requiring PMV hospitalized in LTACH between 01/01/2015 to 06/30/2019 and followed-up until discharge or death or until 12/31/2019. Patients who were admitted to LTACH before 1.1.2015 were included in the analysis. They were divided into three age groups by age at admission to LTACH: 40 to 59 (n = 36), 60 to 79 (n = 146) and 80 and older (n = 126). Successful weaning was defined as two weeks free of mechanical ventilator support. This study was limited to adult PMV patients aged 40 and above at time of admission to LTACH. Young adults and pediatric PMV patients were excluded because of their unique clinical background.
Variables
Physical, neurological, and cognitive function were retrieved at three time points: 1. prior to the acute event leading to initiation of mechanical ventilation (at any of community/home, nursing home/closed psychiatric ward and geriatric hospital/long-term ward in acute care hospital) 2. at admission to LTACH, and 3. at the end of follow-up/at discharge or one week before death in case of in-LTACH death. Data from period one were retrieved from EHR at ACH and LTACH, and data from periods two and three were retrieved from the EHR of the multi-disciplinary team at LTACH. The Katz Index of Independence in Activities of Daily Living (ADL-Katz score) was calculated with a score ranging from 0 (dependent on help of others in feeding, continence, transferring, toileting, dressing and bathing) to 6 (fully independent in each). Feeding route at the same three time points was documented. Neurological function was measured and determined by categories. The categories included vegetative state/minimally conscious state (VS/MCS), which was diagnosed using the Revised JFK-Coma Recovery Scale;14 severe cognitive impairment (SCI) was defined as the Global Deterioration Scale/Functional Assessment Staging (GDS/FAST)15 stages six and seven; and mild/moderate cognitive impairment according to GDS/FAST stages three to five; or no cognitive impairment, or intellectual disability/psychiatric disorder according to the diagnosis on admission. A multi-disciplinary team performed the evaluation on admission and at frequent intervals. For each patient, we retrieved the number of transfers to the ER (defined as the number of times the patient was transferred to the ER during LTACH hospitalization) and the number of admissions to ACH (defined as the number of times the patient was transferred to the ER and remained more than 48 hours at the ACH during LTACH hospitalization). The other clinical variables retrieved are detailed in the supplemental file.
Weaning Methodology and Outcomes
Weaning is performed by a multi-disciplinary team including physicians, nurses and respiratory therapists with incremental lengths of disconnection time, when deemed suitable. We defined the status of ventilation upon admission to LTACH and a weaning outcome at the end of follow-up/at discharge from LTACH, which we divided into each of five categories: full ventilation (24h), up to 4h daily disconnection from mechanical ventilation, 5 to 16h daily disconnection from ventilation, overnight (nocturnal) ventilation, and weaned (entirely free from mechanical ventilation for two weeks or more).
Clinical Outcomes
The main clinical outcomes were recorded at the end of follow up or at discharge and included: length of stay (LOS) at LTACH and length of ventilation (LOV) from initiation of mechanical ventilation until discharge/end of follow-up, place of discharge, in-LTACH mortality, ADL-Katz score, daily ventilation time, feeding route, and consciousness and cognitive state.
Ethics Approval
The study was approved by the institutional ethics committee, which waived participants’ or family informed consent, authorization number: 340-19.
Statistical Analysis
Normally distributed quantitative variables were expressed as means, together with standard deviations, whereas non-normally distributed quantitative variables were expressed as medians, together with interquartile ranges. Categorical variables were expressed as frequencies and percentages. In order to test the association between two categorical variables, the Chi-square test as well as the Fisher's exact test were used. The comparison of quantitative variables between two independent groups was carried out using the Mann-Whitney non-parametric test. The comparison of quantitative variables between three or more independent groups was carried out using either the ANOVA test or the Kruskal-Wallis non-parametric test. Non-parametric tests were used for non-normally distributed variables. The McNemar-Bowker test was used to compare the symmetry of change of consciousness and cognitive state (improvement vs. worsening) at two time points. The Kaplan-Meier survival analysis with the log-rank test for the comparison of survival curves was used for assessing the effect of categorical variables on survival (LOS at LTACH). The Cox-regression model was used as the multivariate model to assess simultaneously the effect of independent predictors on in-LTACH mortality. This model was performed using the forward step-wise likelihood ratio approach. All analyses used SPSS version 25.0 (SPSS Inc., Chicago, IL). P ≤ .05 (two-tailed) was considered statistically significant.
Results
Demographic and Clinical Variables
The proportion of patients residing in a nursing home/psychiatric ward before initiation of mechanical ventilation increased with age, while those residing in geriatric hospitals/long-term acute ward in an ACH before initiation of mechanical ventilation decreased with age. Place of intubation, while not statistically significant (p = .08), showed a distinct pattern. The younger age group had a 50% greater risk to be intubated either at home or in the ER than the older age groups, who were more prone to intensive care unit (ICU) and at-ward intubation. ICU admission during acute hospital stay decreased significantly with increasing age, from 61.1% among the youngest age group to 25.4% at ≥ 80 (p < .001) (Table 1). The main reason for ventilation was pneumonia/ other acute pulmonary condition for 29.9% of patients, post-cardiopulmonary resuscitation/ anoxic brain damage for 26.6%, exacerbation or end stage chronic lung disease for 10.1%, acute neurological event for 9.1%. There was no statistically significant difference in the main reasons for ventilation between age groups (p = .486) (Supplemental Table 1).
Table 1.
Demographic and Clinical Characteristics of Prolonged Mechanically Ventilated Subjects by Age Groups.
| Characteristic | Total (n = 308) | 40-59 (n = 36) | 60-79 (n = 146) | ≥ 80 (n = 126) | P* |
|---|---|---|---|---|---|
| Age(y) mean ± SD | 75.3 ± 12.5 | 52.1 ± 4.9 | 70.9 ± 5.6 | 87.1 ± 5.1 | |
| Female, n (%) | 156 (50.6) | 10 (27.8) | 65 (44.5) | 81 (64.3) | <.001 |
| Ethnic/Religious Background, n (%) | <.001 | ||||
| Jewish | 253 (82.1) | 21 (58.3) | 120 (82.2) | 112 (88.9) | |
| Other | 55 (17.9) | 15 (41.7) | 26 (17.8) | 14 (11.1) | |
| Marital status, n (%) | <.001 | ||||
| Married/Partner | 158 (51.5) | 16 (44.4) | 95 (65.1) | 47 (37.6) | |
| Divorced | 15 (4.9) | 5 (13.9) | 9 (6.2) | 1 (0.8) | |
| Widowed | 105 (34.2) | 1 (2.8) | 30 (20.5) | 74 (59.2) | |
| Single | 29 (9.4) | 14 (38.9) | 12 (8.2) | 3 (2.4) | |
| Offspring, mean ± SD | 4.4 ± 3.4 | 2.4 ± 2.5 | 4.4 ± 3.4 | 5.1 ± 3.3 | <.001 |
| Residence before AHS, n (%) | .13 | ||||
| Community/Home | 243 (78.9) | 28 (77.8) | 119 (81.5) | 96 (76.2) | |
| Nursing home/Psychiatric Ward | 31 (10.1) | 2 (5.6) | 10 (6.8) | 19 (15.1) | |
| Geriatric Hospital/LWAH | 34 (11.0) | 6 (16.7) | 17 (11.6) | 11 (8.7) | |
| Place of Intubation, n (%) | .08 | ||||
| Community-Based Institutions | 13 (4.2) | 1 (2.8) | 3 (2.1) | 9 (7.1) | |
| Home | 66 (21.4) | 11 (30.6) | 28 (19.2) | 27 (21.4) | |
| ER | 71 (23.1) | 13 (36.1) | 31 (21.2) | 27 (21.4) | |
| ICU/OR | 34 (11.0) | 1 (2.8) | 19 (13.0) | 14 (11.1) | |
| Ward | 124 (40.3) | 10 (27.8) | 65 (44.5) | 49 (38.9) | |
| ICU Admission during AHS, n (%) | 119 (38.8) | 22 (61.1) | 65 (44.8) | 32 (25.4) | <.001 |
AHS = acute hospital stay; ER = emergency room; ICU = intensive care unit; LWAH = long-term ward in acute hospital; OR = operating room.
* P values refer to differences between the three age groups.
Physical, Neurological and Weaning Outcomes
LOS in LTACH decreased with age, with the oldest presenting less than half of the youngest cohort LOS (Table 2). Range of LOS and LOV was wide, at a maximum of almost 16 years (189.6 months) for the youngest group and ten years for the two other age groups. Physical function, as assessed by the ADL-Katz scores prior to the event, had a median of 4.5 and 4 in the two younger age groups versus 2 at age ≥ 80. However, at admission to LTACH and at the end of follow up/discharge, the ADL-Katz scale had a median of 0 among all age cohorts. With increasing age, in-LTACH death rose, while the number of transfers to the ER and the number of admissions to ACH during LTACH hospitalization decreased. Interestingly, the same proportion of patients, about 5% among all age groups, were discharged to their home. Discharge to rehabilitation departments decreased with age. Feeding route prior to acute event was mostly per os (PO), at around 90% in all age cohorts (p = .87), and greatly decreased on admission to LTACH, but increased slightly at the end of follow-up/discharge, 19.4% and 21.9% among the two younger age groups respectively, and 13.5%, at the age ≥ 80 group (p = .18) (Table 2).
Table 2.
General Outcomes of Prolonged Mechanically Ventilated Subjects by Age Groups.
| Characteristic | Total (n = 308) | 40-59 (n = 36) | 60-79 (n = 146) | ≥80 (n = 126) | P* |
|---|---|---|---|---|---|
| Length of stay (months), mean ± SD, (range) | 19.0 ± 25.1 (0.0-189.6) | 34.6 ± 42.6 (0.7-189.6) | 19.1 ± 22.3 (0.0-117.5) | 14.4 ± 19.3 (0.1-126.3) | .006 |
| Length of ventilation (months), mean ± SD, (range) | 21.8 ± 25.6 (1.0-191.1) | 37.0 ± 42.2 (2.1-191.1) | 22.1 ± 23.4 (1.0-119.5) | 17.1 ± 19.6 (1.4-128.2) | .007 |
| ADL-Katz, median (IQR) | |||||
| Prior to the event | 3 (0-6) | 4.5 (0-6) | 4 (0-6) | 2 (0-5) | .002 |
| At admission to LTACH | 0 (0-0) | 0 (0-0) | 0 (0-0) | 0 (0-0) | .075 |
| At the end of follow-up | 0 (0-0) | 0 (0-0) | 0 (0-0) | 0 (0-0) | .23 |
| Feeding route - prior to event, n (%) | .87 | ||||
| Oral feeding | 275 (89.3) | 33 (91.7) | 131 (89.7) | 111 (88.1) | |
| Nasogastric/PEG | 33 (10.7) | 3 (8.3) | 15 (10.3) | 15 (11.9) | |
| Feeding route- at admission to LTACH, n (%) | .025 | ||||
| Oral feeding | 26 (8.4) | 1 (2.8) | 19 (13.0) | 6 (4.8) | |
| Nasogastric/PEG | 282 (91.6) | 35 (97.2) | 127 (87.0) | 120 (95.2) | |
| Feeding route- at the end of follow up, n (%) | .18 | ||||
| Oral feeding | 56 (18.2) | 7 (19.4) | 32 (21.9) | 17 (13.5) | |
| Nasogastric/PEG | 252 (81.8) | 29 (80.6) | 114 (78.1) | 109 (86.5) | |
| Place of discharge, n (%) | .12 | ||||
| Dead | 140 (45.5) | 11 (30.6) | 60 (41.1) | 69 (54.8) | |
| Home | 17 (5.5) | 2 (5.6) | 9 (6.2) | 6 (4.8) | |
| Alive at ventilation ward | 78 (25.3) | 11 (30.6) | 43 (29.5) | 24 (19.0) | |
| Acute hospital | 66 (21.4) | 10 (27.8) | 31 (21.2) | 25 (19.8) | |
| Complex nursing care | 4 (1.3) | 1 (2.8) | 1 (0.7) | 2 (1.6) | |
| Rehabilitation | 3 (1.0) | 1 (2.8) | 2 (1.4) | 0 (0) | |
| Number of transfers to ER, mean ± SD | 1.2 ± 2.4 | 2.5 ± 5.6 | 1.2 ± 1.6 | 0.8 ± 1.1 | .09 |
| Number of admissions to ACH, mean ± SD | 0.8 ± 1.4 | 1.4 ± 2.8 | 0.8 ± 1.3 | 0.6 ± 0.9 | .33 |
ACH = acute care hospital; ADL = activities of daily living; ER = emergency room; LTACH = long term acute care hospital; PEG = percutaneous endoscopic gastrostomy; SD = standard deviation.
* P values refer to differences between age groups.
Prior to the event leading to ACH admission, the severity and prevalence of cognitive impairment increased with age. At admission to LTACH, 52.8% of the younger cohort suffered from VS/MCS, and 54.8% of those 80 years or older had severe cognitive impairment (SCI). Of note, among VS/MCS patients at admission to LTACH, 80.8% were ventilated due to anoxic brain damage, 14.6% due to an acute neurological event, 3.8% due to a traumatic brain injury, and 0.8% due to end-stage neuromuscular disease. The prevalence of SCI was higher in the oldest age group than in the younger groups. These findings are similar to those seen at the end of follow-up/discharge from LTACH (Supplemental Table 2).
At admission to LTACH, 91.7% of the younger age cohorts were undergoing full, 24h daily ventilation compared to 96.8% of those aged 80 years and above. The rest were ventilated either from eight to 23 hours daily or only overnight (p = .21), (Supplemental Table 3). At the end of follow-up/at discharge, more patients in the older age group were fully ventilated, while nocturnal ventilation or weaning were more often seen in the younger age groups (p = .02). In addition, the mean age (±SD) of those weaned from ventilation at the end of follow-up was 69.0 ± 13.8 years, and those still ventilated was 75.9 ± 12.4 (p = .055). LOS and LOV in months were (mean ± SD) 6.0 ± 4.8 and 6.5 ± 4.4 respectively for those weaned at the end of follow-up and 19.3 ± 24.9 and 22.2 ± 25.4 for those still ventilated at LTACH at the end of follow-up (p = .062 and p = .005 for LOS and LOV respectively). LOV was longer than LOS in the LTACH since initiation of mechanical ventilation was either just before admission to ACH or during hospitalization at the ACH (Table 1).
Predictors for Survival in LTACH and Mortality in LTACH
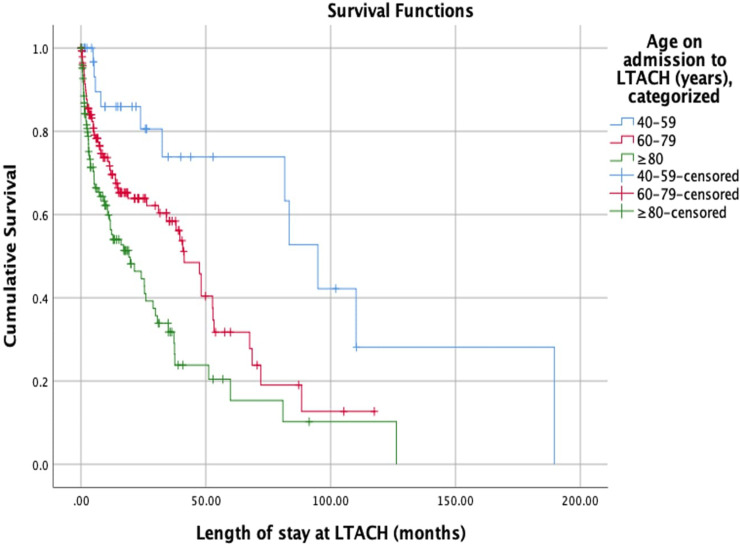
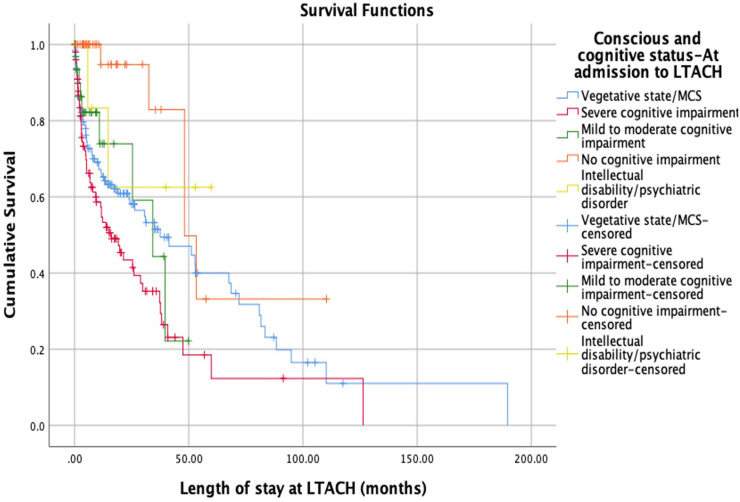
In-LTACH survival according to age groups at admission of the 308 patients with PMV decreased with older age (Figure 1 and Table 2). In LTACH, the highest LOS was for patients in a vegetative state, followed by those without cognitive impairment (p = .02). The highest in-LTACH mortality rate was for those with SCI and VS/MCS, in a decreasing order (p <.001) (Figure 2 and Table 3). (In LTACH, the patients with intellectual disability/mental disorders had a mean survival of 30.1 ± 23.8 months. However, there were only six patients in this group).
Figure 1.
Kaplan-Meir estimate of survival at LTACH of 308 patients undergoing prolonged mechanical ventilation according to age group at admission to LTACH. LTACH – Long-Term Care Acute Hospital.
Figure 2.
Kaplan-Meir estimate of survival at LTACH of 308 patients undergoing prolonged mechanical ventilation according to consciousness and cognitive state at admission to LTACH. LTACH – Long-Term Care Acute Hospital.
Table 3.
Association Between Consciousness and Cognitive State at Admission to LTACH and Age on Admission to LTACH, LOV, LOS, Number of Transfers to ER and Admissions to ACH.
| Consciousness and Cognitive State- at Admission to LTACH | Age on Admission to LTACH Mean ± SD | In-LTACH mortality, n (%) | LOV months ± SD, (range) | LOS at LTACH months ± SD, (range) | Number of Transfers to ER Mean ± SD | Number of Admissions to ACH Mean ± SD |
|---|---|---|---|---|---|---|
| VS/MCS (n = 130) | 72.9 ± 12.6 | 66 (50.8) | 26.2 ± 30.8 (1.0-191.1) | 23.8 ± 30.7 (0.1-189.6) | 1.1 ± 3.1 | 0.6 ± 1.6 |
| SCI (n = 100) | 83.1 ± 9.5 | 58 (58.0) | 17.7 ± 20.0 (1.5-128.2) | 15.1 ± 19.5 (0.4-126.4) | 1.0 ± 1.2 | 0.7 ± 1.0 |
| Mild/Moderate Cognitive Impairment (n = 34) | 76.6 ± 9.1 | 9 (26.5) | 14.5 ± 15.3 (1.5-61.5) | 10.0 ± 12.8 (0.2-49.9) | 1.7 ± 1.6 | 1.1 ± 1.1 |
| No Cognitive Impairment (n = 38) | 66.5 ± 10.2 | 5 (13.2) | 22.2 ± 24.3 (1.5-111.1) | 18.9 ± 21.9 (0-110.4) | 1.6 ± 1.8 | 0.9 ± 1.5 |
| Intellectual Disability/Psychiatric Disorder (n = 6) | 59.8 ± 13.8 | 2 (33.3) | 32.6 ± 23.8 (7.5-61.8) | 30.1 ± 23.8 (5.8-59.8) | 3.8 ± 3.7 | 2.7 ± 3.0 |
| P | < .001 | < .001 | .09 | .02 | < .001 | < .001 |
ACH = acute care hospital; ER = emergency room; LOS = length of stay; LOV = length of ventilation; LTACH = long-term acute care hospital; SCI = severe cognitive impairment; SD = standard deviation; VS/MCS = vegetative state/minimally conscious state.
The cox regression multivariable model for mortality was performed for 303 patients, using the forward stepwise likelihood ratio method (Table 4). Data was incomplete for five patients, so they were excluded from this analysis. Using the univariate model, nine variables were associated with mortality. Consequently, these nine variables were entered for the multivariable model, from which only four variables remained statistically significant. The statistically significant variables were age ≥ 80 at admission to LTACH, non-neurological event as the main reason for ventilation, chronic condition: diabetes mellitus, and number of transfers to ER. First, the oldest cohort had three times the risk of death than the youngest (adjusted hazard ratio (HR) for oldest cohort compared to youngest = 2.97, 95% CI = 1.49-5.92, p = .002). Diabetes mellitus was the only statistically significant chronic condition associated with in LTACH mortality in the univariate or multivariate model. Of note, the middle-aged cohort was not statistically significantly associated with increased mortality compared to the youngest cohort (adjusted HR for the middle cohort compared to youngest = 1.74, 95% CI = 0.87-3.46, p = .12). For each additional transfer to the ER during LTACH hospitalization, the likelihood of dying in LTACH was reduced by a factor of 0.69 (95% CI = 0.58-0.83, p < .001).
Table 4.
Logistic Regression Analysis for the Likelihood of Dying in-LTACH among 303 Adult Subjects.
| Variables | B | Adjusted HR (95% CI) | P |
|---|---|---|---|
| Age(y) groups on Admission to LTACH | |||
| 40-59 | |||
| 60-79 | 0.552 | 1.74 (0.87-3.46) | .12 |
| ≥ 80 | 1.090 | 2.97 (1.49-5.92) | .002 |
| Not having acute neurological event as main reason for ventilation* | 0.997 | 2.71 (1.30-5.65) | .008 |
| Chronic Condition: DM | 0.414 | 1.51 (1.07-2.13) | .02 |
| Number of Transfers to ER | -0.369 | 0.69 (0.58-0.83) | .001 |
DM = diabetes mellitus; ER = emergency room; HR = hazard ratio; LTACH = long-term acute care hospital.
*Acute neurological event: ischemic stroke, intracerebral hemorrhage, epileptic seizure.
Association of Consciousness and Cognitive State at Admission to LTACH with Age, Main Reasons for Ventilation, in-LTACH Mortality, LOV, LOS, Number of Transfers to ER and Consciousness and Cognitive State at the End of Follow-Up
Patients with VS/MCS were younger and their in-LTACH mortality was lower than patients with SCI. Patients with SCI were the oldest and had shorter LOS and LOV. Their in-LTACH mortality rate was the highest among all consciousness and cognitive states, more than four times higher than those with no cognitive impairment (p < .001) (Table 3). In terms of the main reasons leading to ventilation, 45.4% of VS/MCS patients were ventilated due to anoxic brain damage/ post-cardiopulmonary resuscitation in comparison to 16.0% of SCI patients. Among SCI patients, 44.0% were ventilated following pneumonia/ other acute pulmonary condition in comparison to 18.5% of VS/MCS and 29.4% of patients with mild to moderate cognitive impairment. As a whole, patients ventilated post-operatively or due to acute/ progressive neuromuscular condition presented less cognitive impairment (p < .001) (Supplemental Table 4).
Patients in VS/MCS and SCI were transferred less frequently to the ER and were less likely to be admitted to the ACH during LTACH hospitalization than those with mild to moderate cognitive impairment or with no cognitive impairment (Table 3).
In terms of the association between consciousness and cognitive state at admission to LTACH and weaning at the end of follow-up, the lower the consciousness/cognitive state, the higher the risk of remaining ventilated at the end of follow-up. Although only 14 out of 306 patients (two were excluded due to incomplete data) were weaned at the end of follow-up, the vast majority of them had no cognitive impairment or only mild to moderate cognitive impairment, and the rest SCI (p < .001). Of note, only one patient in VS/MCS at admission to LTACH was weaned at the end of follow-up (Supplemental Table 5).
Among 168 PMV patients who did not die at LTACH, a third of the patients with mild to moderate or no cognitive impairment at the end of follow-up were discharged either to their home or to nursing care/rehabilitation. Only 9.6% of SCI patients were discharged to their home, and all of the VS/MCS either stayed at LTACH or were transferred to ACH (p < .001) (Supplemental Table 6).
Among 130 VS/MCS patients at admission to LTACH, 84 had no cognitive impairment prior to the event leading to intubation. Among 100 patients with SCI at admission, 80 had cognitive impairment prior to the event. Of note, 23.1% of all patients admitted to LTACH presented SCI before the event leading to intubation (Supplemental Table 7).
Among 130 patients in VS/MCS at admission, nine had SCI and one patient improved to mild/moderate cognitive impairment at the end of follow-up. Among 100 patients with SCI at admission, three were in VS/MCS, and five improved to mild/moderate cognitive impairment at the end of the follow-up. The vast majority of patients presented no change in their consciousness and cognitive state at the end of follow-up. There was no significant difference in the McNemar-Bowker test of symmetry between cognitive state improvement and worsening (p = .395) (Supplemental Table 8).
Discussion
In this study, we found that among patients with prolonged mechanical ventilation, age was significantly associated with unfavorable cognitive and weaning outcomes and in-LTACH survival. While in-LTACH mortality was at a high 45.5% during the study period, only a small proportion of the patients of all ages were discharged to their home, to rehabilitation departments, or to departments of complex nursing care. Others remained at LTACH or were referred to ER in ACHs.
Because inclusion criteria were hospitalization between 01/01/2015 and 6/30/2019, patients admitted years before were included in the analysis, hence the wide LOS and LOV range at a maximum of 16 years for both. On the other hand, there was an underestimation of LOS because the follow up period at the end of the patient recruitment was only six months. The mean LOS at LTACH was highest for VS/MCS patients at admission and for those with no cognitive impairment. One possible explanation is that the cognitive and usually the physical state prior to the event leading to the PMV initiation of patients with VS/MCS was vastly better than for patients with severe cognitive impairment at admission. This suggests that patients with SCI had more comorbidity and may have received less optimal treatment at the outpatient setting before the event than the former. Another explanation, which derives from the previous one, is that some VS/MCS patients can survive with adequate medical and nursing care for more than a decade hence skewing LOS and LOV toward higher values.
Of 130 patients presenting with VS/MCS at admission to LTACH, at the end of follow-up 120 were in VS/MCS, with nine presenting SCI and only one improving to mild to moderate cognitive impairment. The latter was the only patient being fed PO at the end of follow-up among those patients. This reflects the “natural history” of patients in VS/MCS in a setting where terminal weaning is not feasible. The main etiology of the VS/MCS in this study was non-traumatic, which has been shown to have a worse prognosis in terms of survival and neurological recovery according to many longitudinal studies.16,17 Our study included only ventilated patients who may have had a worse prognosis and more severe brain injury than non-ventilated patients. However, other studies such as the study by Estraneo et al18 did not demonstrate the association between etiology and prognosis in patients with VS/MCS.18,19
Among the 100 SCI patients at admission to LTACH, the condition of three worsened to VS/MCS, and the cognitive impairment of five improved to mild to moderate levels. The rest remained with SCI. The proportion of SCI patients remaining in the same cognitive state was expected due to their GDS/FAST scores of 6-7 at admission and the natural history of advanced dementia.20 Of note, 71 patients were in SCI before initiation of mechanical ventilation.
Daily ventilation time was mostly full (24h/day) at admission to LTACH among all age groups. At the end of follow-up, only a handful of patients aged 80 years and above were either weaned or on nocturnal ventilation compared to almost a quarter of the youngest age group. It is important to note that the unit admits PMV patients without taking into consideration either the potential for weaning or their prognosis.
In the Frengley et al11 study about weaning outcomes among PMV patients according to age, the likelihood of being weaned decreased from 36% for the cohort ages 65-69 years to 7% in the ≥90 year cohort (p = .002). The underlying diagnoses leading to PMV support in Frengley's study were similar to those in the current study, except that none of their patients had VS/MCS or a record of dementia. They reported that 63% of patients died at LTACH and that only 4% of patients were discharged home and 9% to nursing homes compared to 5.5% and 1.3% in the current study. In their multivariate model, age was not a significant factor in predicting outcomes. In contrast, in our study, the 80 years and above cohort was independently associated with in-LTACH mortality. In a meta analysis, Damuth et al6 described the survival of PMV patients at ACH and LTACH in the United States versus internationally. The pooled mortality at time-points between two and four years was 69% (95%CI 63%-74%) in studies in acute care hospital ICUs, 56% (95%CI 45%-66%) in acute care hospital weaning units, and 64% (95%CI 52%-74%) in post-acute care hospitals. The rate of weaning from ventilation at one year in post-acute care hospitals was 47% (95%CI 42%-51%) in the United States versus 63% (95%CI 59%-68%) internationally. However, it is important to keep in mind that the LTACH studies included in the meta-analysis comprised patient pools with a different distribution of underlying diagnoses for PMV than in the current study. For example, Modawal et al21 reported outcomes of PMV patients in a rehabilitation unit. After a two-year follow-up, they achieved 50.3% weaning from ventilation. However, theirs was a rehabilitation facility with no mention of dementia or prolonged disorders of consciousness as a result of brain anoxic damage.
Greater cognitive impairment was associated with older age and fewer transfers to ER during hospitalization in LTACH. In the cox regression multivariable model, an increased number of transfers to ER was associated with decreased mortality, at an adjusted HR of 0.69. This may be due to practitioner bias of selecting patients with supposedly more treatable and reversible conditions who are sent to the ER for further treatment. This is in line with considerations of “medical futility”, whereby older patients with unfavorable prognoses are treated conservatively, therefore decreasing the potential number of referrals to ACH.
However, in Israel, cultural perceptions of the “sanctity of life” among traditional segments of Israeli society result in a percentage of patients with severe cognitive impairment being referred to ACH regardless of the patient's age, physical/cognitive state, or quality of life, and subsequently are ventilated. In the current study, almost a quarter of patients admitted to LTACH presented severe cognitive impairment and a handful were in VS/MCS prior to the event leading to intubation.
In Israel, the sociocultural, religious, and legal setting may be a factor in the described outcomes. Many patients with severe cognitive impairment are intubated, and due to the 2005 Patient Dying Act,12 it is illegal to hasten death actively, eg, in the form of withdrawing ventilation. In order to prevent the current situation, the Israeli public can file advance directives and ask for “Do-not-resuscitate” (DNR)/ “Do-not-intubate” (DNI) status, among others in certain situations. However, administrative encumbrance and inefficiency may prevent these directives from being signed or activated. As of early 2020, of 6.6 million adults aged 15 years and above,22 only about 19,500 people nationally had filed these directives with the Central Data Bank of Preliminary Medical Directives, (data bequeathed by a request to the Israeli Ministry of Health; request number: 631809). In the study of Jacobs et al,23 of 120 PMV patients, some were ventilated at home and others in the LTACH of this current study, 119 (99.2%) did not have advance directives.
This situation results in many patients being ventilated indefinitely in Israeli LTACHs, without knowing what their end-of-life preferences would have been. In a study of Sviri et al,24 relatives of PMV patients were more likely to request invasive procedures for their relatives, than for themselves. Specifically, if it were legally possible, half of them would have requested withdrawal of ventilation for themselves, if deemed unconscious with a minimal chance of recovery, while none would make such a request on behalf of their ventilated relatives. As a whole, the increase in the PMV patient population has wide economic and social repercussions for their immediate family and for the health system. In a Canadian study by Dale et al25 about support needs and health-related quality of life of family caregivers of patients requiring PMV, stress-related health changes experienced by family caregivers included alterations in eating habits, body weight, quantity and quality of sleep, and energy levels that persist well beyond the ICU and LTACH stay.
Of note, a minority of medically stable PMV patients with more favorable cognitive and physical conditions can be redirected to home ventilation. Jacobs et al26 compared home-ventilated patients with those ventilated in the LTACH of this current study. They found that patients ventilated at home were, on the average, younger, had less comorbidity, were more likely to be alert and able to communicate, and were ventilated for a longer period of time.26 The cost to the HMO was a third that of LTACH, with lower depression rates among patients. However, the patients ventilated at home were put on a ventilator mainly for degenerative neuromuscular diseases or chronic lung disease, whereas LTACH patients suffered more from acute neurological or medical changes. In that study PMV patients reported few severe distressing symptoms and 85% would have chosen ventilation if asked again.23 This is consistent with a 2019 study from Jubran et al,27 whereby six months after discharge, improvement in muscle function enabled patients to perform daily activities, and 84.7% indicated willingness to undergo mechanical ventilation again.
Significantly, in the face of prognostic uncertainties, especially in a multicultural setting, physicians are able to choose (or to discourage) life-prolonging therapies. Data on patients in 22 European ICUs in 2015-2016, who received limited treatment or who died, were compared with data reported from the same ICUs in 1999-2000.28 Limiting the use of life-prolonging therapies occurred significantly more frequently, in 2015-2016. Compared to countries in northern Europe and central Europe, Israel had the longest median length of stay in ICU and the longest median time from ICU admission until the first limitation of life-sustaining therapy.28 The results of this current study are relevant in countries where, for cultural reasons, terminal weaning is not accepted because of the belief in the sanctity of life or the strong hope for improvement in the patient's condition. From another perspective, it is important to learn the natural history and prognosis of PMV patients from a wide range of etiologies in order to assist family members, health professionals, and health policy-makers in decision-making.
This study sheds light on the natural course of disease of a PMV population by a multi-disciplinary team with regular and frequent structured assessments of cognitive and physical functions and care, in a setting where law does not permit terminal weaning. The strength of this study is in our use of validated tools such as the JFK Revised Coma Recovery Scale, for diagnosis of VS/MCS as recommended by professional guidelines,29,30 and the GDS/FAST scale for assessment of the level of cognitive impairment. Furthermore, the underlying diagnoses for PMV in a large proportion of patients are different from what other centers have reported and published.
Limitations
This is a single-center study of PMV patients in a LTACH setting in a country where terminal weaning is not feasible. Therefore, our results may have limited generalizability to some countries where this practice is more common. No data was available on patients discharged or transferred from the LTACH. There is an underestimation of LOS at LTACH because the follow up after the end of the patient recruitment for the study was only six months long. In addition, only adult PMV patients aged 40 years and above at time of admission to LTACH were included in this study. Young adults and pediatric PMV patients were excluded because of their unique clinical background. Nutritional status and comorbidity score were not accounted for in this analysis.
Conclusions
This study shows the outcomes of PMV patients in a country where terminal weaning of mechanical ventilation is not implemented in clinical practice. In-LTACH mortality was associated with increasing age and worsening consciousness and cognitive state. Age was associated with worsening physical, neurological and weaning outcomes. Longer stay in LTACH and lack of neurological improvement in patients in a vegetative state or with severe cognitive impairment, places a long-term physical and emotional burden on caregivers, poses a significant cost to society, and raises clinical and ethical questions. In this study, many patients with severe cognitive impairment before the event were subsequently ventilated, an intervention that might have prolonged their suffering. There is a need for discussion regarding end-of-life decisions from the initial decision to resuscitate/intubate patients to the long-term management of these patients.
Supplemental Material
Supplemental material, sj-pdf-1-jic-10.1177_08850666221088800 for Prognosis of Chronically Ventilated Patients in a Long-Term Ventilation Facility: Association with Age, Consciousness and Cognitive State by David Stein, Sigal Sviri, Michael Beil, Ilana Stav and Esther-Lee Marcus in Journal of Intensive Care Medicine
Supplemental material, sj-docx-1-jic-10.1177_08850666221088800 for Prognosis of Chronically Ventilated Patients in a Long-Term Ventilation Facility: Association with Age, Consciousness and Cognitive State by David Stein, Sigal Sviri, Michael Beil, Ilana Stav and Esther-Lee Marcus in Journal of Intensive Care Medicine
Supplemental material, sj-docx-2-jic-10.1177_08850666221088800 for Prognosis of Chronically Ventilated Patients in a Long-Term Ventilation Facility: Association with Age, Consciousness and Cognitive State by David Stein, Sigal Sviri, Michael Beil, Ilana Stav and Esther-Lee Marcus in Journal of Intensive Care Medicine
Acknowledgments
The authors thank Tali Bdolah-Abram, statistician, Faculty of Medicine, Hebrew University of Jerusalem, Israel, for her statistical support.
Footnotes
Author Contributions: DS, SS, and E-LM contributed to literature search. DS and IS performed data collection. DS, SS, E-LM, IS, and MB contributed to analysis and interpretation of data. DS drafted the manuscript. SS, E-LM, MB, and IS revised the manuscript. All authors read and approved the final manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: The study was approved by the institutional ethics committee, which waived participants’ or family informed consent, authorization number: 340-19.
ORCID iD: David Stein https://orcid.org/0000-0001-8708-876X
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Windisch W, Dellweg D, Geiseler Jet al. et al. Prolonged weaning from mechanical ventilation: results from specialized weaning centers—a registry-based study from the WeanNet Initiative. Dtsch Arztebl Int. 2020;117(12):197-204. doi: 10.3238/arztebl.2020.0197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Girard K, Raffin TA. The chronically critically ill: to save or let die? Respir Care. 1985;30(5):339-347. [PubMed] [Google Scholar]
- 3.Nelson JE, Cox CE, Hope AA, Carson SS. Chronic critical illness. Am J Respir Crit Care Med. 2010;182(4):446-454. doi: 10.1164/rccm.201002-0210CI [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lamas D. Chronic critical illness. N Engl J Med. 2014;370(2):175-177. doi: 10.1056/NEJMms1310675 [DOI] [PubMed] [Google Scholar]
- 5.MacIntyre NR, Epstein SK, Carson S, Scheinhorn D, Christopher K, Muldoon S. National Association for Medical Direction of Respiratory Care. Management of patients requiring prolonged mechanical ventilation: report of a NAMDRC consensus conference. Chest. 2005;128(6):3937-3954. doi: 10.1378/chest.128.6.3937 [DOI] [PubMed] [Google Scholar]
- 6.Damuth E, Mitchell JA, Bartock JL, Roberts BW, Trzeciak S. Long-term survival of critically ill patients treated with prolonged mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med. 2015;3(7):544-553. doi: 10.1016/S2213-2600(15)00150-2 [DOI] [PubMed] [Google Scholar]
- 7.Chelluri L, Im KA, Belle SHet al. Long-term mortality and quality of life after prolonged mechanical ventilation. Crit Care Med. 2004;32(1):61-69. doi: 10.1097/01.CCM.0000098029.65347.F9 [DOI] [PubMed] [Google Scholar]
- 8.Kahn JM, Le T, Angus DCet al. et al. The epidemiology of chronic critical illness in the United States. Crit Care Med. 2015;43(2):282-287. doi: 10.1097/CCM.0000000000000710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seneff MG, Wagner D, Thompson D, Honeycutt C, Silver MR. The impact of long-term acute-care facilities on the outcome and cost of care for patients undergoing prolonged mechanical ventilation. Crit Care Med. 2000;28(2):342-350. doi: 10.1097/00003246-200002000-00009 [DOI] [PubMed] [Google Scholar]
- 10.Dettmer MR, Damuth E, Zarbiv S, Mitchell JA, Bartock JL, Trzeciak S. Prognostic factors for long-term mortality in critically ill patients treated with prolonged mechanical ventilation: a systematic review. Crit Care Med. 2017;45(1):69-74. doi: 10.1097/CCM.0000000000002022 [DOI] [PubMed] [Google Scholar]
- 11.Frengley JD, Sansone GR, Shakya K, Kaner RJ. Prolonged mechanical ventilation in 540 seriously ill patients aged 65 years and older: effects of increasing age on clinical outcomes and survival. J Am Geriatr Soc. 2014;62(1):1-9. doi: 10.1111/jgs.12597 [DOI] [PubMed] [Google Scholar]
- 12.Schönhofer B, Euteneuer S, Nava S, Suchi S, Köhler D. Survival of mechanically ventilated patients admitted to a specialised weaning centre. Intensive Care Med. 2002;28(7):908-916. doi: 10.1007/s00134-002-1287-5 [DOI] [PubMed] [Google Scholar]
- 13.Steinberg A, Sprung CL. The dying patient act, 2005: Israeli innovative legislation. Isr Med Assoc J. 2007;9(7):550-552.17710789 [PubMed] [Google Scholar]
- 14.Giacino JT, Kalmar K, Whyte J. The JFK Coma Recovery Scale-Revised: measurement characteristics and diagnostic utility. Arch Phys Med Rehabil. 2004;85(12):2020-2029. doi: 10.1016/j.apmr.2004.02.033 [DOI] [PubMed] [Google Scholar]
- 15.Auer S, Reisberg B. The GDS/FAST staging system. Int Psychogeriatr. 1997;9(Suppl 1):167-171. doi: 10.1017/S1041610297004869 [DOI] [PubMed] [Google Scholar]
- 16.Whyte J, Gosseries O, Chervoneva Iet al. Predictors of short-term outcome in brain-injured patients with disorders of consciousness. Prog Brain Res. 2009;177:63-72. doi: 10.1016/S0079-6123(09)17706-3 [DOI] [PubMed] [Google Scholar]
- 17.Nekrasova J, Kanarskii M, Borisov Iet al. One-year demographical and clinical indices of patients with chronic disorders of consciousness. Brain Sci. 2021;11(5):651. doi: 10.3390/brainsci11050651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Estraneo A, De Bellis F, Masotta Oet al. et al. Demographical and clinical indices for long-term evolution of patients in vegetative or in minimally conscious state. Brain Inj. 2019;33(13-14):1633-1639. doi: 10.1080/02699052.2019.1658220 [DOI] [PubMed] [Google Scholar]
- 19.Portaccio E, Morrocchesi A, Romoli AMet al. Score on coma recovery scale-revised at admission predicts outcome at discharge in intensive rehabilitation after severe brain injury. Brain Inj. 2018;32(3):730-734. doi: 10.1080/02699052.2018.1440420 [DOI] [PubMed] [Google Scholar]
- 20.Mitchell SL, Teno JM, Kiely DKet al. The clinical course of advanced dementia. N Engl J Med. 2009;361(16):1529-1538. doi: 10.1056/NEJMoa0902234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Modawal A, Candadai NP, Mandell KMet al. et al. Weaning success among ventilator-dependent patients in a rehabilitation facility. Arch Phys Med Rehabil. 2002;83(2):154-157. doi: 10.1053/apmr.2002.29614 [DOI] [PubMed] [Google Scholar]
- 22. Central Bureau of Statistics – Statistical Abstract of Israel 2020 – No. 71 https://www.cbs.gov.il/en/publications/Pages/2020/Population-Statistical-Abstract-of-Israel-2020-No-71.aspx.
- 23.Jacobs JM, Marcus EL, Stessman J. Prolonged mechanical ventilation: symptomatology, well-being, and attitudes to life. J Am Med Dir Assoc. 2021;22(6):1242-1247. doi: 10.1016/j.jamda.2020.07.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sviri S, Garb Y, Stav Iet al. et al. Contradictions in end-of-life decisions for self and other, expressed by relatives of chronically ventilated patients. J Crit Care. 2009;24(2):293-301. doi: 10.1016/j.jcrc.2009.01.011 [DOI] [PubMed] [Google Scholar]
- 25.Dale CM, Carbone S, Istanboulian Let al. et al. Support needs and health-related quality of life of family caregivers of patients requiring prolonged mechanical ventilation and admission to a specialised weaning centre: a qualitative longitudinal interview study. Intensive Crit Care Nurs. 2020;58:102808. doi: 10.1016/j.iccn.2020.102808 [DOI] [PubMed] [Google Scholar]
- 26.Jacobs JM, Marcus EL, Stessman J. Prolonged mechanical ventilation: a comparison of patients treated at home compared with hospital long-term care. J Am Med Dir Assoc. 2021;22(2):418-424. doi: 10.1016/j.jamda.2020.06.038 [DOI] [PubMed] [Google Scholar]
- 27.Jubran A, Grant BJB, Duffner LAet al. et al. Long-term outcome after prolonged mechanical ventilation. A long-term acute-care hospital study. Am J Respir Crit Care Med. 2019;199(12):1508-1516. doi: 10.1164/rccm.201806-1131OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sprung CL, Ricou B, Hartog CSet al. Changes in end-of-life practices in European intensive care units from 1999 to 2016. JAMA. 2019;322(17):1692-1704. doi: 10.1001/jama.2019.14608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Giacino JT, Katz DI, Schiff NDet al. Practice guideline update recommendations summary: disorders of consciousness: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research. Neurology. 2018;91(10):450-460. doi: 10.1212/WNL.0000000000005926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kondziella D, Bender A, Diserens Ket al. et al. EAN Panel on Coma, Disorders of Consciousness . European Academy of Neurology guideline on the diagnosis of coma and other disorders of consciousness. Eur J Neurol. 2020;27(5):741-756. doi: 10.1111/ene.14151 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-jic-10.1177_08850666221088800 for Prognosis of Chronically Ventilated Patients in a Long-Term Ventilation Facility: Association with Age, Consciousness and Cognitive State by David Stein, Sigal Sviri, Michael Beil, Ilana Stav and Esther-Lee Marcus in Journal of Intensive Care Medicine
Supplemental material, sj-docx-1-jic-10.1177_08850666221088800 for Prognosis of Chronically Ventilated Patients in a Long-Term Ventilation Facility: Association with Age, Consciousness and Cognitive State by David Stein, Sigal Sviri, Michael Beil, Ilana Stav and Esther-Lee Marcus in Journal of Intensive Care Medicine
Supplemental material, sj-docx-2-jic-10.1177_08850666221088800 for Prognosis of Chronically Ventilated Patients in a Long-Term Ventilation Facility: Association with Age, Consciousness and Cognitive State by David Stein, Sigal Sviri, Michael Beil, Ilana Stav and Esther-Lee Marcus in Journal of Intensive Care Medicine