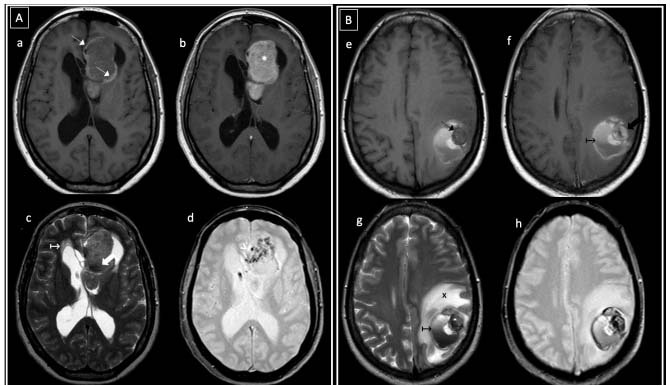
Figure 3. Intraventricular primary melanoma (A) and amelanocytic metastatic melanoma (B). In (A), a 46-year-old woman presented with headache. Axial T1WI pre and post-Gd (a, b) showed a heterogeneous left frontal intraventricular mass, with peripheral high signal areas (thin white arrows) and marked contrast enhancement (* in b). T2WI and GRE (c, d) showed hypointense foci (thick white arrows) and intratumoral magnetic susceptibility artifacts (white arrowhead). No restricted diffusion was observed (not shown). Hydrocephalus was present (white ↦ in c). In (B), a 48-year-old woman with a history of cutaneous melanoma presented with seizures. Axial MRI images (e-h) showed a hypointense-T1WI left parietal intra-axial peripheral nodule (thin black arrow in e) with heterogeneous contrast enhancement (thick black arrow in f). The lesion was surrounded by hemorrhagic products and hematocrit level (black ↦). Extensive vasogenic edema was observed (black x in g).