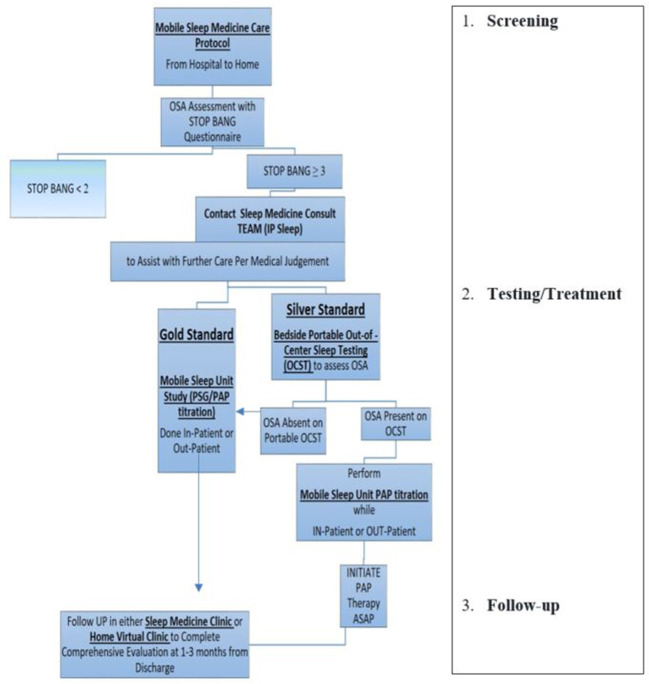
Figure 1.
Example of mobile sleep medicine care protocol. (1) Screening: Designed to provide effective and efficient SDB screening for patients admitted to hospital (or any other health care facility, e.g., rehab, specialty/subspecialty clinic, etc.), including patients with a high risk of CCV (stroke, MI, CHF, atrial fibrillation, hypertension, preeclampsia, etc.). After completing SDB screening either in-person, via EMR, or via Tele-Virtual/My Chart system, the Primary Team communicates with the Mobile Sleep Medicine Team/ in-patient Sleep Medicine Consulting Team (IP Sleep) to request sleep consultation for further management. (2) Testing/Treatment: The board-certified sleep medicine physician from the integrated mobile sleep medicine Team will discuss the sleep study results with patients and coordinate further management. Designed to deliver timely sleep medicine expertise to patients who screen positive for OSA. The IP sleep/mobile sleep medicine team evaluates patients and develops the diagnostic and treatment plan using mobile sleep unit technology. (3) Follow-up: IP sleep/mobile sleep medicine team coordinates further sleep medicine care in a sleep clinic, sleep lab, home health, and virtual telemedicine health. https://d11tooehygcg9z.cloudfront.net/My.AASM/AgentsOfChange/587417.pdf; https://aasm.org/winners-of-inaugural-change-agents-competition-propose-new-approaches-for-sleep-apnea-care.