Abstract
Digestive fistula on mesh is an exceptional and late complication of hernioplasty. The type of mesh and its position are often implicated in its occurrence. Clinical presentation is multiform. Morphological examinations are essential to confirm the diagnosis, and the curative treatment remains surgical.
Keywords: fistula, surgical mesh, ventral hernia
Because of its rarity and the late onset after hernioplasty, digestive fistula on mesh is a little‐known complication. Any abscess of the anterior abdominal wall that occurs even many years after hernioplasty should lead the clinician to evoke this diagnosis.
1. INTRODUCTION
The use of mesh in the treatment of anterior abdominal wall hernias is older than thoughts. 1 It has been an alternative to herniorrhaphy since 1890. 1 This method is widely used today because it offers several advantages. In fact, it strengthens the areas of parietal weakness, allows tension‐free closure, and allows the body to colonize and strengthen it with collagen fibers. 1 However, as it is a foreign body, the nature of the mesh must be as little harmful as possible.
There was a variety of mesh such as cotton or silk. The type of the mesh used is always a matter since 1890. 2 The work of Francis Usher led to a radical change in the mesh materials used, with the use of polymeric materials. 3 Multifilament polyester meshes such as Mersilene belong to the first generation of meshes. 1 Its use reached its peak in the 1980s, especially for large hernias of the anterior abdominal wall. 4 It offered several advantages such as the low risk of infection on the mesh and of hernia recurrence. 1 , 4
Although early complications of mesh cure are dominated by hematoma, seroma and infection. Recurrence is the most common late complication. 5 However, rare late complications include fistulas and intestinal or colonic migration of the mesh. 6
We report a case of intestinal fistula on mesh that occurred 30 years later after a cure of an umbilical hernia.
2. CASE SUMMARY
2.1. Clinical presentation
A 75‐year‐old woman, hypertensive, diabetic on oral antidiabetics, with a history of a median sub‐umbilical scar eventration after caesarean section, was treated with a pre‐peritoneal Mersilene prosthesis 30 years ago.
She consulted for a painful umbilical mass, evolving for 5 days, with no recent weight loss or associated transit disorders.
On examination, the patient was apyretic, with a firm umbilical mass, 10 cm in diameter, surmounted by a fistulous orifice with pus discharge. The rest of the abdomen was soft, and the hernial orifices were free. Pelvic touch was normal.
2.2. Differential diagnosis, investigations and treatment
The biological tests showed white blood cells at 11,000 elements/mm3, C‐reactive protein (CRP) at 25 mg/L, hemoglobin at 7 g/dl, and a normal renal function. The rest of the biological work‐up was normal.
An emergency abdominal Computerized Tomography (CT) scan was performed showing a 4‐cm air and fluid collection, suggestive of an abscess. This collection was in contact with an agglomeration of small bowel, around a hyperdense intraluminal foreign body, fistulated to the anterior abdominal wall, in the umbilical region.
The retained diagnosis was an anterior abdominal wall abscess complicating an enterocutaneous fistula on an old Mersilene mesh.
Empirical intravenous antibiotic therapy with cefotaxime and metronidazole was administered immediately after diagnosis. A short 48‐h preparation was performed: A transfusion with post‐transfusion hemoglobin of 10.6 g/dl, management of co‐morbidities, combined with respiratory and psychological preparation, and nutritional support.
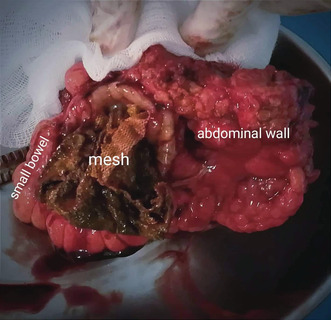
The procedure was performed by median laparotomy. Intraoperative exploration showed a 10‐cm umbilical inflammatory swelling, located on the old scar, surmounted by a fistulous orifice. A careful incision was made with pus drainage. A bacteriological sample of the pus was taken. Access to the peritoneal cavity was started 2–3 cm below the xiphoid to avoid injuring the small intestine agglomerated under the umbilicus. Release of the intestinal and parietal adhesions was laborious, individualizing a small loop fistulated to the skin through an intraperitoneal mesh. This loop was located 50 cm from Bauhin's valve. A single block resection of the fistulated bowel loop, the Mersilene mesh, the adjacent fascia and skin, was performed (Figure 1), followed by a manual side‐to‐side bowel anastomosis. A polyglactin mesh was placed between the intestines and the abdominal wall. The fascial plan was closed in free tension by separate stitches. The skin plan over abscess cavity was left open to avoid secondary purulent retentions.
FIGURE 1.
The monobloc resected operative specimen, showing from left to right: the victim bowel loop, the eroding mesh soiled with fecal material from the fistula, and the part of the wall communicating with the bowel segment.
2.3. Outcome and follow‐up
The postoperative course was simple. Transit was restored on the second postoperative day and oral feeding was allowed. Antibiotic therapy was stopped immediately postoperatively. Intraoperative bacteriological cultures were positive for Escherichia coli and Klebsiella oxytoca, both sensitive to cefotaxime. Local wound care was performed with directed wound healing for the skin loss.
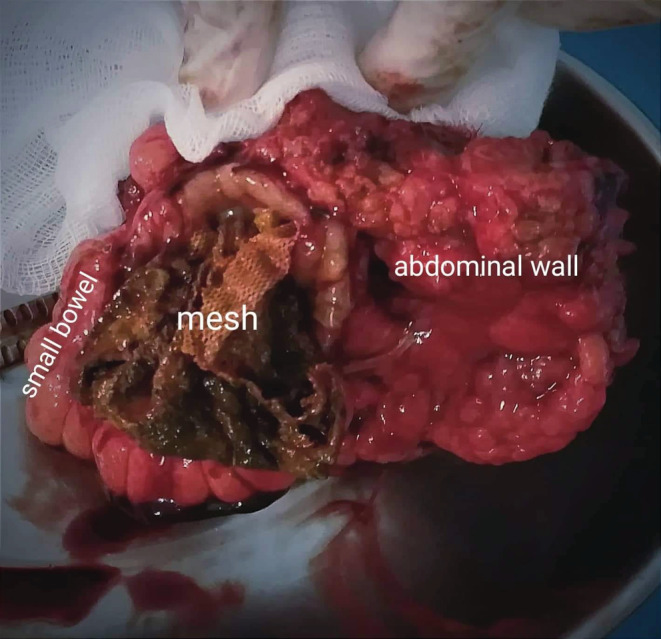
The patient was discharged at day 5 post‐surgery. The wound healed after 10 weeks. Anatomopathological examination of the surgical specimen revealed an intestinal loop with a foreign body type inflammatory reaction, adhering to a solid fibro‐fatty and muscular mass, not well limited, including a synthetic membrane (Figure 2).
FIGURE 2.
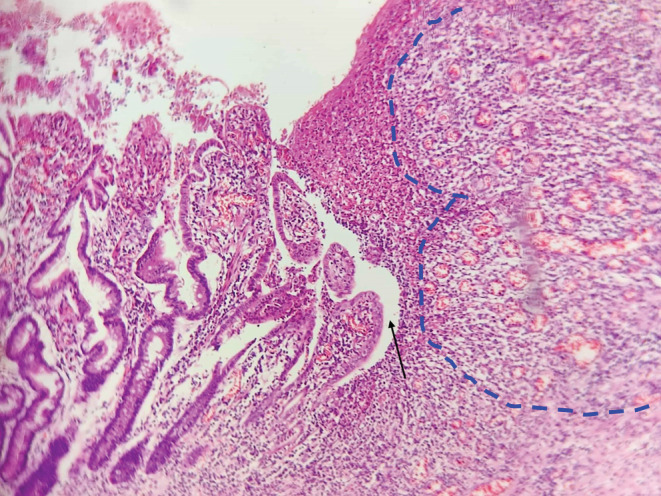
Histopathological examination showing a foreign body reaction and inflammatory granulomas forming the fistula path.
Actually, the patient has no recurrence of the eventration after 2 years of follow‐up.
3. DISCUSSION
Our case is important for four reasons: the diagnostic discussion in front of this clinical presentation of abdominal wall abscess is quite rich. It focuses on a rare complication of anterior abdominal wall Hernioplasty. The very long time (30 years) between the placement of the mesh and the occurrence of the complication is a very important point to mention. The type of mesh that is no longer used but that many patients are living with today is a matter for discussion as it is as essential as the type of complication.
In the presence of anterior abdominal wall abscess, several diagnoses may be discussed, starting with deep abdominal diseases: The first diagnoses to be evocated are infected colonic tumor, fistulated to the skin, and fistulated abscessed colonic diverticulitis. In our situation, the patient's age is in favor of these diagnoses, but the umbilical location and the absence of transit disorders are not in line with these diagnoses. 7 , 8 Then, we should evoke Crohn's disease complicated by enterocutaneous fistula. It occurs at any age and can affect all segments of the digestive tract. In our patient, the absence of chronic diarrhea is an argument against this diagnosis. 9 Also, digestive tuberculosis in its fistulizing form must be evoked systematically in an endemic country. 10 At last, superficial affections can be considered, like abscessed, 11 an abscess complicating a furuncle, which especially occurs in diabetic patient, 12 or an abdominal abscess complicating an insulin injection. 13 But in our patient, there was no history of furuncle or insulin injections. The fistula on the old Mersilene mesh was not evoked by our clinicians before the CT scan results. The CT scan is of great importance in the etiologic diagnosis of any suppuration of the abdominal wall. 14 , 15
Digestive mesh fistula is a rare and late complication of abdominal parietal surgery. 6 , 16 The mesh involved is mainly that made of synthetic materials. 6 , 17 The efforts made by Rives and Louis have succeeded in reducing the rate of this complication by prohibiting the intraperitoneal implantation of synthetic meshes, which are capable of eroding the digestive tract. 6 , 18 The clinical presentation is often made of suppuration on the scar. The chronic and recurrent nature of the suppuration should suggest a digestive fistula. Sometimes, an intestinal occlusion may occur if the mesh migrates into the intestine and obstructs its lumen. Rarely, it is a urinary tract infection if the mesh migrates into the bladder. 6 The clinical presentation in our patient was an acute parietal suppuration. The progression to chronicity might have been inevitable if intervention had not been made.
In the study published by Morin et al., 6 the authors reported 22 cases from the literature of digestive fistula appearing after mesh cure of eventration. Among those cases, fistula occurred after a mean period of 6.7 years with extremes ranging from 18 months to 15 years. However, in the current case, the interval was 30 years, which is part of the originality of this case and represents a diagnostic pitfall.
For the mesh's material responsible for this complication, literature data place polyester meshes such as Mersilene and Dacron in first place with 64% of cases of digestive fistulas or intra‐digestive migration of mesh, far ahead of polyethylene meshes such as Marlex with only about 23% of cases. 6 In our patient, the mesh was made of polyester.
Overviewing our study, our patient had all the key elements of the clinical case presented: A parietal surgery dating back several years, using a mesh with a high risk associated with digestive fistula, placed in a pre‐peritoneal position, which is more predisposing to this complication. The clinical features were almost typical and the abdominal CT scan allowed to retain the diagnosis and to eliminate differential diagnoses. The surgical treatment had resolved the problem radically with simple postoperative course.
4. CONCLUSION
Digestive fistula on mesh is a rare and late complication of hernioplasty. Good knowledge of mesh materials and their interaction with the body, the advent of composite meshes, and improved surgical techniques have reduced the risk of its occurrence. However, this complication must always be suspected in any patient with a mesh, who presents an acute or chronic suppuration on the scar, and keeping in mind other differential diagnoses.
AUTHORS CONTRIBUTIONS
Mohamed Farès Mahjoubi has drafted the work. Nada Essid has made data collection. Bochra Rezgui and Mohamed Zran have made substantial contributions to the literature research. Karim Haouet revised the work. Mounir Ben Moussa has made substantial contributions to the conception of the work.
FUNDING INFORMATION
No specific funding was received from any bodies in the public, commercial or not‐for‐profit sectors to carry out the work described in this article.
CONFLICT OF INTEREST
Authors have no conflict of interests.
ETHICAL APPROVAL
Our locally appointed ethics committee “Charles Nicolle Hospital local committee” has approved the research protocol and informed consent has been obtained from the subject.
CONSENT
Written informed consent was obtained from the patient.
HUMAN AND ANIMAL RIGHTS
Our study complies with the Declaration of Helsinki.
ACKNOWLEDGMENT
None.
Mahjoubi MF, Essid N, Rezgui B, Zran M, Haouet K, Ben Moussa M. When a polyester mesh causes an enterocutaneous fistula, 30 years after its implantation. Clin Case Rep. 2022;10:e06519. doi: 10.1002/ccr3.6519
DATA AVAILABILITY STATEMENT
The data and supportive information is available within the article.
REFERENCES
- 1. Baylón K, Rodríguez‐Camarillo P, Elías‐Zúñiga A, Díaz‐Elizondo JA, Gilkerson R, Lozano K. Past, present and future of surgical meshes: a review. Membranes. 2017;7(3):47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chowbey P. Endoscopic Repair of Abdominal Wall Hernias. Byword Books Private Limited; 2012:221. [Google Scholar]
- 3. Usher FC, Hill JR, Ochsner JL. Hernia repair with Marlex mesh. A comparison of techniques. Surgery. 1959;46:718‐724. [PubMed] [Google Scholar]
- 4. Cerise EJ, Busuttil RW, Craighead CC, Ogden WW. The use of Mersilene mesh in repair of abdominal wall hernias: a clinical and experimental study. Ann Surg. 1975;181(5):728‐734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lau H, Patil NG. Umbilical hernia in adults. Surg Endosc. 2003;17(12):2016‐2020. [DOI] [PubMed] [Google Scholar]
- 6. Morin B, Bonnamy C, Maurel J, Samama G, Gignoux M. Fistules intestinales tardives après implantation de prothèse pariétale abdominale. Ann Chir. 2001;126(9):876‐880. [DOI] [PubMed] [Google Scholar]
- 7. Andaz S, Heald RJ. Abdominal wall abscess–an unusual primary presentation of a transverse colonic carcinoma. Postgrad Med J. 1993;69(816):826‐828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Qaseem A, Etxeandia‐Ikobaltzeta I, Lin JS, et al. Diagnosis and management of acute left‐sided colonic diverticulitis: a clinical guideline from the American College of Physicians. Ann Intern Med. 2022;175(3):399‐415. [DOI] [PubMed] [Google Scholar]
- 9. Gajendran M, Loganathan P, Catinella AP, Hashash JG. A comprehensive review and update on Crohn's disease. Dis Mon. 2018;64(2):20‐57. [DOI] [PubMed] [Google Scholar]
- 10. Gan DEY, Sibin R, Payus AO, Hayati F. Colo‐appendico‐duodenal fistula: rare presentation of extrapulmonary tuberculosis. Clin Case Rep. 2021;9(10):e04797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Torabi H, Shirini K, Ghaffari R. Rare case of umbilical urachal sinus mimicking infected umbilical abscess: a case report. Clin Case Rep. 2022;10(3):e05598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nowicka D, Grywalska E. Staphylococcus aureus and host immunity in recurrent furunculosis. Dermatology. 2019;235(4):295‐305. [DOI] [PubMed] [Google Scholar]
- 13. Han VX, Loke KY, Chan SM. Recurrent Mycobacterium fortuitum insulin injection site abscesses. J Paediatr Child Health. 2018;54(3):316‐318. [DOI] [PubMed] [Google Scholar]
- 14. Tsukuda K, Ikeda E, Miyake T, et al. Abdominal wall and thigh abscess resulting from the penetration of ascending colon cancer. Acta Med Okayama. 2005;59(6):281‐283. [DOI] [PubMed] [Google Scholar]
- 15. Patel SH, Bihlmeyer S, Eggenberger JC, Shanker BA, Cleary RK. Locally advanced perforated appendiceal cancer: case report and review. Clin Case Rep. 2022;10(2):e05349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Takayama Y, Kaneoka Y, Maeda A, Takahashi T, Seita K. Long‐term outcomes using a questionnaire after inguinal hernia repair in female. Indian J Surg. 2022. doi: 10.1007/s12262-022-03323-5 [DOI] [Google Scholar]
- 17. Licari L, Viola S, Salamone G. The synthetic scaffolds for ventral hernia repair: perspectives for regenerative surgery—systematic review. Indian J Surg. 2022. doi: 10.1007/s12262-021-03205-2 [DOI] [Google Scholar]
- 18. Louis D, Stoppa R, Henry X, Verhaeghe P. Postoperative eventrations. Apropos of 247 surgically treated cases. J Chir (Paris). 1985;122(10):523‐527. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data and supportive information is available within the article.


