Abstract
For better or worse, the people one lives with may exert a powerful influence on one’s mental health, perhaps especially during times of stress. The COVID-19 pandemic—a large-scale stressor that prompted health recommendations to stay home to reduce disease spread—provided a unique context for examining how the people who share one’s home may shape one’s mental health. A seven-wave longitudinal study assessed mental health month to month before and during the pandemic (February through September 2020) in two diverse samples of U.S. adults (N = 656; N = 544). Preregistered analyses demonstrated that people living with close others (children and/or romantic partners) experienced better well-being before and during the pandemic’s first 6 months. These groups also experienced unique increases in ill-being during the pandemic’s onset, but parents’ ill-being also recovered more quickly. These findings highlight the crucial protective function of close relationships for mental health both generally and amid a pandemic.
Keywords: COVID-19, mental health, well-being, parenting, close relationships, open data, open materials, preregistered
For better or worse, people who live together may affect one another’s mental health. In times of stress—when relationships may be strained but may also become the greatest source of support—the people who share one’s home may exert a particularly powerful influence on one’s mental health. The COVID-19 pandemic is a global stressor and a far-reaching threat to mental health. This stressor has also prompted a public-health focus on staying home to curb disease spread (U.S. Centers for Disease Control and Prevention, 2020), which presents a unique context for examining how the people one lives with may shape mental health. On the one hand, these people may be a source of tension and frustration, putting mental health at risk. On the other hand, they may be a source of social connection, fostering better mental health. To understand who may be most vulnerable, it is crucial to examine how the people one lives with, especially during a pandemic, can help or harm mental health.
The current work bridges social psychological science with clinical psychological science to determine how living with close others may risk or protect people’s mental health. We focus on parent–child relationships and romantic relationships because they are among people’s most important relationships (Lemay & Neal, 2014; Nelson et al., 2013). By leveraging a seven-wave longitudinal design that followed parents living with children and people living with romantic partners both before COVID-19 was declared a pandemic (February 2020) and after (March through September 2020), our preregistered analyses allowed us to disentangle the unique mental-health outcomes that (a) predate the pandemic, (b) are specific to the pandemic onset, and (c) persisted across the pandemic’s first 6 months.
Mental-Health Risks for People in Close Relationships
Both news headlines and initial empirical evidence have suggested that people living with close others may be more vulnerable to the mental-health threat posed by the COVID-19 pandemic. Specifically, news articles have often suggested that parents living with children are particularly vulnerable to poor mental health in this context because of life disruptions and anxiety surrounding children’s care and education (Grose, 2020). This impression is substantiated by initial empirical evidence collected during the COVID-19 pandemic demonstrating that parents are experiencing significantly higher stress than nonparents because of increased child-care duties (American Psychological Association, 2020; Calarco et al., 2020). Many parents are also now faced with increased difficulty in balancing work and family responsibilities while working from home (Chung et al., 2020; Craig & Churchill, 2021). Furthermore, unprecedented increases in unemployment and poverty due to the pandemic may disproportionately affect parents living with children given that they are more likely than nonparents to report stress about meeting their basic needs (e.g., nutrition; American Psychological Association, 2020; Fontanesi et al., 2020). Research drawing from prior crises (e.g., natural disasters) has also suggested that parents’ mental health may be particularly at risk in the face of a large-scale stressor (Prime et al., 2020). Overall, parents living with children are facing several challenges because of COVID-19 that may further threaten their mental health.
People living with romantic partners may also be at an increased vulnerability to the negative mental-health effects of the pandemic—an impression similarly supported by both news headlines and some empirical evidence. News articles have warned that COVID-19 is a “pressure cooker” for romantic relationships and may result in conflict and divorce (Prasso, 2020; Stroh, 2020). Research has indeed found that a third of romantic partners are experiencing conflict because of the pandemic, which was linked to lower intimacy in their relationships (Luetke et al., 2020). Researchers have theorized that romantic relationships may be particularly strained during the pandemic (Pietromonaco & Overall, 2021) because of increased time spent together or feeling confined by safety measures implemented to curb disease spread. Furthermore, romantic partners may be one of the few sources of accessible social support during stay-at-home recommendations, but the stress induced by major external stressors can make it difficult to provide and receive effective support (as suggested by research on other stressors, including natural disasters; Cohan, 2010). Consequently, romantic partners may be particularly prone to feeling that their needs are not being met. In addition, other research has demonstrated that external stress (e.g., due to economic strain) is linked to greater relationship conflict (Prime et al., 2020) and lower relationship satisfaction (Harper et al., 2000; Neff & Karney, 2004). Thus, people living with romantic partners are likely facing numerous challenges to their mental health because of the COVID-19 pandemic.
Overall, theorizing and some prior evidence suggest that people living with close others (children and/or romantic partners) may experience worse mental health than people who are not, perhaps especially during the COVID-19 pandemic.
Protective Benefits of Close Relationships
In contrast to the growing evidence that people living with close others may be particularly prone to poor mental health during the COVID-19 pandemic, long-standing relationships research suggests a starkly different pattern. Indeed, people living with close others—their children and/or romantic partners—tend to experience better mental health on average (Lemay & Neal, 2014; Nelson et al., 2014), which may extend to the COVID-19 context. More specifically, prior research has revealed that parents derive a sense of meaning and purpose from parenting (Nelson et al., 2014) and that compared with nonparents, parents experience greater emotional well-being (Nelson et al., 2013). These benefits may offset the costs of unanticipated disruptions to life routines caused by the pandemic. For instance, some qualitative research has revealed that at least some parents are enjoying extra time spent with their children because of pandemic school closures, which may function as a unique source of happiness for parents in an otherwise stressful context (Calarco et al., 2020). Consequently, parents living with children may be buffered from poorer mental-health outcomes during the pandemic.
Relationship science has also consistently demonstrated that romantic relationships are a key determinant of greater well-being in general (Diener & Seligman, 2002; Proulx et al., 2007), which may extend to the COVID-19 pandemic context. Specifically, satisfying romantic relationships are a key source of social-need fulfillment and support, which tend to predict better well-being (Lemay & Neal, 2014; Pietromonaco & Collins, 2017) and can buffer partners from negative mental-health outcomes (S. Cohen, 2004) like depression (Whisman, 2001). Staying at home more because of the pandemic may also provide couples with more opportunities for intimacy, which can reduce stress (Jakubiak & Feeney, 2019). By having access to a key source of physical and emotional intimacy, people living with a romantic partner may be better able to cope with the stress associated with the COVID-19 pandemic and bolster their well-being to a greater degree than people living without a romantic partner (Elmer et al., 2020; Jakubiak & Feeney, 2019). Such findings suggest that people living with romantic partners may also be protected from COVID-19-related challenges to mental health.
Overall, and in contrast to other research, existing theory and evidence suggest that people living with children and/or romantic partners may actually experience better mental health than people living without these close others, even within the COVID-19 pandemic context.
Current Investigation
It is currently an open question whether people living with close others (vs. people not living with close others) during a time of intense stress—such as the COVID-19 pandemic—are at risk for worse mental health or experience better mental health. The available literature suggests a very mixed pattern. This literature is also limited by the fact that very few empirical studies examining the pandemic’s impact on mental health have considered mental health before the pandemic, and thus, these differences may have existed before the onset of the pandemic. Therefore, it is unclear how the mental health of people living with close others may differ from people who are not, and whether any differences are unique to the COVID-19 pandemic. In the current work, we sought to address this mixed evidence by examining the mental health of people living with children and/or romantic partners—two of people’s most influential relationships—and identifying mental-health differences existing before the pandemic compared with differences uniquely driven by it and whether these differences persist over time. Addressing these urgent questions will reveal whose mental health is the most vulnerable and the people in need of the most support.
As part of a longitudinal study investigating individuals’ responses to the COVID-19 pandemic, we conducted a preregistered seven-wave longitudinal test of how the mental health of people living with children and/or romantic partners may differ from people not living with children and/or romantic partners. We collected monthly data from two diverse U.S. samples (Sample A: N = 656; Sample B: N = 544), starting before the COVID-19 pandemic (February 2020) and continuing during its onset (February to March 2020) and across its first 6 months (March through September 2020). This allowed us to disentangle the unique differences in mental health between people living with close others (compared with people not living with close others) that (a) predate the pandemic, (b) are specific to the onset of the pandemic, and (c) persisted across 6 months of the pandemic. We measured mental health using indices of well-being (i.e., life satisfaction, meaning in life) and ill-being (i.e., depression and anxiety) to capture both flourishing and symptoms, respectively (Keyes, 2007).
Method
Participants
Two separate samples of U.S. participants were recruited from Amazon Mechanical Turk. This platform allowed us to recruit participants and collect time-sensitive assessments of mental health that we may have missed through traditional longitudinal-study recruitment techniques (e.g., community flyers). To be eligible, participants were required to have a 95% or greater approval rating, be U.S. residents, and have completed at least 100 human intelligence tasks on the platform. To promote high-quality data collection, participants completed multiple attention checks at every time point. Surveys with one or more failed attention checks and multiple surveys completed by the same participant were excluded from the final data sets. Participants provided informed consent and were compensated approximately $9 per hr. This procedure was approved by the University of Toronto Research Ethics Board (Protocol 00033962). Participants with at least one assessment of mental health and parental or relationship status after February (T1) were included in analyses.1
Sample A
Sample A (N = 656) ranged in age from 18 to 75 years (M = 37, SD = 11). This sample was recruited to be diverse with respect to racial and ethnic identity (with an a priori goal to recruit at least 200 people from three different racial and ethnic backgrounds, which was met). To assess racial and ethnic identity, participants responded to the question, “What ethnicity do you identify with most?” Although this item asks solely about ethnicity, the response options included both racial and ethnic identities. Thus, we refer to this construct as racial and ethnic identity throughout. The sample was 35% European American/White, 31% East or South Asian/Asian American, 30% African/African American, and 4% other race or ethnicity. The sample was 53% women and 44% men; 3% reported other gender or did not report gender. More than a third (38%) of participants reported an income between $50,001 and $100,000 (range = < $15,000 to > $200,000). Missing data across measurement occasions ranged from 11.4% in March (T2) to 32.8% in September (T7). On average, participants provided data for 5.53 measurement occasions (SD = 1.72) out of seven.
Sample B
Sample B (N = 544) ranged in age from 20 to 81 years or older (M = 43, SD = 13). This sample was recruited to be diverse with respect to political ideology (with an a priori goal to recruit at least 300 people from the two dominant U.S. political parties, which was met2). The participant sample was 83% European American/White, 6% African or African American, 5% East or South Asian/Asian American, 6% other race or ethnicity; 49% Democrat and 51% Republican. This sample included 50% women, 49% men, and less than 1% reported other gender or did not report gender. Comparable with Sample A, more than a third (41%) of participants reported an income between $50,001 and $100,000 (range = < $15,000 to > $200,000). Missing data across measurement occasions ranged from 2.2% in March (T2) to 25.6% in August (T6). On average, participants provided data for 5.95 measurement occasions (SD = 1.48) out of seven.
Procedure and measures
Procedure
Sample A and Sample B participants completed monthly assessments of well-being and ill-being at the same time each month from February (T1) through September (T7)3 in reference to the “past four weeks,” with one exception: Sample B completed T1 2 weeks after Sample A, in reference to the “past two weeks.” Participants also completed several assessments of parental and partner status during the study.
Well-being and ill-being
We assessed well-being (i.e., life satisfaction and meaning in life) using the Satisfaction With Life Scale (αs = .91–.93; Diener et al., 1985) and items from the Meaning in Life Questionnaire (αs = .89–.93; Steger et al., 2006). Given the high correlations between these two scales (rs = .74–.84) and that both scales produced the same results in our main comparisons when analyzed separately, we created a composite measure. Specifically, we used percentage of maximum possible (POMP) scoring (P. Cohen et al., 1999) so that both well-being scales were on the same scale from 0 to 100. We then averaged them to create a well-being composite.
We assessed ill-being (i.e., depression and anxiety) using the Center for Epidemiological Studies Depression Scale (αs = .89–.92; Radloff, 1977) and the anxiety items from the Hospital Anxiety and Depression Scale (αs = .89–.90; Zigmond & Snaith, 1983). Given that the two ill-being scales were highly correlated (rs = .62–.70) and that both scales produced the same results in our main comparisons when analyzed separately, we created a composite measure. Specifically, similar to our handling of well-being measures, we used POMP scoring so that both ill-being scales were on the same scale from 0 to 100 and then averaged them to create an ill-being composite.
Parent and partner analysis and comparison groups
Parental and relationship status were assessed multiple times across the seven time points. Participants were asked about the number of children they have (i.e., are the parents of) and live with, their romantic relationship status, and whether they were living with a romantic partner. Participants were considered to be parents living with children if they indicated at least once that they both had and were living with a child or children. Participants were considered to be living with a partner if they indicated at least once that they both had and were living with a romantic partner. See Tables 1 and 2 for demographic information across groups in both samples.
Table 1.
Comparison of the Sociodemographic Characteristics of Parents Living With Children and Nonparents and Parents Not Living With Children in Samples A and B
| Characteristic | Sample A | Sample B | ||||||
|---|---|---|---|---|---|---|---|---|
| Parents living with children | Test of the difference | Parents living with children | Test of the difference | |||||
| Yes | Noa | Statistic | p | Yes | Noa | Statistic | p | |
| Age (years) |
M = 39.8 (SD = 8.4) |
M = 35.9 (SD = 12.3) |
t(592) = 4.73 | < .001 |
M = 42.5 (SD = 10.0) |
M = 43.7 (SD = 15.2) |
t(527) = 1.16 | .246 |
| Gender (%) | χ2(1, N = 650) = 21.66 | χ2(1, N = 543) = 0.44 | .506 | |||||
| Men | 32.3 | 50.5 | < .001 | 47.9 | 50.9 | |||
| Women | 66.8 | 46.1 | 52.1 | 48.7 | ||||
| Racial and ethnic identity (%) | χ2(3, N = 655) = 7.27 | .064 | χ2(3, N = 543) = 8.23 | .041 | ||||
| African or African American | 35.9 | 27.1 | 4.6 | 6.9 | ||||
| East Asian or East Asian American | 17.7 | 24.3 | 1.7 | 4.9 | ||||
| White/European/ European American | 32.7 | 35.3 | 84.0 | 82.4 | ||||
| Other racial or ethnic identity | 12.7 | 11.0 | 9.7 | 5.6 | ||||
| Political affiliation (%) | χ2(2, N = 655) = 5.49 | .064 | χ2(1, N = 543) = 9.19 | .002 | ||||
| Republican | 20.0 | 13.1 | 58.4 | 44.8 | ||||
| Democrat | 49.5 | 50.5 | 41.6 | 54.9 | ||||
| Independent/other | 29.5 | 34.2 | — | — | ||||
This group included both parents not living with their children and people who did not have children.
Table 2.
Comparison of the Sociodemographic Characteristics of People Living With Partners and People Not in a Romantic Relationship or Not Living With Their Romantic Partners in Samples A and B
| Characteristic | Sample A | Sample B | ||||||
|---|---|---|---|---|---|---|---|---|
| Living with a romantic partner | Test of the difference | Living with a romantic partner | Test of the difference | |||||
| Yes | Noa | Statistic | p | Yes | Noa | Statistic | p | |
| Age (years) |
M = 39.3 (SD = 10.8) |
M = 35.7 (SD = 11.3) |
t(617) = 4.04 | < .001 |
M = 44.0 (SD = 12.1) |
M = 42.1 (SD = 14.4) |
t(454) = 1.58 | .114 |
| Gender (%) | χ2(1, N = 633) = 17.77 | < .001 | χ2(1, N = 543) = 0.00 | .952 | ||||
| Men | 35.1 | 52.0 | 50.0 | 49.2 | ||||
| Women | 62.1 | 45.8 | 50.0 | 50.4 | ||||
| Racial and ethnic identity (%) | χ2(3, N = 637) = 6.13 | .105 | χ2(3, N = 543) = 9.98 | .019 | ||||
| African or African American | 25.1 | 34.1 | 3.2 | 9.3 | ||||
| East Asian or East Asian American | 23.7 | 21.2 | 2.9 | 4.2 | ||||
| White/European/ European American | 36.8 | 32.7 | 86.0 | 79.2 | ||||
| Other racial or ethnic identity | 12.4 | 10.3 | 7.8 | 6.8 | ||||
| Political affiliation (%) | χ2(2, N = 637) = 7.97 | .019 | χ2(1, N = 543) = 9.67 | .002 | ||||
| Republican | 19.2 | 11.7 | 56.8 | 42.8 | ||||
| Democrat | 46.0 | 53.9 | 43.2 | 56.8 | ||||
| Independent/other | 32.6 | 32.6 | — | — | ||||
This group included both people not in a romantic relationship and people not living with their romantic partners.
As per our preregistration, to focus on the mental health of people living with close others, participants who had children (i.e., are parents) but were not currently living with them were not included in the parent analysis group (instead, they were included in the comparison group along with people without children). Likewise, participants who had romantic partners (i.e., were in a committed relationship) but were not currently living with their partners were not included in the partner analysis group (instead, they were included in the comparison group along with people without a romantic partner). Thus, these preregistered comparison groups provided a particularly stringent test of our hypotheses; but to ensure that the present results were not attributable to these heterogeneous comparison groups, we also preregistered analyses with narrower comparison groups (i.e., only people without children and only people without romantic partners). Results of these preregistered supplementary analyses paralleled those of the main comparison groups (for more details, see the Supplemental Material available online).
Analytic overview
We preregistered the analytic strategy before analyzing the data (available at https://osf.io/pcyeg). The design for this ongoing longitudinal study was not preregistered before beginning data collection. All analyses were conducted in the R software environment (Version 3.6.1; R Core Team, 2019) using the nlme (Version 3.1-151; Pinheiro et al., 2020) and effsize (Version 0.8.1; Torchiano, 2020) packages.
We examined the mental health of parents living with children (vs. a comparison group: nonparents and parents not living with children) and people living with romantic partners (vs. a comparison group: people not in a romantic relationship and people not living with their romantic partners). To test group differences (i.e., regarding parental or romantic-relationship status) in mental health before the pandemic (February 2020), we used independent samples t tests. To test group differences in change in mental health during pandemic onset (February to March 2020), we used random-intercept multilevel models predicting well-being and ill-being from group, time (spanning February to March 2020), and their interaction (in linear models). To test group differences in the rate of change in mental health after pandemic onset (March to September 2020), we used random-intercept, random-slope multilevel models predicting well-being and ill-being from group, time (spanning March to September), and their interaction (in linear models) and separately for group, time, time squared, and interactions between group and the time variables (in quadratic models). To test group differences in levels of mental health across the same periods (February to March and March to September), we used random-intercept multilevel models predicting well-being and ill-being from group.
Discrete time was assessed in weeks and mean-centered. In all multilevel models, time points were nested within individuals. Given the large number of tests (46 primary tests and additional sensitivity tests), we used false-discovery-rate (FDR) correction to interpret statistical significance (Benjamini & Hochberg, 1995). FDR correction compares the largest p value with the set α level (i.e., .05) and then compares each descending p value with an increasingly smaller α level. We selected the critical p value from each of the 46 preregistered primary tests and applied FDR correction to each p value separately within each sample. FDR-corrected p values and uncorrected 95% confidence intervals (CIs) are reported. Results that were significant after FDR correction are interpreted as reliable, and results that were significant before FDR correction (i.e., 95% CIs that do not contain zero) are considered suggestive. All analyses were conducted separately for each sample with one exception: We combined the two samples for the Parent × Partner Status interaction models to increase our power to detect this two-way interaction.
Results
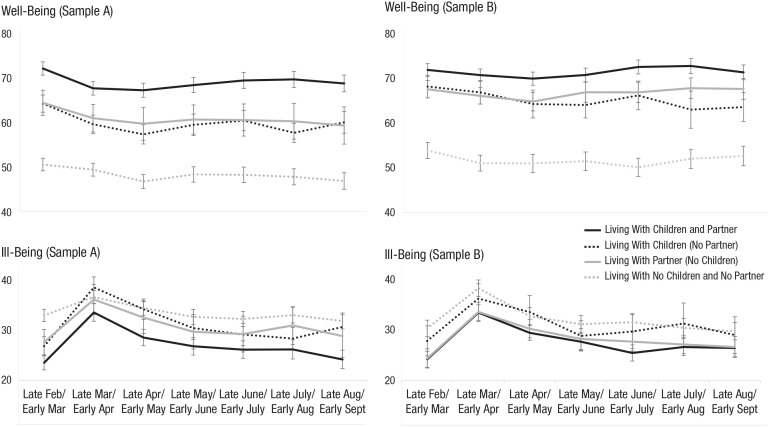
Figure 1 depicts mental-health trajectories from February to September 2020 for people living with close others (i.e., children, a partner, or both children and a partner) and people who were not. These separate trajectories are displayed for descriptive purposes only—we did not observe any interactions between parent and partner status regarding well-being or ill-being—see the Additional Analyses (Preregistered) section below. The following primary results focus on the distinct mental health of parents living with children and people living with a romantic partner. Key parameter estimates are reported in text, and results of all primary and additional models and statistical code are available at https://osf.io/pcyeg.
Fig. 1.
Well-being and ill-being trajectories for parents living with children (vs. a comparison group: nonparents and parents not living with children) and people living with partners (vs. a comparison group: people not in a romantic relationship and people not living with their partners) before the COVID-19 pandemic (February), during its onset (March), and across its first 6 months (March–September) in 2020. Well-being and ill-being ranged from 0 to 100 (y-axis is truncated). Error bars indicate ±1 SE.
In the following sections, we refer to the comparison group for parents living with children as “people not living with children” (which included both nonparents and parents not living with their children) and the comparison group for people living with a romantic partner as “people not living with a romantic partner” (which included both people who were not in a relationship and people not living with a romantic partner).
Primary analyses
Before pandemic onset
Parents living with children (compared with people not living with children) had much higher well-being in both samples (Sample A: Cohen’s d = 0.66; Sample B: Cohen’s d = 0.53) and somewhat lower ill-being (Sample A: Cohen’s d = 0.36; Sample B: Cohen’s d = 0.15). People living with a romantic partner (compared with people not living with a romantic partner) also had much higher well-being (Sample A: Cohen’s d = 0.70; Sample B: Cohen’s d = 0.60) and somewhat lower ill-being (Sample A: Cohen’s d = 0.33; Sample B: Cohen’s d = 0.29) in both samples. Thus, the mental health of parents living with children and people living with romantic partners was higher than their comparison groups before the onset of the pandemic.
During pandemic onset
Across all participants, well-being decreased slightly (ds = 0.08–0.11) and ill-being increased moderately (ds = 0.33–0.43) during pandemic onset (for all statistics regarding average trajectories across all participants, see the Supplemental Material).
For models examining parents, see Tables 3 and 4. In both samples, parents living with children experienced similar decreases in well-being compared with people who were not living with children, FDR ps > .070. However, parents living with children experienced greater increases in ill-being in Sample A compared with people who were not living with children (interaction: β = 1.37, 95% confidence interval [CI] = [0.70, 2.05], FDR p = .007; although not in Sample B, interaction: β = 0.12, 95% CI = [−0.37, 0.60], FDR p = .879).
Table 3.
Multilevel Models Predicting Well-Being for Parents Living With Children (vs. a Comparison Group: Nonparents and Parents Not Living With Children)
| Predictor | Sample A (N = 656) | Sample B (N = 544) | ||||||
|---|---|---|---|---|---|---|---|---|
| b | 95% CI | SE | p | b | 95% CI | SE | p | |
| Change in well-being during pandemic onset (T1 to T2)a | ||||||||
| Intercept | 53.95 | [51.84, 56.06] | 1.08 | < .001 | 58.07 | [55.67, 60.47] | 1.22 | < .001 |
| Time | −0.45 | [−0.78, −0.11] | 0.17 | .009 | −0.39 | [−0.60, −0.18] | 0.11 | < .001 |
| Parent | 13.83 | [10.19, 17.46] | 1.85 | < .001 | 12.50 | [8.88, 16.13] | 1.85 | < .001 |
| Time × Parent | −0.67 | [−1.23, −0.11] | 0.29 | .020 | 0.19 | [−0.13, 0.52] | 0.16 | .242 |
| Linear change in well-being after pandemic onset (T2 through T7) | ||||||||
| Intercept | 51.82 | [49.70, 53.94] | 1.08 | < .001 | 57.22 | [54.75, 59.69] | 1.26 | < .001 |
| Time | −0.03 | [−0.10, 0.04] | 0.04 | .393 | 0.06 | [−0.01, 0.13] | 0.04 | .098 |
| Parent | 14.62 | [10.96, 18.29] | 1.87 | < .001 | 12.51 | [8.76, 16.25] | 1.91 | < .001 |
| Time × Parent | 0.14 | [0.02, 0.26] | 0.06 | .024 | −0.03 | [−0.14, 0.07] | 0.05 | .538 |
| Quadratic change in well-being after pandemic onset (T2 through T7) | ||||||||
| Intercept | 51.45 | [49.23, 53.67] | 1.13 | < .001 | 57.03 | [54.41, 59.64] | 1.33 | < .001 |
| Time | −0.03 | [−0.10, 0.04] | 0.04 | .422 | 0.06 | [−0.01, 0.13] | 0.04 | .075 |
| Time2 | 0.01 | [−0.00, 0.02] | 0.01 | .166 | 0.00 | [−0.01, 0.01] | 0.01 | .484 |
| Parent | 14.94 | [11.11, 18.78] | 1.95 | < .001 | 12.47 | [8.51, 16.43] | 2.02 | < .001 |
| Time × Parent | 0.14 | [0.02, 0.26] | 0.06 | .022 | −0.03 | [−0.13, 0.07] | 0.05 | .562 |
| Time2 × Parent | −0.01 | [−0.02, 0.01] | 0.01 | .449 | 0.00 | [−0.02, 0.02] | 0.01 | .947 |
| Average well-being after pandemic onset (T2 through T7) | ||||||||
| Intercept | 51.85 | [49.74, 53.96] | 1.08 | < .001 | 57.17 | [54.71, 59.62] | 1.25 | < .001 |
| Parent | 14.40 | [10.76, 18.05] | 1.86 | < .001 | 12.55 | [8.84, 16.27] | 1.89 | < .001 |
Note: CI = confidence interval; T1 = February 2020; T2 = March 2020; T7 = September 2020.
For these analyses, sample sizes were 654 for Sample A and 543 for Sample B.
Table 4.
Multilevel Models Predicting Ill-Being for Parents Living With Children (vs. a Comparison Group: Nonparents and Parents Not Living With Children)
| Predictor | Sample A (N = 656) | Sample B (N = 544) | ||||||
|---|---|---|---|---|---|---|---|---|
| b | 95% CI | SE | p | b | 95) CI | SE | p | |
| Change in ill-being during pandemic onset (T1 to T2)a | ||||||||
| Intercept | 34.40 | [32.53, 36.26] | 0.95 | < .001 | 32.31 | [30.22, 34.40] | 1.06 | < .011 |
| Time | 1.27 | [0.87, 1.67] | 0.20 | < .001 | 1.42 | [1.11, 1.74] | 0.16 | < .001 |
| Parent | −4.65 | [−7.85, −1.44] | 1.63 | .005 | –2.66 | [−5.83, 0.50] | 1.61 | .099 |
| Time × Parent | 1.37 | [0.70, 2.05] | 0.35 | < .001 | 0.12 | [−0.37, 0.60] | 0.25 | .631 |
| Linear change in ill-being after pandemic onset (T2 through T7) | ||||||||
| Intercept | 33.75 | [31.83, 35.67] | 0.98 | < .001 | 31.73 | [29.57, 33.90] | 1.10 | < .001 |
| Time | –0.24 | [−0.32, −0.16] | 0.04 | <.001 | –0.31 | [−0.39, −0.23] | 0.04 | < .001 |
| Parent | –5.18 | [−8.49, −1.87] | 1.69 | .002 | –2.17 | [−5.45, 1.11] | 1.67 | .194 |
| Time × Parent | –0.19 | [−0.33, −0.06] | 0.07 | .005 | –0.01 | [−0.14, 0.12] | 0.06 | .874 |
| Quadratic change in ill-being after pandemic onset (T2 through T7) | ||||||||
| Intercept | 32.74 | [30.76, 34.73] | 1.01 | < .001 | 30.43 | [28.17, 32.70] | 1.16 | < .001 |
| Time | –0.23 | [−0.30, −0.15] | 0.04 | < .001 | –0.29 | [0.38, −0.21] | 0.04 | < .001 |
| Time2 | 0.02 | [0.01, 0.03] | 0.01 | < .001 | 0.03 | [0.01, 0.03] | 0.01 | < .001 |
| Parent | –5.67 | [−9.10, −2.23] | 1.75 | .001 | –2.24 | [−5.68, 1.19] | 1.75 | .200 |
| Time × Parent | –0.19 | [−0.32, −0.05] | 0.07 | .006 | –0.01 | [−0.13, 0.11] | 0.06 | .916 |
| Time2 × Parent | 0.01 | [−0.01, 0.03] | 0.01 | .232 | 0.00 | [−0.01, 0.02] | 0.01 | .749 |
| Average ill-being after pandemic onset (T2 through T7) | ||||||||
| Intercept | 34.08 | [32.17, 36.00] | 0.98 | < .001 | 32.18 | [30.00, 34.35] | 1.11 | < .001 |
| Parent | –4.77 | [−8.07, −1.46] | 1.69 | .005 | –2.17 | [−5.47, 1.13] | 1.68 | .196 |
Note: CI = confidence interval; T1 = February 2020; T2 = March 2020; T7 = September 2020.
For these analyses, sample sizes were 654 for Sample A and 543 for Sample B.
For models examining partners, see Tables 5 and 6. In both samples, people living with a romantic partner experienced similar decreases in well-being compared with people not living with a romantic partner, FDR ps > .100. However, people living with partners experienced greater increases in ill-being in Sample A compared with people not living with a romantic partner (interaction: β = 1.03, 95% CI = [0.37, 1.68], FDR p = .010; although not in Sample B, interaction: β = 0.18, 95% CI = [−0.30, 0.67], FDR p = .774).
Table 5.
Multilevel Models Predicting Well-Being for People Living With a Partner (vs. a Comparison Group: People Not in a Romantic Relationship and People Not Living With Their Romantic Partners)
| Predictor | Sample A (N = 649) | Sample B (N = 544) | ||||||
|---|---|---|---|---|---|---|---|---|
| b | 95% CI | SE | p | b | 95% CI | SE | p | |
| Change in well-being during pandemic onset (T1 to T2)a | ||||||||
| Intercept | 51.85 | [49.56, 54.14] | 1.17 | < .001 | 55.65 | [52.94, 58.36] | 1.38 | < .001 |
| Time | −0.42 | [−0.78, −0.05] | 0.19 | .025 | –0.41 | [−0.65, −0.17] | 0.12 | .001 |
| Partner | 14.93 | [11.50, 18.35] | 1.74 | < .001 | 13.92 | [10.33, 17.51] | 1.83 | < .001 |
| Time × Partner | −0.57 | [−1.11, −0.03] | 0.28 | .037 | 0.18 | [−0.14, 0.51] | 0.16 | .273 |
| Linear change in well-being after pandemic onset (T2 through T7) | ||||||||
| Intercept | 49.77 | [47.45, 52.10] | 1.18 | < .001 | 54.82 | [52.02, 57.62] | 1.43 | < .001 |
| Time | −0.02 | [−0.10, 0.06] | 0.04 | .617 | 0.06 | [−0.03, 0.14] | 0.04 | .175 |
| Partner | 15.30 | [11.84, 18.76] | 1.76 | < .001 | 13.87 | [10.15, 17.58] | 1.89 | < .001 |
| Time × Partner | 0.08 | [−0.04, 0.19] | 0.06 | .199 | –0.02 | [−0.13, 0.09] | 0.05 | .689 |
| Quadratic change in well-being after pandemic onset (T2 through T7) | ||||||||
| Intercept | 49.31 | [46.87, 51.75] | 1.24 | < .001 | 54.66 | [51.69, 57.64] | 1.52 | < .001 |
| Time | −0.02 | [−0.10, 0.06] | 0.04 | .675 | 0.06 | [−0.02, 0.14] | 0.04 | .162 |
| Time2 | 0.01 | [−0.00, 0.02] | 0.01 | .130 | 0.00 | [−0.01, 0.02] | 0.01 | .676 |
| Partner | 15.73 | [12.11, 19.35] | 1.84 | < .001 | 13.79 | [9.86, 17.73] | 2.01 | < .001 |
| Time × Partner | 0.07 | [−0.04, 0.19] | 0.06 | .207 | –0.02 | [−0.12, 0.09] | 0.05 | .758 |
| Time2 × Partner | −0.01 | [−0.03, 0.01] | 0.01 | .331 | 0.00 | [−0.01, 0.02] | 0.01 | .788 |
| Average well-being after pandemic onset (T2 through T7) | ||||||||
| Intercept | 49.80 | [47.49, 52.11] | 1.18 | < .001 | 54.72 | [51.95, 57.50] | 1.41 | < .001 |
| Partner | 15.20 | [11.76, 18.64] | 1.75 | < .001 | 13.96 | [10.28, 17.65] | 1.88 | < .001 |
Note: CI = confidence interval; T1 = February 2020; T2 = March 2020; T7 = September 2020.
For these analyses, sample sizes were 647 for Sample A and 543 for Sample B.
Table 6.
Multilevel Models Predicting Ill-Being for People Living With a Partner (vs. a Comparison Group: People Not in a Romantic Relationship and People Not Living With Their Romantic Partners)
| Predictor | Sample A (N = 649) | Sample B (N = 544) | ||||||
|---|---|---|---|---|---|---|---|---|
| b | 95% CI | SE | p | b | 95% CI | SE | p | |
| Change in ill-being during pandemic onset (T1 to T2)a | ||||||||
| Intercept | 34.72 | [32.66, 36.77] | 1.05 | < .001 | 33.99 | [31.62, 36.36] | 1.21 | < .001 |
| Time | 1.29 | [0.85, 1.73] | 0.23 | < .001 | 1.37 | [1.01, 1.74] | 0.19 | < .001 |
| Partner | −4.52 | [−7.58, −1.45] | 1.56 | .004 | –5.02 | [−8.16, −1.87] | 1.60 | .002 |
| Time × Partner | 1.03 | [0.37, 1.68] | 0.33 | .002 | 0.18 | [−0.30, 0.67] | 0.25 | .455 |
| Linear change in ill-being after pandemic onset (T2 through T7) | ||||||||
| Intercept | 34.23 | [32.11, 36.35] | 1.08 | < .001 | 33.03 | [30.56, 35.50] | 1.26 | < .001 |
| Time | −0.25 | [−0.33, −0.16] | 0.05 | < .001 | –0.33 | [−0.43, −0.23] | 0.05 | < .001 |
| Partner | −5.13 | [−8.28, −1.99] | 1.60 | .001 | –3.95 | [−7.22, −0.67] | 1.67 | .018 |
| Time × Partner | −0.12 | [−0.25, 0.01] | 0.07 | .068 | 0.03 | [−0.10, 0.16] | 0.07 | .617 |
| Quadratic change in ill-being after pandemic onset (T2 through T7) | ||||||||
| Intercept | 33.24 | [31.04, 35.45] | 1.12 | < .001 | 31.78 | [29.17, 34.38] | 1.33 | < .001 |
| Time | −0.23 | [−0.32, −0.15] | 0.04 | < .001 | –0.31 | [−0.41, 0.21] | 0.05 | < .001 |
| Time2 | 0.02 | [0.01, 0.03] | 0.01 | < .001 | 0.03 | [0.01, 0.04] | 0.01 | < .001 |
| Partner | −5.52 | [−8.78, −2.26] | 1.66 | < .001 | –4.07 | [−7.50, −0.63] | 1.75 | .021 |
| Time × Partner | −0.11 | [−0.24, 0.01] | 0.06 | .081 | 0.03 | [−0.10, 0.15] | 0.06 | .690 |
| Time2 × Partner | 0.01 | [−0.01, 0.03] | 0.01 | .220 | 0.00 | [−0.02, 0.02] | 0.01 | .781 |
| Average ill-being after pandemic onset (T2 through T7) | ||||||||
| Intercept | 34.66 | [32.54, 36.77] | 1.08 | < .001 | 33.63 | [31.15, 36.11] | 1.26 | < .001 |
| Partner | −5.12 | [−8.27, −1.98] | 1.60 | .002 | –4.21 | [−7.51, −0.93] | 1.67 | .012 |
Note: CI = confidence interval; T1 = February 2020; T2 = March 2020; T7 = September 2020.
For these analyses, sample sizes were 647 for Sample A and 543 for Sample B.
Thus, parents living with children and people living with partners experienced similar declines in well-being at the onset of the pandemic when compared with their respective comparison groups. However, in one sample, parents living with children and people living with partners experienced particularly steep increases in ill-being at the onset of the pandemic. This pattern suggests that people living with close others may have been more severely affected by the onset of the pandemic—particularly with regard to symptoms of anxiety and depression—than people living without these close others. Although this pattern was replicated across parents living with children and people living with a romantic partner, this pattern was observed only in Sample A and thus may not represent a broadly generalizable pattern.
After pandemic onset
Across all participants, when considering rates of change across the first 6 months of the pandemic, well-being remained stable (FDR ps > .338 for linear and quadratic time), and ill-being followed a quadratic trajectory across those 6 months, first decreasing and then stabilizing near baseline levels (FDR ps < .008 for linear and quadratic time; for all statistics, see the Supplemental Material).
Considering well-being, we found that parents living with children experienced comparable rates of change in well-being in both samples compared with people not living with children (Table 3; interaction: FDR ps > .078). Likewise, people living with a romantic partner experienced comparable rates of change in well-being compared with people not living with a romantic partner (Table 5; interaction: FDR p > .381). Considering ill-being, we found that parents living with children experienced steeper decreases in ill-being compared with people not living with children in Sample A (Table 4; interaction: β = −0.19, 95% CI = [−0.33, −0.06], FDR p = .021; although not in Sample B, interaction: β = −0.01, 95% CI = [−0.14, 0.12], FDR p = .945). People living with a romantic partner experienced comparable rates of change in ill-being in both samples compared with people not living with a romantic partner (Table 5; interaction: FDR ps > .174). Thus, parents living with children and people living with partners experienced similar well-being trajectories compared with people living without these close others. Although parents living with children may have initially experienced greater ill-being at the onset of the pandemic in one sample, these results also suggest that their ill-being recovered more quickly than people living without children.
We also examined parents’ and partners’ average well-being and ill-being across the first 6 months of the pandemic. Considering well-being, we found that parents living with children experienced higher average well-being in both samples compared with people not living with children (Table 3; Sample A: β = 14.40, 95% CI = [10.76, 18.05], FDR p = .007; Sample B: β = 12.55, 95% CI = [8.84, 16.27], FDR p = .008). People living with a romantic partner also experienced higher average well-being in both samples compared with people not in a romantic relationship and people not living with a romantic partner (Table 5; Sample A: β = 15.20, 95% CI = [11.76, 18.64], FDR p = .007; Sample B: β = 13.96, 95% CI = [10.28, 17.65], FDR p = .008). When accounting for prepandemic levels of well-being, we found that the well-being difference between parents living with children and people not living with children remained suggestive in both samples (Sample A: uncorrected p = .046; Sample B: uncorrected p = .010), and the well-being difference between people living with a romantic partner and people not living with a romantic partner was marginal or suggestive (Sample A: uncorrected p = .054; Sample B: uncorrected p = .008). These results provide some evidence that people living with close others experienced uniquely better well-being during the pandemic that was not attributable to preexisting well-being differences.
Considering ill-being, we found that parents living with children experienced lower average ill-being in Sample A compared with people not living with children (Table 4; β = −4.77, 95% CI = [−8.07, −1.46], FDR p = .021; although not in Sample B: β = −2.17, 95% CI = [−5.47, 1.13], FDR p = .501). People living with a romantic partner also experienced lower ill-being in Sample A compared with people not living with a romantic partner (Table 6; β = −5.12, 95% CI = [−8.27, −1.98], FDR p = .010; suggestive in Sample B: β = −4.21, 95% CI = [−7.51, −0.93], FDR p = .079). Analyses adjusting for prepandemic ill-being suggest that ill-being differences between parents living with children and people living with a partner (vs. people who were not) after pandemic onset are likely attributable to preexisting differences for both parents (Sample A: uncorrected p = .443; Sample B: uncorrected p = .985) and partners (Sample A: uncorrected p = .918; Sample B: uncorrected p = .956).
Additional analyses (preregistered)
We conducted additional preregistered analyses to examine possible gender differences and interactions between living with one’s children and living with one’s romantic partner. We report key statistics for each of these analyses below (for all statistics, see the Supplemental Material).
Gender differences
To examine whether mental-health differences in parents living with children and people living with a partner (relative to people not living with children and people not living with a romantic partner) differentially predicted mental health for men compared with women, we tested for gender interactions in all primary models. The only statistically significant interaction (after FDR correction) was an interaction of being a parent living with children (vs. not being a parent living with children), time, and gender in predicting well-being in Sample A, β = 0.36, 95% CI = [0.11, 0.62], FDR p = .023, but this three-way interaction was not a significant predictor of ill-being in Sample A or of either well-being or ill-being in Sample B. Thus, we conclude that the results were largely similar for men and women.
Parent and partner status interactions
To examine whether there was an interaction between living with one’s children and living with one’s partner in predicting mental health, we repeated all primary models with the inclusion of an interaction between the parent and partner-status variables. No interactions were statistically significant after FDR correction (FDR ps > .100). Thus, people living with multiple close others do not appear to have particularly greater mental health compared with people living with only children or a romantic partner.
Additional analyses (not preregistered)
We also conducted additional exploratory analyses to determine whether parents of younger and/or more children experienced worse mental health than people living with older and/or fewer children and whether sociodemographic differences might account for our findings. In a final set of exploratory analyses, we leveraged the heterogeneous mix of people in the comparison groups (which consisted of people living alone and people living with others who were not romantic partners or children) to examine whether the mental-health benefits of living with close others also extended to living with other types of people (e.g., roommates) compared with living alone.
Child age and number of children
To determine whether parents living with younger and/or more children had worse mental health than people living with older and/or fewer children, we conducted exploratory analyses examining average child age and number of children as predictors of well-being and ill-being levels within the group of parents living with children. Child age was assessed only in Sample A, and in this sample, parents living with younger children had higher ill-being at baseline (β = −0.40, 95% CI = [−0.79, −0.02], uncorrected p = .041), but there were no differences in ill-being or well-being levels or change during the pandemic (uncorrected ps > .156). Number of children was assessed in both samples and was not associated with well-being or ill-being levels (at baseline or during the pandemic) or change in well-being or ill-being in either sample (uncorrected ps > .278). Thus, parents living with younger and/or more children did not experience worse mental health after the onset of the pandemic, although parents living with younger children did experience greater ill-being before the onset of the pandemic.
Sociodemographic differences
Given that there were sociodemographic differences between people living with close others (i.e., children and romantic partners) and our comparison groups in both samples (see Tables 1 and 2), we also conducted exploratory analyses that adjusted for these differences in each sample.
Specifically, in Sample A, the group of parents living with children included more older people and more women compared with people who were not living with children. Thus, we repeated all primary analyses in which parent status was a predictor of mental health while also adjusting for gender and age. Likewise, the group of people living with a romantic partner included more older people, more women, and more people of Republican political affiliation compared with people not living with a romantic partner. Thus, we repeated all primary analyses in which partner status was a predictor of mental health while also adjusting for gender, age, and political affiliation. The statistical significance and direction of all effects remained the same. Thus, our results in Sample A were largely consistent whether adjusting for sociodemographic differences or not, which suggests that sociodemographic differences are unlikely to explain the reported group differences.
In Sample B, the group of parents living with children differed by racial and ethnic identity and included more people of Republican political affiliation compared with people who were not living with children. Thus, we repeated all primary analyses in which parent status was a predictor of mental health while also adjusting for racial and ethnic identity and political affiliation. Likewise, the group of people living with a romantic partner differed by racial and ethnic identity and included more people of Republican political affiliation compared with people not living with a romantic partner. Thus, we repeated all primary analyses in which partner status was a predictor of mental health while also adjusting for racial and ethnic identity and political affiliation. The statistical significance and direction of effects remained the same for all primary analyses. Thus, our results in Sample B were also consistent when adjusting for sociodemographic differences, again suggesting that sociodemographic differences are unlikely to account for the reported group differences.
Living with others compared with living alone
To better understand whether people living with other people (but not children or a partner) also experienced better mental health compared with people living alone, we compared people who consistently reported living alone with people who reported at least once that they were living with housemates other than children and partners (e.g., roommates). The two subgroups did not differ from one another with regard to well-being or ill-being (uncorrected ps > .119). This suggests that the mental health of people living with others (but not children or partners) was comparable with people living alone and was still worse than the mental health of people living with children or romantic partners.
Discussion
The current research bridges social psychological science with clinical psychological science to address mixed findings and theoretical predictions regarding mental health during the COVID-19 pandemic. Specifically, research from other crises has shown that close relationships may jeopardize mental health in response to harrowing experiences (e.g., Pietromonaco & Overall, 2021). However, our findings add to a large body of research that instead highlights the benefits of close relationships for mental health (e.g., Holt-Lunstad et al., 2010; Lemay & Neal, 2014) and demonstrates these benefits even amid intense and ongoing life disruptions caused by a major stressor like COVID-19.
Our unique longitudinal approach allowed us to examine not only the mental health of people living with close others during the pandemic but also prepandemic mental health. Across two diverse samples, we found that people living with close others experienced substantially greater well-being and lower ill-being both before the pandemic and across the first 6 months of the pandemic. When considering well-being in particular, these benefits persisted even when accounting for prepandemic levels of well-being. Together, these results suggest that living with close others may crucially protect mental health both in general and during a global crisis. Thus, people living without these close others are at risk for poorer mental health both within and outside of the COVID-19 context and may need the most support.
It is important to note that all groups experienced declines in mental health at the onset of the pandemic. Thus, these findings do not suggest that people living with close others do not need societal support. Indeed, some evidence suggests that although parents living with children recovered faster than the comparison groups, people living with close others (children and/or parents) experienced uniquely steeper decreases in mental health during the onset of the pandemic. This result is in line with some initial evidence that suggests that parents living with children may have experienced increased stress surrounding child-care duties (American Psychological Association, 2020) and that the pandemic may have led to romantic couples experiencing greater conflict (e.g., Stroh, 2020). In addition, parents’ uniquely quick mental-health recovery over the next 6 months may have been due in part to societal support mechanisms available to families (e.g., the Coronavirus Aid, Relief, and Economic Security [CARES] Act), which could have helped them weather COVID-19-related challenges more effectively. These recovery findings are also in line with relational regulation theorizing that suggests that everyday interactions with close others—in addition to actual support behaviors—bolster the mental health of people in close relationships (Lakey & Orehek, 2011).
We also note substantial variability in mental health within each of our analysis groups, which indicates that some people were experiencing poor mental health in all groups. Thus, although our results highlight the greater mental health of people living with close others, they also highlight the continued need for support for people from all walks of life facing the COVID-19 pandemic and future global stressors.
Despite the strengths of our longitudinal approach, this study has several limitations that highlight avenues for future research. First, future work is needed to examine the underlying mechanisms that may explain why people living with close others experienced better mental health than people who were not. For example, increased emotional support from close others or feelings of companionship may drive these patterns.
Second, although our U.S. samples are diverse regarding racial and ethnic identity, political ideology, gender, and age, these findings may not reflect the experiences of people in cultural contexts outside the United States. Thus, empirical research on samples from other countries would help to elucidate and further the generalizability of these findings.
Third, we observed some inconsistent results across the two samples. For example, parents living with children and people living with a romantic partner experienced steeper decreases in mental health at pandemic onset only in Sample A, the relatively diverse sample with respect to racial and ethnic identity (but not Sample B, the relatively politically diverse sample). Thus, these findings should be interpreted with caution, and further investigation into the mental health of people living with and without close others surrounding the onset of major stressors is needed to determine the robustness of these findings. Although we examined whether sociodemographic differences in our samples may explain our findings—and did not find any consistent evidence for this—it remains possible that different intersecting identities (e.g., the interplay between one’s gender, age, and racial or ethnic identity) could still play a role in explaining our reported group differences or the few inconsistencies across samples. Thus, future research would benefit from continuing to study mental health in the context of widespread global stressors in large, sociodemographically diverse samples.
Finally, although our research examined mental-health differences among people living with close others (vs. people who were not) before the pandemic and across its first 6 months and thus provides cross-sectional and longitudinal evidence for these differences, we cannot discern whether living with close others caused these differences in mental health in our data. Alternatively, better mental health may play a causal role in who is more likely to live with close others. Empirical evidence supports both causal pathways—that close relationships promote mental health (e.g., Holt-Lunstad et al., 2010) and that mental health promotes close relationships (e.g., Fowler & Gasiorek, 2017). Given these patterns, it is likely that the complex association between close relationships and mental health is bidirectional (Braithwaite & Holt-Lunstad, 2017). In line with the protective benefits of living with close others, some evidence suggests that close relationships exert more influence on mental health than vice versa (Braithwaite & Holt-Lunstad, 2017). However, additional long-term longitudinal and experimental (when possible) evidence is needed to further elucidate these causal pathways.
Overall, our research provides a novel and rigorous longitudinal examination of the mental health of people living with close others before, during, and after the onset of the pandemic. The mental health of parents living with children and people living with partners was greater than people who were not, but people from all walks of life have been affected by this crisis and may benefit from mental-health support.
Supplemental Material
Supplemental material, sj-pdf-1-cpx-10.1177_21677026211053320 for The Benefits of Living With Close Others: A Longitudinal Examination of Mental Health Before and During a Global Stressor by Natalie M. Sisson, Emily C. Willroth, Bonnie M. Le and Brett Q. Ford in Clinical Psychological Science
In attrition analyses (not preregistered), we examined whether mental health differed in people who dropped out of the study after the onset of the pandemic (i.e., after T2) compared with people who did not drop out of the study. These groups did not differ in T2 well-being or ill-being in either of the two different samples, which suggests that the results summarized here cannot be attributed to people whose mental health was more affected by the pandemic being more likely to stay in the study. However, for full transparency, we also note that people who dropped out of the study after the first time point (T1)—who we preregistered to exclude from the present analyses because they did not provide at least one longitudinal measure of mental health—did report poorer mental health at T1 than people who completed at least one additional time point of the study.
Sample B was originally recruited in February (2020) for a different study centered on politics (N = 842). In March, these participants were invited to join the COVID-19-pandemic-centered study, and this subsample is the focus of the present study (N = 544).
After collecting data from February 2020 through September 2020, we preregistered a plan to analyze those data in September 2020. We continued to collect data on an approximately monthly basis. Following the same procedure as in the currently reported analyses, we conducted additional analyses in February 2021 that included data from February 2020 to January 2021. After running these analyses, we collected data from two more times (March and April 2021), but we have not tested models including these data given that this time was marked by widespread vaccination and likely represents a qualitative shift in the pandemic context. Given that all the patterns regarding mental health in these new analyses replicated the patterns in the preregistered analyses, we focus here on our preregistered analysis plan to include data from February 2020 to September 2020.
Footnotes
ORCID iDs: Natalie M. Sisson  https://orcid.org/0000-0003-0758-3803
https://orcid.org/0000-0003-0758-3803
Bonnie M. Le  https://orcid.org/0000-0002-1857-6716
https://orcid.org/0000-0002-1857-6716
Brett Q. Ford  https://orcid.org/0000-0002-7943-4447
https://orcid.org/0000-0002-7943-4447
Supplemental Material: Additional supporting information can be found at http://journals.sagepub.com/doi/suppl/10.1177/21677026211053320
Transparency.
Action Editor: Darby Saxbe
Editor: Jennifer L. Tackett
Author Contributions
B. Q. Ford and N. M. Sisson designed the research study. All of the authors designed the preregistration and analysis plan. N. M. Sisson and E. C. Willroth analyzed the data and wrote the first draft. All of the authors contributed to draft revisions and approved the final manuscript for submission.
The author(s) declared that there were no conflicts of interest with respect to the authorship or the publication of this article.
Funding: This research was funded by a Social Sciences and Humanities Research Council Insight Grant, a PEACE Grant from the Mind & Life Institute, and a University of Toronto COVID-19 Student Engagement Award (all awarded to B. Q. Ford).
Open Practices: All data and materials have been made publicly available via OSF and can be accessed at https://osf.io/pcyeg. The design and analysis plans for the experiments were preregistered at OSF and can be accessed at https://osf.io/pcyeg. This article has received badges for Open Data, Open Materials, and Preregistration. More information about the Open Practices badges can be found at https://www.psychologicalscience.org/publications/badges.



References
- American Psychological Association. (2020, May). Stress in America 2020: Stress in the time of COVID-19, volume one [Press release]. https://www.apa.org/news/press/releases/stress/2020/report
- Benjamini Y., Hochberg Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society B: Methodological, 57, 289–300. [Google Scholar]
- Braithwaite S., Holt-Lunstad J. (2017). Romantic relationships and mental health. Current Opinion in Psychology, 13, 120–125. [DOI] [PubMed] [Google Scholar]
- Calarco J. M., Anderson E., Meanwell E. V., Knopf A. (2020, October 4). “Let’s not pretend it’s fun”: How COVID-19-related school and childcare closures are damaging mothers’ well-being. SocArXiv. 10.31235/osf.io/jyvk4 [DOI]
- Chung G., Chan X., Lanier P., Ju P. W. Y. (2020, June 25). Associations between work-family balance, parenting stress, and marital conflicts during COVID-19 pandemic in Singapore. PsyArXiv. 10.31219/osf.io/nz9s8 [DOI] [PMC free article] [PubMed]
- Cohan C. L. (2010). Family transitions following natural and terrorist disaster: Hurricane Hugo and the September 11 terrorist attack. In Miller T. W. (Ed.), Handbook of stressful transitions across the lifespan (pp. 149–164). Springer Science + Business Media. [Google Scholar]
- Cohen P., Cohen J., Aiken L. S., West S. G. (1999). The problem of units and the circumstance for POMP. Multivariate Behavioral Research, 34, 315–346. [Google Scholar]
- Cohen S. (2004). Social relationships and health. American Psychologist, 59, 676–684. [DOI] [PubMed] [Google Scholar]
- Craig L., Churchill B. (2021). Dual-earner parent couples’ work and care during COVID-19. Gender, Work & Organization, 28, 514–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener E., Emmons R. A., Larsen R. J., Griffin S. (1985). The satisfaction with life scale. Journal of Personality Assessment, 49, 71–75. [DOI] [PubMed] [Google Scholar]
- Diener E., Seligman M. E. P. (2002). Very happy people. Psychological Science, 13(1), 81–84. 10.1111/1467-9280.00415 [DOI] [PubMed] [Google Scholar]
- Elmer T., Mepham K., Stadtfeld C. (2020). Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLOS ONE, 15, Article e0236337. 10.1371/journal.pone.0236337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontanesi L., Marchetti D., Mazza C., Di Giandomenico S., Roma P., Verrocchio M. C. (2020). The effect of the COVID-19 lockdown on parents: A call to adopt urgent measures. Psychological Trauma: Theory, Research, Practice, and Policy, 12, S79–S81. [DOI] [PubMed] [Google Scholar]
- Fowler C., Gasiorek J. (2017). Depressive symptoms, excessive reassurance seeking, and relationship maintenance. Journal of Social and Personal Relationships, 34, 91–113. [Google Scholar]
- Grose J. (2020, September 9). The pandemic is a ‘mental health crisis’ for parents. The New York Times. https://www.nytimes.com/2020/09/09/parenting/mental-health-parents-coronavirus.html
- Harper J. M., Schaalje B. G., Sandberg J. G. (2000). Daily hassles, intimacy, and marital quality in later life marriages. American Journal of Family Therapy, 28, 1–18. [Google Scholar]
- Holt-Lunstad J., Smith T. B., Layton J. B. (2010). Social relationships and mortality risk: A meta-analytic review. PLOS Medicine, 7(7), Article e1000316. 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakubiak B. K., Feeney B. C. (2019). Interpersonal touch as a resource to facilitate positive personal and relational outcomes during stress discussions. Journal of Social and Personal Relationships, 36, 2918–2936. [Google Scholar]
- Keyes C. L. M. (2007). Promoting and protecting mental health as flourishing: A complementary strategy for improving national mental health. American Psychologist, 62, 95–108. [DOI] [PubMed] [Google Scholar]
- Lakey B., Orehek E. (2011). Relational regulation theory: A new approach to explain the link between perceived social support and mental health. Psychological Review, 118, 482–495. [DOI] [PubMed] [Google Scholar]
- Lemay E. P., Neal A. M. (2014). Accurate and biased perceptions of responsive support predict well-being. Motivation and Emotion, 38, 270–286. [Google Scholar]
- Luetke M., Hensel D., Herbenick D., Rosenberg M. (2020). Romantic relationship conflict due to the COVID-19 pandemic and changes in intimate and sexual behaviors in a nationally representative sample of American adults. Journal of Sex & Marital Therapy, 46, 1–16. [DOI] [PubMed] [Google Scholar]
- Neff L. A., Karney B. R. (2004). How does context affect intimate relationships? Linking external stress and cognitive processes within marriage. Personality and Social Psychology Bulletin, 30, 134–148. [DOI] [PubMed] [Google Scholar]
- Nelson S. K., Kushlev K., English T., Dunn E. W., Lyubomirsky S. (2013). In defense of parenthood: Children are associated with more joy than misery. Psychological Science, 24, 3–10. [DOI] [PubMed] [Google Scholar]
- Nelson S. K., Kushlev K., Lyubomirsky S. (2014). The pains and pleasures of parenting: When, why, and how is parenthood associated with more or less well-being? Psychological Bulletin, 140, 846–895. [DOI] [PubMed] [Google Scholar]
- Pietromonaco P. R., Collins N. L. (2017). Interpersonal mechanisms linking close relationships to health. American Psychologist, 72, 531–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietromonaco P. R., Overall N. C. (2021). Applying relationship science to evaluate how the COVID-19 pandemic may impact couples’ relationships. American Psychologist, 76(3), 438–450. 10.1037/amp0000714 [DOI] [PubMed] [Google Scholar]
- Pinheiro J., Bates D., DebRoy S., Sarkar D., & R Core Team. (2020). nlme: Linear and nonlinear mixed effects models [Computer software] (Version 3.1-151). Comprehensive R Archive Network. https://cran.r-project.org/package=nlme [Google Scholar]
- Prasso S. (2020, March 31). China’s divorce spike is a warning to the rest of the locked-down world. Bloomberg Businessweek. https://www.bloomberg.com/news/articles/2020-03-31/divorces-spike-in-china-after-coronavirus-quarantines
- Prime H., Wade M., Browne D. T. (2020). Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist, 75, 631–643. [DOI] [PubMed] [Google Scholar]
- Proulx C. M., Helms H. M., Buehler C. (2007). Marital quality and personal well-being: A meta-analysis. Journal of Marriage and Family, 69, 576–593. [Google Scholar]
- Radloff L. (1977). The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- R Core Team. (2019). R: A language and environment for statistical computing (Version 3.6.1) [Computer software]. R Foundation for Statistical Computing. http://www.R-project.org [Google Scholar]
- Steger M. F., Frazier P., Oishi S., Kaler M. (2006). The meaning in life questionnaire: Assessing the presence of and search for meaning in life. Journal of Counseling Psychology, 53, 80–93. [Google Scholar]
- Stroh P. (2020, November 18). Pandemic ‘pressure cooker’ is driving more couples to seek advice about separation, divorce: Family lawyers report increase in calls seeking help to dissolve relationships. Canadian Broadcasting Corporation. https://www.cbc.ca/news/canada/covid-19-panemic-divorce-rates-1.5795625 [Google Scholar]
- Torchiano M. (2020). effsize: Efficient effect size computation [Computer software] (Version 0.8.1). Comprehensive R Archive Network. https://cran.r-project.org/package=effsize [Google Scholar]
- U.S. Centers for Disease Control and Prevention. (2020). Covid-19: Preventing getting sick. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/index.html
- Whisman M. A. (2001). The association between depression and marital dissatisfaction. In Beach S. R. H. (Ed.), Marital and family processes in depression: A scientific foundation for clinical practice (pp. 3–24). American Psychological Association. [Google Scholar]
- Zigmond A. S., Snaith R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatry Scandinavica, 67, 361–370. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-cpx-10.1177_21677026211053320 for The Benefits of Living With Close Others: A Longitudinal Examination of Mental Health Before and During a Global Stressor by Natalie M. Sisson, Emily C. Willroth, Bonnie M. Le and Brett Q. Ford in Clinical Psychological Science