Background:
Percutaneous nephrostomy (PCN) and Double J stenting (DJS) are the 2 main treatment options of ureteral obstruction. We evaluate which of these 2 methods is superior concerning the course of procedure, postoperative complication and quality of life.
Methods:
A detailed review of electronic databases including PubMed, Embase, Cochrane Library, China Biology Medicine disc, China National Knowledge Infrastructure up to February 21st, 2021 was searched. Continuous data were evaluated using mean difference (MD) with 95% confidence interval (CI), while nominal data were analyzed by risk ratio (RR) with 95% CI. Meanwhile, we performed the subgroup analysis based on study design, disease type, sample size, sepsis, DJ diameter, nephrostomy diameter, anesthesia type and guidance under X-ray or ultrasound.
Results:
There were 18 previous studies included in current study. As a result, we found that there were significant differences in fluoroscopy time (MD = 0.31; 95% CI, 0.14–0.48, P < .001) and hospital stay (MD = 1.23; 95% CI, 0.60–1.85, P < .001). However, no statistic difference was detected in operative time (MD = 5.40; 95% CI, −1.78 to 12.58, P = .140) between the paired groups. Although DJS showed a higher rate of postoperative complications (25.19% vs 17.61%), there was no significant difference in the incidence of complications following DJS and PCN (RR = 0.92; 95% CI, 0.60–1.43; P = .720). Based on the EuroQol analysis, the 2 main treatment options had different impacts on quality of life. The pooled results showed that PCN patients reported more difficulties in self-care compared to DJS patients (RR = 3.07; 95% CI, 1.32–7.14; P = .009).
Conclusions:
DJS is a safe and better method of temporary urinary diversion than PCN for management of ureteral obstruction with shorter fluoroscopy time and hospital stay. As for quality of life, patients receiving PCN had a distinct difficulty in self-care compared to those receiving DJS. However, these 2 treatment options often depends on the individual situation.
Keywords: meta-analysis, percutaneous nephrostomy, systematic review, ureteral obstruction, ureteral stents
1. Introduction
Ureteral obstruction is one of the most common clinical problems, with etiologies ranging from upper urinary calculi to strictures secondary to operation and tumor invasion.[1] Effective treatment should be performed immediately as long-term obstruction may result in pain, infection, and ultimately renal failure. Active management can relieve the suffering of patients, protect the renal function and improve quality of life, even prolong cancer prognosis.[2] To date, the existing options for ureteral obstruction are diverse, including percutaneous nephrostomy (PCN) or Double J stenting (DJS), with or without eventual antegrade stent insertion.[3,4] However, we are often confronted with the dilemma of which PCN or DJS is a better method for ureteral obstruction in practice.
Currently, there are no clear guidelines regarding ideal treatment for ureteral obstruction. DJS placement is generally considered the preferred method for alleviating hydronephrosis secondary to ureteral obstruction, but it is difficult for cancer patients under some circumstances. Meanwhile, PCN can also cause many complications, which reduces the patient quality of life. Therefore, the best treatment for patients with ureteral obstruction is still unclear.
It is important to evaluate the superiority of PCN versus DJS for ureteral obstruction. Meta-analysis is a statistical and epidemiological tool that incorporates all available data to get a relatively accurate result.[5] Therefore, we assess which of the 2 main methods is superior for patients with ureteral obstruction concerning the course of procedure, postoperative complication and quality of life.
2. Methods
2.1. Search strategy
A detailed review of English and Chinese literature was conducted from PubMed, Embase, Cochrane Library, China Biology Medicine disc, China National Knowledge Infrastructure, using the terms (“Nephrostomies” or “Percutaneous Nephrostomies” or “percutaneous nephrostomy” or “nephrostomy” or “PCN” or “nephrostom”) and (“Stents ” or “stent” or “stents” or “stenting” or “DJS” or “ureteral stent” or “double j” or “JJ” or “Double j”). The literature search was last updated on February 21st, 2021. No limits were applied to language, publication date, or publication status. Reference lists of relevant systematic reviews and meta-analyses were reviewed to ensure completeness of data acquisition.The preferred reporting items for systematic reviews and meta-analyses was cited in this meta-analysis.[6] In addition, the ethical approval was not applied in current study because there was no patient’s privacy or clinical samples.
2.2. Inclusion and exclusion criteria
Relevant studies should meet the following criteria before being included: the comparative studies that compare the efficacy of PCN versus DJS for ureteral obstruction; the studies provided available data; As per the exclusion criteria: no analysis data; studies involved cell lines and/or animals; similar or duplicate study; reviews, case reports, letters.
2.3. Data extraction
After searching of the mentioned databases, 2 authors (Zhang KP and Zhang Y) screened the titles and abstracts of the reminded references independently. Any disagreement was resolved upon discussion by a third author (Chao M) and reaching consensus. The full texts of relevant articles were reviewed to assess the eligibility criteria. We extracted the relevant information including author, publication year, age, study design, disease type, no of patients, follow-up time, sepsis, DJ diameter, nephrostomy diameter, anesthesia type, guidance under X-ray or ultrasound and conclusions. Primary outcomes contained the fluoroscopy time, procedures time, hospital stay, no of complications and data of life quality between the paired groups. Moreover, we performed subgroup analysis based on sample sizes (≥50 vs <50), study design (retrospective vs prospective study), sepsis (septic vs non-septic), DJ diameter (<6F vs >5F), nephrostomy diameter (<12 F vs >11F), anesthesia type (local vs general) and guidance under X-ray or ultrasound. In addition, the standardized Clavien-Dindo classification of surgical complications is introduced in current study as a simple and widely widely used tool to assess and report postoperative complications.[7]
2.4. Statistical analysis
We analyzed these data by using Review Manager 5.3 (Cochrane Collaboration, Oxford, UK) and STATA 12.0 software (Stata Corpotation, College Station, TX). For accurate assessment of continuous data, mean-standard deviation and parametric tests were used. Nominal data were extracted as risk ratio (RR). Mean difference (MD) (95% confidence interval [CI]) or RR (95% CI) was obtained for assessing the efficacy of PCN and DJS for ureteral obstruction. Meanwhile, the Q statistics and I2 test were applied to calculate the heterogeneity of eligible study. P < .05 and/or I2 > 50% was considered as statistically heterogeneous, and the random effects (DerSimonian and Laird method) model was used to analyze the results.[8,9] Otherwise, the fixed effects (Mantel-Haenszel method) model was applied.[10] The stability of the results was assessed by applying one-way sensitivity analyses, which individually removed studies in meta-analysis to explore the impact of each study on the pooled RR. Potential publication biases were assessed by the Begg’s funnel plots in which the log RR was plotted against its standard error. P < .05 by Begg’s funnel plots was considered as a statistically significant publication bias. Additionally, we classified studies into different subgroups, including study design, disease type, sample size, sepsis, DJ diameter, nephrostomy diameter, anesthesia type and guidance under X-ray or ultrasound.
3. Results
3.1. Study characteristics
After searching of the databases, we roughly screened the titles and abstracts, and then obtained the full text. 76 potentially relevant studies were further evaluated. According to inclusion and exclusion criteria, totally 18 studies were included for pooled analyses.[11–28] (Fig. 1). The main study characteristics were presented in Table 1. Of 3 studies,[14,17,24] insertion of a DJS was regarded as the primary intervention. If it failed, subsequent PCN tube placement was required. The failed rates of DJS and PCN were 3% (19/624) and 14.7% (113/769) in the primary intervention, respectively.
Figure 1.
Flow diagram of the study selection process in the meta-analysis.
Table 1.
Summary of studies characteristics included in the meta-analysis.
| Author | Year | Study design | Age | Disease type | Nephrostomy | Complications | Stent | Complications | Follow-up | Nesthesia | Sepsis | DJ diameter | Nephrostomy diameter | Ultrasound or X-ray | Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ahmad I | 2013 | Retrospective study (2010–2011) | 40 ± 10.35; 43 ± 9.65 | Obstructive uropathy | 200 | Fever; septicemia; bleeding; hematuria; PCN dislodgement | 100 | Fever; septicemia; bleeding; pain; ureteral perforation; migration; encrustation | 15 days to 3 months | Local | Non-septic | 5–6F | 8F | Ultrasound | PCN is a safe and better method than double J stenting with lower incidence of complications |
| de Sousa Morais N | 2018 | Prospective cohort study (2017) | 63.1 ± 12.5; 54.5 ± 15.5 | Ureteric calculi | 18 | / | 32 | / | / | / | Non-septic | / | / | / | PCN was associated with a higher rate of spontaneous stone, and fewer urinary symptoms |
| Elbatanouny AM | 2020 | Prospective randomized study (2017–2019) | 48.6 ± 12.5; 51 ± 11.7 | Kidney stone | 71 | Fever; sepsis; hematuria; slippage; leakage; urgency; dysuria; pain | 72 | Fever; sepsis; hematuria; slippage; urgency; urge incontinence; dysuria; pain | / | Local | Non-septic | 6F | 10F | X-ray | PCN facilitates subsequent percutaneous nephrolithotomy, and a JJ stent facilitates subsequent ureteroscopy |
| ElSheemy MS | 2015 | Prospective randomized study (2011–2013) | 4.78 ± 2.295; 4.07 ± 2.093 | Ureteral calculi | 45 | Hematuria; leakage; febrile UTI; PCN Slippage | 45 | Febrile UTI; mucosal complications | / | General | Non-septic | 5–6F | 6–8F | X-ray | JJ was an initial urinary drainage in stones prepared for chemolytic dissolution or ESWL. PCN is considered if the stone size is >2 cm |
| Feng MI | 1999 | Retrospective study (1984–1996) | (37–85) | Pelvic malignancy | 9 | Stent replacement | 22 | Intractable pain | 2 weeks to 7 years | / | Non-septic | 6–7F | 18F | / | Antegrade drainage should be considered initially in patients who are likely to fail internal drainage |
| Joshi HB | 2001 | Prospective nonrandomized study | 56 ± 9; 55 ± 14 | Obstructing ureteral stones | 13 | Four urinary symptoms | 21 | Four urinary symptoms | / | Local/general | Non-septic | 6F | 8.3F | X-ray | Patients with “JJ” stents have more irritative urinary symptoms and a high chance of local discomfort than patients with nephrostomy tubes |
| Ku JH | 2004 | Retrospective study (2000–2002) | 57.3 (20–84) | Malignant ureteral obstruction | 80 | Fever, pyelonephritis | 68 | Fever, pyelonephritis | 1 to 42 months | / | Non-septic | 7–8F | / | / | Morbidities after internal or external diversion were minimal in cases of malignant obstruction |
| Mokhmalji H | 2001 | Prospective randomized study (1996–1998) | 55; 49 | Hydronephrosis caused by stones | 20 | Fever | 20 | Fever | / | Local | Septic | / | 12F | X-ray | Percutaneous nephrostomy is superior to ureteral stents for diversion of hydronephrosis caused by stones |
| Monsky WL | 2013 | Prospective survey | / | Malignant ureteral obstruction | 16 | Dislodged; pain; infection; clogged; leak | 15 | Dislodged; pain; infection; fistula | 16 months | Local/general | Non-septic | 8F | 8F | X-ray | A greater incidence of pain in those receiving double J stents and more frequent tube changes in those with nephrostomy tubes should be considered |
| Pearle MS | 1998 | Prospective randomized study (1995–1997) | 41.3 ± 13.0; 41.3 ± 14.5 | Ureteral calculi | 21 | PCN dislodgement | 21 | / | / | Local/general | Septic | 6–7F | 8–12F | X-ray | Both effectively relieve obstruction. Neither modality demonstrated superiority in promoting a more rapid recovery |
| Rammohan T | 2015 | Randomized prospective study (2012–2014) | 25–65 | Ureteral or renal pelvic stones | 20 | / | 20 | / | / | Local | Septic | 4.5–5F | 12F | X-ray | No significant difference in the efficacy of relieving obstruction/symptoms in either procedure |
| Shoshany O | 2019 | Prospective bi-centered study | 54 (46.5–61); 55 (39–70.5) | Acute ureteral obstruction | 30 | Procedural complication | 45 | Procedural complication | 2 yr | Local/general | Non-septic | 6F | 8.5F | X-ray | The 2 techniques had a distinct different impact on quality of life |
| Song Y | 2011 | Retrospective study (2006–2010) | 55.9 ± 7.7; 58.3 ± 15.3 | Gynecological malignancies | 25 | Fever; flank pain; urinary tract infection | 50 | Fever; flank pain; urinary tract infection | / | Local | Non-septic | / | / | X-ray | ureteral stenting is a first-line option for managing ureteral obstruction caused by gynecologic malignancies |
| Song Y | 2013 | Retrospective study (2001–2012) | 26.9; 27.2 | Ureteral calculi during pregnancy | 16 | Skin infection; hematuria; tube obstruction | 17 | Retained and encrusted stent; pain; bladder irritation; stent replacement | / | Local | Non-septic | / | / | ultrasound | Ureteroscopic lithotripsy was found to be an effective intervention during pregnancy |
| Tan ST | 2019 | Retrospective study (2008–2018) | 50.3 (25–78) | Cervical cancer | 29 | Catheter dislocation; hematuria; waist discomfort | 60 | Stent retraction; stent falling into the bladder | / | Local | Non-septic | / | / | X-ray | Ureteral stent placement is the preferred method for the treatment of hydronephrosis secondary to cervical cancer |
| Tiago KT | 2018 | Retrospective study (2012–2018) | 65.6 ± 9.5 | Malignant uropathy | 15 | Minor complication | 26 | Minor complications | 30 d | General | Non-septic | 5–6F | 10F | X-ray | JJ stenting is a suitable alternative in patients with malignant ureteral obstruction, providing signifcant cost savings and high success rates |
| Xu ZH | 2021 | Randomized study (2019–2020) | 65 (49–72); 64.5 (54–70) | Acute urinary tract obstruction | 35 | No complication | 30 | No complication | / | Local | Septic | / | / | Ultrasound | PCN had a better outcome than RUS in emergency drainage with urosepsis, especially for patients with severe inflammation and fever |
| Yoshimura K | 2005 | Retrospective study (1994–2003) | 67.3 ± 15.7; 59.5 ± 17.4 | Urosepsis with urinary calculi | 24 | / | 35 | / | / | / | Septic | / | / | / | The frequency of emergency drainage in elderly patients with poor performance status has increased in recent years |
DJS = DJ stenting, ESWL = extracorporeal shock wave lithotripsy, PCN = percutaneous nephrostomy, UT = urinary tract infection.
3.2. Operative time, fluoroscopy time and hospital stay
We found that there were 7, 5 and 4 studies explored the operative time,[11,14,22,24–27] fluoroscopy time[11,16,22,26,27] and hospital stay,[14,20,22,24] respectively. The pooled results showed significant differences in fluoroscopy time (MD = 0.31; 95% CI, 0.14–0.48, P < .001) and hospital stay (MD = 1.23; 95% CI, 0.60–1.85, P < .001). It indicated that PCN patients had shorter fluoroscopy time and hospital stay than DJS patients. However, no significant difference was explored in operative time of the paired group (MD = 5.40; 95% CI, −1.78 to 12.58, P = .140). The forest plot was shown in Figure 2. In addition, a significant heterogeneity was found in the group of hospital stay and operative time (86% and 98%). We performed the subgroup analysis based on study design, disease type sample size, sepsis, DJ diameter, nephrostomy diameter, anesthesia type and guidance under X-ray or ultrasound. As shown in Table 2, a positive result was explored in the subgroup of hospital stay (retrospective: MD = 1.21; 95% CI, 0.54–1.89, P = .000; malignant: MD = 1.30; 95% CI, 0.91–1.70, P = .000; sample size > 50: MD = 1.21; 95% CI, 0.54–1.89, P = .000; septic: MD = 4.50; 95% CI, 1.02–7.98, P = .011; nephrostomy diameter > 11F: MD = 4.05; 95% CI, 0.50–7.60, P = .025; X-ray: MD = 1.30; 95% CI, 0.96–1.66, P = .000). Meanwhile, there was a statistic difference in the subgroup of operative time (non-septic: MD = 1.30; 95% CI, 0.91–1.70, P = .000; local: MD = 1.30; 95% CI, 0.91–1.70, P = .000).
Figure 2.
Forest plot of data on fluoroscopy time, hospital stay and operative time (A: fluoroscopy time; B: hospital stay; C: operative time). 95% CI = 95% confidence interval, DJS = double J stenting, PCN = percutaneous nephrostomy.
Table 2.
Stratified analysis of the hospital stay, operative time and postoperative complications between the paired group.
| Categories | Subgroups | Hospital Stay | Operative time | Complication | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| MD (95%CI) | P | I 2 | MD (95%CI) | P | I 2 | RR (95%CI) | P | I 2 | ||
| Study design | Prospective | 1.30 (−0.68 to 3.28) | 0.199 | / | 0.38 (−6.37 to 7.14) | 0.912 | 96.4% | 1.11 (0.67–1.81) | 0.691 | 0 |
| Retrospective | 1.21 (0.54–1.89) | 0.000 | 90.7% | 10.31 (−2.14 to 23.03) | 0.112 | 97% | 0.86 (0.49–1.53) | 0.611 | 75.7% | |
| Disease type | Benign | −8.04 (−27.60 to 11.52) | 0.420 | 92.9% | 0.38 (−6.37 to 7.14) | 0.912 | 96.4% | 0.75 (0.41–1.39) | 0.366 | 61.5% |
| Malignant | 1.30 (0.91–1.70) | 0.000 | 85.4% | 10.31 (−2.14 to 23.03) | 0.112 | 97% | 1.09 (0.79–1.51) | 0.600 | 34.5% | |
| Sample size | <50 | 1.30 (−0.68 to 3.28) | 0.199 | / | 2.45 (−4.57 to 9.46) | 0.494 | 77.8% | 1.34 (0.83–2.17) | 0.236 | 19.6% |
| >50 | 1.21 (0.54–1.89) | 0.000 | 86.1% | 6.39 (−3.77 to 16.55) | 0.218 | 98.9% | 0.73 (0.42–1.28) | 0.274 | 76.6% | |
| Sepsis | Septic | 4.50 (1.02–7.98) | 0.011 | 41.5% | −8.04 (−27.60 to 11.52) | 0.420 | 92.9% | 1.63 (0.79–3.32) | 0.184 | 0.0% |
| Non-septic | 4.55 (−4.06 to 13.16) | 0.301 | 98.5% | 1.30 (0.91–1.70) | 0.000 | 85.4% | 0.83 (0.51–1.36) | 0.469 | 70.1% | |
| DJ diameter | <6F | 0.66 (−2.42 to 3.74) | 0.673 | 69.1% | / | / | / | 0.89 (0.32–2.42) | 0.813 | 70.5% |
| >5F | 2.42 (−21.48 to 26.32) | 0.843 | 85.5% | 1.30 (−0.68 to 3.28) | 0.199 | / | 0.89 (0.44–1.77) | 0.731 | 41.5% | |
| Nephrostomy diameter | <12F | −1.81 (−8.08 to 4.47) | 0.573 | 95.5% | 1.30 (−0.68 to 3.28) | 0.199 | / | 0.73 (0.30–1.75) | 0.481 | 62.1% |
| >11F | 4.05 (0.50–7.60) | 0.025 | / | / | / | / | 1.82 (0.94–3.50) | 0.074 | 0.0% | |
| Anesthesia type | General | −0.64 (−3.80 to 2.52) | 0.691 | 57.8% | / | / | / | 1.26 (0.62–2.55) | 0.518 | 0.0 |
| Local | 7.36 (−6.46 to 21.18) | 0.297 | 98.9% | 1.30 (0.91–1.70) | 0.000 | 85.4% | 0.82 (0.46–1.47) | 0.505 | 78.4% | |
| Combination | 16.50 (−1.82 to 34.82) | 0.077 | / | 1.30 (−0.68 to 3.28) | 0.199 | / | 0.51 (0.11–2.27) | 0.377 | 40.4% | |
| Guidance | X-ray | 1.30 (0.96–1.66) | 0.000 | 70.9% | 5.40 (−1.78 to 12.58) | 0.141 | 97.8% | 1.10 (0.82–1.46) | 0.531 | 0.0% |
| Ultrasound | / | / | / | / | / | / | 0.41 (0.28–0.59) | 0.000 | 0.0% | |
CI = confidence interval, MD = mean difference, RR = risk ratio.
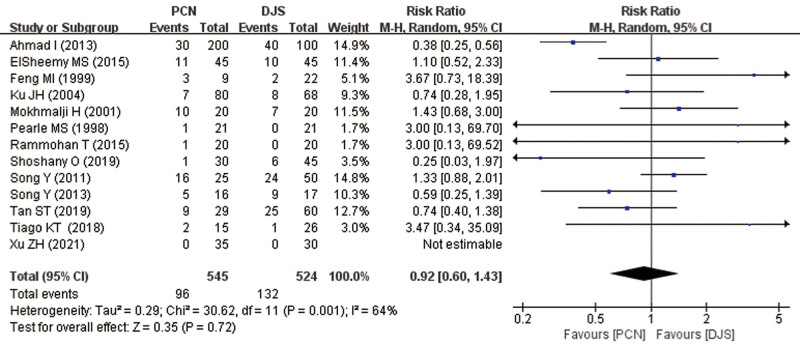
3.3. Postoperative complications
13 studies described the postoperative complications between the paired groups.[11,12,14,15,17,18,22–26,28] According to Clavien classification, Grade I included fever, hematuria, pain, urgency, urge incontinence, dysuria, waist discomfort; Grade II contained septicemia, bleeding, encrustation, pyelonephritis, infection; Grade III consisted of PCN dislodgement, ureteral perforation, migration, slippage, tube obstruction. The rates of complications were 17.61% and 25.19% in the group of PCN and DJS, respectively. However, there was no statistically significant difference (RR = 0.92; 95% CI, 0.60–1.43; P = .72). The forest plot was shown in Figure 3. However, the extreme heterogeneity was explored (64%). Subgroup analysis based on study design, disease type, sample size, sepsis, DJ diameter, nephrostomy diameter and anesthesia type was explored. Eventually, a similar result was detected except for the subgroup of guidance under ultrasound (MD = 0.41; 95% CI, 0.28–0.59, P = .000) (Table 2).
Figure 3.
Forest plot of data on postoperative complication. 95% CI = 95% confidence interval, DJS = double J stenting, PCN = percutaneous nephrostomy.
3.4. Health-related quality of life of the patient (HRQoL)
The impact of drainage interventions on HRQoL was assessed by EQ-5D questionnaire. EQ-5D questionnaire contains a system with 5 attributes including mobility, self-care, usual activities, pain/discomfort and anxiety/depression. There were 3 studies involved with the effect of drainage interventions on HRQoL.[13,21,23] Consequently, no significant statistically differences were detected in mobility (RR = 0.78; 95% CI, 0.25–2.48; P = .670), usual activities (RR = 1.72; 95% CI, 0.49–6.04; P = .400), pain/discomfort (RR = 0.88; 95% CI, 0.67–1.17; P = .390) and anxiety/depression (RR = 0.77; 95% CI, 0.53–1.12; P = .170), rather than self-care (RR = 3.07; 95% CI, 1.32–7.14; P = .009) between the paired group (Fig. 4). It showed that PCN patients had a distinct difficulty in self-care compared to DJS patients.
Figure 4.
Forest plot of data on quality of life (A: mobility; B: self-care; C: usual activities; D: pain/discomfort; E: anxiety/depression). 95% CI = 95% confidence interval, DJS = double J stenting, PCN = percutaneous nephrostomy.
3.5. Sensitivity analysis and publication bias evaluation
Sensitivity analysis by deleting each single study at a time was performed to assess the reliability of the pooled results. It demonstrated that our conclusions were relatively stable. Among them one-way sensitivity analysis of operative time and post-operative complications were shown in Figure 5. Begg’s funnel plot was used to detect the publication bias of the eligible studies, and observed no publication bias in meta-analysis of complication (Fig. 6). Meanwhile, similar results were detected in the groups of surgery time (P = .652), fluoroscopy time (P = .624), and hospital stay (P = .174).
Figure 5.
One-way sensitivity analysis of operative time and post-operative complications between 2 paired groups. CI = confidence interval.
Figure 6.
Begg’s funnel plot of postoperative complication. RR = risk ratio.
4. Discussion
The prevalence of ureteral obstruction has risen in recent years. In young and middle age, ureteral calculi is the main etiological factors of obstruction[29] For the elderly, obstruction often commonly caused by advanced malignant diseases or by a direct extension of the process.[30] Those patients often suffer pain, urinary infections, irreversible renal dysfunction, urosepsis and even death, which require emergency treatment.[1] The placement of PCN or DJS is an alternative drainage method for temporary relief of obstruction, and both of them are the mainstream surgical procedures.[31] However, we are often faced with the dilemma of choosing between PCN and DJS.
The goal of external drainage systems is to obtain ureteral drainage and maintain renal function. Both PCN and DJS placements have their own merits and demerits. Their drawbacks contain the risk of infection and displacement, as well as the discomfort of catheter and stent. Moreover, ureteral stents should be exchanged every 6 to 8 weeks because of encrustation and bacterial colonization.[32] Generally, stent placement is minimally traumatic and has a high success rate for its natural orifice surgery. In addition, it does not require an external tube, and poses a little effect on patients’ quality of life. PCN surgery reduces renal pelvis pressure and the risk of bacteremia.[28] It commonly could be completed by an interventionist under X-ray guidance, but now it is performed under local anesthesia by a urologist using ultrasonographic guidance.[28] This is a part of the reason why urologist considers PCN to be superior to DJS. A postal questionnaire survey among urologists and radiologists found that 53% of radiologists and 55% of urologists preferred PCN to ureteral stenting.[33] Likewise, oncologists were more likely to recommend PCN as the next step after stent failure in unilateral obstruction.[34] Another study also reported a more rapid return of serum creatinine to normal levels with PCN tubes than DJS.[35] Moreover, unstable patients who had larger stones and were severely ill should be treated with PCN under local anesthesia.[36] But in practice, the proper option is affected by many factors. Therefore, when selecting a surgical procedure, the physician must comprehensively consider the factors including disease severity, surgery time, hospital stay, quality of life, or even availability of in-house interventional radiology services.
In recent decades, studies evaluate the superiority of 2 common drainage technique. These results are inconsistent and inconclusive, which may be explained by small sample-sized studies. Meta-analysis is a useful tool for providing convincing evidence. Thus, we compared PCN and DJS for decompression of urinary tract obstruction. The pooled results showed DJS is a safe and better method of temporary urinary diversion than PCN for management of ureteral obstruction with shorter fluoroscopy time and hospital stay. However, no similar result was detected in operative time. On the other hand, DJS showed a relatively higher rate of postoperative complications. Analysis of the EuroQol revealed PCN patients reported more difficulties in self-care, and had a statistical difference.
Although DJS is superior to PCN for temporary urinary diversion with shorter fluoroscopy time and hospital stay in current study, the choice of treatment depends on the individual situation. For example, PCN as a better option for temporary urinary diversion in obstructive uropathy of advanced malignancies. Also, it remains an option for patients who have failed to place retrograde stent or faced recurrence of the obstruction after stent remove.[37] Moreover, PCN is now performed under local anesthesia using ultrasonographic guidance, which might be preferable for patients who might not be able to tolerate general anesthesia under X-ray guidance.[38] Thus, the ideal choice between PCN and DJS often depends on the individual situation.
Actually, our meta-analysis has its limitations. Firstly, only published studies might not provide sufficient evidences. Meanwhile, the heterogeneity suggested that potential or undiscovered factors might be ignored. Whereas, in spite of limitations, our results show that Both DJS placement and PCN drainage appear effective. DJS has the superiority in fluoroscopy time and hospital stay. Meanwhile, the 2 techniques had distinct and significantly different impacts on quality of life.
In conclusion, DJS is a safer and better method than PCN for management of ureteral obstruction with shorter fluoroscopy time and hospital stay. Moreover, PCN patients have a difficulty in self-care compared to DJS patients. However, the choice between PCN and DJS often depends on the individual situation.
Author contributions
Conceptualization: Kai-Ping Zhang.
Data curation: Kai-Ping Zhang.
Formal analysis: Kai-Ping Zhang.
Investigation: Yin Zhang.
Methodology: Yin Zhang.
Project administration: Kai-Ping Zhang, Min Chao.
Resources: Kai-Ping Zhang.
Software: Kai-Ping Zhang.
Supervision: Kai-Ping Zhang, Min Chao.
Validation: Kai-Ping Zhang, Yin Zhang, Min Chao.
Visualization: Min Chao.
Writing – original draft: Yin Zhang, Min Chao.
Writing – review & editing: Kai-Ping Zhang, Yin Zhang, Min Chao.
Abbreviations:
- CI =
- confidence interval
- DJS =
- Double J stenting
- HRQoL =
- health-related quality of life of the patient
- MD =
- mean difference
- PCN =
- percutaneous nephrostomy
- RR =
- risk ratio
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are publicly available.
How to cite this article: Zhang K-P, Zhang Y, Chao M. Which is the best way for patients with ureteral obstruction? Percutaneous nephrostomy versus double J stenting. Medicine 2022;101:45(e31194).
Contributor Information
Kai-Ping Zhang, Email: 814491329@qq.com.
Yin Zhang, Email: 814491329@qq.com.
References
- [1].Tabib C, Nethala D, Kozel Z, et al. Management and treatment options when facing malignant ureteral obstruction. Int J Urol. 2020;27:591–8. [DOI] [PubMed] [Google Scholar]
- [2].Yoon JH, Park S, Park S, et al. Renal function is associated with prognosis in stent-change therapy for malignant ureteral obstruction. Investig Clin Urol. 2018;59:376–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Netsch C, Becker B, Gross AJ. Therapie der Harnleiterobstruktion: Stellenwert von perkutaner Nephrostomie und von Harnleiterschienen [Management of ureteral obstruction: value of percutaneous nephrostomy and ureteral stents]. Urologe A. 2016;55:1497–510. [DOI] [PubMed] [Google Scholar]
- [4].Hardie EM, Kyles AE. Management of ureteral obstruction. Vet Clin North Am Small Anim Pract. 2004;34:989–1010. [DOI] [PubMed] [Google Scholar]
- [5].Munafo MR, Flint J. Meta-analysis of genetic association studies. Trends Genet. 2004;20:439–44. [DOI] [PubMed] [Google Scholar]
- [6].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34. [DOI] [PubMed] [Google Scholar]
- [7].Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–26. [PubMed] [Google Scholar]
- [8].Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- [9].DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. [DOI] [PubMed] [Google Scholar]
- [10].Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–48. [PubMed] [Google Scholar]
- [11].Rammohan T, Panduranga RK, Prasad DV, et al. A comparative study of percutaneous nephrostomy versus DJ stenting in infective hydronephrosis in calculous disease. J Evol Med Dent Sci. 2015;4:3143–53. [Google Scholar]
- [12].Ku JH, Lee SW, Jeon HG, et al. Percutaneous nephrostomy versus indwelling ureteral stents in the management of extrinsic ureteral obstruction in advanced malignancies: are there differences? Urology. 2004;64:895–9. [DOI] [PubMed] [Google Scholar]
- [13].Joshi HB, Adams S, Obadeyi OO, et al. Nephrostomy tube or “JJ” ureteric stent in ureteric obstruction: assessment of patient perspectives using quality-of-life survey and utility analysis. Eur Urol. 2001;39:695–701. [DOI] [PubMed] [Google Scholar]
- [14].Song Y, Fei X, Song Y. Percutaneous nephrostomy versus indwelling ureteral stent in the management of gynecological malignancies. Int J Gynecol Cancer. 2012;22:697–702. [DOI] [PubMed] [Google Scholar]
- [15].Ahmad I, Saeed Pansota M, Tariq M, et al. Comparison between double J (DJ) ureteral stenting and percutaneous nephrostomy (PCN) in obstructive uropathy. Pak J Med Sci. 2013;29:725–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Monsky WL, Molloy C, Jin B, et al. Quality-of-life assessment after palliative interventions to manage malignant ureteral obstruction. Cardiovasc Intervent Radiol. 2013;36:1355–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Feng MI, Bellman GC, Shapiro CE. Management of ureteral obstruction secondary to pelvic malignancies. J Endourol. 1999;13:521–4. [DOI] [PubMed] [Google Scholar]
- [18].Song Y, Fei X, Song Y. Diagnosis and operative intervention for problematic ureteral calculi during pregnancy. Int J Gynaecol Obstet. 2013;121:115–8. [DOI] [PubMed] [Google Scholar]
- [19].Mokhmalji H, Braun PM, Martinez Portillo FJ, et al. Percutaneous nephrostomy versus ureteral stents for diversion of hydronephrosis caused by stones: a prospective, randomized clinical trial. J Urol. 2001;165:1088–92. [PubMed] [Google Scholar]
- [20].Yoshimura K, Utsunomiya N, Ichioka K, et al. Emergency drainage for urosepsis associated with upper urinary tract calculi. J Urol. 2005;173:458–62. [DOI] [PubMed] [Google Scholar]
- [21].de Sousa Morais N, Pereira JP, Mota P, et al. Percutaneous nephrostomy vs ureteral stent for hydronephrosis secondary to ureteric calculi: impact on spontaneous stone passage and health-related quality of life-a prospective study. Urolithiasis. 2019;47:567–73. [DOI] [PubMed] [Google Scholar]
- [22].Pearle MS, Pierce HL, Miller GL, et al. Optimal method of urgent decompression of the collecting system for obstruction and infection due to ureteral calculi. J Urol. 1998;160:1260–4. [PubMed] [Google Scholar]
- [23].Shoshany O, Erlich T, Golan S, et al. Ureteric stent versus percutaneous nephrostomy for acute ureteral obstruction – clinical outcome and quality of life: a bi-center prospective study. BMC Urol. 2019;19:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Tan ST, Tao Z, Bian X, et al. Ureteral stent placement and percutaneous nephrostomy in the management of hydronephrosis secondary to cervical cancer. Eur J Obstet Gynecol Reprod Biol. 2019;241:99–103. [DOI] [PubMed] [Google Scholar]
- [25].Tiago KT, Grubert RM, Santos RFT, et al. Percutaneous nephrostomy versus antegrade double-J stent placement in the treatment of malignant obstructive uropathy: a cost-effectiveness analysis from the perspective of the Brazilian public health care system. Radiol Bras. 2019;52:305–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].ElSheemy MS, Shouman AM, Shoukry AI, et al. Ureteric stents vs percutaneous nephrostomy for initial urinary drainage in children with obstructive anuria and acute renal failure due to ureteric calculi: a prospective, randomised study. BJU Int. 2015;115:473–9. [DOI] [PubMed] [Google Scholar]
- [27].Elbatanouny AM, Ragheb AM, Abdelbary AM, et al. Percutaneous nephrostomy versus JJ ureteric stent as the initial drainage method in kidney stone patients presenting with acute kidney injury: a prospective randomized study. Int J Urol. 2020;27:916–21. [DOI] [PubMed] [Google Scholar]
- [28].Xu ZH, Yang YH, Zhou S, et al. Percutaneous nephrostomy versus retrograde ureteral stent for acute upper urinary tract obstruction with urosepsis. J Infect Chemother. 2021;27:323–8. [DOI] [PubMed] [Google Scholar]
- [29].Zhang Z, Wang X, Chen D, et al. Minimally invasive management of acute ureteral obstruction and severe infection caused by upper urinary tract calculi. J X-Ray Sci Technol. 2020;28:125–35. [DOI] [PubMed] [Google Scholar]
- [30].Kumar A, Mynderse L, Patel K, et al. Ureteral obstruction in cancer patients: a qualitative study. Psychooncology. 2016;25:605–9. [DOI] [PubMed] [Google Scholar]
- [31].Hsu L, Li H, Pucheril D, et al. Use of percutaneous nephrostomy and ureteral stenting in management of ureteral obstruction. World J Nephrol. 2016;5:172–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Loughlin KR, Bailey RB, Jr. Internal ureteral stents for conservative management of ureteral calculi during pregnancy. N Engl J Med. 1986;315:1647–9. [DOI] [PubMed] [Google Scholar]
- [33].Lynch MF, Anson KM, Patel U. Percutaneous nephrostomy and ureteric stent insertion for acute renal deobstruction: consensus based guidance. Br J Med Surg Urol. 2008;1:120–5. [Google Scholar]
- [34].Hyams ES, Shah O. Malignant extrinsic ureteral obstruction: a survey of urologists and medical oncologists regarding treatment patterns and preferences. Urology. 2008;72:51–6. [DOI] [PubMed] [Google Scholar]
- [35].Elgammal MA, Abdel-Kader MS, Kurkar A, et al. Management of calculus anuria in children: experience of 54 cases. J Pediatr Urol. 2009;5:462–5. [DOI] [PubMed] [Google Scholar]
- [36].Goldsmith ZG, Oredein-McCoy O, Gerber L, et al. Emergent ureteric stent vs percutaneous nephrostomy for obstructive urolithiasis with sepsis: patterns of use and outcomes from a 15-year experience. BJU Int. 2013;112:E122–8. [DOI] [PubMed] [Google Scholar]
- [37].Lau MW, Temperley DE, Mehta S, et al. Urinary tract obstruction and nephrostomy drainage in pelvic malignant disease. Br J Urol. 1995;76:565–9. [DOI] [PubMed] [Google Scholar]
- [38].Bres-Niewada E. Ureteral obstruction in pregnancy – the “Stone Mountain” for the urologist. Cent Eur J Urol. 2017;70:101–2. [DOI] [PMC free article] [PubMed] [Google Scholar]