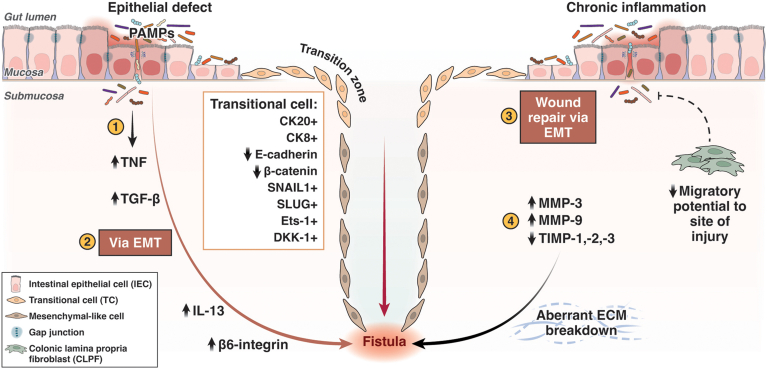
Figure 2.
Schematic of the pathogenesis of CD-associated fistula formation. (1) IECs undergo EMT converting to TC in response to a defect in the epithelial barrier; resultant infiltration of pathogen associated molecular patterns enter the gut mucosa, which elicits an immune response. (2) An upregulation of TNF, a potent inducer of TGF-β, occurs which stimulates a cascade of pro-inflammatory cytokines (IL-13) and cell invasive molecules (β6-integrin) resulting in TCs adopting features of an invasive mesenchymal-like cell. TCs preserve their epithelial origins (CK20/8+); however, they down-regulate expression of epithelial cell adhesion molecules (E-cadherin, β-catenin) and highly express EMT-inducing transcription factors (SNAIL1, SLUG, Ets-1) and cell migratory molecule, DKK-1. In addition, TCs may appear more disordered with a loss of gap junctions and fragmented basement membranes. (3) Chronic inflammation results in reduced epithelial repair and reduced migratory capabilities of CLPFs, which contribute to poor wound healing in fistulating CD; IECs compensate by undergoing EMT in an attempt to restore the epithelial barrier. (4) MMPs (MMP-3, MMP-9) are highly expressed and unopposed (reduced TIMP-1, -2, -3) in fistulating CD tissue, resulting in aberrant breakdown of the extracellular matrix and tissue remodeling. These pathways consequently contribute to fistula formation. (Figure created with BioRender.com and adapted from Siegmund et al.12 CK, Cytokeratins; PAMP, pathogen-associated molecular pattern.