Case 7.
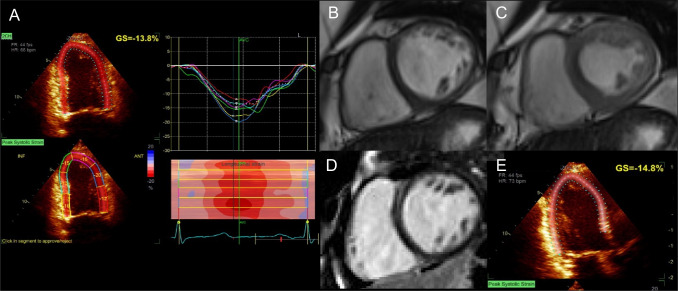
Acute onset of dyspnea in a 47-year-old woman with breast cancer. A 74-year-old woman without CVRFs presented with a human epidermal growth factor receptor 2 (HER2)-positive, hormone receptor (HR)-negative, locally advanced left-sided breast cancer with ipsilateral axillary lymph node extension (pT2N1M0, stage IIB). Given her age and the absence of indication for radiotherapy, she underwent surgical treatment by mastectomy and axillary lymph node dissection. Adjuvant chemotherapy was planned, consisting of 4 cycles doxorubicin (60 mg/m2) plus cyclophosphamide (500 mg/m2) and 12 cycles of weekly paclitaxel (75 mg/m2) plus trastuzumab (2 mg/kg) followed by 1 year of trastuzumab maintenance (3-weekly, 6 mg/kg). Pre-treatment echocardiography showed a normal LVEF (65%) and a normal GLS (18%). Following the third cycle [cumulative dose of anthracycline 180 mg/m2 (recommended maximum cumulative dose 400 mg/m2)], the patient presented with an acute onset of dyspnea requiring oxygen therapy. NT-proBNP and troponin I were increased (1026 ng/mL, ULN 738 ng/mL and 0.26 μg/L, ULN 0.10 μg/L, respectively). Echocardiography showed decreased LVEF (45%) and GLS (13.8%, N > 15%). A Doxorubicin-induced CTRCD was suspected, and a CMR was performed confirming reduced LVEF (42%). B and C Balanced SSFP short-axis view of mid-LV. LGE sequences showed no sign of scar (D). Chemotherapy was withheld and HF treatments consisting of diuretic, betablockers, and angiotensin-converting enzyme inhibitor were initiated, and control echocardiography showed an increase of LVEF but persistence of mildly decreased GLS (E), indicating persistent subclinical cardiotoxicity. Any further exposure to doxorubicin was omitted. Continuation of the treatment with paclitaxel and trastuzumab was planned to be initiated when LVEF would recover to approximately 50% under regular echocardiographic and laboratory monitoring. With breast cancer becoming the most prevalent cancer worldwide in 2020 [234], a shift of the overall burden of cancer treatment-related cardiac complications towards women can be expected. Increasing awareness about the intertwining of cardiac diseases and cancer is therefore paramount to cardiac imagers. The detection of subclinical cardiotoxicity before the onset of heart failure using advanced imaging criteria, such as GLS, or obtaining cardiovascular information from oncological imaging exams [213] could help to reduce the complications of cancer treatments and should therefore be part of the routine monitoring of patients undergoing potentially cardiotoxic therapies. Abbreviations: CMR: cardiac magnetic resonance; CTRCD: cancer treatment-related cardiac disease; CVRF: cardiovascular risk factor; GLS: global longitudinal strain; HF: heart failure; LGE: late gadolinium enhancement; LV: left ventricle; LVEF: left ventricular ejection fraction; NT-proBNP: N-terminal brain natriuretic peptide; SSFP: steady-state free precession; ULN: upper limit of normal