Abstract
Background:
Falls are common in older adults and can lead to severe injuries. The Strategies to Reduce Injuries and Develop Confidence in Elders (STRIDE) trial cluster-randomized 86 primary care practices across 10 health systems to a multifactorial intervention to prevent fall injuries, delivered by registered nurses trained as falls care managers, or enhanced usual care. STRIDE enrolled 5451 community-dwelling older adults age ≥ 70 at increased fall injury risk.
Methods:
We assessed fall-related outcomes via telephone interviews of participants (or proxies) every four months. At baseline, 12 and 24 months, we assessed health-related quality of life (HRQOL) using the EQ-5D-5L and EQ-VAS. We used Poisson models to assess intervention effects on falls, fall-related fractures, fall injuries leading to hospital admission, and fall injuries leading to medical attention. We used hierarchical longitudinal linear models to assess HRQOL.
Results:
For recurrent event models, intervention versus control incidence rate ratios were 0.97 (95% confidence interval (CI), 0.93–1.00; p=0.048) for falls, 0.93 (95% CI, 0.80–1.08; p=0.337) for self-reported fractures, 0.89 (95% CI, 0.73–1.07; p=0.205) for adjudicated fractures, 0.91 (95% CI, 0.77–1.07; p=0.263) for falls leading to hospital admission, and 0.97 (95% CI, 0.89–1.06; p=0.477) for falls leading to medical attention. Similar effect sizes (non-significant) were obtained for dichotomous outcomes (e.g., participants with ≥ 1 events). The difference in least square mean change over time in EQ-5D-5L (intervention minus control) was 0.009 (95% CI −0.002 to 0.019, p=0.106) at 12 months and 0.005 (95% CI −0.006 to 0.015, p=0.384) at 24 months.
Conclusions:
Across a standard set of outcomes typically reported in fall prevention studies, we observed modest improvements, one of which was statistically significant. Future work should focus on patient-, practice-, and organization-level operational strategies to increase the real-world effectiveness of interventions, and improving the ability to detect small but potentially meaningful clinical effects.
Keywords: older persons, care management, health-related quality of life, pragmatic trials
Introduction
Twenty-nine percent of community-dwelling older adults fall at least once annually, with about 10% of these falls resulting in serious injuries (e.g., fractures).1 The Strategies to Reduce Injuries and Develop Confidence in Elders (STRIDE) study was a cluster-randomized trial of a multifactorial fall injury prevention intervention in community-dwelling older adults age 70 or older at increased fall injury risk.2 The STRIDE study found no statistically significant reduction in its primary outcome (the time to first adjudicated serious fall injury) but did find a modest statistically significant reduction in time to first self-reported fall injury, a broader measure including injuries that did and did not lead to medical attention.3
To compare results across studies, international consensus guidance recommends that fall prevention trials report a range of outcomes, including falls, fall injuries, psychological consequences of falling, health-related quality of life, and physical activity.4 The Cochrane review of multifactorial fall prevention interventions provides results on falls, fall-related fractures, falls leading to hospital admission, falls leading to medical attention, health-related quality of life, and adverse events.5 In addition to the primary outcome of the time to first adjudicated serious fall injury,3 we have previously reported STRIDE results on serious adverse events3 and psychological consequences of falling.6 To facilitate comparison with the broader literature on fall prevention studies, we now report STRIDE’s effect on fall-related outcomes (falls, fall-related fractures, fall injuries leading to hospital admission, fall injuries leading to medical attention) and health-related quality of life.
Methods
STRIDE included 10 healthcare systems across the US, with 86 practices cluster-randomized in a 1:1 ratio to either a multifactorial, patient-centered intervention delivered in primary care settings by registered nurses trained as falls care managers, or to enhanced usual care, including an informational pamphlet about falls and encouragement of participants to discuss falls with their primary care provider. To identify individuals who were at increased risk for fall injuries, STRIDE included participants who answered “yes” to at least one of three items: (a) have you fallen and hurt yourself in past year?, (b) have you fallen ≥ 2 times in past year?, and (c) are you afraid that you might fall because of balance or walking problems? Prior work provides details of STRIDE’s design,2 screening and recruitment procedures,7 intervention,8 and participant retention.9 STRIDE was approved by a single institutional review board at the Massachusetts General Brigham Healthcare System, Boston, MA.
Data
The primary source for fall-related outcome ascertainment was structured telephone interviews of participants (or their proxies), conducted by masked, trained interviewers at the Yale Recruitment and Assessment Center, beginning at four months post-enrollment and continuing every four months thereafter. Participants were mailed fall calendars to prospectively record their falls and to serve as a memory aid for follow-up interviews. If participants did not complete a particular follow-up interview, the next follow-up interview asked about falls over the time window since the participant was last interviewed. Completion of follow-up interviews was greater than 93% at each time point. Most participants completed all (71.8%) or all but one (9.2%) of the follow-up interviews.9 As part of STRIDE’s outcome adjudication process, fall-related fracture events were adjudicated, but thoracic and lumbar vertebral fractures were excluded from adjudication due to STRIDE’s primary outcome definition.10 Given this distinction, we report results for both self-reported and adjudicated fractures. Further details about data definitions and coding may be found in the Supplementary Text S1.
At baseline, 12-month, and 24-month interviews, STRIDE participants were administered the EQ-5D-5L, a measure of health-related quality of life,11,12 and the EQ-VAS, a global rating of health.13 The dimensions of EQ-5D-5L include mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Responses for each dimension have five levels: “no problems,” “slight problems,” “moderate problems,” “severe problems,” and “unable to /extreme problems.” We used US community weights to convert responses on the five EQ-5D-5L dimensions into a single index value calibrated such that a value of 1 represents perfect health and a value of 0 represents death (values less than 0 are possible), based on a Tobit model.14 Scores on the EQ-VAS range from 0 (worst health imaginable) to 100 (best health imaginable).
Statistical Analysis
We conducted all analyses using an “intention to treat” approach. We calculated fall-related outcomes as rates, and summarized EQ-5D-5L and EQ-VAS results using means and standard deviations. We used practice-level Poisson regression (consistent with prior STRIDE analyses3) to analyze recurrent fall-related outcomes as a function of intervention versus control group status, adjusting for covariates prespecified in the STRIDE statistical analysis plan: 1) healthcare system and 2) practice-level factors used in covariate-constrained randomization, including a) practice size (by tertile), b) geography (urban versus rural), and c) practice race/ethnicity (majority of patients’ primary identification: nonwhite versus white).15 To evaluate dichotomous outcomes in intervention and control groups, we used participant-level population-averaged Poisson models clustered by practice,16 adjusting for the prespecified covariates.
As in prior STRIDE work with repeated continuous measures,6 we analyzed EQ-5D-5L and EQ-VAS results in intervention versus control groups using hierarchical longitudinal linear models, with the dependent variable represented as the change in values from baseline to 12 months, and from baseline to 24 months. We included a random intercept for practice and for participant and estimated treatment by time interactions (at 12 and 24 months) as quantifying mean treatment effects. In addition to those previously specified, covariates included baseline values of the dependent variable and baseline factors found to be associated with missing follow-up data (age, education, self-rated health, whether participant or surrogate completed baseline interview, use of walking aid outside). Data were assumed to be missing at random (after adjustment for factors above).
All analyses were performed using Stata 17 (College Station, TX) and used two-tailed significance tests, with p-values less than 0.05 denoting statistical significance. No adjustment was made for multiple testing.
Results
STRIDE participants were mean age 80, 62% female, 91% white, and 52% had at least a college degree (Table 1). Participants had a mean of 2.1 chronic conditions, 5% had a prior hip fracture after age 50, and 33% had a prior non-hip fracture after age 50. Baseline characteristics were well-balanced between intervention and control groups.
Table 1.
Baseline Demographic and Clinical Characteristicsa
| Characteristic | Intervention (N=2802) | Control (N=2649) | Total (N=5451) |
|---|---|---|---|
| Age — yr | 79.8 ± 6.5 | 79.5 ± 6.0 | 79.7 ± 6.2 |
| Female sex — no. (%) | 1752 (62.5) | 1629 (61.5) | 3381 (62.0) |
| Race — no. (%)b | |||
| White | 2571 (91.8) | 2394 (90.4) | 4965 (91.1) |
| Black | 128 (4.6) | 164 (6.2) | 292 (5.4) |
| Other or unknown | 103 (3.7) | 91 (3.4) | 194 (3.6) |
| Hispanic ethnic group — no. (%)b | 196 (7.0) | 211 (8.0) | 407 (7.5) |
| Educational level — no. (%) | |||
| High school graduate or less | 602 (21.5) | 643 (24.3) | 1245 (22.8) |
| Some college or equivalent | 697 (24.9) | 659 (24.9) | 1356 (24.9) |
| College graduate or higher | 1502 (53.6) | 1343 (50.7) | 2845 (52.2) |
| Unknown | 1 (<0.1) | 4 (0.2) | 5 (0.1) |
| Chronic conditionsc | |||
| No. per participant | 2.1±1.3 | 2.1±1.3 | 2.1±1.3 |
| Fracture other than of the hip after 50 yr of age — no. (%) | 918 (32.8) | 876 (33.1) | 1794 (32.9) |
| Hip fracture after 50 yr of age — no. (%) | 132 (4.7) | 119 (4.5) | 251 (4.6) |
| Clinically significant cognitive impairment — no. (%)d | 85 (3.0) | 75 (2.8) | 160 (2.9) |
| Use of a mobility aid or inability to ambulate — no. (%) | 972 (34.7) | 909 (34.3) | 1881 (34.5) |
| Screening risk questions for fall injuries — no. (%) | |||
| Fell two or more times in the past year | 1015 (36.2) | 896 (33.8) | 1911 (35.1) |
| Had a fall-related injury in the past year | 1089 (38.9) | 1031 (38.9) | 2120 (38.9) |
| Was afraid of falling because of problems with walking or balance | 2405 (85.8) | 2273 (85.8) | 4678 (85.8) |
Plus–minus values are means ±SD. Percentages may not total 100 because of rounding.
Race and ethnic group were reported by the participant.
Other chronic conditions reported included hypertension, cancer, arthritis, diabetes, chronic lung disease, myocardial infarction, stroke, congestive heart failure, and Parkinson’s disease.
Based on four or more errors on the six-item Callahan cognitive screening instrument or if the initial telephone interview was completed entirely by proxy.
Figure 1 and Table 2 show fall-related outcomes, providing Cochrane review results for comparison, where available.5 For recurrent event models (Figure 1), intervention versus control incidence rate ratios were 0.97 (95% confidence interval (CI), 0.93–1.00; p=0.048) for falls, 0.93 (95% CI, 0.80–1.08; p=0.337) for self-reported fractures, 0.89 (95% CI, 0.73–1.07; p=0.205) for adjudicated fractures, 0.91 (95% CI, 0.77–1.07; p=0.263) for falls leading to hospital admission, and 0.97 (95% CI, 0.89–1.06; p=0.477) for falls leading to medical attention. Similar results (all statistically non-significant) were obtained for dichotomous outcomes (Table 2).
Figure 1:
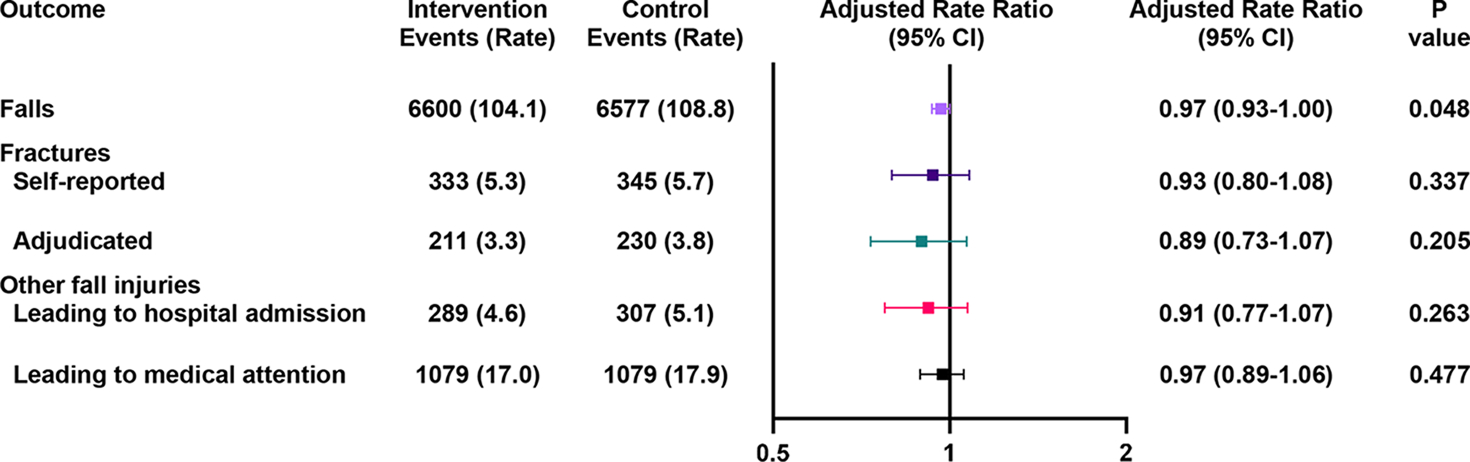
Rates of recurrent events for fall-related outcomes. The intervention group included 2802 participants and 6338.3 person-years of follow-up, while the control group included 2649 participants and 6042.5 person-years of follow-up. Rates are reported per 100 person years. Rate ratios are based on practice-level Poisson regression adjusted for constrained randomization variables and healthcare system. In the Cochrane review of multifactorial interventions to prevent falls, the rate ratio (95% CI) for falls was 0.77 (0.67–0.87) in 5853 participants (19 randomized trials).5 CI, confidence interval.
Table 2.
Dichotomous fall, fall-related fracture, and other fall injury outcomes, as compared with Cochrane review.5
| STRIDE | Cochrane Review | ||||||
|---|---|---|---|---|---|---|---|
| Outcomea | Intervention (N=2802) no. (%) | Control (N=2649) n (%) | Adjusted Rate Ratio (95% CI)b | P value | Risk Ratio (95% CI) | Participants N | Studies N |
| Falls | |||||||
| One or more falls | 1833 (65.4) | 1798 (67.9) | 0.99 (0.91–1.08) | 0.836 | 0.96 (0.90–1.03) | 9637 | 29 |
| Two or more falls | 1242 (44.3) | 1220 (46.1) | 0.97 (0.91–1.04) | 0.389 | 0.87 (0.74–1.03) | 3368 | 12 |
| Fractures | |||||||
| One or more self-reported fall-related fractures | 287 (10.2) | 296 (11.2) | 0.94 (0.79–1.12) | 0.482 | 0.73 (0.53–1.01)c | 2850 | 9 |
| One or more adjudicated fall-related fractures | 184 (6.6) | 203 (7.7) | 0.87 (0.72–1.05) | 0.140 | |||
| Other fall injuries | |||||||
| One or more hospital admissions for fall-related injuries | 242 (8.6) | 266 (10.0) | 0.88 (0.74–1.04) | 0.125 | 1.00 (0.92–1.07) | 5227 | 15 |
| One or more fall-related injury events leading to medical attention (including hospital admission) | 772 (27.6) | 785 (29.6) | 0.95 (0.86–1.05) | 0.290 | 0.91 (0.75–1.10) | 3078 | 8 |
Outcome assessed for the full duration of follow-up for each participant. Median follow-up was 2.3 years (interquartile range = 2.0–2.7 years).
Participant-level population-averaged Poisson model clustered by practice, adjusted for constrained randomization variables and healthcare system
Cochrane meta-analysis synthesized results across studies with varying ways of ascertaining fractures.
Table 3 provides unadjusted values for the EQ-5D-5L and EQ-VAS at each time point by treatment group. Adjusted regression analyses showed no statistically significant difference in least square mean change over time in the EQ-5D-5L index (intervention change minus control change) at 12 months (0.009, 95% CI: −0.002 to 0.019, p=0.106) or 24 months (0.005, 95% CI: −0.006 to 0.015, p=0.384). Similarly, adjusted analyses showed no difference in change over time between intervention and control groups for the EQ-VAS at 12 months (0.49, 95% CI: −0.42 to 1.40, p=0.289) or 24 months (0.47, 95% CI: −0.46 to 1.39, p=0.322).
Table 3.
Unadjusted Values for EQ-5D-5L and EQ-VASa
| Baseline | 12 months | 24 months | ||||
|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | |
| EQ-5D-5L utility,b mean ± SD | 0.831 ± 0.178 (N=2785) | 0.834 ± 0.166 (N=2634) | 0.822 ± 0.193 (N=2385) | 0.817 ± 0.192 (N=2262) | 0.819 ± 0.202 (N=2242) | 0.815 ± 0.204 (N=2140) |
| EQ-VAS,c mean ± SD | 78.9 ± 16.3 (N=2771) | 78.8 ± 16.2 (N=2627) | 77.0 ± 17.3 (N=2360) | 76.6 ± 17.0 (N=2247) | 77.3 ± 17.3 (N=2234) | 76.7 ± 16.9 (N=2122) |
Sample sizes of available participant responses for each item and time period are shown in parentheses.
Complete case analysis.
EQ-5D-5L scores range from −0.573 to 1,14 where 0 represents death and 1 represents perfect health.
EQ-VAS scores range from 0 to 100, where 0 represents the worst health imaginable and 100 represents the best health imaginable.
Discussion
In the STRIDE study, point estimates favored the multifactorial intervention across a set of outcomes commonly used to summarize the effects of fall prevention interventions,5 but only one result reached statistical significance: a 3% relative reduction in rate of falls. This effect was noticeably more modest than the Cochrane review fall rate (rate ratio 0.77; 95% CI 0.67–0.87).5 For all other outcomes available in both STRIDE and the Cochrane review, 95% confidence intervals substantially overlapped.
STRIDE’s implementation setting (primary care) and multi-center pragmatic design are important strengths that enhance the external validity of results. These same factors may have affected STRIDE’s effectiveness, given the complexity of implementing a multifactorial fall injury prevention intervention across 43 primary care practices in 10 health systems.17 STRIDE falls care managers successfully assessed participants’ underlying risk factors for fall injuries, but process evaluations from STRIDE (and PreFIT, another large, recently published pragmatic fall prevention trial18,19) point to a drop-off between risk factors identified during assessment, and risk factors acted upon (or prioritized for action).3 Additional data available only in PreFIT show stepwise drop-off between referral to exercise, to attendance at first exercise session, and to actual completion of the PreFIT exercise program.18,19 Because STRIDE’s pragmatic design relied upon existing medical and community resources for exercise, with data suggesting that costs (e.g., copayments for physical therapy) may have posed a barrier to adherence,17 it is possible that lack of sustained adherence to exercise, a key intervention to reduce falls,20 may have contributed to STRIDE’s largely null results.
It is possible that, applied at the population level, STRIDE’s approach would produce a small but meaningful (i.e., 7–11%) relative reduction in fractures and falls leading to hospital admission, the circumstance most consistent with what we observed in the trial, but also one that STRIDE was not powered to detect. An effect size of this magnitude is consistent with community-based dissemination efforts such as the Connecticut Collaboration for Fall Prevention, which found a 9% statistically significant relative reduction in serious fall injuries.21 Outcome ascertainment using routinely collected data (e.g., from claims or electronic health records) could reduce the cost of conducting larger, simpler trials that would be powered to detect small but potentially meaningful effects.
Simplifying intervention delivery could potentially enhance STRIDE’s effectiveness. Options for simplification include focusing the risk assessment on a smaller set of factors, which, if identified and addressed, would yield the highest benefit at the population level, and then more intensely working with patients to address this smaller set of risk factors (e.g., gait/balance/strength; and medications, including pharmacologic treatment of osteoporosis and reduction of fall risk increasing drugs). A complementary approach might decrease the number of steps between screening, assessment, intervention uptake, and intervention adherence, to reduce drop-off at each step.17,22 For example, for those deemed eligible, a standardized exercise program delivered virtually might facilitate uptake and adherence; recent work demonstrates proof of concept for this approach, albeit in a healthier population.23 However, even with simpler, more powerful interventions, variation in implementation – and thus dilution of intervention effect – should be expected in large, pragmatic studies.
Our results are limited by several factors. First, the reported analyses were not pre-specified in STRIDE’s statistical analysis plan;15 this limitation was mitigated by following standard definitions of outcomes as used in the Cochrane review of multifactorial fall prevention interventions5 and mirroring analytic approaches used in STRIDE’s prespecified analyses wherever possible. Second, since STRIDE focused on fall injuries and not falls per se, STRIDE participants were not asked about whether their falls without injury met the Prevention of Falls Network Europe definition of a fall.4 Third, as is true for all multifactorial fall prevention interventions, participants could not be blinded to group assignment. Being aware of group assignment could have led intervention participants to take actions to reduce falls independent of actions agreed upon with the falls care manager, or led to reporting bias for the non-adjudicated outcomes evaluated in the current study; the direction of this latter bias is unclear. Fourth, for the outcome of self-reported fall injuries leading to medical attention, intervention participants may have been sensitized to seek medical attention through interaction with their falls care manager (biasing results for this outcome to the null),24,25 although intervention protocols for fall care managers were designed to minimize this bias. This limitation applies less to fracture outcomes and falls leading to hospital admission, given that these more severe events would likely come to medical attention regardless of treatment arm.
In conclusion, across a standard set of outcomes typically reported in fall prevention studies, modest, mostly statistically non-significant improvements were observed favoring the STRIDE intervention. Future work should focus on simplifying implementation, strengthening intervention components (including incorporating strategies to promote long term adherence to exercise and other behaviors), and improving the ability to detect small but clinically meaningful effects.
Supplementary Material
Supplementary Text S1: Additional Details on Methods, and Full Acknowledgments.
Key points:
To compare the effectiveness of fall prevention interventions, consensus guidance recommends that a standard set of outcomes be reported for each study; this report provides results for fall, fall injury, and health-related quality of life outcomes in the Strategies to Reduce Injuries and Develop Confidence in Elders (STRIDE) study, a pragmatic cluster-randomized trial of a multifactorial fall injury prevention intervention.
For all outcomes, point estimates favored the intervention group, but effect sizes were modest, and results for only one outcome were statistically significant.
To enhance the effectiveness of fall prevention interventions in primary care settings, future work should refine patient-, practice-, and organization-level strategies to improve implementation and adherence; improving the ability to detect small but potentially meaningful clinical effects is also critical.
Why does this matter?
Based on the findings from this report, dissemination of multifactorial fall injury prevention programs across multiple health systems will have at best modest effects on fall, fall injury, and health-related quality of life outcomes. Whether these dissemination efforts provide sufficient population benefit to warrant the resources invested is an important topic to consider in future research.
Acknowledgments
Please see Supplementary Text S1 for a full list of acknowledgments for the STRIDE study.
Funding sources:
Supported by the Patient-Centered Outcomes Research Institute and the National Institute on Aging of the National Institutes of Health (NIH) through a cooperative agreement (5U01AG048270) between the National Institute on Aging and Brigham and Women’s Hospital. Drs. Greene, Esserman, Dziura, and Peduzzi were also supported by a CTSA grant (UL1TR000142) from the National Center for Advancing Translational Sciences (NCATS), a component of the NIH. Dr. McMahon was also supported by grants (KL2TR000113 and UL1TR000114) from the University of Minnesota Clinical and Translational Science Institute, funded by NCATS. Dr. Bhasin was supported in part by the Boston Claude D. Pepper Older Americans Independence Center (P30AG013679). Dr. Gill and Ms. Araujo were also supported by the Yale Claude D. Pepper Older Americans Independence Center (P30AG021342). Dr. Alexander was also supported in part by the Michigan Claude D. Pepper Older Americans Independence Center (P30 AG024824). Drs. Greenspan and Resnick were also supported in part by the Pittsburgh Claude D. Pepper Older Americans Independence Center (P30 AG024827). Dr. Volpi was supported in part by the UTMB Claude D. Pepper Older Americans Independence Center (P30AG024832).
Sponsor’s Role:
The organizations funding this study had no role in the design or conduct of the study; in the collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript. The content of this publication is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the Department of Veterans Affairs, or the United States government.
Footnotes
Clinicaltrials.gov identifier: NCT02475850
Conflict of Interest: Dr. Magaziner reports board membership on the Fragility Fracture Network and Own the Bone Multi-disciplinary Advisory Board of the American Orthopedic Association. All other authors report no conflicts.
References
- 1.Ganz DA, Latham NK. Prevention of Falls in Community-Dwelling Older Adults. N Engl J Med. 2020;382(8):734–743. [DOI] [PubMed] [Google Scholar]
- 2.Bhasin S, Gill TM, Reuben DB, et al. Strategies to Reduce Injuries and Develop Confidence in Elders (STRIDE): A Cluster-Randomized Pragmatic Trial of a Multifactorial Fall Injury Prevention Strategy: Design and Methods. J Gerontol A Biol Sci Med Sci. 2018;73(8):1053–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhasin S, Gill TM, Reuben DB, et al. A Randomized Trial of a Multifactorial Strategy to Prevent Serious Fall Injuries. N Engl J Med. 2020;383(2):129–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53(9):1618–1622. [DOI] [PubMed] [Google Scholar]
- 5.Hopewell S, Adedire O, Copsey BJ, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2018;7:CD012221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gill TM, Bhasin S, Reuben DB, et al. Effect of a Multifactorial Fall Injury Prevention Intervention on Patient Well-Being: The STRIDE Study. J Am Geriatr Soc. 2021;69(1):173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gill TM, McGloin JM, Latham NK, et al. Screening, Recruitment, and Baseline Characteristics for the Strategies to Reduce Injuries and Develop Confidence in Elders (STRIDE) Study. J Gerontol A Biol Sci Med Sci. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reuben DB, Gazarian P, Alexander N, et al. The Strategies to Reduce Injuries and Develop Confidence in Elders Intervention: Falls Risk Factor Assessment and Management, Patient Engagement, and Nurse Co-management. J Am Geriatr Soc. 2017;65(12):2733–2739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gill TM, McGloin JM, Shelton A, et al. Optimizing Retention in a Pragmatic Trial of Community-Living Older Persons: The STRIDE Study. J Am Geriatr Soc. 2020;68(6):1242–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ganz DA, Siu AL, Magaziner J, et al. Protocol for serious fall injury adjudication in the Strategies to Reduce Injuries and Develop Confidence in Elders (STRIDE) study. Inj Epidemiol. 2019;6:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McClure NS, Sayah FA, Ohinmaa A, Johnson JA. Minimally Important Difference of the EQ-5D-5L Index Score in Adults with Type 2 Diabetes. Value Health. 2018;21(9):1090–1097. [DOI] [PubMed] [Google Scholar]
- 13.Zanini A, Aiello M, Adamo D, et al. Estimation of minimal clinically important difference in EQ-5D visual analog scale score after pulmonary rehabilitation in subjects with COPD. Respir Care. 2015;60(1):88–95. [DOI] [PubMed] [Google Scholar]
- 14.Pickard AS, Law EH, Jiang R, et al. United States Valuation of EQ-5D-5L Health States Using an International Protocol. Value Health. 2019;22(8):931–941. [DOI] [PubMed] [Google Scholar]
- 15.Peduzzi P, Esserman D, Miller M, Travison T. Statistical Analysis Plan, Strategies to Reduce Injuries and Develop Confidence in Elders (STRIDE) Randomized Trial of a Multifactorial Fall injury Prevention Strategy 2020; Version 2.0:https://clinicaltrials.gov/ProvidedDocs/50/NCT02475850/SAP_000.pdf. Accessed April 10, 2022.
- 16.Yelland LN, Salter AB, Ryan P. Performance of the modified Poisson regression approach for estimating relative risks from clustered prospective data. Am J Epidemiol. 2011;174(8):984–992. [DOI] [PubMed] [Google Scholar]
- 17.Reckrey JM, Gazarian P, Reuben DB, et al. Barriers to implementation of STRIDE, a national study to prevent fall-related injuries. J Am Geriatr Soc. 2021;69(5):1334–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lamb SE, Bruce J, Hossain A, et al. Screening and Intervention to Prevent Falls and Fractures in Older People. N Engl J Med. 2020;383(19):1848–1859. [DOI] [PubMed] [Google Scholar]
- 19.Bruce J, Hossain A, Lall R, et al. Fall prevention interventions in primary care to reduce fractures and falls in people aged 70 years and over: the PreFIT three-arm cluster RCT. Health Technol Assess. 2021;25(34):1–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1:CD012424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tinetti ME, Baker DI, King M, et al. Effect of dissemination of evidence in reducing injuries from falls. N Engl J Med. 2008;359(3):252–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Campbell AJ, Robertson MC. Rethinking individual and community fall prevention strategies: a meta-regression comparing single and multifactorial interventions. Age Ageing. 2007;36(6):656–662. [DOI] [PubMed] [Google Scholar]
- 23.Delbaere K, Valenzuela T, Lord SR, et al. E-health StandingTall balance exercise for fall prevention in older people: results of a two year randomised controlled trial. BMJ. 2021;373:n740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Esserman DA, Gill TM, Miller ME, et al. A case study of ascertainment bias for the primary outcome in the Strategies to Reduce Injuries and Develop Confidence in Elders (STRIDE) trial. Clin Trials. 2021;18(2):207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Greene EJ, Peduzzi P, Dziura J, et al. Estimation of ascertainment bias and its effect on power in clinical trials with time-to-event outcomes. Stat Med. 2021;40(5):1306–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Text S1: Additional Details on Methods, and Full Acknowledgments.


