Abstract
Background
Non‐specific low back pain is a common, potentially disabling condition usually treated with self‐care and non‐prescription medication. For chronic low back pain, current guidelines recommend exercise therapy. Yoga is a mind–body exercise sometimes used for non‐specific low back pain.
Objectives
To evaluate the benefits and harms of yoga for treating chronic non‐specific low back pain in adults compared to sham yoga, no specific treatment, a minimal intervention (e.g. education), or another active treatment, focusing on pain, function, quality of life, and adverse events.
Search methods
We used standard, extensive Cochrane search methods. The latest search date was 31 August 2021 without language or publication status restrictions.
Selection criteria
We included randomized controlled trials of yoga compared to sham yoga, no intervention, any other intervention and yoga added to other therapies.
Data collection and analysis
We followed standard Cochrane methods. Our major outcomes were 1. back‐specific function, 2. pain, 3. clinical improvement, 4. mental and physical quality of life, 5. depression, and 6. adverse events. Our minor outcome was 1. work disability. We used GRADE to assess certainty of evidence for the major outcomes.
Main results
We included 21 trials (2223 participants) from the USA, India, the UK, Croatia, Germany, Sweden, and Turkey. Participants were recruited from both clinical and community settings. Most were women in their 40s or 50s. Most trials used iyengar, hatha, or viniyoga yoga. Trials compared yoga to a non‐exercise control including waiting list, usual care, or education (10 trials); back‐focused exercise such as physical therapy (five trials); both exercise and non‐exercise controls (four trials); both non‐exercise and another mind–body exercise (qigong) (one trial); and yoga plus exercise to exercise alone (one trial). One trial comparing yoga to exercise was an intensive residential one‐week program, and we analyzed this trial separately. All trials were at high risk of performance and detection bias because participants and providers were not blinded to treatment, and outcomes were self‐assessed.
We found no trials comparing yoga to sham yoga.
Low‐certainty evidence from 11 trials showed that there may be a small clinically unimportant improvement in back‐specific function with yoga (mean difference [MD] −1.69, 95% confidence interval [CI] −2.73 to −0.65 on the 0‐ to 24‐point Roland‐Morris Disability Questionnaire [RMDQ], lower = better, minimal clinically important difference [MCID] 5 points; 1155 participants) and moderate‐certainty evidence from nine trials showed a clinically unimportant improvement in pain (MD −4.53, 95% CI −6.61 to −2.46 on a 0 to 100 scale, 0 no pain, MCID 15 points; 946 participants) compared to no exercise at three months. Low‐certainty evidence from four trials showed that there may be a clinical improvement with yoga (risk ratio [RR] 2.33, 95% CI 1.46 to 3.71; assessed as participant rating that back pain was improved or resolved; 353 participants). Moderate‐certainty evidence from six trials showed that there is probably a small improvement in physical and mental quality of life (physical: MD 1.80, 95% CI 0.27 to 3.33 on the 36‐item Short Form [SF‐36] physical health scale, higher = better; mental: MD 2.38, 95% CI 0.60 to 4.17 on the SF‐36 mental health scale, higher = better; both 686 participants). Low‐certainty evidence from three trials showed little to no improvement in depression (MD −1.25, 95% CI −2.90 to 0.46 on the Beck Depression Inventory, lower = better; 241 participants). There was low‐certainty evidence from eight trials that yoga increased the risk of adverse events, primarily increased back pain, at six to 12 months (RR 4.76, 95% CI 2.08 to 10.89; 43/1000 with yoga and 9/1000 with no exercise; 1037 participants).
For yoga compared to back‐focused exercise controls (8 trials, 912 participants) at three months, we found moderate‐certainty evidence from four trials for little or no difference in back‐specific function (MD −0.38, 95% CI −1.33 to 0.62 on the RMDQ, lower = better; 575 participants) and very low‐certainty evidence from two trials for little or no difference in pain (MD 2.68, 95% CI −2.01 to 7.36 on a 0 to 100 scale, lower = better; 326 participants). We found very low‐certainty evidence from three trials for no difference in clinical improvement assessed as participant rating that back pain was improved or resolved (RR 0.97, 95% CI 0.72 to 1.31; 433 participants) and very low‐certainty evidence from one trial for little or no difference in physical and mental quality of life (physical: MD 1.30, 95% CI −0.95 to 3.55 on the SF‐36 physical health scale, higher = better; mental: MD 1.90, 95% CI −1.17 to 4.97 on the SF‐36 mental health scale, higher = better; both 237 participants). No studies reported depression. Low‐certainty evidence from five trials showed that there was little or no difference between yoga and exercise in the risk of adverse events at six to 12 months (RR 0.93, 95% CI 0.56 to 1.53; 84/1000 with yoga and 91/1000 with non‐yoga exercise; 640 participants).
Authors' conclusions
There is low‐ to moderate‐certainty evidence that yoga compared to no exercise results in small and clinically unimportant improvements in back‐related function and pain. There is probably little or no difference between yoga and other back‐related exercise for back‐related function at three months, although it remains uncertain whether there is any difference between yoga and other exercise for pain and quality of life. Yoga is associated with more adverse events than no exercise, but may have the same risk of adverse events as other exercise. In light of these results, decisions to use yoga instead of no exercise or another exercise may depend on availability, cost, and participant or provider preference. Since all studies were unblinded and at high risk of performance and detection bias, it is unlikely that blinded comparisons would find a clinically important benefit.
Plain language summary
Yoga for chronic non‐specific low back pain
Key message
For people with long‐lasting low back pain without a known cause (chronic non‐specific low back pain), after three months of doing yoga or not doing yoga, yoga is probably better than not doing exercise for improving pain and back‐related function, although the improvements are small.
There is probably little or no difference between yoga and other types of back‐focused exercise in improving back‐related function, but we are uncertain about differences between yoga and other exercise for improving pain.
Back pain was the most common harm reported in yoga trials. Risk of harms was higher with yoga than with no yoga, but similar for yoga and other exercise. There was no suggestion that yoga was associated with a risk of serious harms.
What is non‐specific low back pain?
Low back pain is a common health problem. In many cases, there is no known cause for the pain and it is termed 'non‐specific' back pain. For some people, the pain may last for three months or more and at this point it is termed 'chronic.' Non‐specific low back pain is usually treated with over‐the‐counter pain medicines and exercise, and does not require surgery or other invasive procedures. Yoga is sometimes used to help treat or manage low back pain.
What did we want to find out?
We wanted to find out if yoga improves function (for example, ability to walk, do jobs around the house, getting dressed), pain and quality of life associated with low back pain.
What did we do?
We searched medical databases for clinical trials comparing yoga practices using physical postures (often called 'hatha yoga') to any other treatment, sham (pretend) yoga, or to no treatment in adults (aged 18 years or older). We also included trials comparing yoga added to other treatments, versus those other treatments alone.
What did we find?
We included 21 trials with 2223 participants. Ten trials were carried out in the USA, five in India, two in the UK, and one each in Croatia, Germany, Sweden, and Turkey. Most participants were women in their 40s or 50s.
Key results
No trials compared yoga to sham yoga.
Ten trials compared yoga to non‐exercise, which included usual care, delayed yoga treatment, or education (e.g. booklets and lectures). Six trials compared yoga to back‐focused exercise or similar exercise programs. Five trials compared yoga, non‐exercise, and another form of exercise.
At three months, there was low‐ to moderate‐quality evidence that yoga was slightly better than no exercise in improving back function and pain, but the differences were not sufficiently important to the person with low back pain. There was low‐quality evidence for more clinical improvement with yoga. There was moderate‐quality evidence for a slight improvement in both physical (able to be active) and mental (emotional problems) quality of life and low‐quality evidence for little to no improvement in depression.
At three months, there was moderate‐quality evidence that there was little or no difference between yoga and other types of exercise in improving back function. Evidence was very‐low quality for effects on pain at three months and we remain uncertain whether there is any difference between yoga and other exercise for pain. Evidence was also of very‐low quality for clinical improvement and changes in physical and mental quality of life.
The most common harms reported in the trials were increased back pain. There was low‐quality evidence that the risk of harms was higher with yoga than with non‐exercise, and low‐quality evidence that the risk of harms was similar between yoga and back‐focused exercise. None of the trials reported yoga to be associated with a risk of serious side effects.
What are the limitations of the evidence?
Because we did not find any trials comparing yoga to sham yoga, we cannot say how yoga would affect low back pain if people did not know they were doing yoga. Participants in all the trials were aware of whether they were practicing yoga or not, and this may have influenced their interpretation of whether their back pain had changed. In addition, some trials were very small, there were few trials in some comparisons, and the trials in some comparisons had inconsistent results. Therefore, we downgraded the quality of the evidence to moderate, low, or very low.
How up to date is this evidence?
The evidence is current to August 2021.
Summary of findings
Summary of findings 1. Yoga compared to sham yoga for chronic non‐specific low back pain.
| Yoga compared to sham yoga for chronic non‐specific low back pain | ||||||
|
Patient or population: people with chronic non‐specific low back pain Settings: any Intervention: yoga Comparison: sham yoga | ||||||
| Outcomes | Anticipated absolute effects (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with sham yoga | Risk with yoga | |||||
| Back‐specific functional status | — | — | — | — | — | No relevant studies. |
| Pain | — | — | — | — | — | No relevant studies. |
| Physical quality of life | — | — | — | — | — | No relevant studies. |
| Mental quality of life | — | — | — | — | — | No relevant studies. |
| Depression | — | — | — | — | — | No relevant studies. |
| Adverse events | — | — | — | — | — | No relevant studies. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
Summary of findings 2. Yoga compared to non‐exercise for chronic non‐specific low back pain.
| Yoga compared to non‐exercise (a waiting list, a minimal intervention, or usual care) for chronic non‐specific low back pain | ||||||
|
Patient or population: people with chronic non‐specific low back pain Setting: mix of participants seeking medical care and participants in the community Intervention: yoga Comparison: non‐exercise (a waiting list, a minimal intervention [e.g. education], or usual care) | ||||||
| Outcomesa | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with non‐exercise | Risk with yoga | |||||
|
Back‐specific functional status
Assessed with RMDQ Scale 0–24, lower = better, MCID 5 points Follow‐up: 3 months |
Mean back‐specific function was 7.24 points (SD 5.45) | The MD was 1.69 points lower in the yoga group (2.73 lower to 0.65 lower) | — | 1155 (11 RCTs) | ⊕⊕⊝⊝ Lowb,c | Yoga may result in a slight improvement in back‐specific function but the difference in improvement between groups did not reach the predefined clinically relevant difference (a 5‐point reduction on the RMDQ). The corresponding risk estimated using the SMD was −0.31 (95% CI −0.50 to −0.12). |
|
Pain Assessed with numerical scale 0–100, lower = better, MCID 15 points Follow‐up: 3 months |
Mean pain was 25.24 points (SD 12.23) | The MD was 4.53 points lower in the yoga group (6.61 lower to 2.46 lower) | — | 946 (9 RCTs) | ⊕⊕⊕⊝ Moderateb | Yoga probably results in a slight reduction in pain but the difference in pain reduction between groups did not reach the predetermined clinically relevant difference (a 15‐point reduction on a 0–100 scale). |
|
Clinical improvement Assessed as participant rating that back pain was improved or resolved. Improvement measured differently in each study Follow‐up: 3 months |
195 per 1000 | 454 per 1000 (284 to 723) | RR 2.33 (1.46 to 3.71) | 353 (4 RCTs) | ⊕⊕⊝⊝ Lowb,d | Yoga may increase the risk of clinical improvement. Absolute difference 26% higher (9% higher to 53% higher); NNTB 4 (95% CI 2 to 12). |
|
Physical quality of life Assessed with physical health score on the SF‐36. Scale 0–100, higher = better Follow‐up: 3 months |
Mean physical quality of life score was 41.2 points (SD 9) | The MD was 1.80 higher in the yoga group (0.27 higher to 3.33 higher) | — | 686 (6 RCTs) | ⊕⊕⊕⊝ Moderateb | Yoga probably results in a slightly greater improvement in physical quality of life. The corresponding risk estimated using the SMD was 0.20 (95% CI 0.03 to 0.37). |
|
Mental quality of life Assessed with mental health score on the SF‐36. Scale 0–100, higher = better Follow‐up: 3 months |
Mean mental quality of life score was 44.2 points (SD 11.9) | The MD was 2.38 higher in the yoga group (0.60 higher to 4.17 higher) | — | 686 (6 RCTs) | ⊕⊕⊕⊝ Moderateb | Yoga probably results in a slightly greater improvement in mental quality of life. The corresponding risk estimated using the SMD was 0.20 (95% CI 0.05 to 0.35). |
|
Depression Assessed with: Beck Depression Inventory. Scale 0–63, lower = better Follow‐up: 3 months |
Mean depression score was 8.1 points (SD 6.58) | The MD was 1.25 lower in the yoga group (2.90 lower to 0.46 higher | — | 241 (3 RCTs) | ⊕⊕⊝⊝ Lowb,d | Yoga may result in little or no greater reduction in depression. The corresponding risk estimated using the SMD was −0.19 (95% CI −0.44 to 0.07). |
|
Adverse events (1 participant withdrew due to increased back pain) Follow‐up: up to 12 months |
9 per 1000 | 43 per 1000 (19 to 98) | RR 4.76 (2.08 to 10.89) | 1037 (8 RCTs) | ⊕⊕⊝⊝ Lowb,e | Yoga may result in an increased risk of adverse events. Absolute increase 3% (1% to 9%); NNTH 30 (95% CI 12 to 103). |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MCID: minimal clinically important difference; MD: mean difference; NNTB: number needed to treat for an additional beneficial outcome; NNTH: number needed to treat for an additional harmful outcome; RCT: randomized controlled trial; RMDQ: Roland‐Morris Disability Questionnaire; RR: risk ratio; SD: standard deviation; SF‐36: 36‐item Short Form; SMD: standardized mean difference. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aWhen there was more than one study for an outcome, we chose the control group mean from the included study that had the most representative population and the greatest weight in the meta‐analysis. For back‐specific function and pain this was Tilbrook 2011, for physical and mental quality of life this was Saper 2017, and for depression this was Williams 2009. bDowngraded one level for risk of performance and detection bias due to no blinding of the intervention. cDowngraded one level for inconsistency due to unexplained variation between studies (Chi² test statistically significant and I² > 50%). dDowngraded one level for imprecision: the number of participants in the analysis was lower than indicated in GRADE guidance (fewer than 400 participants). eThere were fewer than 300 events in the analysis, and we downgraded for imprecision.
Summary of findings 3. Yoga compared to exercise for chronic non‐specific low back pain.
| Yoga compared to exercise for chronic non‐specific low back pain | ||||||
|
Patient or population: people with chronic non‐specific low back pain Setting: mix of participants seeking medical care and participants in the community Intervention: yoga Comparison: another exercise intervention such as stretching or physical therapy | ||||||
| Outcomesa | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with another active intervention: yoga compared to exercise | Risk with yoga | |||||
|
Back‐specific functional status Assessed with RMDQ Scale 0–24, lower = better, MCID 5 points Follow‐up: 3 months |
The mean back‐specific function was 4.5 points (SD 3.8) | The MD was 0.38 points lower in the yoga group (1.33 lower to 0.62 higher) | — | 575 (4 RCTs) | ⊕⊕⊕⊝ Moderateb | Yoga probably results in little to no difference in back‐specific function compared with other exercise. The corresponding risk estimated using the SMD was −0.08 (95% CI −0.28 to 0.13). |
|
Pain
Assessed with numerical scale 0–100, lower = better, MCID 15 points Follow‐up: 3 months |
The mean pain score was 50 points (SD 21) | The MD was 2.68 points higher in the yoga group (2.01 lower to 7.36 higher) | — | 326 (2 RCTs) | ⊕⊝⊝⊝ Very lowc,d | We are uncertain whether there is any difference in pain. |
|
Clinical improvement Assessed as participant rating that back pain was improved or resolved. Improvement measured differently in each study Follow‐up: 3 months |
474 per 1000 | 460 per 1000 (341 to 621) | RR 0.97 (0.72 to 1.31) | 433 (3 RCTs) | ⊕⊝⊝⊝ Very lowc,d,e | We are uncertain whether there is any difference in the risk of clinical improvement. |
|
Physical quality of life Assessed with physical health score on the SF‐36. Scale 0–100, higher = better Follow‐up: 3 months |
The mean physical quality of life score was 40.1 points (SD 9) | The MD was 1.30 points higher in the yoga group (0.95 lower to 3.55 higher) | — | 237 (1 RCT) | ⊕⊝⊝⊝ Very lowc,d | We are uncertain whether there is any difference in physical quality of life. The corresponding risk using the SMD was 0.15 (95% CI −0.11 to 0.40). |
|
Mental quality of life Assessed with mental health score on the SF‐36. Scale 0–100, higher = better Follow‐up: 3 months |
The mean mental quality of life score was 45.2 points (SD 11.7) | The MD was 1.90 points higher in the yoga group (1.17 lower to 4.97 higher) | — | 237 (1 RCT) | ⊕⊝⊝⊝ Very lowc,d | We are uncertain whether there is any difference in mental quality of life. The corresponding risk using the SMD was 0.16 (95% CI −0.10 to 0.41). |
| Depression | — | — | — | — | — | Not reported. |
|
Adverse events Follow‐up: up to 12 months |
91 per 1000 | 84 per 1000 (51 to 139) | RR 0.93 (0.56 to 1.53) | 640 (5 RCTs) | ⊕⊕⊝⊝ Lowb,d | There may be little to no difference in adverse events between yoga and other exercise. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MCID: minimal clinically important difference; MD: mean difference; RCT: randomized controlled trial; RMDQ: Roland‐Morris Disability Questionnaire; RR: risk ratio; SD: standard deviation; SF‐36: 36‐item Short Form; SMD: standardized mean difference. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aWhen there was more than one study for an outcome, we chose the control group mean from the included study that had the most representative population and the greatest weight in the meta‐analysis. For back‐specific function this was Sherman 2011, and for pain and physical and mental quality of life this was Saper 2017. bDowngraded one level for risk of performance and detection bias due to no blinding of the intervention. cDowngraded two levels for risk of performance and detection bias due to no blinding of the intervention and attrition bias due to loss to follow‐up. dDowngraded one level for imprecision: the number of participants or events in the analysis was lower than indicated in GRADE guidance (fewer than 400 participants or fewer than 300 events). eDowngraded one level for inconsistency due to unexplained variation between studies (Chi²test statistically significant and I² > 50%).
Background
Description of the condition
Low back pain, defined as pain or discomfort in the area between the lower rib and the gluteal folds (Koes 2006), is a common condition. The latest estimate of the prevalence of low back pain from the Global Burden of Disease (GBD) study 2019 are 568 million cases worldwide, an increase of 13.5% from the estimated prevalence in 2010 (GBD 2020). The condition is responsible for 2.5% of disability‐adjusted life years (DALY) and for 63.7 million years lived with disability (YLDs) which is approximately 7.4% of YLDs worldwide (GBD 2020). Low back pain is common in men and women from youth into old age and is among the top 10 causes of DALYs from age 10 to 24 years onwards, only falling to 13th place among people aged 75 years or greater (GBD 2020). Low back pain is common in high‐income countries; in the 2018 US National Health Interview Survey (NHIS), approximately 30% of adults aged 18 years or greater reported low back pain in the past three months, an estimate that has remained stable since 2015 (NHIS 2018). However, low back pain is a global issue. When countries are classified by the sociodemographic index (SDI), a composite of income per capita, education, and fertility, low back pain is the top cause of YLDs in high, high–middle, and middle SDI countries, while it is the third cause in low–middle SDI countries and the second cause in low SDI countries (GBD 2017). Low back pain is not only associated with disability and lost working days but also high numbers of medical visits and substantial direct healthcare costs (Dagenais 2008; Lo 2020; Luckhaupt 2019).
Back pain is sometimes associated with a likely etiology (e.g. radiculopathy or spinal stenosis), but most low back pain cases are of unknown origin and are classified as mechanical or non‐specific (Will 2018). Low back pain may also be classified according to the duration of pain. Acute and subacute low back pain is pain that lasts for four weeks to less than 12 weeks and chronic low back pain is pain that lasts for 12 weeks or more (Oliveira 2018). Most episodes of low back pain improve during the first six weeks (Buchbinder 2012; Costa 2012). However, it is common for some pain and disability to persist or recur (Heuch 2013; Pengel 2003). For example, among primary care patients with low back pain, it is estimated that 26% still have pain or impaired functional status at three to six months and 21% have persistent problems at one year (Chou 2010). Meanwhile, among people with a resolved episode of low back pain, it is estimated that between 24% and 74% will have a recurrent episode within one year (Machado 2017; Pengel 2003; Stanton 2008). Research suggests that most people with low back pain experience a low or medium level of pain that is either persistent or fluctuating (Axén 2013; Kongsted 2016). Global estimates of the prevalence of chronic low back pain vary but range up to 23% (Airaksinen 2006; Balague 2012). In the 2009 to 2010 US National Health and Nutrition Examination Survey, the prevalence of chronic low back pain, defined as a history of pain occurring almost every day and lasting at least three months, was 13.1% in adults aged 20 to 69 years (Shmagel 2016). These recurrent, severe, chronic (or a combination of these) cases are responsible for much of the disability and related costs due to low back pain (Dutmer 2019; Luo 2004).
The usual treatment for low back pain is reassurance, self‐care, and non‐prescription medication. For chronic low back pain, there is some variation across guidelines, but most treatment guidelines suggest non‐steroidal anti‐inflammatory drugs, psychosocial approaches, and antidepressants when necessary, and all treatment guidelines suggest exercise therapies (Oliveira 2018). There is variation in the types (e.g. stretching, tai‐chi, yoga) and delivery modes (e.g. one‐on‐one classes, group classes) of exercise therapy that are recommended (Oliveira 2018). Guidance suggests that treatments should be tailored to the needs and preferences of the individual (NICE 2016); however, evidence showing one form of exercise is better than another is not available and there is no guidance on selecting one exercise approach over another or when specific exercise therapies are warranted (Foster 2018).
Description of the intervention
Yoga is a mind–body practice originating from ancient India that has also become popular in the West over the last century (Saper 2004). There are many branches and styles of yoga practice, with varying philosophies and practices, but all may be characterized by the integration of physical poses (asanas) and controlled breathing (pranayama), and frequently also the incorporation of meditation (dhyana) (Hayes 2010; Hewitt 2001). According to the 2007 NHIS, the use of yoga in the US increased between 2002 and 2007, and in 2007 over 13 million adults had used yoga during the previous year (Barnes 2008; Birdee 2008). According to the 2012 NHIS, the use of yoga in the US increased further in subsequent years and in 2012 over 21 million adults had used yoga during the previous year (Cramer 2016a).
Therapeutic yoga is the use of yoga to help people with health problems manage their condition and reduce their symptoms (IAYT 2016). Yoga has been suggested as being useful in managing pain and associated disability across a range of conditions, including back pain (Bussing 2012; McCall 2007). In the 2002 NHIS Alternative Medicine Supplement survey over 10 million US adults described using yoga for health reasons; 10.5% of yoga users said that their use was for musculoskeletal conditions and 76% of these users reported that the yoga was helpful (Birdee 2008). In the 2012 NHIS, 19.7% of yoga users said their use was specifically for back pain (Cramer 2016a).
How the intervention might work
Several potential benefits have been proposed in relation to the practice of yoga in persistent pain conditions, including changes in physiologic, behavioral, and psychological factors (Wren 2011). Potential mechanisms for these changes include improved flexibility and muscular strength derived from practicing the physical poses of yoga, increased mental and physical relaxation derived from practicing controlled breathing or meditation exercises, and improved body awareness gained through both the physical and mental aspects of yoga (Daubenmier 2012; Sorosky 2008).
Why it is important to do this review
Yoga is one of several complementary therapies often used to treat low back pain, and in surveys people frequently report that it is helpful (Birdee 2008; Wolsko 2003). Yoga continues to be a commonly used therapy for low back pain, a highly prevalent, recurrent, and bothersome health problem for which there are no clearly satisfactory treatments. Several new randomized controlled trials (RCTs) examining yoga for the treatment of chronic non‐specific low back pain have been completed since the initial publication of this review. Therefore, it is important to prepare an updated critical evaluation of the evidence for yoga as a treatment for low back pain, and update our initial review.
Objectives
To evaluate the benefits and harms of yoga for treating chronic non‐specific low back pain in adults compared to sham yoga, no specific treatment, a minimal intervention (e.g. education), or another active treatment, focusing on pain, function, quality of life, and adverse events.
Methods
Criteria for considering studies for this review
Types of studies
We included RCTs, including parallel, cross‐over, and cluster designs. We excluded quasi‐randomized trials. We did not restrict study eligibility by language or publication status.
Types of participants
We included trials in adults (aged 18 years or greater) with current chronic non‐specific low back pain. We defined chronic low back pain as pain with a duration of three months or more (Chou 2007; van Tulder 2006). In our description of population and setting, we specified whether the participants were recruited from populations seeking medical care or from the community.
Types of interventions
We included studies of yoga as an intervention for low back pain. The study was required to specify that the intervention was 'yoga.' We excluded interventions based on yoga (e.g. stretching exercises based on yoga) but not characterized as yoga. We did not restrict studies according to the yoga tradition used, or according to the class length, frequency, or duration of the yoga intervention. However, we excluded studies examining yogic meditation or a yoga lifestyle without a physical practice component.
We included studies comparing yoga to any other intervention or to no intervention. We also included any studies comparing yoga as an adjunct to other therapies, versus those other therapies alone. The comparisons of interest were:
yoga versus a sham yoga intervention;
yoga versus no treatment or a waiting list, a minimal intervention (e.g. booklets, lectures, or other educational interventions), or usual care (i.e. yoga compared to no specific intervention);
yoga versus another active intervention (e.g. yoga versus drugs), for which different types of active interventions were considered separately (e.g. yoga versus drugs, yoga versus manipulation) (i.e. yoga compared to exercise controls); and
yoga plus an intervention versus that intervention alone, for which different types of co‐intervention were considered separately (e.g. yoga plus drugs versus drugs alone, yoga plus exercise versus exercise alone).
Studies with co‐interventions were allowed, if the co‐interventions were comparable between intervention groups (e.g. both groups were allowed the use of pain relief medications).
Types of outcome measures
We chose outcome measures that were important in assessment of low back pain, so that this review may produce results that are easily compared to or combined with those of other systematic reviews of treatment for low back pain. All outcomes were assessed at short‐term (closest to four weeks), short–intermediate term (closest to three months), intermediate‐term (closest to six months), and long‐term (closest to 12 months) time points.
Major outcomes
Back‐specific functional status (e.g. as measured by the Roland‐Morris Disability Questionnaire [RMDQ])
Pain (e.g. as measured by the visual analog scale [VAS] for pain)
Clinical improvement (as defined by each study)
Measures of mental or physical quality of life (e.g. as measured on the 36‐item Short Form [SF‐36])
Depression (as measured by each study)
Adverse events
Minor outcomes
Measures of work disability
The suggested threshold for a minimal clinically important difference (MCID) on the RMDQ is a 5‐point reduction or a 30% reduction from baseline (Jordan 2006), and the suggested threshold for a MCID on a 0‐ to 100‐point VAS scale measuring pain is a 15‐point reduction or a 30% reduction from baseline (Ostelo 2008). We acknowledge that the MCID is intended to measure the change in individual patients and not changes within or between groups (Chung 2017). However, current definitions for moderate effect size based on mean between‐group differences are similar (i.e. a moderate effect is greater than 2 to 5 points on the RMDQ and 10 to 20 points on a 0‐ to 100‐ point VAS scale measuring pain) (Chou 2017). In the absence of established MCID values for between‐group differences, we used the threshold of 5 points between‐group difference on the RMDQ and 15 points between‐group difference on a 0‐ to 100‐point VAS scale to estimate the clinical importance of effect estimates.
Search methods for identification of studies
Electronic searches
We used the search methods recommended by Lefebvre 2011 and Furlan 2015a to search the following databases from inception to 31 August 2021 without restrictions to language or publication status:
Cochrane Back and Neck group Trials Register (CRS web; 31 August 2021; Appendix 1);
Cochrane Complementary Medicine Field Trials Register (CRS web; 31 August 2021; Appendix 2);
Cochrane Central Register of Controlled Trials (CENTRAL, searched via CRS Web; 31 August 2021; Appendix 1);
MEDLINE (Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R)) (OvidSP, 1946 to 31 August 2021; Appendix 1);
Embase (OvidSP, 1980 to 2021 week 34) and Embase Classic+Embase (OvidSP, 1947 to 31 August 2021; Appendix 1);
Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO, 1981 to 31 August 2021; Appendix 1);
PsycINFO (OvidSP, 2002 to May week 4 2019; APA, 1806 to August Week 4 2021 Appendix 2);
Allied and Complementary Medicine Database (AMED) (OvidSP, 1985 to 31 August 2021; Appendix 2);
IndMED (indmed.nic.in/; last searched 2018; Appendix 2);
US National Institutes of Health ClinicalTrials.gov (31 August 2021; Appendix 2);
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP; 31 August 2021 Appendix 2).
In 2018, we began searching MEDLINE (Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R)), which allows multiple MEDLINE databases to be searched through one Ovid interface. In 2018, we began searching CENTRAL, the Cochrane Back and Neck group Trials Register and the Complementary Medicine Field Trials Register through CRS Web. We have not been able to access the IndMED database since 2018. PsycINFO's provider changed from OvidSP to APA in 2020.
Searching other resources
We screened the reference lists of included studies and contacted experts in the field (e.g. authors of included studies) for information on additional trials, including unpublished or ongoing studies.
Data collection and analysis
Selection of studies
Two review authors (LSW and NS or SH) independently screened the titles and abstracts of the references retrieved from updated searches. We obtained the full text for references that either author considered to be potentially relevant. Two review authors (LSW and NS, SH, or RV) independently assessed the full‐text references for inclusion according to the Criteria for considering studies for this review. When study reports were unclear about inclusion or exclusion criteria, one review author (LSW, NS, or RV) contacted the study authors for clarification. We resolved disagreements by consensus or by consultation with a third review author (NS or SH).
Data extraction and management
One review author (LSW) used a standardized and pilot‐tested form to extract data on study characteristics, and a second review author (NS) checked these data. Two review authors (LSW and KP) independently extracted data on funding or sponsorship.
Two review authors (LSW, NS) used a standardized and pilot‐tested form to independently extract data on outcomes for each trial. If key information was missing from the study report, we contacted the study authors to obtain the information, and reported the results of these contacts in the Notes section of the Characteristics of included studies table. When studies reported back‐related function using multiple scales, we extracted data from, in order of preference, the RMDQ and the Oswestry Disability Index or Oswestry Low Back Pain Disability Questionnaire. When studies reported pain data on a scale other than 0 to 100 (e.g. 0 to 5, 0 to 10) we transformed the data into a 0 to 100 scale. When both endpoint and change data were available, we used endpoint data in our primary analysis. In cases where neither endpoint nor change data were available, one review author (RV) used Plot Digitizer to extract endpoint values from figures (Jelicic Kadic 2016). We used these values together with the baseline standard deviation (SD) in our primary analysis. In cases where study participants were lost to follow‐up and intention‐to‐treat analyses were conducted using imputation alongside available‐case analyses, we used the imputed data for our primary analysis. In cases where both unadjusted and adjusted data were available, we used the adjusted data for our primary analysis. We resolved disagreements on dually extracted information by consensus.
Assessment of risk of bias in included studies
Two review authors (LSW, KP) independently assessed the risk of bias for each included study using the 13 risk of bias items recommended by the Cochrane Neck and Back group (Furlan 2015a). These items are an adaptation of the risk of bias criteria described in the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2011a). The description of each item and how to rate each item as 'low risk of bias,' 'high risk of bias,' or 'unclear risk of bias' are presented in Table 4 and Table 5. For rating compliance, we considered trials to be at low risk of bias if at least 50% of yoga participants were reported to have attended at least 50% of classes. Disagreements on risk of bias were resolved by consensus.
1. Sources of risk of bias.
| Bias domain | Source of bias | Possible answers |
| Selection | (1) Was the method of randomization adequate? | Yes/No/Unsure |
| Selection | (2) Was the treatment allocation concealed? | Yes/No/Unsure |
| Performance | (3) Was the patient blinded to the intervention? | Yes/No/Unsure |
| Performance | (4) Was the care provider blinded to the intervention? | Yes/No/Unsure |
| Detection | (5) Was the outcome assessor blinded to the intervention? | Yes/No/Unsure |
| Attrition | (6) Was the dropout rate described and acceptable? | Yes/No/Unsure |
| Attrition | (7) Were all randomized participants analyzed in the group to which they were allocated? | Yes/No/Unsure |
| Reporting | (8) Are reports of the study free of suggestion of selective outcome reporting? | Yes/No/Unsure |
| Selection | (9) Were the groups similar at baseline regarding the most important prognostic indicators? | Yes/No/Unsure |
| Performance | (10) Were co‐interventions avoided or similar? | Yes/No/Unsure |
| Performance | (11) Was the compliance acceptable in all groups? | Yes/No/Unsure |
| Detection | (12) Was the timing of the outcome assessment similar in all groups? | Yes/No/Unsure |
| Other | (13) Are other sources of potential bias unlikely? | Yes/No/Unsure |
2. Criteria for a judgment of 'Yes' for the sources of risk of bias.
| 1 | A random (unpredictable) assignment sequence. Examples of adequate methods are coin toss (for studies with 2 groups), rolling a dice (for studies with ≥ 2 groups), drawing of balls of different colors, drawing of ballots with the study group labels from a dark bag, computer‐generated random sequence, preordered sealed envelopes, sequentially ordered vials, telephone call to a central office, and preordered list of treatment assignments. Examples of inadequate methods are: alternation, birth date, social insurance/security number, date in which they are invited to participate in the study, and hospital registration number. |
| 2 | Assignment generated by an independent person not responsible for determining the eligibility of the participants. This person has no information about the people included in the trial and has no influence on the assignment sequence or on the decision about eligibility of the participant. |
| 3 | Index and control groups are indistinguishable for the participants or if the success of blinding was tested among the participants and it was successful. |
| 4 | Index and control groups are indistinguishable for the care providers or if the success of blinding was tested among the care providers and it was successful. |
| 5 | Adequacy of blinding should be assessed for each major outcome separately. This item should be scored 'yes' if the success of blinding was tested among the outcome assessors and it was successful or:
|
| 6 | The number of participants who were included in the study but did not complete the observation period or were not included in the analysis must be described and reasons given. If the percentage of withdrawals and dropouts does not exceed 20% for short‐term follow‐up and 30% for long‐term follow‐up and does not lead to substantial bias a 'yes' is scored. (Note: these percentages are arbitrary, not supported by literature.) |
| 7 | All randomized participants are reported/analyzed in the group they were allocated to by randomization for the most important moments of effect measurement (minus missing values) irrespective of non‐compliance and co‐interventions. |
| 8 | All the results from all prespecified outcomes have been adequately reported in the published report of the trial. This information is either obtained by comparing the protocol and the report, or in the absence of the protocol, assessing that the published report includes enough information to make this judgment. |
| 9 | Groups have to be similar at baseline regarding demographic factors, duration and severity of complaints, percentage of participants with neurologic symptoms, and value of main outcome measure(s). |
| 10 | If there were no co‐interventions or they were similar between the index and control groups. |
| 11 | The reviewer determines if the compliance with the interventions is acceptable, based on the reported intensity, duration, number and frequency of sessions for both the index intervention and control intervention(s). For example, physiotherapy treatment is usually administered for several sessions; therefore, it is necessary to assess how many sessions each participant attended. For single‐session interventions (e.g. surgery), this item is irrelevant. |
| 12 | Timing of outcome assessment should be identical for all intervention groups and for all major outcome measures. |
| 13 | Other types of biases. For example:
|
Lack of allocation concealment, failure to blind participants and outcome assessors, and a high dropout rate or a marked difference between intervention groups in numbers of dropouts or reasons for dropout are all empirically associated with bias (Furlan 2015a). For this review, we used the ratings of risk of bias to produce a summary of the risk of bias in each study across five domains: selection bias, performance bias, detection bias, attrition bias, and reporting bias (Higgins 2017). We expected most studies to have a high risk of performance and detection bias because the yoga intervention cannot be blinded and we expected most outcomes to be self‐reported. We classified studies as having a high risk of bias if they had a high or unclear risk of selection bias, high or unclear risk of attrition bias, or a high risk of reporting bias. We conducted a sensitivity analysis for the major outcomes to explore the effects of including and excluding trials at high risk of bias (Sensitivity analysis).
Measures of treatment effect
We analyzed dichotomous outcomes (i.e. overall clinical improvement, adverse events) by calculating the risk ratio (RR) with 95% confidence intervals (CI). We analyzed continuous outcomes (i.e. back‐related function, pain, quality of life, depression) by calculating the mean difference (MD) when studies used the same scale or standardized mean difference (SMD) when studies used different scales, with 95% CIs. When we calculated SMDs, we did not combine endpoint and change values (Deeks 2011). We considered a minimum clinically important change on the 0 to 100 pain scale to be 15 (Ostelo 2008). For non‐pain outcomes, we used Cohen's three levels for the size of between‐group effects to classify the effect estimates as small (SMD at least 0.2 but less than 0.5), medium (SMD from 0.5 to less than 0.8), or large (SMD 0.8 or greater) (Cohen 1988). We additionally used the original scale to report the MD for results when the effects were based upon a single study or multiple studies using the same scale. When the effects were based upon multiple studies using different scales, we chose a representative study or studies using a single familiar scale, calculated the pooled SD of all studies using the familiar scale, and used this information to re‐express the SMD in MD units of that familiar scale (Schünemann 2019). We also reported the absolute and relative percent differences using the single familiar scale. Finally, we used the Dr Chris Cates' Visual Rx (www.nntonline.net/visualrx/) to calculate the number needed to treat for an additional beneficial outcome (NNTB) or an additional harmful outcome (NNTH) for all dichotomous estimates that were statistically significant. Measures of treatment effect are considered significant when P was less than 0.05 or the 95% CI excluded one (for the RR) or zero (for the MD or SMD).
Unit of analysis issues
We planned to follow the guidance on cluster‐randomized or cross‐over trials in Chapters 16.3 and 16.4 of the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2011b), but we did not find any cluster‐randomized or cross‐over trials to include in this review.
Dealing with missing data
We contacted the first author or primary investigator for trials in which data for key study characteristics or major outcomes were missing or incomplete.
Assessment of heterogeneity
We assessed clinical heterogeneity (i.e. differences in study populations, interventions, and outcomes) between studies qualitatively. For studies that we judged to have sufficient clinical homogeneity to combine in a meta‐analysis, we assessed statistical heterogeneity using the I² statistic, which describes the percentage of the variability in the effect estimate that is due to clinical or methodologic heterogeneity rather than to chance. An I² value of 30% to 60% may represent moderate heterogeneity, a value of 50% to 90% may represent substantial heterogeneity, and a value of 75% to 100% may represent considerable heterogeneity (Deeks 2011).
Assessment of reporting biases
We used funnel plots to assess the potential for small‐study bias in meta‐analyses that included at least 10 studies. We assessed the possibility of selective outcome reporting for each study as part of the risk of bias assessment.
Data synthesis
When the population, interventions, outcomes, and time of assessment were clinically comparable across trials, we carried out a meta‐analysis using Review Manager 5 (Review Manager 2014). We used a random‐effects model because we expected some between‐study variation. When the data were considered not sufficiently clinically similar to be combined in a meta‐analysis, we described the results from clinically comparable trials using narrative synthesis methods.
Regardless of whether sufficient data were available to use quantitative analyses to summarize the data, two review authors (LSW, NS) independently assessed the overall certainty of the evidence for each comparison/outcome, using the GRADE approach and GRADEpro GDT (GRADEpro GDT), as recommended in the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2011b; Schünemann 2019), and adapted in the updated Cochrane Back and Neck group method guidelines (Furlan 2015a). Factors that may decrease the certainty of the evidence are: study design and risk of bias, inconsistency of results, indirectness (not generalizable), imprecision (sparse data), and other factors (e.g. suspicion of publication bias). The certainty of the evidence for a specific outcome was reduced one to two levels, according to the performance of the studies against each of these five factors. The factors and criteria are outlined in Appendix 3 (Furlan 2015b). We resolved disagreements between review authors by discussion. We reported the GRADE certainty of the evidence in the Results and summary of findings tables.
Subgroup analysis and investigation of heterogeneity
We did not identify studies that tested yoga interventions clearly omitting a mind component (i.e. studies that tested only the physical practice component of yoga and did not include meditation, relaxation, or breathing exercises). Therefore, we were unable to conduct planned subgroup analyses to evaluate the differences in outcomes between yoga interventions with and without a mind component. We were unable to carry out planned subgroup analyses of trials conducted with participants who had major comorbidities (e.g. heart disease) versus trials conducted with participants who did not have these major comorbidities, as data for this subgroup analysis were not available. We planned to carry out a subgroup analysis of trials conducted with lower socioeconomic status (SES) or lower‐educated populations versus higher SES or higher‐educated populations, and identified two trials with participants specifically recruited from a lower SES or lower‐educated population (Saper 2009; Saper 2017). When both trials were present in an analysis, we used a significance test to investigate whether there were statistically significant differences in outcomes between subgroups.
We planned to carry out a subgroup analysis of trials conducted in older (mean age 65 years or greater) versus younger populations, and identified one trial conducted in an older population (Teut 2016). However, to use a significance test to investigate whether a subgroup variable is associated with a statistically significant difference in outcomes between subgroups, it is necessary to have at least two trials in each subgroup (Deeks 2001), thus, this test was not appropriate.
Sensitivity analysis
For pain and function, we compared analyses including and excluding trials at high risk of bias (as defined in Assessment of risk of bias in included studies) to explore the impact of risk of bias on estimates of treatment effects. We also used sensitivity analyses to explore the effects of using imputed versus available‐case data, and the effects of using endpoint versus change data.
Summary of findings and assessment of the certainty of the evidence
We prepared summary of findings tables for the main comparisons of yoga versus non‐exercise controls and yoga versus other exercise controls to present the estimates of effects and certainty of the evidence for all major outcomes of back‐related function, pain, clinical improvement, physical quality of life, mental quality of life, depression, and adverse events. We chose the short–intermediate follow‐up (closest to three months) for the summary of findings tables as we believe this is the earliest clinically significant time point for observing outcomes in people with a chronic condition. When we reported the results from an analysis using the SMD, we re‐expressed the SMD in MD units of a familiar scale. We reported the adverse events in the summary of findings tables as of the longest available time point from each study, as we wished to capture all available information on adverse events.
Results
Description of studies
Results of the search
The flow of studies is presented in the PRISMA chart in Figure 1.
1.
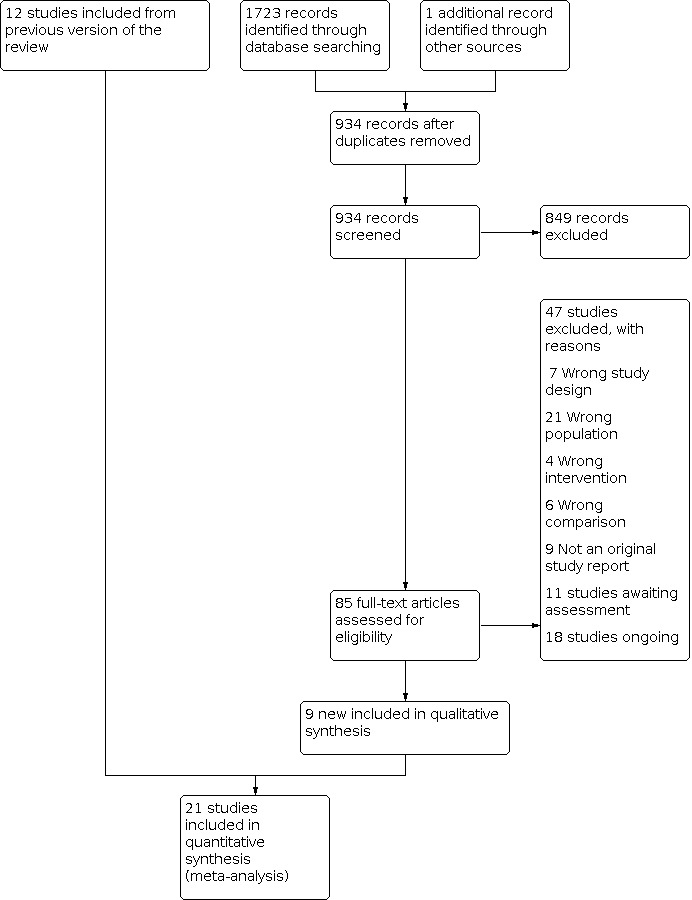
Study flow diagram.
The searches retrieved 1724 records. After removing duplicates, we screened 934 titles and abstracts and 85 full‐text articles. We identified eight new studies from our recent searches (Bramberg 2017; Demirel 2019; Groessl 2017; Highland 2018; Kuvacic 2018; Patil 2018; Saper 2017; Teut 2016), one new study through contact with an expert (Neyaz 2019), and included the 12 studies from the previous version of the review (Cox 2010; Galantino 2004; Jacobs 2004; Nambi 2014; Saper 2009; Sherman 2005; Sherman 2011; Tekur 2008; Tilbrook 2011; Wattamwar 2013; Williams 2005; Williams 2009) for a total of 21 included studies (63 publications). Many studies are associated with multiple references. In all cases the study rather than the reference was the unit of interest in the review. We excluded 47 studies. Eleven studies (15 publications) are awaiting classification and 18 are ongoing. We will review and incorporate them into the next update.
Included studies
We included 21 parallel RCTs (2223 participants). Ten studies were conducted in the USA (Galantino 2004; Groessl 2017; Highland 2018; Jacobs 2004; Saper 2009; Saper 2017; Sherman 2005; Sherman 2011; Williams 2005; Williams 2009; 1123 participants); five were conducted in India (Nambi 2014; Neyaz 2019; Patil 2018; Tekur 2008; Wattamwar 2013; 322 participants); two were conducted in the UK (Cox 2010; Tilbrook 2011; 333 participants); and one conducted in each of Croatia (Kuvacic 2018; 30 participants), Germany (Teut 2016; 176 participants), Sweden (Bramberg 2017; 159 participants), and Turkey (Demirel 2019; 80 participants). Seventeen studies were clearly carried out between 2001 and 2017; four studies did not report the dates of study conduct (Demirel 2019; Galantino 2004; Kuvacic 2018; Wattamwar 2013). All trials were published in English.
We provided details about each included trial in the Characteristics of included studies table. We have also provided detailed information about the study populations, study interventions and comparisons, and the intervention design and delivery in additional tables (Table 6; Table 7; Table 8; Table 9).
3. Baseline characteristics of study populations.
| Study | Total number randomized | Participant age (mean in years) | Sex (% women) | Race/ethnicity (% for categories in study) | Education (% for categories in study, or as reported) |
| Bramberg 2017 | 159 | 45.7 (SD 10.3)a | 75%a | — | Compulsory school < 10%; upper secondary school about 50%; university/university college about 40% |
| Cox 2010 | 20 | 45 | 65% | — | — |
| Demirel 2019 | 80 | 44.9 (SD 10.6)a | 80.5% | — | — |
| Galantino 2004 | 22 | — | 80%a | — | — |
| Groessl 2017 | 150 | 53.4 (SD 13.2) | 25% | African‐American or Black 17%; White 49%; Native American 1.3%; Hispanic 20%; Asian/Pacific Islander 6%; other 6% | Grade school 0.7%; high school diploma/General Educational Development 6.8%; some college 38%; college graduate 31%; postgraduate 23% |
| Highland 2018 | 68 | 44.3 (SD 12.7) | 63% | White 63%; Black 22%; not specified 15%a | — |
| Jacobs 2004 | 52 | 43.4 (range 25–65) | — | White 63.5%; Black 15.4%; Hispanic 3.8%; Asian 9.62%; other 1.9% | Median education = college graduate |
| Kuvacic 2018 | 30 | 34.2 (range 25–42) | 47% | — | Elementary school 0; middle school 3 (10%); high school 8 (27%); university education 19 (63%) |
| Nambi 2014 | 60 | 43.9 (SD 8.9)a | 53%a | — | — |
| Neyaz 2019 | 70 | 35.9 (SD 10.6) | 50% | — | — |
| Patil 2018 | 88 | 32.1 (SD 3.6)a | 100% | — | Auxiliary nursing midwifery 11 (13%); general nursing midwifery 60 (68%); Bachelor of nursing 17 (19%) |
| Saper 2009 | 30 | 44 (SD 12) | 83% | White 24%; Black 70%; Asian 3%; native American 3%; Hispanic 13% | College graduate 24%; some college 43%; high school graduate or less 33% |
| Saper 2017 | 320 | 46 (SD 10.7)a | 63.8%a | Non‐Hispanic White 57 (17.8%); Non‐Hispanic Black 183 (57.2%); Hispanic 44 (13.8%); other/missing 36 (11.3%)a | Earned college degree or higher 93 (29.1%)a |
| Sherman 2005 | 101 | 44 (SD 13) | 66% | White 80% | Attended some college 97% |
| Sherman 2011 | 228 | 48.4 (SD 9.8) | 64% | White 87% | College graduate 62% |
| Tekur 2008 | 80 | 48.5 (SD 3.8)a | 45%a | — | Postgraduate 21%; college 51%; high school 28% |
| Teut 2016 | 176 | 73 (SD 5.6) | 89% | — | > 10 years of school 15 (36.9%) |
| Tilbrook 2011 | 313 | 46.3 (SD 11.4)a | 70%a | — | Completed further education since leaving school, college, or university 58% |
| Wattamwar 2013 | 24 | 34a | — | — | — |
| Williams 2005 | 60 | 48.3 (SD 7.1)a,b | 68%a,b | Caucasian 91%; African‐American 5%; Asian 2%; Native American 2%a,b | College 75%; high school 25%a,b |
| Williams 2009 | 90 | 48.0 (SD 1.17) | 76.7% | White 93.3%; African‐American 2.2%; Asian‐American 4.4% | College graduate 73%; some college or less 27% |
aCalculated from information in the publication. bData provided for completers only.
SD: standard deviation.
4. Interventions and comparisons.
| Study | Yoga intervention(s) | Comparison intervention(s) | Restricted co‐interventions | Duration of treatment | Duration of follow‐up |
| Bramberg 2017 | Yoga classes of 60 min held twice per week for 6 weeks + suggested home practice at least twice per week. Self‐care advice. | 2 groups
|
— | 6 weeks | 12 months |
| Cox 2010 | Yoga classes of 75 min held once per week for 12 weeks + suggested home practice. Booklet on how to manage back pain. Usual care. | Booklet on how to manage back pain. Usual care. | — | 12 weeks | 12 weeks |
| Demirel 2019 | Yoga classes of 60 min held 3 times per week for 6 weeks. Usual care. | Stabilization exercise classes of 60 min held 3 times per week for 6 weeks. Usual care. | — | 6 weeks | 6 weeks |
| Galantino 2004 | Yoga classes of 60 min held twice per week for 6 weeks + home practice of 1 hour per day. Usual care. | Usual care. | Changes in pain medication not allowed during study. | 6 weeks | 3 months (yoga participants only) |
| Groessl 2017 | Yoga classes of 60 min held twice per week for 12 weeks + home practice of 15–20 min on days when there are not classes. Usual care. | Usual care. Asked not to practice yoga until after follow‐up. | — | 12 weeks | 6 months |
| Highland 2018 | Individual yoga classes of 60 min held twice per week in weeks 1–4 and once per week in weeks 5–8. Usual care. | Usual care. | — | 8 weeks | 6 months |
| Jacobs 2004 | Yoga classes of 90 min held twice per week for 12 weeks, + home practice of 30 min for 5 days/week. Usual care. | Waiting list for yoga. Usual care + a 'back pain educational booklet.' | — | 12 weeks | 6 months |
| Kuvacic 2018 | Yoga classes of 75 min held twice per week for 8 weeks. "Education on spine anatomy/ biomechanics and the management of CLBP [chronic low back pain]." | Pamphlet with recommendations for posture, movement, and breathing. Newsletter twice per week. | — | 8 weeks | 8 weeks |
| Nambi 2014 | Yoga classes of 60 min held once per week for 4 weeks, + home practice of 30 min for 5 days/week. 1‐hour lecture and handouts on physiotherapy for chronic low back pain, 2 weeks before beginning of intervention period. | Individually prescribed exercises for 4 weeks, beginning with 3 days/week and increasing to 5 days/week. 1‐hour lecture and handouts on physiotherapy for chronic low back pain, 2 weeks before beginning of intervention period. | Exercise group participants asked not to participate in any other exercises for low back pain. | 4 weeks | 7 months |
| Neyaz 2019 | Yoga classes of 35 min held once per week for 6 weeks + home practice of 30 min on non‐class days + continued home practice for an additional 6 weeks. Education regarding posture. | Conventional therapeutic exercise classes of 35 min held once per week for 6 weeks + home practice of 30 min on non‐class days + continued home practice for an additional 6 weeks. Education regarding posture. | — | 6 weeks | 12 weeks |
| Patil 2018 | Yoga classes of 60 min held 5 times per week for 6 weeks. | Physical exercise sessions of 60 min held 5 times per week for 6 weeks. | — | 6 weeks | 6 weeks |
| Saper 2009 | Yoga classes of 75 min held once per week for 12 weeks + 30 min/day home practice. A copy of The Back Pain Helpbook and usual care. | Waiting list for yoga. A copy of The Back Pain Helpbook and usual care. | Participants were discouraged from beginning any new back pain treatments during the study. | 12 weeks | 26 weeks |
| Saper 2017 | Yoga classes of 75 min held once per week for 12 weeks + 30 min/day home practice on non‐class days. Usual care. | 2 groups:
|
— | 12 weeks followed by re‐randomization to different intervention maintenance conditions for an additional 40 weeks | 52 weeks |
| Sherman 2005 | Yoga classes of 75 min held once per week for 12 weeks + daily home practice. Usual care. | 2 groups
|
— | 12 weeks | 26 weeks |
| Sherman 2011 | Yoga classes of 75 min held once per week for 12 weeks + 20 min of home practice on non‐class days. Usual care. | 2 groups
|
— | 12 weeks | 26 weeks |
| Tekur 2008 | Intensive 1‐week residential yoga program, including approximately 2 hours of yoga‐based special techniques (e.g. postures) per day as well as yogic meditation, breathing, chanting, and lectures. | Intensive 1‐week residential program of non‐yogic physical exercises and education. | — | 7 days | 7 days |
| Teut 2016 | 24 × 45‐min yoga classes held over 3 months. | 2 groups
|
No physiotherapy or pain medication acting on central nervous system. | 3 months | 6 months |
| Tilbrook 2011 | 1 × 75‐min yoga class once per week for 12 weeks + 30 min/day practice or practice ≥ 2 times/week. Booklet on managing back pain. Usual care. | Book or booklet (The Back Book) on managing back pain. Usual care. | — | 12 weeks | 12 months |
| Wattamwar 2013 | 1 × 45‐ to 60‐min yoga session per week for 10 weeks. 2 × 45‐ to 60‐min occupational therapy sessions per week for 10 weeks, with some simple asanas and pranayama added. Home practice of back exercises with additional simple asanas and pranayama was suggested. | 3 × 45‐ to 60‐min occupational therapy sessions per week for 10 weeks, + a home program of back exercises. | — | 10 weeks | 10 weeks |
| Williams 2005 | 1 × 90‐min yoga class per week for 16 weeks, + home practice 30 min/day for 5 days/week. 16 weekly newsletters on back care. Usual care. Prior to study start, 2 × 1‐hour lectures on low back pain and some instructional handouts. | 16 weekly newsletters on back care. Prior to study start, 2 × 1‐hour lectures on low back pain and some instructional handouts. Usual care. | Participants were only eligible for the study if they agreed to forgo other forms of complementary and alternative medicines treatment during the study. | 16 weeks | 7 months |
| Williams 2009 | 2 × 90‐min yoga classes per week for 24 weeks, + home practice 30 min/day on non‐class days. | Waiting list for yoga. Usual care. | Participants were only eligible for the study if they agreed to forgo chiropractic, massage, Pilates, acupuncture, or any other yoga treatment during the study. | 24 weeks | 48 weeks |
min: minute.
5. Yoga intervention – type, components and design a.
| Study | Type of yoga | Components of yoga intervention | How yoga intervention was designed |
| Bramberg 2017 | Kundalini yoga | Postures (Asanas) Breathing (Pranayama) Relaxation Mental focus |
Quote: "A prestructured standardized kundalini yoga programme adapted for back pain was used." |
| Cox 2010 | Iyengar yoga | Postures (Asanas) Breathing (Pranayama) Relaxation Mental focus |
Quote: "[D]evised by an iyengar yoga teacher (IYAUK) and LBP [low back pain] yoga specialist, in collaboration with a British Wheel of Yoga teacher (BWY), who delivered the intervention. The structure was based on that previously used in the US Karen Sherman yoga trial, … whilst ensuring that a common ground was found between the two associations of IYAUK and BWY. Other influences included Geeta and B.K.S. iyengar, who has taught yoga for over 70 years and has applied therapeutic variations of classical poses to many health problems including LBP." |
| Demirel 2019 | — | Postures (Asanas) Breathing (Pranayama) Philosophy |
— |
| Galantino 2004 | Hatha yoga | Postures (Asanas) Breathing (Pranayama) Relaxation Ethics (Yamas and Niyamas) |
Quote: "An expert panel of two hatha yoga instructors with greater than 10 years of experience and a physical therapist specializing in spine treatment established an initial yoga protocol for this study. Postures were selected based on orthopedic biomechanics." |
| Groessl 2017 | Hatha yoga | Postures (Asanas) Breathing (Pranayama) Meditation Mental focus |
Quote: "[T]he yoga intervention that will be tested in the proposed RCT [randomized controlled trial] will be very similar to the yoga currently provided in the clinical yoga program that has been specifically tailored to the needs of veterans with CLBP [chronic low back pain]." Comment: unclear how program was developed. |
| Highland 2018 | "Based on therapeutic yoga" | Postures (Asanas) Breathing (Pranayama) Meditation |
Quote: "Yoga‐treatment researchers and experts developed a 50‐hour RESTORE yoga teacher training program. RESTORE is based on therapeutic yoga, targeting major muscles affected by chronic LBP [low back pain],… including back and core strengthening/stretching for postural alignment." |
| Jacobs 2004 | Iyengar style of hatha yoga | Postures (Asanas) Breathing (Pranayama) Relaxation Mental focus |
Comment: a panel of experts developed the yoga intervention. Quote: "The panel included 8 senior iyengar yoga instructors of national and international recognition with greater than 10 years experience teaching yoga. The protocol was constructed by consensus after 2 meetings and several months of discussion." |
| Kuvacic 2018 | — | Postures (Asanas) Breathing (Pranayama) Relaxation (Yoga Nidra) Meditation (Vipassana) |
Quote: "Contemporary yoga practices suited to CLBP [chronic low back pain]." |
| Nambi 2014 | Iyengar yoga | Postures (Asanas) Relaxation |
— |
| Neyaz 2019 | "Integrated yoga therapy module … developed from traditional hatha practices" | Postures (Asanas) Breathing (Pranayama) Relaxation Meditation Yoga philosophy |
Quote: "An integrated Yoga therapy module for CNLBP was developed from traditional hatha yoga practices, in collaboration with CIMR [Centre for Integrative Medicine and Research]." |
| Patil 2018 | Integrated approach of yoga therapy (IAYT) | Postures (Asanas) Breathing (Pranayama) Relaxation Meditation |
Quote: "A 1h integrated yoga therapy module (IYTM) was designed after reviewing the literature in the field of yoga and LBP by utilizing the components of yoga at the body, subtle energy, and mind level, respectively. The designed IYTM was validated by subject experts." |
| Saper 2009 | Hatha yoga | Postures (Asanas) Breathing (Pranayama) Relaxation |
Quote: "To design the protocol, we performed a systematic search of the peer‐reviewed and lay literature on yoga for low back pain. We collected and distributed this literature to an expert panel with a broad range of experience in different yoga styles. After reviewing the literature, the panel met and synthesized information from the literature with their professional experience to draft a protocol that was subsequently refined iteratively through discussion, consensus, and use in nonstudy yoga classes." |
| Saper 2017 | Hatha yoga | Postures (Asanas) Breathing (Pranayama) Relaxation Yoga philosophy |
Quote: "A manualized yoga protocol of 12 weekly 75‐minute classes was adapted from previous studies in similar populations with input from expert yoga instructors, investigators, and former study participants (Table 2 of Supplement 2)." |
| Sherman 2005 | Viniyoga | Postures (Asanas) Breathing (Pranayama) Relaxation Mental focus |
Quote: "Our class instructor and a senior teacher of viniyoga, who has written a book about its therapeutic uses …, designed the yoga intervention for patients with back pain who did not have previous yoga experience." |
| Sherman 2011 | Viniyoga | Postures (Asanas) Breathing (Pranayama) Relaxation |
Used intervention developed by the class instructor and senior viniyoga teacher for previous trial. The developers are named and acknowledged in the protocol publication for this trial. |
| Tekur 2008 | 'Integrated Approach of Yoga Therapy (IAYT)' | Postures (Asanas) Breathing (Pranayama) Relaxation Meditation Mental focus Chanting Yoga philosophy/lifestyle |
Quote: "The specific 'integrated yoga therapy module for low back pain' was developed by a team of two yoga experts and a physiatrist. The concepts of the modules were taken from traditional yoga scriptures (patanjali yoga sutra, and yoga vasishtha) that highlight a holistic approach to health management at physical, mental, emotional and intellectual levels." |
| Teut 2016 | Viniyoga | Postures (Asanas) Breathing (Pranayama) Concentration |
Quote: "The classes were developed by a group of experienced viniyoga teachers during a consensus process." |
| Tilbrook 2011 | Iyengar and British Wheel of Yoga (described as hatha yoga on the website) | Postures (Asanas) Breathing (Pranayama) Relaxation Mental focus Yoga philosophy/lifestyle |
Quote from protocol publication: "Within the first three months of the study, whilst we gain ethics permission and NHS Research and Development approval, we will conduct a series of meetings between experienced yoga practitioners in order to agree on a basic package of yoga that can be delivered by yoga teachers of these two national organisations [British Wheel of Yoga and Iyengar Yoga Association (UK)]." |
| Wattamwar 2013 | Combination of iyengar and traditional yoga | Postures (Asanas) Breathing (Pranayama) Prayer |
— |
| Williams 2005 | Iyengar yoga | Postures (Asanas) | Quote: "The yoga intervention was developed with the consultation of senior iyengar yoga instructors who had experience with iyengar's protocol for treating CLBP [chronic low back pain]. The principal investigator, an iyengar student for 14 years and teacher in training for 9 years, was introduced to the protocol for CLBP by Geeta Iyengar at Ramamani Memorial Institute in Pune, India in 1998. Since then she has utilized this therapeutic protocol and studied under senior iyengar teachers with a minimum of 25 years of experience." |
| Williams 2009 | Iyengar yoga | Postures (Asanas) | Quote: "The yoga therapy was developed in collaboration with 2 senior iyengar teachers and approved by B. K. S. Iyengar." |
aAll information is as explicitly described in study publication(s) or report(s).
6. Yoga intervention – reporting, flexibility, monitoring, and setting a.
| Study (country) | Specific yoga poses listed or pictured | Flexibility of intervention | Monitoring for treatment fidelity | Setting for intervention delivery | Training and experience of teachers |
| Bramberg 2017 (Sweden) | Listed. | — | — | University/medical school was setting of study. Yoga classes held at a medical school. | Quote: "an experienced yoga instructor." |
| Cox 2010 (UK) | — | Quote: "Modifications of poses were available for people who needed them." | — | — | 2 experienced yoga teachers assisted in developing the intervention and were coauthors of the trial report. It appears that the yoga classes were taught by 1 of these teachers. |
|
Demirel 2019 (Turkey) |
Listed. | — | — | Study run out of university, setting for yoga classes and stabilization exercises not described. | — |
| Galantino 2004 (USA) | Listed. | Quote: "Yoga postures were demonstrated and adapted to the capabilities of each individual to prevent injury." | — | — | Quote: "A single instructor, who was certified by the Yoga Alliance directed each one hour hatha yoga session…" |
|
Groessl 2017 (USA) |
Protocol described class structure in general and referred to a standardized manual. | Quote: "Instructors used a prescriptive manual to guide each session, but were allowed to change the order of poses to provide some variety." | — | — | Quote: "Yoga sessions were led by a single certified yoga instructor with over 7 years of experience teaching yoga to people with cLBP [chronic low back pain]." |
|
Highland 2018 (USA) |
Listed. | Intervention was modified according to (quotes) "instructor judgment and participant receptivity." "Instructors formulated and adapted treatment plans…" | Quote: "Master yoga instructors observed RESTORE instructors once monthly, in‐person, or videotaped with participant's permission for fidelity monitoring." | Study run out of Walter Reed National Military Medical Center. Location of yoga classes was not described. | Quote: "RESTORE instructors had completed a 200‐ hour teacher training through an authorized Yoga Alliance program and additional research ethics training, as well as RESTORE training led by 2 master yoga instructors." |
| Jacobs 2004 (USA) | Listed. | The intervention was described as semi‐structured so that individual poses could be selected for different classes depending on the needs of the class. No explicit mention of modifications for participants. | — | — | Quote: "Four iyengar yoga instructors were selected to teach the participants. Each instructor was required to meet University of California, San Francisco credentialing criteria, and, in addition, to have a minimum of 10 years experience teaching yoga, and experience working with patients with chronic back pain." |
| Kuvacic 2018 (Croatia) | — | — | — | Study run from ≥ 1 universities. Location of yoga classes unclear. | — |
| Nambi 2014 (India) | Listed and pictured. | — | — | Outpatient department of a physiotherapy college. | — |
| Neyaz 2019 (India) | Listed. | — | — | Quote: "The study was conducted at Department of Physical Medicine and Rehabilitation and Centre for Integrative Medicine and Research (CIMR) of a tertiary care hospital." Yoga sessions provided at CIM. | "Yoga sessions were administered by a trained yoga therapist." |
| Patil 2018 (India) | Listed. | — | — | Study was carried out at a tertiary care teaching hospital. Location of yoga classes was not described. | — |
| Saper 2009 (USA) | Listed and pictured. | Quote: "The protocol provided variations and used various aids (e.g., chair, strap, block) to accommodate different abilities." | Quote: "The 2 national yoga experts from the panel observed several classes in person to provide feedback to the instructors on accurate, effective, and safe protocol delivery." | A community health center. | Quote: "[Classes] were taught by a team of 2 female yoga instructors, 1 white and 1 African American. Both were registered yoga teachers with Yoga Alliance, and each had approximately 4 years of teaching experience." |
|
Saper 2017 (USA) |
Listed (supplement 2). | Quote: "Pose variations and aids (such as chair, strap, and blocks) accommodated various abilities." | Quote: "Staff observed approximately 10% of classes to assess protocol fidelity by using a checklist." | Large academic safety‐net hospital and 7 affiliated community health centers. Yoga classes were held at the community health centers. | Quote: "Thirteen yoga instructors completed 8 hours of training and taught classes at 6 sites." |
| Sherman 2005 (USA) | Listed and pictured. | Text stated that some postures had available adaptations. | — | Integrated health system facilities (number not stated). | 1 yoga teacher was mentioned in the text and acknowledgments as helping to develop the yoga intervention and teaching the yoga classes. No further details about teacher qualifications or experience. |
| Sherman 2011 (USA) | Listed in protocol paper. | Text stated there were variations and adaptations. | Quote: "One researcher (KJS) attended 1 class for each intervention for each cohort to evaluate adherence to the protocols." | Integrated health system facilities (number not stated). | Teachers: (quote) "Classes were taught by instructors with at least 500 hours of viniyoga training, 5 years of teaching experience, and familiarity with the selected postures and who were briefed by our yoga consultant." |
| Tekur 2008 (India) | Listed. | — | — | Residential holistic health center. | — |
| Teut 2016 (Germany) | — | Quote: "These exercises were adapted to the individual needs of the participants." | — | Study was based at a university and the yoga classes were held either at the university or at retirement homes. | — |
| Tilbrook 2011 (UK) | The poses were not listed or pictured; however, an audio clip and comments on the journal website provided a link to a further website where the manual and accompanying CD may be purchased. | — | Quote: "Treatment fidelity was assessed on 2 separate occasions by the back‐up yoga teachers. At each assessment, a report was completed and sent to the trial coordinators for review. The fidelity of content was verified by this process, and no changes resulted from the monitoring sessions." | Non‐medical centers at 5 sites. | Quote: "Twenty experienced yoga teachers … were recruited for the study. Teachers attended program training sessions over 2 weekends. All teachers taught the same form of yoga according to the teachers' manual class plans and the pose descriptions and sequences contained in the students' manual. For each course, 2 teachers were selected: 1 to teach and 1 to serve as back‐up." |
| Wattamwar 2013 (India) | Listed and pictured. | — | — | Iyenger Yoga center. | — |
| Williams 2005 (USA) | Listed. | — | — | Community yoga studio. | Quote: "The yoga instructors have trained in the iyengar method for over 10 years, teaching yoga for 8 years and have experience teaching persons with CLBP [chronic low back pain]." |
| Williams 2009 (USA) | Listed and pictured. | — | — | Yoga studio. | "Certified iyengar yoga instructor and 2 assistants with experience delivering yoga therapy to persons with CLBP [chronic low back pain]." |
aAll information is as explicitly described in study publication(s) or report(s).
Participants
In 15 studies, the mean age of participants was between 43 and 53 years, in three studies the mean or median age was between 30 and 40 years (Kuvacic 2018; Neyaz 2019; Patil 2018; Wattamwar 2013), in one study the participants had a mean age of 73 (Teut 2016), and one study did not report the age of participants (Galantino 2004).
One Indian study focused exclusively on female nurses (Patil 2018), and two of the remaining Indian studies enrolled approximately 50% women (Neyaz 2019; Tekur 2008). One study carried out in the USA focused on military veterans and the percentage of women included in the study was 26% (Groessl 2017). The percentage of women was just under 50% in one small study carried out in Croatia (Kuvacic 2018). Two studies did not report participants' gender (Jacobs 2004; Wattamwar 2013). All other studies enrolled mostly women (from 64% to 90%).
Nine trials reported race or ethnicity, and the percentage of participants reported to be 'Caucasian' or 'White' ranged from a low of less than 25% (Saper 2009; Saper 2017) to 49% (Groessl 2017) to 63% (Highland 2018; Jacobs 2004), and was over 80% in the remaining studies (Sherman 2005; Sherman 2011; Williams 2005; Williams 2009).
Fourteen studies reported education level, and in half of those studies most participants had completed at least some college level education (Groessl 2017; Jacobs 2004; Kuvacic 2018; Saper 2009; Sherman 2005; Sherman 2011; Tekur 2008; Tilbrook 2011; Williams 2005; Williams 2009).
Two studies did not describe the source or methods of recruitment (Kuvacic 2018; Wattamwar 2013). In the other studies, participants were recruited from clinical populations (Cox 2010; Demirel 2019; Groessl 2017; Neyaz 2019; Sherman 2005; Tekur 2008), from both clinical and community populations (Bramberg 2017; Galantino 2004; Highland 2018; Jacobs 2004; Nambi 2014; Patil 2018; Saper 2009; Saper 2017; Sherman 2011; Tilbrook 2011; Williams 2005), or from the community (Teut 2016; Williams 2009). For studies in which participants were recruited throw ugh a mix of clinical and community outreach, most of those screened appeared to be self‐referred from the community in Bramberg 2017 and Williams 2005, and to be physician‐referred potential participants in Tilbrook 2011. The other studies did not describe the mix of recruitment sources. Most studies were co‐ordinated and implemented from a single clinical or academic site; however, two studies were carried out at multiple community health center sites (Saper 2009; Saper 2017), one study was carried out through 39 general medical practices (Tilbrook 2011), and two studies were carried out at a co‐ordinated healthcare system with multiple clinical sites (Sherman 2005; Sherman 2011); the exact number of sites was not reported.
Interventions
Five studies had three comparison arms (Bramberg 2017; Saper 2017; Sherman 2005; Sherman 2011; Teut 2016), and all other studies had two arms. We did not find any studies comparing yoga to sham yoga for chronic back pain. Studies compared yoga to a waiting list or usual care (Cox 2010; Galantino 2004; Groessl 2017; Highland 2018; Jacobs 2004; Saper 2009; Teut 2016; Tilbrook 2011; Williams 2009), to a self‐care book or pamphlets and newsletters (Bramberg 2017; Kuvacic 2018; Saper 2017; Sherman 2005; Sherman 2011), to educational classes and written material (Williams 2005), to back‐focused exercise (Bramberg 2017; Demirel 2019; Nambi 2014; Neyaz 2019; Patil 2018; Saper 2017; Sherman 2005; Sherman 2011; Tekur 2008), or to another mind–body therapy, qigong (Teut 2016). One study compared yoga plus conventional exercise to conventional exercise alone (Wattamwar 2013).
The types of yoga varied between trials. The most common type of yoga described was iyengar yoga or a modification of iyengar yoga. Study authors reported using hatha yoga (Galantino 2004; Groessl 2017; Saper 2009; Saper 2017), iyengar yoga (Cox 2010; Nambi 2014; Williams 2005; Williams 2009), the 'iyengar style of hatha yoga' (Jacobs 2004), a combination of iyengar and British Wheel of Yoga (described as hatha yoga on the British Wheel of Yoga website) (Tilbrook 2011), a combination of iyengar and 'traditional' yoga (Wattamwar 2013), viniyoga (Sherman 2005; Sherman 2011; Teut 2016), or integrated yoga therapy (Neyaz 2019; Patil 2018; Tekur 2008). One study mentioned using 'therapeutic yoga' (Highland 2018), and two studies did not describe the yoga as a particular type or style (Demirel 2019; Kuvacic 2018). All interventions included meditation, relaxation, or breathing exercises in addition to physical yoga poses.
For 19 studies, each yoga class was 35 to 90 minutes in length, the frequency of classes was one to three yoga classes per week, and the duration of the intervention was most commonly 12 weeks but ranged from four to 24 weeks, while the total duration of follow‐up ranged from six to 52 weeks (Bramberg 2017; Cox 2010; Demirel 2019; Galantino 2004; Groessl 2017; Highland 2018; Jacobs 2004; Kuvacic 2018; Nambi 2014; Neyaz 2019; Saper 2009; Saper 2017; Sherman 2005; Sherman 2011; Teut 2016; Tilbrook 2011; Wattamwar 2013; Williams 2005; Williams 2009). In Patil 2018, one hour of yoga class was held five days per week for six weeks. In Tekur 2008, the study was carried out in a residential setting for one week, and the yoga group practiced approximately two hours of yoga postures per day as well as practicing yogic meditation, breathing, and chanting, and receiving yogic lifestyle lectures.
For further details on the intervention components and implementation see Table 7; Table 8; and Table 9.
Outcomes
Nineteen studies assessed back‐specific function (Bramberg 2017; Cox 2010; Demirel 2019; Galantino 2004; Groessl 2017; Highland 2018; Jacobs 2004; Kuvacic 2018; Neyaz 2019; Saper 2009; Saper 2017; Sherman 2005; Sherman 2011; Tekur 2008; Teut 2016; Tilbrook 2011; Wattamwar 2013; Williams 2005; Williams 2009). Studies assessed back‐specific function using the RMDQ (Cox 2010; Groessl 2017; Highland 2018; Jacobs 2004; Neyaz 2019; Saper 2009; Saper 2017; Sherman 2005; Sherman 2011; Tilbrook 2011), the Oswestry Low Back Pain Disability Questionnaire or Oswestry Disability Index (Demirel 2019; Galantino 2004; Jacobs 2004; Kuvacic 2018; Tekur 2008; Wattamwar 2013; Williams 2009), the Pain Disability Index (Williams 2005), or a subscale of the Swedish version of the Chronic Pain Grade Scale (Bramberg 2017).
Nineteen studies assessed pain or pain‐related outcomes (Bramberg 2017; Cox 2010; Demirel 2019; Groessl 2017; Highland 2018; Jacobs 2004; Kuvacic 2018; Nambi 2014; Neyaz 2019; Saper 2009; Saper 2017; Sherman 2005; Sherman 2011; Tekur 2008; Teut 2016; Tilbrook 2011; Wattamwar 2013; Williams 2005; Williams 2009). Studies assessed pain using a 0 to 5 scale (Wattamwar 2013), a 0 to 10 scale (Demirel 2019; Groessl 2017; Highland 2018; Jacobs 2004; Kuvacic 2018; Nambi 2014; Neyaz 2019; Saper 2009; Saper 2017; Tekur 2008; Williams 2005), a 0 to 100 scale (Williams 2009), or the Aberdeen Back Pain Scale (Cox 2010; Tilbrook 2011). One study assessed pain on a subscale of the Swedish Chronic Pain Grade Scale and transformed it into a 0 to 100 scale (Bramberg 2017). Another study measured pain both on the Functional Rating Index (a 0 to 4 scale of mean pain intensity during the previous seven days), and on a 0 to 100 VAS scale for mean pain intensity during the previous seven days (Teut 2016); we chose to extract the VAS scale for consistency with other included studies. Two studies did not report pain but instead reported the pain‐related outcome of 'symptom bothersomeness' (Sherman 2005; Sherman 2011). This measured "the extent to which participants' lives are affected by whatever level of pain they felt", a concept related to, but not the same as, pain (Sherman 2010).
Five studies reported some measure of clinical improvement (Cox 2010; Neyaz 2019; Saper 2009; Saper 2017; Sherman 2011).
Ten studies reported mental and physical quality of life (Cox 2010; Demirel 2019; Highland 2018; Jacobs 2004; Nambi 2014; Patil 2018; Saper 2017; Tekur 2008; Teut 2016; Tilbrook 2011).
Five studies reported depression (Galantino 2004; Jacobs 2004; Kuvacic 2018; Teut 2016; Williams 2009).
Twelve studies mentioned the presence or absence of adverse events (Groessl 2017; Highland 2018; Nambi 2014; Neyaz 2019; Saper 2009; Saper 2017; Sherman 2005; Sherman 2011; Tekur 2008; Tilbrook 2011; Williams 2005; Williams 2009).
One study reported sickness‐related absenteeism from work, which we considered to be a measure of work‐related disability (Bramberg 2017).
Excluded studies
We excluded 47 studies (57 articles) for the following reasons: wrong study design (seven studies; Groessl 2012; Jacob 2017; Lee 2014; NCT02806323; NCT04296344; NCT04773743; Patil 2015); wrong population (21 studies; Biggs 2012; Bindal 2007; CTRI/2012/11/003094; Hartfiel 2012; Holden 2016; Kim 2014; Kumar 2011; Manik 2017; Michalsen 2012; Monro 2015; Namdar 2021; NCT03840304; NCT04113460; NCT04281238; Pushpika Attanayake 2010; Sakuma 2012; Schmid 2019; Sharma 2019; Telles 2009; Telles 2016; Uebelacker 2019); wrong intervention (four studies; CTRI/2017/02/007783; CTRI/2018/01/011098; NCT03324659; NCT04089618); wrong comparison (six studies; De Giorgio 2018; Groessl 2021; Haldavnekar 2014; NCT03504085; NCT04074109; Saper 2013); and not an original study report (nine studies; Anon 2006; Anon 2009; Anon 2017; Borg‐Olivier 2005; Ford 2017; Graves 2004; Horng 2006; Selfridge 2012; Whitehead 2018). See Characteristics of excluded studies table for more information.
Studies awaiting classification
Eleven studies are awaiting classification (CTRI/2018/01/011243; Hartfiel 2017; IRCT20150531022498N27; Krishna 2020; Krokhmal 2017; Lalkate 2020; Michalson 2021; NCT02552992; NCT03432169; Rae 2020; Saper 2016). See Characteristics of studies awaiting classification table.
Ongoing studies
Eighteen studies are ongoing (CTRI/2018/09/015851; CTRI/2018/10/016132; CTRI/2020/04/024951; CTRI/2020/05/025396; CTRI/2020/12/029944; CTRI/2021/03/031733; CTRI/2021/03/031735; CTRI/2021/03/031736; NCT03816007; NCT04000685; NCT04142177; NCT04203888; NCT04270617; NCT04721639; NCT04723225; NCT04787094; NCT04824547; PACTR202001829834757). See Characteristics of ongoing studies table.
Risk of bias in included studies
A summary of the risk of bias for each study is shown in Figure 2 and the overall risk of bias across studies is shown in Figure 3. Overall, the studies were at low risk of selection bias, high risk of performance and detection bias inherent in studies collecting self‐assessed outcomes from comparisons that cannot be blinded, mixed risks of attrition bias, and unclear risk of reporting bias. Based on low risk of selection and attrition bias, and low or unclear risk of reporting bias, we considered six studies to be at relatively low risk of bias (Patil 2018; Sherman 2005; Sherman 2011; Tekur 2008; Teut 2016; Tilbrook 2011).
2.
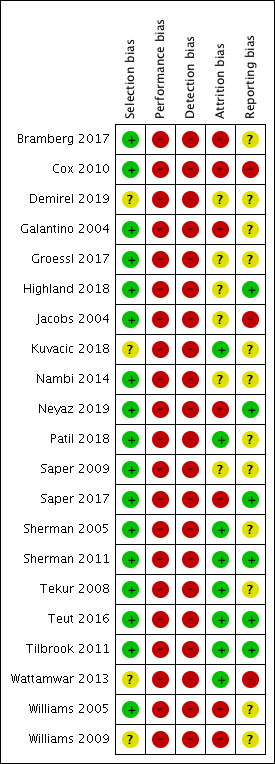
Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
3.
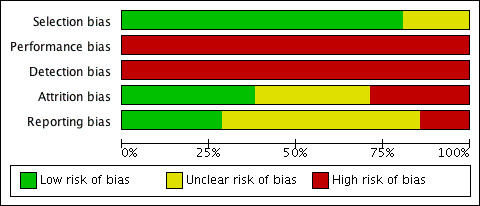
Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.
Allocation
Eleven studies were at low risk of selection bias according to descriptions of the randomization and allocation concealment processes (Bramberg 2017; Cox 2010; Highland 2018; Jacobs 2004; Neyaz 2019; Saper 2009; Sherman 2005; Sherman 2011; Tekur 2008; Teut 2016; Tilbrook 2011). An additional six studies reported methods of randomization but allocation concealment was not clearly reported; however we considered them to be at overall low risk of selection bias (Galantino 2004; Groessl 2017; Nambi 2014; Patil 2018; Saper 2017; Williams 2005). Four studies did not report details of randomization or allocation concealment and we considered them to be at unclear risk of selection bias (Demirel 2019; Kuvacic 2018; Wattamwar 2013; Williams 2009).
Blinding
No studies reported methods to blind participants or providers. This included the studies that compared yoga to an exercise intervention, where there was no suggestion that the exercise intervention was intended to appear similar to yoga, although one study reported the participants did not know the content of the alternative interventions (Bramberg 2017), and one study reported that the participants were blinded (Demirel 2019), although what this entailed was unclear and the same study reported that the outcome assessor was not blinded. Several studies reported that the people collecting outcome information from participants were blinded (Bramberg 2017; Groessl 2017; Nambi 2014; Neyaz 2019; Sherman 2005; Sherman 2011; Tekur 2008; Williams 2005; Williams 2009); however, the measures of pain, function, and quality of life, and the clinical improvement outcomes deriving from those measures, were based on self‐reports by the participants, who were not themselves blinded. Therefore, we considered all studies to be at high risk of performance and detection bias.
Incomplete outcome data
Eight studies were at low risk of attrition bias because they had little or no attrition, and if they had attrition the reasons for dropout did not appear to differ across intervention groups (Kuvacic 2018; Patil 2018; Sherman 2005; Sherman 2011; Tekur 2008; Teut 2016; Tilbrook 2011; Wattamwar 2013). Six studies were at unclear risk of attrition bias because attrition was fairly low, but reasons for attrition were unclear or possibly related to outcomes, or attrition was higher and explanations for attrition were partial or missing data were managed in an unclear or simplistic manner (e.g. last observation carried forward) (Demirel 2019; Groessl 2017; Highland 2018; Jacobs 2004; Nambi 2014; Saper 2009). Seven studies were at high risk of attrition bias because attrition was at least 20% in one or both intervention groups and there were serious concerns about relationships between attrition and the intervention or about how missing data were managed (Bramberg 2017; Cox 2010; Galantino 2004; Neyaz 2019; Saper 2017; Williams 2005; Williams 2009).
Selective reporting
Six studies were at low risk of selective reporting bias because reported outcomes were consistent with protocols (Highland 2018; Neyaz 2019; Saper 2017; Sherman 2011; Teut 2016; Tilbrook 2011). Three studies were at high risk due to discrepancies between methods and results sections (Cox 2010; Jacobs 2004; Wattamwar 2013), and 12 studies were at unclear risk of selective reporting bias. Eight of these studies did not have registered or published protocols, but we did not observe outcome discrepancies between methods and results sections and, therefore, rated the risk of bias as unclear (Demirel 2019; Galantino 2004; Kuvacic 2018; Nambi 2014; Patil 2018; Tekur 2008; Williams 2005; Williams 2009). Four of these studies displayed some omissions or additions when comparing protocols or registrations and study reports, but the discrepancies did not affect major outcomes and were primarily related to omissions rather than new outcomes (Bramberg 2017; Groessl 2017; Saper 2009; Sherman 2005) (e.g. additional publications were likely to report further registered outcomes).
Group similarity at baseline
In 12 studies, comparison groups were similar in important prognostic characteristics, and we rated these studies at low risk of bias (Bramberg 2017; Groessl 2017; Highland 2018; Jacobs 2004; Neyaz 2019; Patil 2018; Saper 2009; Saper 2017; Sherman 2005; Tekur 2008; Teut 2016; Tilbrook 2011). There were important differences in baseline prognostic indicators between groups in three studies, which we rated at high risk of bias (Cox 2010; Demirel 2019; Galantino 2004). There were baseline differences that were of unclear importance in three studies, which we rated at unclear risk of bias (Sherman 2011; Williams 2005; Williams 2009), together with the three studies for which we were unable to assess group similarity at baseline (Kuvacic 2018; Nambi 2014; Wattamwar 2013).
Co‐interventions
We were unable to assess co‐interventions in 11 studies (Bramberg 2017; Cox 2010; Demirel 2019; Galantino 2004; Highland 2018; Jacobs 2004; Kuvacic 2018; Nambi 2014; Patil 2018; Tilbrook 2011; Wattamwar 2013), and in 10 studies the co‐interventions appeared similar between intervention groups (Groessl 2017; Neyaz 2019; Saper 2009; Saper 2017; Sherman 2005; Sherman 2011; Tekur 2008; Teut 2016; Williams 2005; Williams 2009).
Compliance
Eight studies did not report specific information on class attendance, and we rated them at unclear with respect to risk of bias related to compliance (Bramberg 2017; Demirel 2019; Galantino 2004; Kuvacic 2018; Nambi 2014; Patil 2018; Tekur 2008; Wattamwar 2013). Of the remaining studies, we rated one at high risk of bias because only 50% of participants attended any classes, and they attended less than 50% of available classes on average (Cox 2010); one at high risk of bias because we could not identify the exact percentage of participants attending classes, but the study author stated that less than 50% of participants met predefined adherence criteria (Saper 2017); and we rated 11 at low risk of bias because they reported that between 60% and 100% of participants attended at least 50% of classes on average (Groessl 2017; Highland 2018; Jacobs 2004; Neyaz 2019; Saper 2009; Sherman 2005; Sherman 2011; Teut 2016; Tilbrook 2011; Williams 2005; Williams 2009).
Intention‐to‐treat analysis
We rated eight studies that did not mention an intention‐to‐treat analysis at unclear risk of bias (Demirel 2019; Jacobs 2004; Kuvacic 2018; Nambi 2014; Patil 2018; Tekur 2008; Wattamwar 2013; Williams 2005), and the 13 studies that stated an intention‐to‐treat analysis was carried out at low risk of bias (Bramberg 2017; Cox 2010; Galantino 2004; Groessl 2017; Highland 2018; Neyaz 2019; Saper 2009; Saper 2017; Sherman 2005; Sherman 2011; Teut 2016; Tilbrook 2011; Williams 2009). No study clearly failed to analyze participants in the groups to which they were randomized.
Timing of outcome assessments
Timing of outcome assessment was similar for all intervention groups within all studies, and we rated all studies at low risk of bias.
Other potential sources of bias
We did not identify other sources of bias in the included studies. However, an additional potential source of bias in unblinded trials that may be related to performance and detection bias is treatment preference (McPherson 1997). If people who prefer to receive yoga consent to be randomized, some of them will receive the non‐preferred treatment, and this may affect their willingness to continue in the study and comply with treatment. Treatment preference may also be related to expectations of treatment and may affect the participants' subjective interpretation of whether they are benefiting from the treatment. Therefore, it is possible that either through better compliance or through placebo or other psychological processes, participants in an unblinded trial who are allocated to a preferred treatment for which they have good expectations of benefit may experience better outcomes, particularly if those outcomes are self‐assessed.
A first step in assessing the impact of expectations and treatment preference on treatment outcomes is to collect this information at baseline. Among the studies included in this review, three studies asked about treatment preference (Sherman 2005; Sherman 2011; Tilbrook 2011), and six studies assessed treatment expectations (Jacobs 2004; Sherman 2005; Sherman 2011; Teut 2016; Tilbrook 2011; Williams 2009). However, only one study examined whether there was a relationship between expectations or treatment preference and outcomes (Tilbrook 2011). The authors reported that "the effect of treatment [on back‐related function] did not vary by baseline intervention preference (P for interaction = 0.39)."
Individual studies have limited power to detect interactions between participant preferences and treatment. To address this limitation, researchers carried out an individual participant data meta‐analysis of participant preferences among people in musculoskeletal trials (Preference Collaborative Review Group 2008). The meta‐analysis did not show that participants allocated to non‐preferred treatment were more likely to drop out. However, assessment of outcomes among 1398 participants in the trials did show that participants allocated to a preferred treatment had significantly better outcomes than participants who were indifferent to their treatment assignment, and non‐significantly better outcomes than participants who were allocated to a non‐preferred treatment (Preference Collaborative Review Group 2008). It appears that preferences and expectations may play a role in participant‐reported outcomes, but further research on operationalizing preferences and expectations is necessary before the potential influence of these factors in outcomes can be understood (Tran 2015).
Overall assessment of risk of bias
Based on low risk of bias for the areas of allocation and attrition bias, and low or unclear risk of attrition bias (Figure 2), we classified five studies at a lower risk of bias (Sherman 2005; Sherman 2011; Tekur 2008; Teut 2016; Tilbrook 2011). We compared these studies to others when carrying out sensitivity analyses by risk of bias.
Effects of interventions
See: Table 1; Table 2; Table 3
We compared yoga versus sham yoga, yoga versus a waiting list, a minimal intervention such as education, or usual care (grouped together as non‐exercise controls), yoga versus another active intervention (yoga compared to exercise) and yoga plus an intervention versus that intervention alone (yoga plus exercise compared to exercise alone). Within the active interventions, we separated the comparison of yoga and qigong from the comparison of yoga and other exercise interventions because we considered qigong to be a mind–body exercise qualitatively different from the physical exercise comparators in other trials. See Table 1; Table 2; Table 3.
1. Yoga versus sham yoga
We found no studies comparing yoga to a sham yoga intervention.
2. Yoga versus non‐exercise (a waiting list, a minimal intervention, or usual care)
Five studies compared a yoga intervention to a waiting list (Galantino 2004; Groessl 2017; Jacobs 2004; Teut 2016; Williams 2009); one study compared yoga to a usual care condition (Highland 2018); three studies compared a yoga intervention to a self‐care book (Bramberg 2017; Sherman 2005; Sherman 2011); two studies compared yoga to a self‐help book or pamphlet and several newsletters (Kuvacic 2018; Saper 2017); three studies compared a yoga intervention plus a self‐care book to a self‐care book alone (Cox 2010; Saper 2009; Tilbrook 2011); and one study compared yoga plus newsletters, handouts, and lectures to newsletters, handouts, and lectures alone (Williams 2005). We analyzed these studies together (15 studies and 1563 participants) because we believe that the yoga and these non‐exercise control conditions are clinically comparable across studies.
See Table 2.
Major outcomes
Back‐specific functional status
Fifteen trials examined the effect of yoga compared with non‐exercise controls on back‐related function (Bramberg 2017; Cox 2010; Galantino 2004; Groessl 2017; Highland 2018; Jacobs 2004; Kuvacic 2018; Saper 2009; Saper 2017; Sherman 2005; Sherman 2011; Teut 2016; Tilbrook 2011; Williams 2005; Williams 2009) (Analysis 1.1). The studies used different scales and we combined data using SMDs then translated the estimates into the RMDQ. Negative differences correspond to better back‐specific function with yoga, a difference of 5 points on the RMDQ is considered‐clinically significant.
1.1. Analysis.

Comparison 1: Yoga versus non‐exercise, Outcome 1: Back‐specific functional status
At four to eight weeks there was moderate‐certainty evidence (downgraded for risk of bias) that yoga probably provides a small and clinically unimportant improvement in back‐specific function compared to non‐exercise (SMD −0.41, 95% CI −0.61 to −0.21; MD −1.64, 95% CI −2.43 to −0.84; I² = 6%; 8 studies, 474 participants) (MD calculated using control group SD of 3.99 from Sherman 2011). At three months, there was low‐certainty evidence (downgraded for risk of bias and inconsistency) that yoga may provide a small and clinically unimportant improvement in back‐specific function compared to non‐exercise (SMD −0.31, 95% CI −0.50 to −0.12; MD −1.69, 95% CI −2.73 to −0.65; I² = 55%; 11 studies, 1155 participants) (MD calculated using control group SD of 5.45 from Tilbrook 2011). At six months, there was low‐certainty evidence (downgraded for risk of bias and publication bias) that yoga may provide a small and clinically unimportant improvement in back‐specific function compared to non‐exercise (SMD −0.36, 95% CI −0.52 to −0.21; MD −1.76, 95% CI −2.54 to −1.03; I² = 38%; 11 studies, 1157 participants) (MD calculated using control group SD of 4.89 from Tilbrook 2011). At 12 months there was moderate‐certainty evidence (downgraded for risk of bias) that yoga probably provides a small and clinically unimportant improvement in back‐specific function compared to non‐exercise (SMD −0.27, 95% CI −0.45 to −0.10; MD −1.41, 95% CI −2.35 to −0.52; I² = 0%; 3 studies, 532 participants) (MD calculated using control group SD of 5.23 from Tilbrook 2011). Funnel plots for back‐specific function showed publication bias at six months but not three months (Figure 4; Figure 5), and, therefore, we downgraded the evidence at six months for possible publication bias.
4.
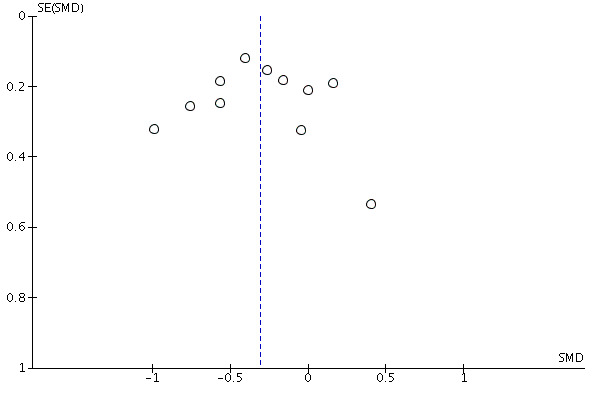
Funnel plot of comparison: 1 Yoga versus non‐exercise, outcome: 1.1.2 Back‐specific function at three to four months.
5.
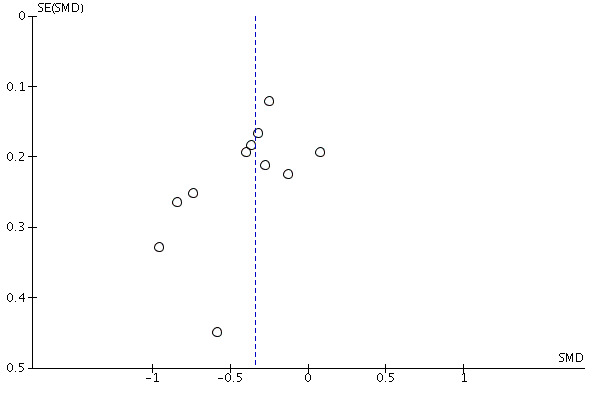
Funnel plot of comparison: 1 Yoga versus non‐exercise, outcome: 1.1.3 Back‐specific function at six months.
Pain
Twelve trials examined the effect of yoga compared with non‐exercise controls on pain (Bramberg 2017; Cox 2010; Groessl 2017; Highland 2018; Jacobs 2004; Kuvacic 2018; Saper 2009; Saper 2017; Teut 2016; Tilbrook 2011; Williams 2005; Williams 2009) (Analysis 1.2). All pain outcomes were standardized to a 0 to 100 scale for analysis and negative differences correspond to less pain with yoga, we considered a difference of 15 points on a 0‐ to 100‐point scale to be clinically significant.
1.2. Analysis.

Comparison 1: Yoga versus non‐exercise, Outcome 2: Pain
At four to eight weeks, there was low‐certainty evidence (downgraded for risk of bias and imprecision) that yoga may provide a small and clinically unimportant improvement in pain compared to non‐exercise (MD −11.05, 95% CI −14.22 to −7.88; I² = 0%; 5 studies, 258 participants). At three months, there was moderate‐certainty evidence (downgraded for risk of bias) that yoga probably provides a small and clinically unimportant improvement in pain compared to non‐exercise (MD −4.53, 95% CI −6.61 to −2.46; I² = 0%; 9 studies, 946 participants). At six months, there was moderate‐certainty evidence (downgraded for risk of bias) that yoga probably provides a small and clinically unimportant improvement in pain compared to non‐exercise (MD −5.40, 95% CI −8.58 to −2.22; I² = 40%; 9 studies, 940 participants). At 12 months, there was low‐certainty evidence (downgraded for risk of bias and inconsistency) that yoga may provide little or no improvement in pain compared to non‐exercise (MD −5.87, 95% CI −12.25 to 0.50; I² = 68%; 3 studies, 521 participants).
Clinical improvement
Four trials examined the effect of yoga compared with non‐exercise controls on clinical improvement (Cox 2010; Saper 2009; Saper 2017; Sherman 2011) (Analysis 1.3). One trial gave the percentage of participants reporting global improvement in back pain (Saper 2009), one trial reported the number of participants who no longer had back pain (Cox 2010), one trial reported the number of participants who rated their back pain as better, much better, or completely gone (Sherman 2011), and one trial reported the number of participants rating their global change in back pain as 5 or 6 on a 0 to 6 Likert scale in which 0 was extremely worsened and 6 was extremely improved (Saper 2017).
1.3. Analysis.

Comparison 1: Yoga versus non‐exercise, Outcome 3: Clinical improvement
Low‐certainty evidence (downgraded for risk of bias and imprecision) showed that yoga may increase clinical improvement compared to non‐exercise at four to six weeks (RR 2.62, 95% CI 1.22 to 5.67; I² = 0%; 2 studies, 141 participants), three months (RR 2.33, 95% CI 1.46 to 3.71; I² = 23%; 4 studies, 353 participants), and six months (RR 2.53, 95% CI 1.36 to 4.71; 1 study, 128 participants). There was no information on clinical improvement at 12 months.
Quality of life
Six trials examined the effect of yoga compared with non‐exercise controls on physical quality of life (Cox 2010; Highland 2018; Jacobs 2004; Saper 2017; Teut 2016; Tilbrook 2011) (Analysis 1.4). Higher values indicate better quality of life. At four weeks, there was low‐certainty evidence (downgraded for risk of bias and imprecision) that yoga may provide a medium improvement in physical quality of life compared to non‐exercise (SMD 0.50, 95% CI 0.05 to 0.95; MD 3.08, 95% CI 0.31 to 5.85 on the PROMIS‐29 physical functioning subscale; I² = 0%; 2 studies, 81 participants) (MD calculated using control group SD of 6.16 from Highland 2018). At three months, there was moderate‐certainty evidence (downgraded for risk of bias) that yoga probably provides a small improvement in physical quality of life compared to non‐exercise (SMD 0.20, 95% CI 0.03 to 0.37; MD 1.80, 95% CI 0.27 to 3.33 on the SF‐36 physical health scale; I² = 10%; 6 studies, 686 participants) (MD calculated using control group SD of 9 from Saper 2017). Low‐certainty evidence (downgraded for risk of bias and inconsistency) showed that yoga may provide little or no improvement in physical quality of life compared to non‐exercise at six months (SMD 0.16, 95% CI −0.13 to 0.46; MD 1.58, 95% CI −1.29 to 4.55 on the 12‐item Short Form (SF‐12) physical health scale; I² = 52%; 3 studies, 434 participants) (MD calculated using control group SD of 9.89 from Tilbrook 2011) and at 12 months (SMD 0.17, 95% CI −0.07 to 0.41; MD 1.67, 95% CI −0.70 to 4.04 on the SF‐12 physical health scale; 1 study, 264 participants).
1.4. Analysis.

Comparison 1: Yoga versus non‐exercise, Outcome 4: Physical quality of life
Six trials examined the effect of yoga compared with non‐exercise controls on mental quality of life (Cox 2010; Highland 2018; Jacobs 2004; Saper 2017; Teut 2016; Tilbrook 2011) (Analysis 1.5). At four weeks, there was very low‐certainty evidence (downgraded for risk of bias, inconsistency, and imprecision) that yoga has no effect on mental quality of life compared to non‐exercise (SMD −0.15, 95% CI −1.24 to 0.93; MD −0.75, 95% CI −6.19 to 4.64; I² = 67%; 2 studies, 81 participants) (MD calculated using control group SD of 4.99 from Highland 2018). Moderate‐certainty evidence (downgraded for risk of bias) showed that yoga probably provides a very small improvement in mental quality of life compared to non‐exercise at three months (SMD 0.20, 95% CI 0.05 to 0.35; MD 2.38, 95% CI 0.60 to 4.17 on the SF‐36 mental scale; I² = 0%; 6 studies, 686 participants) (MD calculated using control group SD of 11.9 from Saper 2017) and at six months (SMD 0.21, 95% CI 0.0 to 0.41; MD 2.24, 95% CI 0 to 4.37 on the SF‐12 mental health scale; I² = 9%; 3 studies, 434 participants) (MD calculated using control group SD of 10.66 from Tilbrook 2011). At 12 months, there was low‐certainty evidence (downgraded for risk of bias and imprecision) that yoga may provide very small or no improvement in mental quality of life compared to non‐exercise (SMD 0.07, 95% CI −0.17 to 0.31; MD 0.73, 95% CI −1.81 to 3.27 on the SF‐12 mental health scale; 1 study, 264 participants).
1.5. Analysis.

Comparison 1: Yoga versus non‐exercise, Outcome 5: Mental quality of life
Depression
Five trials examined the effect of yoga on depression (Galantino 2004; Jacobs 2004; Kuvacic 2018; Teut 2016; Williams 2009) (Analysis 1.6). The studies used different scales and we combined data using SMDs then translated the estimates into the Beck Depression Inventory (BDI). Lower values indicate lower depression.
1.6. Analysis.

Comparison 1: Yoga versus non‐exercise, Outcome 6: Depression
Very low‐certainty evidence (downgraded for very serious risk of bias, inconsistency, and imprecision) showed that we are uncertain about the effects of yoga on depression compared to non‐exercise (SMD −1.44, 95% CI −2.11 to −0.76; MD −14.10, 95% CI −20.66 to −7.44; I² = 0%; 2 studies, 46 participants) (MD calculated using control group SD of 9.79 from Galantino 2004) at six to eight weeks. Low‐certainty evidence (downgraded for risk of bias and imprecision) showed that there may be little to no difference in depression with yoga compared to non‐exercise at three months (SMD −0.19, 95% CI −0.44 to 0.07; MD −1.25, 95% CI −2.90 to 0.46; I² = 0%; 3 studies, 241 participants) (MD calculated using control group SD of 6.58 from Williams 2009), a small improvement in depression at six months (SMD −0.34, 95% CI −0.63 to −0.06; MD −2.19, 95% CI −4.06 to −0.39; I² = 0%; 2 studies, 197 participants) (MD calculated using control group SD of 6.44 from Williams 2009), and a medium improvement in depression at 12 months (SMD −0.50, 95% CI −0.92 to −0.08; MD −2.60, 95% CI −4.71 to −0.49; 1 study, 90 participants).
Adverse events
Five studies did not report collecting adverse event information or give any indication of whether adverse events had occurred (Bramberg 2017; Cox 2010; Galantino 2004; Jacobs 2004; Kuvacic 2018). Highland 2018 reported no adverse events and Teut 2016 reported collecting adverse event information, but did not report whether any adverse events had occurred. Williams 2009 reported "no adverse events due to yoga" but also reported that one yoga participant discontinued the intervention because yoga exacerbated low back pain and we considered this to be evidence of an adverse event in the yoga group. In addition to Williams 2009, the remaining seven studies provided data on adverse events, primarily increased back pain (Groessl 2017; Saper 2009; Saper 2017; Sherman 2005; Sherman 2011; Tilbrook 2011; Williams 2005).
At follow‐up of up to 12 months there was low‐certainty evidence (downgraded for risk of bias and imprecision) that yoga may increase the risk of adverse events compared to non‐exercise (RR 4.76, 95% CI 2.08 to 10.89; I² = 0%; 8 trials, 1037 participants; NNTH 31, 95% CI 13 to 105; Analysis 1.7). The severity of adverse events and the relationship between yoga and adverse events was inconsistently assessed and reported. Two studies described severe adverse events or discontinuation due to adverse events. Tilbrook 2011 reported that a yoga participant who had a history of severe pain in response to physical activity developed severe back pain that was possibly related to yoga and, as mentioned above, Williams 2009 reported that one yoga participant discontinued the intervention because yoga exacerbated low back pain.
1.7. Analysis.

Comparison 1: Yoga versus non‐exercise, Outcome 7: Adverse events
Subgroup analysis
Two trials specifically targeted recruitment to US participants belonging to lower income communities, and stated their trials enrolled a more racially diverse, lower SES population than other trials of yoga for chronic non‐specific low back pain (Saper 2009; Saper 2017). Both studies measured back‐related function and pain at six months. A formal test of the difference between these and other trials revealed no heterogeneity (I² = 0%) for back‐related function (Analysis 2.1) or pain (Analysis 2.2) at six months.
2.1. Analysis.

Comparison 2: Subgroup analyses for yoga versus non‐exercise, Outcome 1: Subgroup analysis by socioeconomic status (SES) for back‐specific functional status at 6 months
2.2. Analysis.

Comparison 2: Subgroup analyses for yoga versus non‐exercise, Outcome 2: Subgroup analysis by SES for pain at 6 months
One of the included studies in the primary analysis did not have the stated goal of recruiting lower SES or disadvantaged participants, but was carried out in US veterans (Groessl 2017). The study authors stated that veterans tend to have fewer economic resources, lower education, and greater comorbidity than the general US population. Therefore, we carried out a sensitivity analysis in which we grouped Groessl 2017 with Saper 2009 and Saper 2017, and we again observed no heterogeneity (I² = 0%) between subgroups for back‐specific function or pain (data not shown).
Sensitivity analysis
Sensitivity analyses restricting studies to those at lower risk of bias (Analysis 3.1; Analysis 3.4) or using complete‐case data (Analysis 3.2; Analysis 3.5) did not reveal marked differences from analyses including all studies. Sensitivity analyses for back function and pain using change scores instead of endpoint values did not reveal marked differences from our primary analyses (Analysis 3.3; Analysis 3.6), with one exception. For back function at four to eight weeks (Analysis 1.1.1), the analysis using change scores (Analysis 3.2.1) resulted in a markedly smaller effect estimate and the CI included no effect. The change values analysis contained only two of the eight studies in the primary analysis, and the larger study of the two reported adjusted change values but unadjusted endpoints in the primary analysis, rendering the two analyses difficult to compare. Sensitivity analyses using the SMD for pain were consistent with the size of effects on a 0 to 100 scale (Analysis 3.7).
3.1. Analysis.

Comparison 3: Sensitivity analyses for yoga versus non‐exercise, Outcome 1: Back‐specific functional status sensitivity analyses (higher‐quality studies)
3.4. Analysis.

Comparison 3: Sensitivity analyses for yoga versus non‐exercise, Outcome 4: Pain sensitivity analyses (higher‐quality studies)
3.2. Analysis.

Comparison 3: Sensitivity analyses for yoga versus non‐exercise, Outcome 2: Back‐specific functional status sensitivity analyses (complete case)
3.5. Analysis.

Comparison 3: Sensitivity analyses for yoga versus non‐exercise, Outcome 5: Pain sensitivity analyses (complete case)
3.3. Analysis.

Comparison 3: Sensitivity analyses for yoga versus non‐exercise, Outcome 3: Back‐specific functional status sensitivity analyses (change values)
3.6. Analysis.

Comparison 3: Sensitivity analyses for yoga versus non‐exercise, Outcome 6: Pain sensitivity analyses (change values)
3.7. Analysis.

Comparison 3: Sensitivity analyses for yoga versus non‐exercise, Outcome 7: Pain sensitivity analyses (standardized mean difference)
Minor outcome
Measures of work disability
One study (83 participants) reported days of sickness‐related absenteeism (Bramberg 2017). At six weeks, six months, and 12 months, there was low‐certainty evidence (downgraded for risk of bias and imprecision) of little to no difference in days of sickness absenteeism with yoga compared to non‐exercise (6 weeks: MD −4.80 days, 95% CI −11.68 to 2.08; 6 months: MD −8.00 days, 95% CI −16.53 to 0.53; 12 months: MD −5.60 days, 95% CI −13.26 to 2.06; Analysis 1.8). There was no assessment of sickness‐related absenteeism at three months.
1.8. Analysis.

Comparison 1: Yoga versus non‐exercise, Outcome 8: Measures of work disability (days)
3. Yoga versus exercise
Nine studies with 992 participants compared yoga to back‐focused exercise (e.g. physical therapy) (Bramberg 2017; Demirel 2019; Nambi 2014; Neyaz 2019; Patil 2018; Saper 2017; Sherman 2005; Sherman 2011; Tekur 2008). The yoga in most studies consisted of one to three weekly classes provided for four to 12 weeks. Two studies carried out in India provided more intensive yoga. In Patil 2018, the interventions were provided for one hour per day for six weeks, and in Tekur 2008, the interventions were provided daily as part of a one‐week residential comprehensive back pain treatment program. We analyzed Tekur 2008 (80 participants) separately from the other trials because of the brief duration, residential setting, and high intensity of both study intervention arms; therefore, we included eight studies with 912 participants in this comparison.
See Table 3.
Major outcomes
Back‐specific functional status
Six studies examined the effect of yoga compared with exercise on back‐related function (Bramberg 2017; Demirel 2019; Neyaz 2019; Saper 2017; Sherman 2005; Sherman 2011) (Analysis 5.1). The studies used several different scales and we combined data using SMDs then translated the estimates using the RMDQ. Lower scores correspond to better back‐specific function, and a 5‐point difference on the RMDQ is considered clinically significant. At six weeks, there was moderate‐certainty evidence (downgraded for risk of bias) that yoga probably provides little or no improvement in back‐specific function compared to exercise (SMD −0.04, 95% CI −0.32 to 0.23; MD −0.12, 95% CI −0.92 to 0.66; I² = 42%; 4 studies, 395 participants) (MD calculated using SD of 2.88 from Sherman 2011 control group). At three months, there was moderate‐certainty evidence (downgraded for risk of bias) that yoga probably provides little or no improvement in back‐specific function compared to exercise (SMD −0.08, 95% CI −0.28 to 0.13; MD −0.38, 95% CI −1.33 to 0.62; I² = 31%; 4 studies, 575 participants) (MD calculated using SD of 3.84 from Sherman 2011 control group). At six months, there was low‐certainty evidence (downgraded for risk of bias and imprecision) that yoga may provide little or no improvement in back‐specific function compared to exercise (SMD −0.08, 95% CI −0.40 to 0.23; MD 95% −0.31, 95% CI −1.54 to 0.88; I² = 47%; 3 studies, 333 participants) (MD calculated using SD of 3.84 from Sherman 2011 control group). At 12 months, very low‐certainty evidence (downgraded for very serious risk of bias and imprecision) provides uncertainty about the effect of yoga on back‐specific function compared to exercise (SMD −0.02, 95% CI −0.29 to 0.26; MD −0.10, −1.89 to 1.69; 1 study, 200 participants) (outcome reported using RMDQ by Saper 2017).
5.1. Analysis.

Comparison 5: Yoga versus exercise, Outcome 1: Back‐specific functional status
Pain
Five studies examined the effect of yoga compared with exercise on pain (Bramberg 2017; Demirel 2019; Nambi 2014; Neyaz 2019; Saper 2017) (Analysis 5.2). All pain outcomes were standardized to a 0 to 100 scale for analysis and lower scores correspond to less pain. Very low‐certainty evidence (downgraded twice for very serious risk of bias and imprecision) showed that compared to exercise we are uncertain about the effects of yoga on pain at four to six weeks (MD −12.47, 95% CI −18.28 to −6.66; I² = 36%; 3 studies, 201 participants), at three months (MD 2.68, 95% CI −2.01 to 7.36; I² = 0%; 2 studies, 326 participants), at six months (MD −6.41, 95% CI −21.66 to 8.83; I² = 93%; 3 studies, 331 participants), and at 12 months (MD 3.00, 95% CI −4.25 to 10.25; 1 study, 199 participants). We note that when Nambi 2014 was omitted from the analysis at six months, the proportion of variation due to heterogeneity was substantially reduced (I² = 49%) and the estimate of effect was also greatly reduced (MD 0.37, 95% CI −7.62 to 8.36). This suggests that the setting, interventions, or methods of Nambi 2014 may have been responsible for a finding of greater improvement in pain with yoga.
5.2. Analysis.

Comparison 5: Yoga versus exercise, Outcome 2: Pain
Clinical improvement
Three studies examined the effect of yoga versus exercise on clinical improvement (Neyaz 2019; Saper 2017; Sherman 2011) (Analysis 5.3). One trial reported the number of participants who rated their back pain as better, much better, or completely gone (Sherman 2011); one trial reported the number of participants rating their global change in back pain as 5 or 6 on a 0 to 6 Likert scale in which 0 was extremely worsened and 6 was extremely improved (Saper 2017); and one trial reported the number of participants rating their back pain as much improved or very much improved (Neyaz 2019). We are uncertain about the effect of yoga on clinical improvement compared to exercise at six weeks (RR 1.01, 95% CI 0.74 to 1.37; I² = 0%; 2 studies, 207 participants), at three months (RR 0.97, 95% CI 0.72 to 1.31; I² = 63%; 3 studies, 433 participants), and at six months (RR 0.99, 95% CI 0.73 to 1.33; 1 study, 163 participants). Evidence was downgraded for risk of bias and very serious imprecision at six weeks and six months, and for very serious risk of bias, imprecision, and inconsistency at three months.
5.3. Analysis.

Comparison 5: Yoga versus exercise, Outcome 3: Clinical improvement
Quality of life
Four studies reported physical and mental quality of life (Demirel 2019; Nambi 2014; Patil 2018; Saper 2017) (Analysis 5.4; Analysis 5.5). The studies reporting data at four to six weeks used several different scales and we combined data using SMDs then translated the estimates into an MD from a known scale. Higher SMDs correspond to better quality of life with yoga.
5.4. Analysis.

Comparison 5: Yoga versus exercise, Outcome 4: Physical quality of life
5.5. Analysis.

Comparison 5: Yoga versus exercise, Outcome 5: Mental quality of life
We are uncertain about the effect of yoga on physical quality of life compared to exercise at four to six weeks (SMD 1.03, 95% CI 0.36 to 1.71; MD 8.83, 95% CI 3.09 to 14.65 on the World Health Organization Quality of Life Brief Questionnaire Physical Health; I² = 82%; 3 studies, 219 participants) (MD calculated using control group SD of 8.57 from Patil 2018), at three months (SMD 0.15, 95% CI −0.11 to 0.40; MD 1.30, 95% CI −0.95 to 3.55 on the SF‐36 physical health scale; 1 study, 237 participants), and at seven months (SMD 1.34, 95% CI 0.75 to 1.94; MD 4.30, 95% CI 2.62 to 5.98 fewer days of poor physical health; 1 study, 54 participants). Evidence was downgraded for risk of bias, inconsistency, and imprecision at four to six weeks, and for very serious risk of bias and imprecision at three and seven months.
We are uncertain about the effect of yoga on mental quality of life compared to exercise at four to six weeks (SMD 1.03, 95% CI −0.44 to 2.51; MD 7.58, 95% CI ‐3.24 to 18.47 on the World Health Organization Quality of Life Brief Questionnaire Mental Health; I² = 96%; 3 studies, 219 participants) (MD calculated using control group SD of 7.36 from Patil 2018), at three months (SMD 0.16, 95% CI −0.10 to 0.41; MD 1.90, 95% CI −1.17 to 4.97 on the SF‐36 physical health scale; 1 study, 237 participants), and at seven months (SMD 1.33, 95% CI 0.74 to 1.92; MD 2.90, 95% CI 1.75 to 4.05 fewer days of poor mental health; 1 study, 54 participants). Evidence was downgraded for risk of bias, inconsistency, and imprecision at four to six weeks, and for very serious risk of bias and imprecision at three and seven months.
Depression
No studies reported depression.
Adverse events
Three studies did not mention any assessment of adverse effects (Bramberg 2017; Demirel 2019; Patil 2018) (Analysis 5.6). Five studies reported data on adverse events, primarily increased back pain (Nambi 2014; Neyaz 2019; Saper 2017; Sherman 2005; Sherman 2011). At 12 months, there was low‐certainty evidence (downgraded for risk of bias and imprecision) of little to no difference in risk of adverse events between people practicing yoga and people practicing other exercise interventions (RR 0.93, 95% CI 0.56 to 1.53; I² = 0%; 5 studies, 640 participants). Severity of adverse events was not consistently assessed or reported. Two studies reported adverse events resulting in treatment discontinuation. Nambi 2014 reported that one person withdrew from the yoga group due to a herniated disk, and two people withdrew from the yoga group due to fears that yoga would aggravate symptomatic osteoarthritis. Sherman 2005 reported that one yoga participant discontinued yoga because some postures precipitated migraine headache.
5.6. Analysis.

Comparison 5: Yoga versus exercise, Outcome 6: Adverse events
Subgroup analysis
Planned subgroup analyses not possible due to insufficient data.
Sensitivity analysis
Sensitivity analyses restricting studies to those at lower risk of bias (Analysis 4.1) and those with complete data (Analysis 4.2; Analysis 4.4) did not reveal marked differences from the primary analyses. Sensitivity analyses using change values instead of endpoint values (Analysis 4.3; Analysis 4.5) produced estimates for pain at four weeks and three months that were smaller than estimates from the primary analysis, and were more favorable for exercise. However, all sensitivity analyses relied upon single studies that had problems with loss to follow‐up and other risks to bias, and it is therefore unclear how to interpret this difference.
4.1. Analysis.

Comparison 4: Sensitivity analyses for yoga versus exercise, Outcome 1: Back‐specific functional status sensitivity analyses (higher‐quality studies)
4.2. Analysis.

Comparison 4: Sensitivity analyses for yoga versus exercise, Outcome 2: Back‐specific functional status sensitivity analyses (complete case)
4.4. Analysis.

Comparison 4: Sensitivity analyses for yoga versus exercise, Outcome 4: Pain sensitivity analyses (complete case)
4.3. Analysis.

Comparison 4: Sensitivity analyses for yoga versus exercise, Outcome 3: Back‐specific functional status sensitivity analyses (change values)
4.5. Analysis.

Comparison 4: Sensitivity analyses for yoga versus exercise, Outcome 5: Pain sensitivity analyses (change values)
Major outcome
Measures of work disability
One study (82 participants) reported days of sickness‐related absenteeism (Bramberg 2017) (Analysis 5.7). Low‐certainty evidence (downgraded for risk of bias and imprecision) showed little to no difference in days of sickness absenteeism with yoga compared to exercise at six weeks, six months and 12 months (6 weeks: MD −0.90 days, 95% CI −4.64 to 2.84; 6 months: MD −2.40 days, 95% CI −6.00 to 1.20; 12 months: MD −5.90 days, 95% CI −13.38 to 1.58).
5.7. Analysis.

Comparison 5: Yoga versus exercise, Outcome 7: Measures of work disability
4. Yoga versus exercise – brief and intensive residential intervention
One study compared yoga with a brief and intensive residential exercise intervention (Tekur 2008).
Major outcomes
Back‐specific functional status
One study with 80 participants reported that there may be a large improvement in back‐related function with intensive yoga compared to intensive exercise at one week (MD −17.05, 95% CI −22.96 to −11.14; low‐certainty evidence [downgraded for risk of bias and imprecision]; Analysis 5.1.5).
Pain
One study with 80 participants reported that there may be an improvement in pain with intensive yoga compared to intensive exercise at one week (MD −14.50, 95% −22.92 to −6.08; low‐certainty evidence [downgraded for risk of bias and imprecision]; Analysis 5.2.5).
Clinical improvement
The study did not report clinical improvement.
Quality of life
One study with 80 participants reported that there may be a large improvement in quality of life with yoga compared to exercise at one week (Physical Component Summary score: MD 2.03, 95% CI 1.20 to 2.86; Mental Component Summary score: MD 1.88, 95% CI 0.94 to 2.82; low‐certainty evidence [downgraded for risk of bias and imprecision]; Analysis 5.4.4; Analysis 5.5.4).
Depression
The study did not report depression.
Adverse events
Tekur 2008 reported that there were no adverse events in either intervention group.
Minor outcome
Measures of work disability
The study did not report work‐related disability.
5. Yoga versus qigong
One study compared three months of viniyoga classes (a total of 24 × 45‐minute classes) to three months of qigong classes (a total of 12 × 90‐minute classes), and followed participants to six months (Teut 2016). Qigong is a traditional Chinese medicine practice that consists of gentle physical movement, breath exercises, and mindfulness).
Major outcomes
Back‐specific functional status
We are uncertain about the effect of yoga on back‐specific function on the Hannover Functional Ability Questionnaire at three and six months compared to qigong (3 months: MD −3.05, 95% CI −7.84 to 1.74; 6 months: MD −2.68, 95% CI −7.58 to 2.22; Analysis 6.1).
6.1. Analysis.

Comparison 6: Yoga versus qigong, Outcome 1: Back‐specific functional status
Pain
We are uncertain on the effects of yoga on pain at three and six months compared to qigong (3 months: MD 1.48, 95% CI −5.91 to 8.87; 6 months: MD 7.91, 95% CI 0.00 to 15.82; very low‐certainty evidence [downgraded for risk of bias and very serious imprecision]; Analysis 6.2).
6.2. Analysis.

Comparison 6: Yoga versus qigong, Outcome 2: Pain
Clinical improvement
The study did not report clinical improvement.
Quality of life
We are uncertain of the effects of yoga on quality of life measured on the SF‐36 at three or six months compared to qigong (3 months: Physical Component scale score: MD −0.77 95% CI −3.71 to 2.17; Mental Component scale score: MD −0.34, 95% CI −4.15 to 3.47; 6 months: Physical Component scale score: MD −3.60, 95% CI −6.65 to −0.55; Mental Component scale score: MD −0.02, 95% CI −3.82 to 3.78; low‐ to very‐low certainty evidence [downgraded for bias and imprecision]; Analysis 6.3; Analysis 6.4).
6.3. Analysis.

Comparison 6: Yoga versus qigong, Outcome 3: Physical quality of life
6.4. Analysis.

Comparison 6: Yoga versus qigong, Outcome 4: Mental quality of life
Depression
We are uncertain of the effect of yoga on depression measured on the Geriatric Depression Scale at three or six months compared to qigong (3 months: MD −0.65, 95% CI −1.58 to 0.28; 6 months: MD −0.30, 95% −1.09 to 0.49; very low‐certainty evidence [downgraded for risk of bias and very serious imprecision]; Analysis 6.5).
6.5. Analysis.

Comparison 6: Yoga versus qigong, Outcome 5: Depression
Adverse events
Teut 2016 reported assessing adverse events, but did not present any results on adverse events.
Minor outcome
Measures of work disability
The study did not report work‐related disability.
6. Yoga plus exercise versus exercise alone
One study compared the effects of yoga plus exercise to exercise alone (Wattamwar 2013) (Analysis 8.1; Analysis 8.2). The study compared three weekly occupational therapy classes (characterized as back school therapy and mat and exercise ball exercises) to two weekly occupational therapy classes and one weekly yoga class.
8.1. Analysis.

Comparison 8: Yoga plus exercise versus exercise alone, Outcome 1: Back‐specific functional status at short–intermediate term (10 weeks)
8.2. Analysis.

Comparison 8: Yoga plus exercise versus exercise alone, Outcome 2: Pain at short–intermediate term (10 weeks)
Major outcomes
Back‐specific functional status
We are uncertain about the effect of yoga plus exercise on back‐specific function measured on the Oswestry Disability Index at 10 weeks compared to exercise alone (MD −3.68, 95% CI −8.44 to 1.08; 24 participants; very low certainty evidence [downgraded for very serious risk of bias and imprecision]).
Pain
We are uncertain about the effect of yoga plus exercise on pain at 10 weeks compared to exercise alone (MD −3.20, 95% CI −13.76 to 7.36; 24 participants; very low certainty evidence [downgraded for very serious risk of bias and imprecision]).
Clinical improvement
The study did not report clinical improvement.
Depression
The study did not report depression.
Quality of life
The study did not report physical or mental quality of life.
Adverse events
The study did not report adverse events.
Minor outcomes
Measures of work disability
The study did not report work‐related disability.
Discussion
Summary of main results
Yoga versus sham yoga
We found no studies comparing yoga to a sham yoga intervention for chronic low back pain. A sham comparison to yoga would clarify the extent to which the effects of yoga are related to the belief that participants are practicing yoga. Depending upon the form of the sham, this could serve as a blinded comparison between yoga and another active intervention. For example, if a yoga intervention was compared to an exercise intervention that is not yoga, but that participants believe is yoga, we would have information on a blinded comparison between yoga and the other exercise.
Yoga versus non‐exercise (a waiting list, a minimal intervention, or usual care)
We found low‐ to moderate‐certainty evidence that yoga results in a small improvements in back‐related function at short, short–intermediate, intermediate, and long term; however, the improvements do not meet predetermined levels of clinical significance at any time point. We also found low‐ to moderate‐certainty evidence that yoga results in small and clinically non‐important improvements in pain at short, short–intermediate, intermediate, and long term. We found low‐certainty evidence that overall clinical improvement was more than twice as likely with yoga at short, short–intermediate, and intermediate term. We found low‐ to moderate‐certainty evidence for small to moderate improvements in physical quality of life at short, short–intermediate, and intermediate term. There was moderate‐certainty evidence for a small improvement in mental quality of life at short–intermediate and intermediate term, and low certainty evidence of little or no improvement in mental quality of life at long term. There was low‐certainty evidence of little to no difference in depression at short–intermediate term and small improvements in depression at intermediate, and long term. One study provided low‐certainty evidence on fewer days of work‐related disability with yoga at short, intermediate, and long term. There was low‐certainty evidence that adverse events, primarily exacerbation of back pain, were more common in yoga than in non‐exercise control groups, although not all studies reported assessing adverse events. Yoga was not described as associated with serious adverse events.
Yoga versus exercise
We found moderate‐certainty evidence of little or no difference between yoga and other exercise in back‐related function at short and short–intermediate term, and low‐certainty evidence of little or no difference at intermediate term. Evidence on differences between yoga and other exercise for pain was very‐low certainty at all time points due to serious risk of bias and imprecision, and we are therefore uncertain about these outcomes. Likewise, evidence on clinical improvement and on physical and mental quality of life was very‐low certainty. One study provided low‐certainty evidence for little to no difference in days of work‐related disability with yoga at short and intermediate term, and possibly slightly fewer days at long term. There was low‐certainty evidence of little or no difference in the risk of adverse events with yoga compared to other back‐focused exercise. Although the quantity of evidence on the comparison between yoga and back‐focused exercise has increased since the original version of this review, the total amount and quality of evidence is still limited, particularly for pain and quality of life outcomes, and for back‐related function at the long term.
Overall completeness and applicability of evidence
The trials included in this review were carried out in the US, India, the UK, Croatia, Germany, Sweden, and Turkey with a mix of primary care and community participants. The type of yoga was primarily iyengar and some other mixed hatha yoga practices, and the yoga interventions were specifically designed for people with low back pain. The instructors had a range of yoga training backgrounds and experience with people with low back pain. The results of this review could be generalized across multiple hatha yoga practices and sources of participants (primary care or community) in different countries. This update provides additional evidence on both yoga compared to non‐exercise controls and yoga compared to exercise controls, as well as some new evidence on yoga compared to qigong. There was also new evidence from low SES populations and older populations. However, there remains a need for additional evidence on yoga compared to exercise and other active interventions, as well as low SES populations, older populations, or populations with serious comorbidities. We found inconsistent reporting of adverse events, with some studies not mentioning safety outcomes, which makes it difficult to assess the balance of benefits and harms for the practice of yoga. It should be noted that the yoga interventions were designed specifically for people with low back pain and classes were supervised by trained instructors, and, therefore, this evidence of benefit and lack of serious harms would not necessarily apply to all yoga practices or to yoga undertaken without expert guidance.
Quality of the evidence
None of the included studies blinded participants or providers to treatment assignment, and all outcomes were self‐reported. Therefore, all studies were at high risk of performance and detection bias, and we judged none of the evidence as high certainty. Several comparisons between yoga and non‐exercise controls were downgraded for imprecision (few participants) or inconsistency (heterogeneity between studies), and, therefore, the comparisons between yoga and non‐exercise controls were primarily of moderate or low certainty.
Despite the addition to this update of four studies comparing yoga to another active intervention, the number of studies on yoga versus exercise controls remains small relative to those comparing yoga to a non‐exercise control such as waiting list or education. Aside from back‐specific function at short and short–intermediate term, the evidence was downgraded for imprecision (few participants or few events, or both) as well as risk of bias and, therefore, all other comparisons between yoga and exercise controls were of low or very low certainty.
Although some heterogeneity was expected, many analyses displayed unexplained heterogeneity that required downgrading the evidence. Potential sources of heterogeneity, including the characteristics of the yoga and control interventions, and the duration of treatment and follow‐up, were difficult to explore through subgroup analysis because of the complex patterns of variation between the trials. We had planned to compare yoga interventions with and without a mind component but found no interventions clearly carried out without a mind component. Although the style of yoga was most frequently characterized as iyengar or hatha, most yoga interventions were specially modified or developed for the trials and we could not identify patterns of yoga postures to use for subgrouping. It should be noted that research indicates that randomized trials of yoga with different yoga styles do not differ in their odds of reaching positive conclusions (Cramer 2016b). Regarding the intensity of the yoga intervention, most studies provided yoga classes once to three times per week, although one study provided daily classes and another provided an all‐day intervention. We separately analyzed the yoga trial that was intensive and provided an all‐day yoga intervention. We considered subgroup analyses by type of non‐exercise intervention, but most studies comparing yoga to a non‐exercise control intervention included some form of booklet or other educational material, and some trials (e.g. Jacobs 2004; Saper 2009) also provided the intervention group with educational materials. Finally, 11 trials reported outcomes several months after the end of yoga classes: approximately three months after treatment (Groessl 2017; Highland 2018; Saper 2009; Sherman 2005; Sherman 2011; Teut 2016; Williams 2005), six months after treatment (Nambi 2014; Williams 2009), and approximately nine months after treatment (Bramberg 2017; Tilbrook 2011). In all but one trial (Williams 2009), all outcomes at intermediate term were measured in participants who were no longer on treatment. Although it is possible that effects of interventions would decrease with increasing time off treatment, and we hypothesized that this was one reason for observing a smaller effect size for pain at six months in higher‐certainty studies that also had shorter treatment durations, we did not observe the same relationship for back‐related function. It was not possible to separate the issue of treatment duration and study quality, and we also could not discern any general relationship between effect size and time after end of treatment.
Potential biases in the review process
We created funnel plots for the two analyses with the required minimum of 10 studies, and because one of the funnel plots was consistent with a pattern of publication bias we downgraded the certainty of the evidence for the effect estimate. It is not yet possible to create additional funnel plots for other analyses. Although we carried out extensive searches for studies, and contacted authors of identified studies to obtain unpublished information as well as clarifications of published data, we cannot rule out the possibility of publication bias. Specifically, we identified one study that appears to have been completed some years ago, but for which there are no published results (Saper 2016). We cannot rule out the possibility that this and additional studies that are unknown to us may have produced results that are less positive than the results we found in published studies. We also note that three of the four studies carried out in India were at high risk of bias, and that trials of yoga conducted in India have been found to be more positive than trials conducted outside of India (Cramer 2015a).
Agreements and disagreements with other studies or reviews
Despite some differences in specific included studies, outcomes assessed, and choices of outcome time points, our findings are in broad agreement with other reviews of yoga as a treatment for low back pain (Chou 2017; Cramer 2013; Crow 2015; Hill 2013; Holtzman 2013; Posadzki 2011; Skelly 2018; Ward 2013). Yoga appears to be more effective than no treatment or minimal interventions such as education for improving function and pain in chronic non‐specific low back pain; effect sizes are small to moderate. This review also agrees with previous reviews in finding that the evidence for comparisons with non‐exercise controls is clearer and the benefits of yoga are larger, while any differences between yoga and back‐focused exercise are relatively uncertain. Finally, this review agrees with a review of interventions for non‐specific low back pain in older adults that the amount of evidence in older adults is very limited (Nascimento 2019).
Although RCTs are not good sources of information on rare adverse events, our review was also consistent with a previous systematic review of the safety of yoga in finding that yoga results in more adverse events than psychological or educational interventions but the same number of adverse events as non‐yoga back‐focused exercise (Cramer 2015b).
With regard to the broader domain of exercise for chronic low back pain, this review and one recent Cochrane Review on exercise for chronic low back pain (Hayden 2021) both found that exercise was better than no exercise for pain. However, the Hayden 2021 review found moderate‐certainty evidence for a clinically significant difference between exercise and no exercise for pain (MD −15.2, 95% CI −18.3 to −12.2), while the current review found moderate‐certainty evidence for a smaller and clinically unimportant difference between yoga and no exercise (MD −4.53, 95% CI −6.61 to −2.46). Meanwhile, when the current review directly compared the effects of yoga and non‐yoga exercise for pain, the current review found very low‐certainty evidence for little or no difference between yoga and non‐yoga exercise (MD 2.68, 95% CI −2.01 to 7.36). It is unclear whether additional evidence will confirm that yoga is indeed a less efficacious form of exercise for pain, or this inconsistency between review findings is related to the specific interventions in the included trials, given variations in components of both yoga and non‐yoga exercise interventions. With regard to back function, the Hayden 2021 review found moderate‐certainty evidence of little or no difference between exercise and no exercise in back‐specific function (MD −0.38, 95% CI −1.33 to 0.62 on the RMDQ), which is consistent with our finding of low‐certainty evidence for a small and clinically unimportant difference between yoga and no exercise (MD −1.69, 95% CI −2.73 to −0.65 on the RMDQ). Further evidence might clarify the effects of both yoga and non‐yoga exercise for back function and identify whether all exercise is of limited benefit for chronic low back pain or there are specific components of yoga and non‐yoga exercise interventions that may be of benefit.
Authors' conclusions
Implications for practice.
We found that compared to no exercise yoga may result in a clinically unimportant improvement in back‐related functioning at three months and is probably more effective than non‐exercise for back‐related functioning at short (four to six weeks) and long term (12 months). Yoga is probably more effective than no exercise in pain reduction at short–intermediate term (three to four months) and intermediate term (six months). Yoga may also be more effective for back‐related function and pain at other time points. However, differences for pain were not clinically significant at any time point, and differences for back function were small to moderate. There is probably no difference between yoga and other exercise for back‐related functioning at short or short–intermediate term and there may be no difference at intermediate term. There is no evidence for other differences between yoga and other exercise but information is limited and conclusions are uncertain. The risk of adverse events is higher with yoga than with no exercise and similar between yoga and other exercise; it appears that yoga is not associated with serious adverse effects. The choice to use yoga instead of no exercise should be made with an understanding that relative improvements in back‐related function and reductions in pain may be clinically unimportant, and the choice to use yoga instead of other forms of exercise should be made with an understanding that there is probably no difference between yoga and other exercise for back‐related function while differences between yoga and other exercise for pain are uncertain. Choices may otherwise depend on availability, cost, and participant or provider preference. Clinicians should caution patients that our knowledge of the effects of yoga relies upon trials in which the yoga interventions were specifically designed for treatment of low back pain, and were provided by experienced teachers, factors which may be related to both effectiveness and safety. This review does not include studies comparing different types or amounts of yoga, and does not provide information on particular types or regimens of yoga practice.
Implications for research.
We found 11 studies that are not yet published or not yet assessed by our review team, and 18 ongoing studies that are potentially relevant to this topic. Additional research testing yoga versus non‐exercise controls might improve the confidence in the estimates of effect for pain and for all outcomes at long term (12 months or longer). Further trials in specific populations, including low socioeconomic populations, older people, and populations with comorbidities, may clarify whether there are subpopulations in whom use of yoga may be helpful or harmful. Meanwhile, additional high‐quality studies testing yoga versus non‐yoga exercise would be useful in clarifying the comparative benefits of these therapies, including what elements of yoga and other exercise interventions might be helpful in chronic low back pain, and whether there are subpopulations in whom yoga or other exercises may be either beneficial or problematic. All studies should include reporting on adverse events at both short and long term. Trials should also include measurement of depression and quality of life, to investigate whether the mind component of yoga is effective in improving these patient‐important outcomes, and should include long‐term follow‐up to demonstrate whether yoga is likely to be acceptable and effective in usual clinical practice. Given the lack of trials of sham yoga, there is also a need for additional methodologic research in this field, particularly into the potential influence of people's preferences and expectations on outcomes within randomized trials of yoga.
What's new
| Date | Event | Description |
|---|---|---|
| 13 November 2022 | New citation required and conclusions have changed | The change in conclusions is primarily that there is now a higher level of confidence in evidence on comparisons between yoga and other exercise for back related function. The certainty of evidence for little or no difference in back‐specific functional status between yoga and non‐yoga exercise has increased. There is new information on pain for the comparison between yoga and non‐yoga exercise. There is new evidence on work‐related disability on yoga compared to qigong. In 2017 the certainty of the evidence was very low at 3‐4 months and 6 months, while in 2022 the certainty of evidence for little or no difference is moderate at 3‐4 months and low at 6 months. |
| 31 August 2021 | New search has been performed | The search was rerun on 31 August 2021. Nine new studies were added to 12 studies from the previous review for a total of 21 included studies (2223 participants). The comparison between yoga and sham yoga was added as the primary comparison for the review, however no studies relevant to this comparison were identified. |
History
Protocol first published: Issue 7, 2013 Review first published: Issue 1, 2017
Acknowledgements
We gratefully acknowledge the provision of unpublished trial data by the following: Michael C Acree, PhD, and Bradly Jacobs, MD, MPH; Elisabeth Björk Brämberg, PhD; Erik Groessl, PhD; Catherine Hewitt, PhD and Helen Tilbrook, MSc; Osama Neyaz, MBBS, DNB; and Robert Saper, MD. We are grateful for additional unpublished data provided by Holger Cramer, PhD.
We gratefully acknowledge the feedback of the Cochrane Back and Neck editors, statisticians, and peer reviewers, including Anita Barros Amorim, School of Health Sciences, Faculty of Medicine and Health, The University of Sydney and Matthew D Jones Department of Exercise Physiology, School of Health Sciences, Faculty of Medicine and Health, The University of New South Wales, Sydney, Australia.
We acknowledge the authorship contribution of Christopher R D'Adamo to the previous version of the review.
Finally, we gratefully acknowledge Maggie Tiong and Joanna Liu from the Institute for Work & Health for search support.
Appendices
Appendix 1. Cochrane Trials Registers, CENTRAL, MEDLINE, Embase, and CINAHL search strategies
Cochrane Back and Neck group Trials Register
Last searched 31 August 2021
1 yoga AND INREGISTER
2 (2020 OR 2021):YR AND INREGISTER
4 #3 AND #2
10 September 2020 search
1 yoga AND INREGISTER
2 2019:YR AND INREGISTER
3 2020:YR AND INREGISTER
4 #3 OR #2
5 #4 AND #1
Complementary Medicine Field Trials Register
Last searched 31 August 2021
1 back OR backache OR pain AND COMPMED:INREGISTER
2 yoga OR asana OR pranayama OR dhyana AND COMPMED:INREGISTER
3 #1 AND #2
4 (2020 OR 2021):YR AND COMPMED:INREGISTER
5 #3 AND #4
10 September 2020 search
1 back OR backache OR pain AND COMPMED:INREGISTER
2 yoga OR asana OR pranayama OR dhyana AND COMPMED:INREGISTER
3 #1 AND #2 5
4 2019:YR AND COMPMED:INREGISTER
5 2020:YR AND COMPMED:INREGISTER
3 June 2019 search
1 (back OR backache OR pain) AND (yoga OR asana OR pranayama OR dhyani) AND COMPMED:INREGISTER
2 #1 AND (2018 TO 2019:YR)
CENTRAL
Last searched 31 August 2021
1 MESH DESCRIPTOR Back Pain EXPLODE ALL AND CENTRAL:TARGET
2 MESH DESCRIPTOR Low Back Pain EXPLODE ALL AND CENTRAL:TARGET
3 dorsalgia AND CENTRAL:TARGET
4 coccyx or coccydynia or spondylosis or sciatica AND CENTRAL:TARGET
5 (lumb* NEAR3 pain) AND CENTRAL:TARGET
6 MESH DESCRIPTOR Spine EXPLODE ALL AND CENTRAL:TARGET
7 MESH DESCRIPTOR Spinal Diseases EXPLODE ALL AND CENTRAL:TARGET
8 (lumbago or discitis) AND CENTRAL:TARGET
9 spinal fusion AND CENTRAL:TARGET
10 facet NEAR joint* AND CENTRAL:TARGET
11 MESH DESCRIPTOR Intervertebral Disc EXPLODE ALL AND CENTRAL:TARGET
12 postlaminectomy AND CENTRAL:TARGET
13 arachnoiditis AND CENTRAL:TARGET
14 failed NEAR back AND CENTRAL:TARGET
15 MESH DESCRIPTOR Cauda Equina EXPLODE ALL AND CENTRAL:TARGET
16 lumb* NEAR vertebra* AND CENTRAL:TARGET
17 stenosis NEAR (spine or root or spinal) AND CENTRAL:TARGET
18 slipped NEAR (disc* or disk*) AND CENTRAL:TARGET
19 degenerat* NEAR (disc* or disk*) AND CENTRAL:TARGET
20 herniat* NEAR (disc* or disk*) AND CENTRAL:TARGET
21 displac* NEAR (disc* or disk*) AND CENTRAL:TARGET
22 prolaps* NEAR (disc* or disk*) AND CENTRAL:TARGET
23 back NEAR pain AND CENTRAL:TARGET
24 back disorder* AND CENTRAL:TARGET
25 MESH DESCRIPTOR Sciatic Neuropathy EXPLODE ALL AND CENTRAL:TARGET
26 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25
27 MESH DESCRIPTOR Yoga EXPLODE ALL AND CENTRAL:TARGET
28 yoga AND CENTRAL:TARGET
29 yogic AND CENTRAL:TARGET
30 yogi AND CENTRAL:TARGET
31 asana* AND CENTRAL:TARGET
32 pranayama AND CENTRAL:TARGET
33 dhyana AND CENTRAL:TARGET
34 #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33
35 #34 AND #26
36 2020:YR AND 01/09/2020_TO_31/08/2021:CRSINCENTRAL AND CENTRAL:TARGET
37 2021:YR AND 01/09/2020_TO_31/08/2021:CRSINCENTRAL AND CENTRAL:TARGET
38 #36 OR #37
39 #35 AND #38
10 September 2020 search
1 MESH DESCRIPTOR Back Pain EXPLODE ALL AND CENTRAL:TARGET
2 MESH DESCRIPTOR Low Back Pain EXPLODE ALL AND CENTRAL:TARGET
3 dorsalgia AND CENTRAL:TARGET 9
4 coccyx or coccydynia or spondylosis or sciatica AND CENTRAL:TARGET
5 (lumb* NEAR pain) AND CENTRAL:TARGET
6 MESH DESCRIPTOR Spine EXPLODE ALL AND CENTRAL:TARGET
7 MESH DESCRIPTOR Spinal Diseases EXPLODE ALL AND CENTRAL:TARGET
8 lumbago or discitis AND CENTRAL:TARGET
9 spinal fusion AND CENTRAL:TARGET
10 facet NEAR joint* AND CENTRAL:TARGET
11 MESH DESCRIPTOR Intervertebral Disc EXPLODE ALL AND CENTRAL:TARGET
12 postlaminectomy AND CENTRAL:TARGET
13 arachnoiditis AND CENTRAL:TARGET
14 failed NEAR back AND CENTRAL:TARGET
15 MESH DESCRIPTOR Cauda Equina EXPLODE ALL AND CENTRAL:TARGET
16 lumb* NEAR vertebra* AND CENTRAL:TARGET
17 stenosis NEAR (spine or root or spinal) AND CENTRAL:TARGET 1
18 (slipped NEAR disc*) OR (slipped NEAR disk*) AND CENTRAL:TARGET
19 (degenerat* NEAR disc*) OR (degenerat* NEAR disk*) AND CENTRAL:TARGET
20 (herniat* NEAR disc*) OR (herniat* NEAR disk*) AND CENTRAL:TARGET
21 (displac* NEAR disc*) OR (displac* NEAR disk*) AND CENTRAL:TARGET
22 (prolaps* NEAR disc*) OR (prolaps* NEAR disk*) AND CENTRAL:TARGET
23 back NEAR pain AND CENTRAL:TARGET
24 back disorder* AND CENTRAL:TARGET
25 MESH DESCRIPTOR Sciatic Neuropathy EXPLODE ALL AND CENTRAL:TARGET
26 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 AND CENTRAL:TARGET
27 MESH DESCRIPTOR Yoga EXPLODE ALL AND CENTRAL:TARGET
28 yoga AND CENTRAL:TARGET
29 yogic AND CENTRAL:TARGET
30 yogi AND CENTRAL:TARGET
31 asana* AND CENTRAL:TARGET
32 pranayama AND CENTRAL:TARGET
33 dhyana AND CENTRAL:TARGET
34 #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33
35 #34 AND #26
36 2019:YR AND CENTRAL:TARGET
37 2020:YR AND CENTRAL:TARGET
38 #36 OR #37
39 #35 AND #38
3 June 2019 search
1 MESH DESCRIPTOR Back Pain EXPLODE ALL AND CENTRAL:TARGET
2 MESH DESCRIPTOR Low Back Pain EXPLODE ALL AND CENTRAL:TARGET
3 dorsalgia AND CENTRAL:TARGET
4 coccyx or coccydynia or spondylosis or sciatica AND CENTRAL:TARGET
5 (lumb* NEAR3 pain) AND CENTRAL:TARGET
6 MESH DESCRIPTOR Spine EXPLODE ALL AND CENTRAL:TARGET
7 MESH DESCRIPTOR Spinal Diseases EXPLODE ALL AND CENTRAL:TARGET
8 (lumbago or discitis) AND CENTRAL:TARGET
9 spinal fusion AND CENTRAL:TARGET
10 facet NEAR joint* AND CENTRAL:TARGET
11 MESH DESCRIPTOR Intervertebral Disc EXPLODE ALL AND CENTRAL:TARGET
12 postlaminectomy AND CENTRAL:TARGET
13 arachnoiditis AND CENTRAL:TARGET
14 failed NEAR back AND CENTRAL:TARGET
15 MESH DESCRIPTOR Cauda Equina EXPLODE ALL AND CENTRAL:TARGET
16 lumb* NEAR vertebra* AND CENTRAL:TARGET
17 stenosis NEAR (spine or root or spinal) AND CENTRAL:TARGET
18 slipped NEAR (disc* or disk*) AND CENTRAL:TARGET
19 degenerat* NEAR (disc* or disk*) AND CENTRAL:TARGET
20 herniat* NEAR (disc* or disk*) AND CENTRAL:TARGET
21 displac* NEAR (disc* or disk*) AND CENTRAL:TARGET
22 prolaps* NEAR (disc* or disk*) AND CENTRAL:TARGET
23 back NEAR pain AND CENTRAL:TARGET
24 back disorder* AND CENTRAL:TARGET
25 MESH DESCRIPTOR Sciatic Neuropathy EXPLODE ALL AND CENTRAL:TARGET
26 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 AND CENTRAL:TARGET
27 MESH DESCRIPTOR Yoga EXPLODE ALL AND CENTRAL:TARGET
28 yoga AND CENTRAL:TARGET
29 yogic AND CENTRAL:TARGET
30 yogi AND CENTRAL:TARGET
31 asana* AND CENTRAL:TARGET
32 pranayama AND CENTRAL:TARGET
33 dhyana AND CENTRAL:TARGET
34 #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 AND CENTRAL:TARGET
35 #34 AND #26 AND CENTRAL:TARGET
36 #35 AND (2018 TO 2019:YR)
MEDLINE
Last searched 31 August 2021
1 randomized controlled trial.pt.
2 controlled clinical trial.pt.
3 pragmatic clinical trial.pt.
4 random*.ti,ab.
5 placebo.ab,ti.
6 controlled.ti,ab.
7 prospective.ti,ab.
8 trial.ab,ti.
9 groups.ab,ti.
10 or/1‐9
11 (animals not (humans and animals)).sh.
12 10 not 11
13 dorsalgia.tw,kf.
14 exp Back Pain/
15 (backache or back‐ache).tw,kf.
16 exp Low Back Pain/
17 (back adj3 pain).tw,kf.
18 (lumb* adj3 pain).tw,kf.
19 coccyx.tw,kf.
20 coccydynia.tw,kf.
21 sciatica.tw,kf.
22 exp sciatic neuropathy/
23 spondylosis.tw,kf.
24 lumbago.tw,kf.
25 back disorder*.tw,kf.
26 or/13‐25
27 Yoga/
28 yoga.tw,kf.
29 yogic.tw,kf.
30 yogi.tw,kf.
31 asana*.tw,kf.
32 pranayama.tw,kf.
33 dhyana.tw,kf.
34 or/27‐33
35 12 and 26 and 34
36 limit 35 to yr=2020‐2021
37 limit 35 to ed=20200910‐20210831
38 36 or 37
November 2018 search. Anatomy and intervention terms were searched in the .tw,kf fields instead of the.mp field
1 randomized controlled trial.pt.
2 controlled clinical trial.pt.
3 pragmatic clinical trial.pt.
4 random*.ti,ab.
5 placebo.ab,ti.
6 controlled.ti,ab.
7 prospective.ti,ab.
8 trial.ab,ti.
9 groups.ab,ti.
10 or/1‐9
11 (animals not (humans and animals)).sh.
12 10 not 11
13 dorsalgia.tw,kf.
14 exp Back Pain/
15 (backache or back‐ache).tw,kf.
16 exp Low Back Pain/
17 ((back or lumb*) adj3 pain).tw,kf.
18 coccyx.tw,kf.
19 coccydynia.tw,kf.
20 sciatica.tw,kf.
21 exp sciatic neuropathy/
22 spondylosis.tw,kf.
23 lumbago.tw,kf.
24 back disorder*.tw,kf.
25 or/13‐24
26 Yoga/
27 yoga.tw,kf.
28 yogic.tw,kf.
29 yogi.tw,kf.
30 asana*.tw,kf.
31 pranayama.tw,kf.
32 dhyana.tw,kf.
33 or/26‐32
34 12 and 25 and 33
35 limit 34 to yr=2016‐2018
36 limit 34 to ed=20160310‐20181107
37 35 or 36
Embase
Last searched 31 August 2021
1 Randomized Controlled Trial/
2 exp controlled Study/
3 Controlled clinical trial/
4 Double Blind Procedure/
5 Single Blind Procedure/
6 randomization/
7 crossover procedure/
8 placebo/
9 random*.ti,ab.
10 placebo?.ti,ab.
11 allocat*.ti,ab.
12 assign*.ti,ab.
13 blind*.ti,ab.
14 (compare or compared or comparing or comparison or comparative).ti,ab.
15 ((controlled adj7 study) or (controlled adj7 design) or (controlled adj7 trial)).ti,ab.
16 (crossover or cross‐over).ti,ab.
17 trial*.ti,ab.
18 ((singl* adj7 blind*) or (doubl* adj7 blind*) or (trebl* adj7 blind*) or (tripl* adj7 blind*) or (singl* adj7 mask*) or (doubl* adj7 mask*) or (trebl* adj7 mask*) or (tripl* adj7 mask*)).ti,ab.
19 or/1‐18
20 exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/
21 human/ or normal human/ or human cell/
22 20 and 21
23 20 not 22
24 19 not 23
25 dorsalgia.tw,kw.
26 back pain.tw,kw.
27 exp LOW BACK PAIN/
28 exp BACKACHE/
29 (lumb* adj3 pain).tw,kw.
30 coccyx.tw,kw.
31 coccydynia.tw,kw.
32 sciatica.tw,kw.
33 sciatica/
34 exp ISCHIALGIA/
35 spondylosis.tw,kw.
36 lumbago.tw,kw.
37 back disorder*.tw,kw.
38 or/25‐37
39 yoga/
40 yoga.tw,kw.
41 yogic.tw,kw.
42 yogi.tw,kw.
43 asana*.tw,kw.
44 pranayama.tw,kw.
45 dhyana.tw,kw.
46 or/39‐45
47 24 and 38 and 46
48 limit 47 to yr=2020‐2021
49 limit 47 to dd=20200910‐20210831
50 48 or 49
3 June 2019 search. Study design filter was revised.
1 Randomized Controlled Trial/
2 exp controlled Study/
3 Controlled clinical trial/
4 Double Blind Procedure/
5 Single Blind Procedure/
6 randomization/
7 crossover procedure/
8 placebo/
9 random*.ti,ab.
10 placebo?.ti,ab.
11 allocat*.ti,ab.
12 assign*.ti,ab.
13 blind*.ti,ab.
14 (compare or compared or comparing or comparison or comparative).ti,ab.
15 (controlled adj7 (study or design or trial)).ti,ab.
16 (crossover or cross‐over).ti,ab.
17 trial*.ti,ab.
18 ((singl* or doubl* or trebl* or tripl*) adj7 (blind* or mask*)).ti,ab.
19 or/1‐18
20 exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/
21 human/ or normal human/ or human cell/
22 20 and 21
23 20 not 22
24 19 not 23
25 dorsalgia.tw,kw.
26 back pain.tw,kw.
27 exp LOW BACK PAIN/
28 exp BACKACHE/
29 (lumb* adj3 pain).tw,kw.
30 coccyx.tw,kw.
31 coccydynia.tw,kw.
32 sciatica.tw,kw.
33 sciatica/
34 exp ISCHIALGIA/
35 spondylosis.tw,kw.
36 lumbago.tw,kw.
37 back disorder*.tw,kw.
38 or/25‐37
39 yoga/
40 yoga.tw,kw.
41 yogic.tw,kw.
42 yogi.tw,kw.
43 asana*.tw,kw.
44 pranayama.tw,kw.
45 dhyana.tw,kw.
46 or/39‐45
47 24 and 38 and 46
48 limit 47 to yr=2018‐2019
49 limit 47 to dd=20181107‐20190603
50 48 or 49
November 2018 search. Anatomy and intervention terms were searched in the .tw,kw fields instead of the.mp field.
1 Randomized Controlled Trial/
2 Controlled Study/
3 Controlled clinical trial/
4 Double Blind Procedure/
5 Single Blind Procedure/
6 crossover procedure/
7 placebo/
8 random*.ti,ab.
9 placebo*.ti,ab.
10 allocat*.ti,ab.
11 assign*.ti,ab.
12 blind*.ti,ab.
13 (clinic* adj25 (study or trial)).ti,ab.
14 (compare or compared or comparing or comparison or comparative).ti,ab.
15 (controlled adj7 (study or design or trial)).ti,ab.
16 (crossover or cross‐over).ti,ab.
17 prospectiv*.ti,ab.
18 ((singl* or doubl* or trebl* or tripl*) adj7 (blind* or mask*)).ti,ab.
19 or/1‐18
20 exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/
21 human/ or normal human/ or human cell/
22 20 and 21
23 20 not 22
24 19 not 23
25 dorsalgia.tw,kw.
26 back pain.tw,kw.
27 exp LOW BACK PAIN/
28 exp BACKACHE/
29 (lumb* adj3 pain).tw,kw.
30 coccyx.tw,kw.
31 coccydynia.tw,kw.
32 sciatica.tw,kw.
33 sciatica/
34 exp ISCHIALGIA/
35 spondylosis.tw,kw.
36 lumbago.tw,kw.
37 back disorder*.tw,kw.
38 or/25‐37
39 yoga/
40 yoga.tw,kw.
41 yogic.tw,kw.
42 yogi.tw,kw.
43 asana*.tw,kw.
44 pranayama.tw,kw.
45 dhyana.tw,kw.
46 or/39‐45
47 24 and 38 and 46
48 limit 47 to yr="2016‐2018"
49 limit 47 to dd=20160311‐20181107
50 48 or 49
CINAHL
Last searched 31 August 2021
S61 S59 OR S60
S60 S58 AND EM 20200910‐20210831
S59 S58 Limiters ‐ Published Date: 20200901‐20210831
S58 S49 AND S57
S57 S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56
S56 "dhyana"
S55 "pranayama"
S54 "asana*"
S53 "yogi"
S52 "yogic"
S51 "yoga"
S50 (MH "Yoga+")
S49 S28 and S48
S48 S35 or S43 or S47
S47 S44 or S45 or S46
S46 "lumbago"
S45 (MH "Spondylolisthesis") OR (MH "Spondylolysis")
S44 (MH "Thoracic Vertebrae")
S43 S36 or S37 or S38 or S39 or S40 or S41 or S42
S42 lumb* N2 vertebra
S41 (MH "Lumbar Vertebrae")
S40 "coccydynia"
S39 "coccyx"
S38 "sciatica"
S37 (MH "Sciatica")
S36 (MH "Coccyx")
S35 S29 or S30 or S31 or S32 or S33 or S34
S34 lumb* N5 pain
S33 back pain
S32 backache or back‐ache
S31 (MH "Low Back Pain")
S30 (MH "Back Pain+")
S29 "dorsalgia"
S28 S26 NOT S27
S27 (MH "Animals")
S26 S7 or S12 or S19 or S25
S25 S20 or S21 or S22 or S23 or S24
S24 volunteer*
S23 prospectiv*
S22 control*
S21 followup stud*
S20 follow‐up stud*
S19 S13 or S14 or S15 or S16 or S17 or S18
S18 (MH "Prospective Studies+")
S17 (MH "Evaluation Research+")
S16 (MH "Comparative Studies")
S15 latin square
S14 (MH "Study Design+")
S13 (MH "Random Sample")
S12 S8 or S9 or S10 or S11
S11 random*
S10 placebo*
S9 (MH "Placebos")
S8 (MH "Placebo Effect")
S7 S1 or S2 or S3 or S4 or S5 or S6
S6 triple‐blind
S5 single‐blind
S4 double‐blind
S3 clinical W3 trial
S2 "randomi?ed controlled trial*"
S1 (MH "Clinical Trials+")
Appendix 2. PsycINFO, AMED, IndMED, trials registry search strategies
PsycINFO
Last searched 31 August 2021
1 clinical trials/
2 control*.mp.
3 random*.mp.
4 placebo.mp.
5 trial.mp.
6 blind.mp.
7 (compare or compared or comparing or comparison or comparative).mp.
8 exp Treatment/
9 or/1‐8
10 back pain/
11 dorsalgia.mp.
12 (backache or back‐ache).mp.
13 (lumb* adj3 pain).mp.
14 back pain.mp.
15 sciatica.mp.
16 lumbago.mp.
17 coccydynia.mp.
18 coccyx.mp.
19 spinal nerves/
20 lumbar spinal cord/
21 ((disc? adj degenerat*) or (disk? adj degenerat*)).mp.
22 ((disc? adj prolapse*) or (disk? adj prolapse*)).mp.
23 ((disc? adj herniat*) or (disk? adj herniat*)).mp.
24 back disorder*.mp.
25 or/10‐24
26 yoga/
27 yoga.mp.
28 yogic.mp.
29 yogi.mp.
30 asana*.mp.
31 pranayama.mp.
32 dhyana.mp.
33 or/26‐32
34 9 and 25 and 33
35 limit 34 to yr=2020‐2021
June 2019 search
1 clinical trials/
2 control*.mp.
3 random*.mp.
4 placebo.mp.
5 trial.mp.
6 (compare or compared or comparing or comparison or comparative).mp.
7 exp Treatment/
8 or/1‐7
9 back pain/
10 dorsalgia.mp.
11 (backache or back‐ache).mp.
12 (lumb* adj3 pain).mp.
13 back pain.mp.
14 sciatica.mp.
15 lumbago.mp.
16 coccydynia.mp.
17 coccyx.mp.
18 spinal nerves/
19 lumbar spinal cord/
20 ((disc? or disk?) adj degenerat*).mp.
21 ((disc? or disk?) adj prolapse*).mp.
22 ((disc? or disk?) adj herniat*).mp.
23 back disorder*.mp.
24 or/9‐23
25 yoga/
26 yoga.mp.
27 yogic.mp.
28 yogi.mp.
29 asana*.mp.
30 pranayama.mp.
31 dhyana.mp.
32 or/25‐31
33 8 and 24 and 32
34 limit 33 to yr=2018‐2019
AMED
Last searched 31 August 2021
1 yoga/
2 yoga.mp.
3 yogic.mp.
4 yogi.mp.
5 asana*.mp.
6 pranayama.mp.
7 dhyana.mp.
8 or/1‐7
9 low back pain/
10 Backache/
11 Back injuries/
12 back pain.mp.
13 (backache or back‐ache).mp.
14 (lumb* adj3 pain).mp.
15 Lumbar vertebrae/
16 coccyx.mp.
17 coccydynia.mp.
18 Sciatica/
19 sciatica.mp.
20 spondylosis.mp.
21 lumbago.mp.
22 dorsalgia.mp.
23 back disorder*.mp.
24 or/9‐23
25 8 and 24
26 limit 25 to yr=2020‐2021
IndMED
Last searched November 2018.
Advanced search, in "Anywhere" field:
yoga or asana or pranayama or dhyana or yogi or yogic
AND back
ClinicalTrials.gov
Last searched 31 August 2021
((yoga OR asana OR pranayama OR dhyana OR yogi OR yogic) AND (back pain OR lumbago OR dorsalgia OR lumbar pain OR sciatica OR coccydynia OR coccyx OR backache)) | First posted from 09/10/2020 to 08/31/2021
WHO ICTRP
Last searched 31 August 2021. Selected studies registered from 2019 to 2021
Basic search: Yoga AND back pain OR yoga AND lumbar pain OR yoga AND sciatica OR yoga AND backache OR yoga and lumbago OR yoga and dorsalgia
November 2018 search
Basic search: Yoga and back pain
Appendix 3. The GRADE approach to evidence synthesis
We categorized the certainty of evidence as follows.
High (⊕⊕⊕⊕): further research is very unlikely to change the confidence in the estimate of effect.
Moderate (⊕⊕⊕⊝): further research is likely to have an important impact in the confidence in the estimate of effect.
Low (⊕⊕⊝⊝): further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low (⊕⊝⊝⊝): any estimate of effect is very uncertain.
We graded the evidence available to answer each subquestion on the domains following criteria based on Ryan 2016.
1. Risk of bias
Confidence in the estimate of the effect decreases if studies have major limitations in design and conduct. We assessed five types of bias, described in detail in Table 4 and Table 5:
selection bias (random sequence generation, allocation concealment, group similarities at baseline);
performance bias (blinding of participants, blinding of personnel or care providers, co‐interventions, compliance);
attrition bias (incomplete outcome data, intention‐to‐treat analysis);
detection bias (blinding of outcome assessors, timing of outcome assessments);
reporting bias (selective reporting).
The certainty of evidence was downgraded one level for an estimate of effect that relied on studies with a high risk of bias in one of these domains. The certainty of evidence was downgraded two levels for an estimate of effect that relied heavily (i.e. approximately 50% or greater weight in the meta‐analysis) on studies with a high risk of bias in two or more of these domains.
2. Inconsistency
Inconsistency refers to heterogeneity between studies that does not have a plausible explanation. The I² statistic is an estimate of the percentage of the variability in effect estimates that is due to clinical or methodologic heterogeneity rather than chance. An I² statistic of 30% to 60% may represent moderate heterogeneity, 50% to 90% may represent substantial heterogeneity, and 75% to 100% may represent considerable heterogeneity (Deeks 2011). The design and conduct of yoga interventions for low back pain are highly variable and, therefore, heterogeneity is expected.
The certainty of evidence was downgraded one level when heterogeneity was substantial (i.e. I² ≥ 50%), and two levels when heterogeneity was considerable (i.e. I² ≥ 75%), unless there was a plausible explanation for the heterogeneity.
3. Indirectness
Indirectness refers to a mismatch between the population, intervention, comparator, or outcomes for the studies included in the review and the population, intervention, comparator, or outcomes for the research question being posed by the systematic review. The certainty of evidence was downgraded one level when there was indirectness for one element of the research question (e.g. population) and two levels when there was indirectness for two or more elements of the research question.
4. Imprecision
Imprecision refers to uncertainty in the results due to few participants or to wide confidence intervals.
We used the following guidance in judging imprecision.
For continuous outcomes
An outcome was downgraded one level for imprecision if:
the total number of participants was fewer than 400; or
the 95% confidence interval around the estimate of effect covered both no effect and a minimally important difference for that outcome, or if a minimally important difference was not prespecified, no effect and a standardized mean difference (SMD) of ± 0.5 or a risk ratio (RR) of ± 1.25 (Guyatt 2011).
An outcome was downgraded two levels for imprecision if both points above were true.
For dichotomous outcomes
An outcome was downgraded one level for imprecision if:
the total number of events was less than 300; or
the 95% confidence interval around the estimate of effect included both no effect and either appreciable benefit or appreciable harm. The threshold for 'appreciable benefit' or 'appreciable harm' was a relative risk reduction (RRR) or relative risk increase (RRI) greater than 25%.
An outcome was downgraded two levels for imprecision if both points above were true.
5. Publication bias
Publication bias refers to the selective publication of studies, which may bias the estimate of effect that is based on available studies.
The certainty of evidence was downgraded one level if a funnel plot to assess the potential for small‐study bias suggests that publication bias was present, or there was any other reason to strongly suspect that publication bias was present.
Data and analyses
Comparison 1. Yoga versus non‐exercise.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Back‐specific functional status | 15 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1.1 Back‐specific function at short term (4–8 weeks) | 8 | 474 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.61, ‐0.21] |
| 1.1.2 Back‐specific function at short–intermediate term (3 months) | 11 | 1155 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.50, ‐0.12] |
| 1.1.3 Back‐specific function at intermediate term (6 months) | 11 | 1157 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.52, ‐0.21] |
| 1.1.4 Back‐specific function at long term (12 months) | 3 | 532 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.45, ‐0.10] |
| 1.2 Pain | 12 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.2.1 Pain at short term (4–8 weeks) | 5 | 258 | Mean Difference (IV, Random, 95% CI) | ‐11.05 [‐14.22, ‐7.88] |
| 1.2.2 Pain at short–intermediate term (3 months) | 9 | 946 | Mean Difference (IV, Random, 95% CI) | ‐4.53 [‐6.61, ‐2.46] |
| 1.2.3 Pain at intermediate term (6 months) | 9 | 940 | Mean Difference (IV, Random, 95% CI) | ‐5.40 [‐8.58, ‐2.22] |
| 1.2.4 Pain at long term (12 months) | 3 | 521 | Mean Difference (IV, Random, 95% CI) | ‐5.87 [‐12.25, 0.50] |
| 1.3 Clinical improvement | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.3.1 Clinical improvement at short term (4–6 weeks) | 2 | 141 | Risk Ratio (M‐H, Random, 95% CI) | 2.62 [1.22, 5.67] |
| 1.3.2 Clinical improvement at short–intermediate term (3 months) | 4 | 353 | Risk Ratio (M‐H, Random, 95% CI) | 2.33 [1.46, 3.71] |
| 1.3.3 Clinical improvement at intermediate term (6 months) | 1 | 128 | Risk Ratio (M‐H, Random, 95% CI) | 2.53 [1.36, 4.71] |
| 1.4 Physical quality of life | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.4.1 Physical quality of life at short term (4 weeks) | 2 | 81 | Std. Mean Difference (IV, Random, 95% CI) | 0.50 [0.05, 0.95] |
| 1.4.2 Physical quality of life at short–intermediate term (3 months) | 6 | 686 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [0.03, 0.37] |
| 1.4.3 Physical quality of life at intermediate term (6 months) | 3 | 434 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.13, 0.46] |
| 1.4.4 Physical quality of life at long term (12 months) | 1 | 264 | Std. Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.07, 0.41] |
| 1.5 Mental quality of life | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.5.1 Mental quality of life at short term (4 weeks) | 2 | 81 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐1.24, 0.93] |
| 1.5.2 Mental quality of life at short–intermediate term (3 months) | 6 | 686 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [0.05, 0.35] |
| 1.5.3 Mental quality of life at intermediate term (6 months) | 3 | 434 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [0.00, 0.41] |
| 1.5.4 Mental quality of life at long term (12 months) | 1 | 264 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.17, 0.31] |
| 1.6 Depression | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.6.1 Depression at short term (6–8 weeks) | 2 | 46 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.44 [‐2.11, ‐0.76] |
| 1.6.2 Depression at short–intermediate term (3 months) | 3 | 241 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.44, 0.07] |
| 1.6.3 Depression at intermediate term (6 months) | 2 | 197 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.63, ‐0.06] |
| 1.6.4 Depression at long term (12 months) | 1 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.92, ‐0.08] |
| 1.7 Adverse events | 8 | 1037 | Risk Ratio (M‐H, Random, 95% CI) | 4.76 [2.08, 10.89] |
| 1.8 Measures of work disability (days) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.8.1 Sickness absenteeism at short term (6 weeks) | 1 | 83 | Mean Difference (IV, Random, 95% CI) | ‐4.80 [‐11.68, 2.08] |
| 1.8.2 Sickness absenteeism at intermediate term (6 months) | 1 | 81 | Mean Difference (IV, Random, 95% CI) | ‐8.00 [‐16.53, 0.53] |
| 1.8.3 Sickness absenteeism at long term (12 months) | 1 | 83 | Mean Difference (IV, Random, 95% CI) | ‐5.60 [‐13.26, 2.06] |
Comparison 2. Subgroup analyses for yoga versus non‐exercise.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Subgroup analysis by socioeconomic status (SES) for back‐specific functional status at 6 months | 11 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1.1 Participants not recruited from low SES population | 9 | 972 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.56, ‐0.18] |
| 2.1.2 Participants recruited from low SES population | 2 | 185 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.66, ‐0.05] |
| 2.2 Subgroup analysis by SES for pain at 6 months | 9 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.2.1 Participants not recruited from low SES population | 7 | 756 | Mean Difference (IV, Random, 95% CI) | ‐4.69 [‐8.53, ‐0.86] |
| 2.2.2 Participants recruited from low SES population | 2 | 184 | Mean Difference (IV, Random, 95% CI) | ‐7.97 [‐13.21, ‐2.73] |
Comparison 3. Sensitivity analyses for yoga versus non‐exercise.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Back‐specific functional status sensitivity analyses (higher‐quality studies) | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1.1 Back‐specific function at short term (6 weeks) limited to higher‐quality studies | 2 | 200 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.75, ‐0.10] |
| 3.1.2 Back‐specific function at short–intermediate term (3–4 months) limited to higher‐quality studies | 4 | 589 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.72, ‐0.03] |
| 3.1.3 Back‐specific function at intermediate term (6 months) limited to higher‐quality studies | 4 | 582 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.60, ‐0.01] |
| 3.1.4 Back‐specific function at long term (12 months) limited to higher‐quality studies | 1 | 275 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.47, 0.01] |
| 3.2 Back‐specific functional status sensitivity analyses (complete case) | 13 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.2.1 Back‐specific function at short term (4–6 weeks) using complete‐case data | 6 | 367 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.57, ‐0.14] |
| 3.2.2 Back‐specific function at short–intermediate term (3–4 months) using complete‐case data | 10 | 1094 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.60, ‐0.17] |
| 3.2.3 Back‐specific function at intermediate term (6 months) using complete‐case data | 10 | 1055 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.58, ‐0.22] |
| 3.2.4 Back‐specific function at long term (12 months) using complete‐case data | 3 | 507 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.48, ‐0.12] |
| 3.3 Back‐specific functional status sensitivity analyses (change values) | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.3.1 Back‐specific function at short term (4–6 weeks) using change values | 2 | 133 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.53, 0.15] |
| 3.3.2 Back‐specific function at short–intermediate term (3–4 months) using change values | 6 | 746 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.45, ‐0.16] |
| 3.3.3 Back‐specific function at intermediate term (6 months) using change values | 3 | 499 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.60, ‐0.19] |
| 3.3.4 Back‐specific function at long term (12 months) using change values | 2 | 390 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.55, ‐0.14] |
| 3.4 Pain sensitivity analyses (higher‐quality studies) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.4.1 Pain at short–intermediate term (3–4 months) limited to higher‐quality studies | 2 | 377 | Mean Difference (IV, Random, 95% CI) | ‐4.49 [‐7.11, ‐1.87] |
| 3.4.2 Pain at intermediate term (6 months) limited to higher‐quality studies | 2 | 366 | Mean Difference (IV, Random, 95% CI) | ‐2.40 [‐5.35, 0.54] |
| 3.4.3 Pain at long term (12 months) limited to higher‐quality studies | 1 | 265 | Mean Difference (IV, Random, 95% CI) | ‐1.41 [‐4.58, 1.76] |
| 3.5 Pain sensitivity analyses (complete case) | 10 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.5.1 Pain at short–intermediate term (3–4 months) using complete‐case data | 8 | 853 | Mean Difference (IV, Random, 95% CI) | ‐4.71 [‐6.85, ‐2.56] |
| 3.5.2 Pain at intermediate term (6 months) using complete‐case data | 8 | 847 | Mean Difference (IV, Random, 95% CI) | ‐6.75 [‐11.05, ‐2.44] |
| 3.5.3 Pain at long term (12 months) using complete‐case data | 3 | 496 | Mean Difference (IV, Random, 95% CI) | ‐8.65 [‐18.11, 0.81] |
| 3.6 Pain sensitivity analyses (change values) | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.6.1 Pain at short term (4–6 weeks) using change scores | 2 | 133 | Mean Difference (IV, Random, 95% CI) | ‐7.67 [‐11.40, ‐3.93] |
| 3.6.2 Pain at short–intermediate term (3–4 months) using change scores | 6 | 717 | Mean Difference (IV, Random, 95% CI) | ‐4.58 [‐7.51, ‐1.66] |
| 3.6.3 Pain at intermediate term (6 months) using change scores | 3 | 472 | Mean Difference (IV, Random, 95% CI) | ‐6.36 [‐12.40, ‐0.33] |
| 3.6.4 Pain at long term (12 months) using change scores | 2 | 363 | Mean Difference (IV, Random, 95% CI) | ‐5.30 [‐15.49, 4.89] |
| 3.7 Pain sensitivity analyses (standardized mean difference) | 12 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.7.1 Pain at short term (4–6 weeks) | 5 | 258 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐1.30, ‐0.29] |
| 3.7.2 Pain at short–intermediate term (3–4 months) | 9 | 946 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.40, ‐0.14] |
| 3.7.3 Pain at intermediate term (6 months) | 9 | 940 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.44, ‐0.11] |
| 3.7.4 Pain at long term (12 months) | 3 | 521 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.61, ‐0.05] |
Comparison 4. Sensitivity analyses for yoga versus exercise.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Back‐specific functional status sensitivity analyses (higher‐quality studies) | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1.1 Back‐specific function at short term (6 weeks) limited to higher‐quality studies | 2 | 248 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.41, 0.37] |
| 4.1.2 Back‐specific function at short–intermediate term (3 months) limited to higher‐quality studies | 2 | 249 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.65, 0.20] |
| 4.1.3 Back‐specific function at intermediate term (6 months) limited to higher‐quality studies | 2 | 249 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.59, 0.19] |
| 4.2 Back‐specific functional status sensitivity analyses (complete case) | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.2.1 Back‐specific function at short term (6 weeks) using complete‐case data | 4 | 349 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.35, 0.29] |
| 4.2.2 Back‐specific function at short–intermediate term (3 months) using complete‐case data | 4 | 519 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.35, 0.19] |
| 4.2.3 Back‐specific function at intermediate term (6 months) using complete‐case data | 3 | 313 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.42, 0.22] |
| 4.3 Back‐specific functional status sensitivity analyses (change values) | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.3.1 Back‐specific function at short term (6 weeks) using change scores | 1 | 77 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.22, 0.67] |
| 4.3.2 Back‐specific function at short–intermediate term (3 months) using change scores | 1 | 256 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.30, 0.19] |
| 4.4 Pain sensitivity analyses (complete case) | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.4.1 Pain at short term (4–6 weeks) using complete‐case data | 3 | 174 | Mean Difference (IV, Random, 95% CI) | ‐13.69 [‐17.75, ‐9.62] |
| 4.4.2 Pain at short–intermediate term (3–4 months) using complete‐case data | 2 | 291 | Mean Difference (IV, Random, 95% CI) | 3.11 [‐1.65, 7.88] |
| 4.5 Pain sensitivity analyses (change values) | 2 | 333 | Mean Difference (IV, Fixed, 95% CI) | 3.30 [‐1.32, 7.92] |
| 4.5.1 Pain at short term (6 weeks) using change scores | 1 | 77 | Mean Difference (IV, Fixed, 95% CI) | ‐5.10 [‐14.48, 4.28] |
| 4.5.2 Pain at short–intermediate term (3–4 months) using change scores | 1 | 256 | Mean Difference (IV, Fixed, 95% CI) | 6.00 [0.69, 11.31] |
| 4.6 Pain sensitivity analyses (standardized mean difference) | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.6.1 Pain at short term (4–6 weeks) | 3 | 201 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.54, ‐0.04] |
| 4.6.2 Pain at short–intermediate term (3 months) | 2 | 326 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.10, 0.34] |
| 4.6.3 Pain at intermediate term (6 months) | 3 | 331 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐1.70, 0.43] |
| 4.6.4 Pain at long term (12 months) | 1 | 199 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.16, 0.39] |
| 4.6.5 Pain at short term (1 week) – intensive intervention | 1 | 80 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐1.20, ‐0.29] |
4.6. Analysis.

Comparison 4: Sensitivity analyses for yoga versus exercise, Outcome 6: Pain sensitivity analyses (standardized mean difference)
Comparison 5. Yoga versus exercise.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Back‐specific functional status | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1.1 Back‐specific function at short term (6 weeks) | 4 | 395 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.32, 0.23] |
| 5.1.2 Back‐specific function at short–intermediate term (3 months) | 4 | 575 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.28, 0.13] |
| 5.1.3 Back‐specific function at intermediate term (6 months) | 3 | 333 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.40, 0.23] |
| 5.1.4 Back‐specific function at long term (12 months) | 1 | 200 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.29, 0.26] |
| 5.1.5 Back‐specific function at short term (1 week) – intensive intervention | 1 | 80 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.25 [‐1.73, ‐0.77] |
| 5.2 Pain | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.2.1 Pain at short term (4–6 weeks) | 3 | 201 | Mean Difference (IV, Random, 95% CI) | ‐12.47 [‐18.28, ‐6.66] |
| 5.2.2 Pain at short–intermediate term (3 months) | 2 | 326 | Mean Difference (IV, Random, 95% CI) | 2.68 [‐2.01, 7.36] |
| 5.2.3 Pain at intermediate term (6 months) | 3 | 331 | Mean Difference (IV, Random, 95% CI) | ‐6.41 [‐21.66, 8.83] |
| 5.2.4 Pain at long term (12 months) | 1 | 199 | Mean Difference (IV, Random, 95% CI) | 3.00 [‐4.25, 10.25] |
| 5.2.5 Pain at short term (1 week) – intensive intervention | 1 | 80 | Mean Difference (IV, Random, 95% CI) | ‐14.50 [‐22.92, ‐6.08] |
| 5.3 Clinical improvement | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.3.1 Clinical improvement at short term (6 weeks) | 2 | 207 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.74, 1.37] |
| 5.3.2 Clinical improvement at short–intermediate term (3 months) | 3 | 433 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.72, 1.31] |
| 5.3.3 Clinical improvement at intermediate term (6 months) | 1 | 163 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.73, 1.33] |
| 5.4 Physical quality of life | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.4.1 Physical quality of life at short term (4–6 weeks) | 3 | 219 | Std. Mean Difference (IV, Random, 95% CI) | 1.03 [0.36, 1.71] |
| 5.4.2 Physical quality of life at short–intermediate term (3 months) | 1 | 237 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.11, 0.40] |
| 5.4.3 Physical quality of life at intermediate term (7 months) | 1 | 54 | Std. Mean Difference (IV, Random, 95% CI) | 1.34 [0.75, 1.94] |
| 5.4.4 Physical quality of life at short term (1 week) – intensive intervention | 1 | 80 | Std. Mean Difference (IV, Random, 95% CI) | 1.06 [0.59, 1.53] |
| 5.5 Mental quality of life | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.5.1 Mental quality of life at short term (4–6 weeks) | 3 | 219 | Std. Mean Difference (IV, Random, 95% CI) | 1.03 [‐0.44, 2.51] |
| 5.5.2 Mental quality of life at short–intermediate term (3 months) | 1 | 237 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.10, 0.41] |
| 5.5.3 Mental quality of life at intermediate term (7 months) | 1 | 54 | Std. Mean Difference (IV, Random, 95% CI) | 1.33 [0.74, 1.92] |
| 5.5.4 Mental quality of life at short term (1 week) – intensive intervention | 1 | 80 | Std. Mean Difference (IV, Random, 95% CI) | 0.87 [0.41, 1.33] |
| 5.6 Adverse events | 5 | 640 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.56, 1.53] |
| 5.7 Measures of work disability | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.7.1 Sickness absenteeism at short term (6 weeks) | 1 | 80 | Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐4.64, 2.84] |
| 5.7.2 Sickness absenteeism at intermediate term (6 months) | 1 | 84 | Mean Difference (IV, Random, 95% CI) | ‐2.40 [‐6.00, 1.20] |
| 5.7.3 Sickness absenteeism at long term (12 months) | 1 | 82 | Mean Difference (IV, Random, 95% CI) | ‐5.90 [‐13.38, 1.58] |
Comparison 6. Yoga versus qigong.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Back‐specific functional status | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1.1 Back‐specific function at short–intermediate term (3 months) | 1 | 111 | Mean Difference (IV, Random, 95% CI) | ‐3.05 [‐7.84, 1.74] |
| 6.1.2 Back‐specific function at intermediate term (6 months) | 1 | 107 | Mean Difference (IV, Random, 95% CI) | ‐2.68 [‐7.58, 2.22] |
| 6.2 Pain | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.2.1 Pain at short–intermediate term (3 months) | 1 | 111 | Mean Difference (IV, Random, 95% CI) | 1.48 [‐5.91, 8.87] |
| 6.2.2 Pain at intermediate term (6 months) | 1 | 107 | Mean Difference (IV, Random, 95% CI) | 7.91 [0.00, 15.82] |
| 6.3 Physical quality of life | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.3.1 Physical quality of life at short–intermediate term (3 months) | 1 | 111 | Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐3.71, 2.17] |
| 6.3.2 Physical quality of life at intermediate term (6 months) | 1 | 107 | Mean Difference (IV, Random, 95% CI) | ‐3.60 [‐6.65, ‐0.55] |
| 6.4 Mental quality of life | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.4.1 Mental quality of life at short–intermediate term (3 months) | 1 | 111 | Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐4.15, 3.47] |
| 6.4.2 Mental quality of life at intermediate term (6 months) | 1 | 107 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐3.82, 3.78] |
| 6.5 Depression | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.5.1 Depression at short–intermediate term (3 months) | 1 | 111 | Mean Difference (IV, Random, 95% CI) | ‐0.65 [‐1.58, 0.28] |
| 6.5.2 Mental quality of life at intermediate term (6 months) | 1 | 107 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.09, 0.49] |
Comparison 7. Sensitivity analyses for yoga versus qigong.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Pain sensitivity analysis (standardized mean difference) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1.1 Pain at short–intermediate term (3 months) | 1 | 111 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.30, 0.45] |
| 7.1.2 Pain at intermediate term (6 months) | 1 | 107 | Std. Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.01, 0.76] |
7.1. Analysis.

Comparison 7: Sensitivity analyses for yoga versus qigong, Outcome 1: Pain sensitivity analysis (standardized mean difference)
Comparison 8. Yoga plus exercise versus exercise alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Back‐specific functional status at short–intermediate term (10 weeks) | 1 | 24 | Mean Difference (IV, Random, 95% CI) | ‐3.68 [‐8.44, 1.08] |
| 8.2 Pain at short–intermediate term (10 weeks) | 1 | 24 | Mean Difference (IV, Random, 95% CI) | ‐3.20 [‐13.76, 7.36] |
Comparison 9. Sensitivity analyses for yoga plus an intervention versus that intervention alone: yoga plus exercise compared to exercise alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 Pain sensitivity analysis (standardized mean difference) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1.1 Pain at short–intermediate term (10 weeks) | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐1.04, 0.57] |
9.1. Analysis.

Comparison 9: Sensitivity analyses for yoga plus an intervention versus that intervention alone: yoga plus exercise compared to exercise alone, Outcome 1: Pain sensitivity analysis (standardized mean difference)
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bramberg 2017.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 159 participants with non‐disabling non‐specific LBP, with or without neck pain, of whom > 90% had chronic non‐specific LBP. Settings: university/medical school. Yoga classes held at a yoga studio. Country: Sweden. Recruitment: April to September 2010, 8 participants recruited from occupational health service units in Stockholm County, Sweden, in accordance with the original plan. However, due to the low influx of people with back and neck pain from the occupational health service, 302 participants were thereafter recruited by advertising in local media. Inclusion criteria: presence of non‐disabling, non‐specific LBP, with or without neck pain, and score ≥ 90 points on the Örebro Musculoskeletal Pain Screening Questionnaire (non‐disabling defined from the perspective of work disability). People were not on sick leave or on sick leave for < 8 weeks; aged 18–60 years and proficient in Swedish. Exclusion criteria: spinal pathology (e.g. tumors or spinal fractures), continuous ongoing sick listing ≥ 8 weeks, comorbidities that could affect the ability to fully participate in the study (e.g. physical disability, psychosis), existing weekly yoga practice or strength training and verified pregnancy. |
|
| Interventions |
Yoga group: (n = 52) 2 × 60‐min standardized kundalini yoga group classes per week for 6 weeks, followed by encouragement to continue home practice at least twice per week for 12 months. Home practice: participants received a CD with instructions and written information, including drawings of each posture. At end of intervention, i.e. after 6 weeks, participants were encouraged to continue practicing yoga programs at least twice a week. Strength training: (n = 52) 5 × 60‐min supervised strength‐training sessions over 6 weeks, followed by encouragement to continue home practice. Home practice: of strength training program ≥ 2 times per week guided by written material and a follow‐up telephone call from physiotherapist 8 weeks after intervention. Advice: (n = 59) control group received a booklet (The Back Book) that contained evidence‐based advice on back pain, and a verbal recommendation to remain active. Common interventions: a minimal intervention comprising self‐care advice was given to all participants. Co‐interventions: no mention of included or excluded co‐interventions. Duration and follow‐up: interventions were provided for 6 weeks and follow‐up ended at 12 months. |
|
| Outcomes | Back‐specific disability subscale of the Swedish version of the Chronic Pain Grade Scale, calculated as the mean intensity and transformed into 0–100, reported at 6 months. Back pain subscale of the Swedish version of the Chronic Pain Grade Scale, calculated as the mean intensity and transformed into 0–100, reported at 6 months. Sickness absenteeism, reported as the mean number of days in past month that participants were absent from work due to illness. Other outcomes collected: sickness presenteeism, process outcomes (number of times exercised per week). |
|
| Notes | Adverse events: no discussion of safety or adverse events. Measurement of expectations or treatment preferences at baseline: none. Unpublished data: none. Funding: non‐profit. Funded by Swedish Research Council for Health, Working life and Welfare (2008‐0849). Clinical trials registration: NCT01653782. Note: LSW contacted the primary author in October 2019 to check the number of participants at each time point in Table 5 and received information by e‐mail on 5 November 2019. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The study used a block randomization design. A random allocation sequence was generated by the statistician (JH)." |
| Allocation concealment (selection bias) | Low risk | Quote: "For each participant an opaque envelope was opened, in consecutive order, by an external research assistant not involved in the inclusion process." |
| Blinding of participants | High risk | Quote: "The participants did not know the content of the different intervention arms." Comment: although the participants did not initially know the content of the intervention groups, they were aware of their intervention after they were allocated to groups. |
| Blinding of personnel/providers | High risk | Quote: "The yoga leader and physiotherapist were not blinded." |
| Blinding of outcome assessors | High risk | Quote: "The research group assessing the study's outcome was blinded during the data collection and data analysis." Comment: although the researchers collecting the data may have been blinded, the participants reporting their subjective states were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Forty participants were lost to follow‐up, i.e. those who discontinued and the non‐responders (yoga 6 (11.5%); strength training 16 (30.7%); CG 18 (32.7%)) at the 12‐month follow‐up. The yoga group had a statistically significantly lower loss to follow‐up than the strength training and CG (Fisher's exact test = 0.017). Sixty percent of those lost to follow‐up were women, mean age was 42.0 years (SD 11.3), mean neck pain intensity was 45.0 (SD 25.3) and mean back pain intensity was 61.6 (SD 14.8). However, there were no significant differences between those who were lost to follow‐up and participants in terms of age, sex, or pre‐intervention values on neck and back pain." Comment: at all follow‐up points, participants were not followed up if they were not responders (Figure 1). |
| Selective reporting (reporting bias) | Unclear risk | Comment: primary outcome of sickness absence was described in ClinicalTrials.gov but the secondary outcomes of back and neck pain and disability were not mentioned in the trial registration. However, these are reasonable outcomes to measure for the condition and there is no positive evidence of selective reporting. |
| Group similarity at baseline | Low risk | Comment: groups appeared similar on all important factors. |
| Co‐interventions | Unclear risk | Comment: it does not appear that any co‐interventions were planned or prohibited and there is no reporting on co‐interventions used by participants, other than the minimal intervention of self‐care advice, which was given to all participants (page 3). There is no mention of medication or other treatments received among participants at baseline. |
| Compliance | Unclear risk | Quote: "The proportion of participants who adhered to the recommendations (exercised at least 2 times/week) during the 6 month follow‐up was: 54% (yoga), 34% (strength training) and 42% (CG)." Comment: 54% attended yoga but attendance rates for strength training was 34% and for non‐exercise control group was 42%. |
| ITT analysis | Low risk | Quote: "An intention‐to‐treat analysis was conducted which included all randomized individuals, irrespective of whether they had adhered to the intervention programme or not. Two conservative imputation analyses were performed on the primary outcome sickness absenteeism. In the first analysis, we used the relative frequencies of zeros and ones in each group to randomly generate zeroes and ones for the drop‐outs. In the second analysis we used "Last value carried forward." Both analyses generated similar results (data not presented) to those presented in the results section." |
| Timing of outcome assessments | Low risk | Comment: outcomes assessed at 6, 24, and 52 weeks for all groups (page 6). |
| Other bias | Low risk | No other biases identified. |
Cox 2010.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 20 participants with LBP. Settings: 1 primary care practice. Location of yoga intervention delivery not described. Country: UK. Recruitment: GP records from a single practice. Inclusion criteria: men and women aged 18–65 years, visiting GP in the previous 18 months for LBP, score ≥ 4 on the RMDQ scale, available to attend yoga classes, possess sufficient physical mobility to participate in the intervention. Exclusion criteria: pregnancy, psychosis or recent substance abuse, already participating in yoga, already in a trial for LBP, not currently experiencing an episode of LBP, previous spinal surgery, or clinical indications of serious spinal or neurologic pathology. |
|
| Interventions |
Yoga group: (n = 10) 12 weekly 75‐min iyengar yoga classes including relaxation and pain‐relieving postures, and poses to improve posture, flexibility, strength, and mobility. Each class had a primary theme (e.g. Sukha – relaxation and comfort). Home practice: participants given a yoga manual and yoga mat, weekly practice handouts and encouraged to practice yoga at home, as well as taught to have better awareness of posture, movement, and correct breathing. Frequency and duration of suggested home practice not described. The Back Book group: (n = 10) control group received a booklet with advice on how to manage LBP (The Back Book. London: The Stationery Office; 2007) and continued their usual care. Common interventions: both the Back Book and the Yoga group received the booklet and usual care. Co‐interventions: no mention of included or excluded co‐interventions. Duration and follow‐up: interventions were provided for 12 weeks and follow‐up ended directly after the end of the intervention. |
|
| Outcomes | Back‐specific function (RMDQ) at 4 and 12 weeks. Back pain (Aberdeen Back Pain Scale) at 4 and 12 weeks. Quality of life – mental (SF−12 Mental Component score) at 4 and 12 weeks. Quality of life – physical (SF‐12 Physical Component score) at 4 and 12 weeks. Clinical improvement (number of participants reporting no LBP) at 4 and 12 weeks. Other outcomes collected: EQ‐5D health index, Pain Self‐Efficacy Questionnaire, number of days spent in bed due to LBP, number of days with restricted activity attributed to LBP, and whether medication was used for LBP over the previous 4 weeks. |
|
| Notes | Adverse events: no discussion of safety or adverse events. Measurement of expectations or treatment preferences at baseline: none. Unpublished data: Dr Holger Cramer sent LSW standard deviations for the change values, data previously obtained from Dr Helen Tilbrook, on 26 November. Dr Catherine Hewitt sent endpoint data to LSW on 9 March 2016. Funding: York Trials Unit, Department of Health Sciences, University of York. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used computer‐generated random numbers to randomize participants. |
| Allocation concealment (selection bias) | Low risk | Randomization carried out by an independent data manager. |
| Blinding of participants | High risk | No blinding as compared with usual care alone; outcomes based on self‐assessment. |
| Blinding of personnel/providers | High risk | No blinding of personnel/providers. |
| Blinding of outcome assessors | High risk | Self‐reported outcomes were collected by mail from the participants, who were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition > 30% in yoga group and it was unclear how missing data were managed. |
| Selective reporting (reporting bias) | High risk | Outcome mentioned in methods was not reported in results (days spent in bed). No protocol available. |
| Group similarity at baseline | High risk | Usual care group were older and had longer duration of back pain. |
| Co‐interventions | Unclear risk | Not possible to assess; usual care not defined. |
| Compliance | High risk | Quote: "Of the ten patients allocated to receive yoga, five (50%) did not attend any one session. … Two patients attended two sessions, two patients attended four sessions and one patient attended five sessions." |
| ITT analysis | Low risk | Authors state ITT analysis was done. |
| Timing of outcome assessments | Low risk | Outcome assessment at set points. |
| Other bias | Low risk | No other biases identified. |
Demirel 2019.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 80 participants with chronic non‐specific LBP. Settings: physiotherapy practice by trialists affiliated with physiotherapy department of a university. Location of yoga intervention delivery not described. Country: Turkey. Recruitment: participants had attended a physiotherapy practice. Further details not reported. Inclusion criteria: diagnosis of chronic non‐specific LBP (pain at lumbar region that was not related to specific pathology and had been ongoing for ≥ 3 months), aged 20–65 years. Exclusion criteria: structural scoliosis; neurologic, metastatic, or metabolic diseases; or had undergone spinal surgery. |
|
| Interventions |
Yoga group: (n = 40) 3 × 60‐min group classes per week for 6 weeks. Classes consisted of instruction in yoga philosophy, asanas, and diaphragmatic breathing. Home practice: none mentioned. Stabilization exercise group: (n = 40) 3 × 60‐min group lessons per week for 6 weeks. Lessons consisted of instruction in contraction of core muscles and diaphragmatic respiration. Home practice: none mentioned. Common interventions: none described. Co‐interventions: no mention of included or excluded co‐interventions. Duration and follow‐up: interventions were provided for 6 weeks and follow‐up ended directly after end of intervention. |
|
| Outcomes | Back‐specific function (Turkish version of the Oswestry Disability Index) at 6 weeks. Back pain (10‐cm VAS scale for pain during activity) at 6 weeks. Quality of life – mental (emotional reactions subscale of the Turkish version of the Nottingham Health Profile) at 6 weeks. Quality of life – physical (physical activity subscale of the Turkish version of the Nottingham Health Profile) at 6 weeks. Other outcomes collected: VAS scale for pain at rest, VAS scale for pain at night, back pain‐related physical performance on the Back Performance Scale. |
|
| Notes | Adverse events: no discussion of safety or adverse events. Measurement of expectations or treatment preferences at baseline: none. Unpublished data: none. Funding: none. Quote: "This research did not receive any specific grant from funding agencies in the public, commercial, or not‐for‐profit sectors." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Eligible patients were allocated randomly into two groups: a yoga group (YG) and a stabilization group (SG) by using a sealed envelope method at a ratio of 1:1." Comment: no information on how sequence was generated – implied that a statistician was involved. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Eligible patients were allocated randomly into two groups: a yoga group (YG) and a stabilization group (SG) by using a sealed envelope method at a ratio of 1:1." Comment: 'sealed envelope method' described under randomization but no further information about the process. |
| Blinding of participants | High risk | Comment: report stated participants were blinded. Unclear how the participants could be unaware of the intervention they were receiving, even if they were not aware of the details of the comparison intervention. |
| Blinding of personnel/providers | High risk | Personnel delivering the interventions could not be blinded. |
| Blinding of outcome assessors | High risk | Quote: "The statistician and patients were blinded, but the study was not double blinded since the outcome assessor already knew about the groups." Comment: although the participants were claimed to be blinded, their self‐reports were collected by an outcome assessor who was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: small percentage of participants lost to follow‐up. All losses were from 1 group (exercise) and unclear whether this was related to the intervention or outcomes. |
| Selective reporting (reporting bias) | Unclear risk | Comment: outcomes in the methods and results sections corresponded; however, there was no protocol or trial registration. |
| Group similarity at baseline | High risk | Quote: "All participants had similar data in terms of age, sex, and body mass index (p > 0.05, Table 4). Pain intensity during activity, back‐pain‐related disability, and the pain sub‐scale of NHP [Nottingham Health Profile] were higher in SG [stabilization group] at baseline." Comment: multiple outcomes higher in exercise group at baseline. |
| Co‐interventions | Unclear risk | Comment: no mention of co‐interventions. |
| Compliance | Unclear risk | Comment: no mention of compliance. |
| ITT analysis | Unclear risk | Comment: there was no evidence that an ITT analysis was not performed; however, it was not mentioned explicitly and there was no sensitivity analysis for the missing data. |
| Timing of outcome assessments | Low risk | Comment: both groups were assessed before treatment and after treatment. |
| Other bias | Low risk | No other biases identified. |
Galantino 2004.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 22 participants with chronic LBP. Settings: setting for trial and location of yoga intervention delivery not described. Country: USA. Recruitment: self‐referral through newspaper advertisements and referral through healthcare practitioners. Inclusion criteria: men and women aged 30–65 years with back pain for > 6 months and > 2 previous conservative medical interventions (physical therapy and chiropractic) without prolonged relief. Exclusion criteria: current history of chronic systemic disease, previous yoga experience, changes in pain medication during past 14 days. |
|
| Interventions |
Yoga group: (n = 11) formal 1‐hour hatha yoga class twice per week for 6 weeks. Home practice: suggested 1 hour per day but not mandated or monitored. Control group: (n = 11) no treatment during observation period. Common interventions: usual care continued for both groups. Co‐interventions: changes in pain medication were not allowed during study. Duration and follow‐up: interventions provided for 6 weeks and there was an additional follow‐up at 3 months for yoga participants only. |
|
| Outcomes | Back‐specific function (Oswestry Disability Index) at 6 weeks. Depression (Beck Depression Inventory) at 6 weeks. Other outcomes collected: Sit and Reach Test and Functional Reach Test. |
|
| Notes | Adverse events: no discussion of safety or adverse events. Measurement of expectations or treatment preferences at baseline: none. Funding: not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used random numbers to generate sequence. |
| Allocation concealment (selection bias) | Unclear risk | No details reported in publication. |
| Blinding of participants | High risk | No blinding as control participants received no treatment; outcomes based on self‐assessment. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | Participants were not blinded, and outcomes were self‐reported. No mention of blinding of those who collected the information on outcomes from the participants. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition > 30% in control group. 6/11 control group participants had missing outcomes and were treated as 'failures' in a dichotomous analysis. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Group similarity at baseline | High risk | Beck Depression Inventory substantially higher in control group. |
| Co‐interventions | Unclear risk | Not possible to assess; recorded by participants but not reported. |
| Compliance | Unclear risk | No information on class attendance. |
| ITT analysis | Low risk | ITT analysis stated. |
| Timing of outcome assessments | Low risk | Outcome assessments at a set point. |
| Other bias | Low risk | No other biases identified. |
Groessl 2017.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 152 veterans with chronic LBP persisting > 6 months. Settings: veterans' medical center. Location of yoga classes not described. Country: USA. Recruitment: via referral by VA clinicians. Study staff notified care providers about study recruitment via e‐mail, brief presentations, and word of mouth. Primary care, physical medicine, pain medicine, and psychology were main clinics targeted for recruitment. In addition, flyers posted in common areas and waiting rooms at medical center. VA patients receiving study information from providers or from flyers contacted study personnel to learn about study enrollment criteria. Those interested were scheduled for a screening exam. Inclusion criteria: VA patients, aged ≥ 18 years, chronic LBP diagnosis ≥ 6 months, English literacy, no new pain treatments in last month, willing to attend yoga or be assigned to delayed treatment, willing to attend 4 assessments, and willing to remain on present pain treatments. Exclusion criteria: recent back surgery (in last 12 months), back pain from systemic conditions, morbid obesity, acute sciatica/nerve compression, chronic lumbar radicular pain, serious unstable coexisting medical or psychiatric conditions, potential metastatic disease, positive Romberg test, or practiced yoga more than once in last year. |
|
| Interventions |
Yoga group: (n = 76) 12 weeks of twice‐weekly 60‐min yoga classes. Home practice: participants received a home practice manual recommending 15–20 min of yoga home practice on days that instructor‐led sessions were not held. Delayed treatment group: (n = 76) usual care and no yoga practice until end of – month assessment. Common interventions: none described other than continued usual care. Co‐interventions: no mention of included or excluded co‐interventions. Duration and follow‐up: interventions provided for 12 weeks and follow‐up ended at 6 months. |
|
| Outcomes | Back‐specific function (RMDQ) at 6 weeks, 12 weeks, and 6 months. Pain (short version of the Brief Pain Inventory) at 6 weeks, 12 weeks, and 6 months. Other outcomes collected: medication use, process outcomes (class attendance and home practice), and additional outcomes recorded in protocol but not included in current publications (pain intensity, pain interference, depression, anxiety, fatigue/energy, quality of life, self‐efficacy, sleep quality, and medication usage). |
|
| Notes | Adverse events: no serious adverse events reported during 6‐month follow‐up. 2 adverse events identified. 1 participant reported increased levels of back pain after 1 session and declined to attend further. 1 participant attended 7 consecutive yoga sessions and stopped attending because his "back went out." Neither participant directly attributed the event to yoga practice. Measurement of expectations or treatment preferences at baseline: none. Funding: government. Veteran Affairs Rehabilitation Research and Development (Grant #RX000474). Note: LSW e‐mailed the first author in September 2019 and obtained unadjusted endpoint values to use in primary analyses. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "After the baseline assessment was complete, the study coordinator used a secure, web‐based data management system to randomly assign participants to one of two groups (yoga or DT [delayed treatment]). Participants were notified of group assignment the following day. The binary non‐stratified randomization sequence was computer generated, at a 1:1 allocation ratio in blocks of 10 participants to facilitate balanced group assignment." |
| Allocation concealment (selection bias) | Unclear risk | Comment: likely that allocation concealment was used because randomization was carried out by computer; however, who notified the participants and other aspects of the allocation process not specified. |
| Blinding of participants | High risk | No blinding. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | Quote: "Assessors were initially blinded to group assignment and did not have access to group assignment data. Prior to assessments, the study coordinator asked participants to not discuss their group assignment or experiences with any study staff at the assessments." Comment: although efforts were made to blind the assessors to group assignment, the outcomes relied upon self‐reports of the participants, and the participants were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Attrition from follow‐up assessment periods was 20% attrition at the 6‐ and 12‐week assessments and 27.3% attrition at the 6‐month assessment. Attrition rates were not significantly different between groups at any time point. (p 0.31–0.99). No differences were found on any baseline characteristics between attriters for each group, suggesting data was missing at random." Comment: attrition was balanced between groups and was not associated with baseline characteristics; however, it was relatively high (> 20%) in both groups and simple LOCF was used for imputation. Reasons given for attrition from yoga group, but unclear reasons for attrition from wait list group. |
| Selective reporting (reporting bias) | Unclear risk | Comment: primary outcome was change in back pain‐related disability measured using RMDQ at baseline and 12 weeks. Secondary outcomes included pain intensity, pain interference, depression, anxiety, fatigue/energy, quality of life, self‐efficacy, sleep quality, and medication usage (from abstract of methods paper). Several other outcomes from the methods paper were not mentioned, although it is possible they will be included in additional publications. |
| Group similarity at baseline | Low risk | Comment: more yoga participants (48%) than waiting group participants (31%) had previously practiced yoga (P = 0.45); however, observation of this 1 difference was consistent with randomization of a relatively small sample size. Other prognostic factors were balanced between groups. |
| Co‐interventions | Low risk | Quote: "All participants continued to receive usual care. To avoid confounding effects, all participants were asked to refrain from changing treatments for their cLBP [chronic LBP] during the study period unless medically necessary (provider determined). DT [delayed treatment] during this time period varied, but most commonly consisted of prescription and nonprescription pain medications, physical therapy, spinal manipulation, exercise, and various other self‐help treatments." Quote: "Compliance with these instructions was assessed at each time point." |
| Compliance | Low risk | Quote: "The median number of instructor‐led sessions attended by subjects randomized to yoga was 14 of 24 classes (58%; mean 12.3 classes)." |
| ITT analysis | Low risk | Quote: "An "intent‐to‐treat" "approach was followed for all study outcomes and all analyses were conducted using statistical software R, version 3.3.0 in 2016." |
| Timing of outcome assessments | Low risk | Comment: although the participants were recruited and treated in sequential cohorts over 2 years, there was no indication of differential timing of outcome assessment for the randomized groups. |
| Other bias | Low risk | No other biases identified. |
Highland 2018.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 68 current or former US military service members with chronic non‐specific LBP. Settings: military medical center (Walter Reed National Military Medical Center). Location of yoga classes not described. Country: USA. Recruitment: from Walter Reed National Military Medical Center from 9 December 2013 to 22 January 2015 via healthcare provider referral or self‐referral. Inclusion criteria: eligible for Department of Defense health care, had an LBP diagnosis documented within the electronic health record, endorse a Defense & Veterans Pain Rating Scale 2.0 score of 4 for > 3 months, aged 18–68 years, and able to read/understand English. Exclusion criteria: medically advised against mild/moderate exercise; unable to sit on floor for 2 min or stand independently; had complex regional pain syndrome, fibromyalgia, chronic fatigue syndrome, autoimmune disease‐related pain, other chronic medical conditions (i.e. advanced diabetic neuropathies), or history of severe traumatic brain injury; practiced yoga within past 6 months; scheduled for back surgery in following 3 months; had back surgery within past year; pregnant; or undergoing a Medical Evaluation Board assessment to determine discharge. |
|
| Interventions |
Yoga group: (n = 34) 2 × 60‐min individual yoga sessions per week in weeks 1–4 and then weekly sessions in weeks 5–8. Home practice: participants received an audio CD with instructions for optional home practice. Usual care treatment group: (n = 34) usual care that was specific to the participant and included a range of therapies. Common interventions: none described other than usual care. Co‐interventions: no mention of included or excluded co‐interventions. Duration and follow‐up: interventions were provided for 8 weeks and follow‐up ended at 6 months. |
|
| Outcomes | Back‐specific function (RMDQ) at 4, 8, and 12 weeks, and 6 months. Pain (Defense & Veterans Pain Rating Scale) at 4, 8, and 12 weeks, and 6 months. Quality of life – mental (Symptom Burden composite from the Sleep Disturbance, Pain Interference, Anxiety, Depression, and Fatigue subscales of PROMIS‐29 (higher burden is worse mental quality of life) at 4, 8, and 12 weeks, and 6 months. Quality of life – physical (PROMIS‐29) at 4, 8 and 12 weeks, and 6 months. Other outcomes collected: process outcomes (sessions completed for active intervention group). |
|
| Notes | Adverse events: mentioned as monitored and in the discussion section reported that there was a lack of adverse events or side effects. Measurement of expectations or treatment preferences at baseline: none. Funding: government. Quote: "Supported by the U.S. Department of the Army, Telemedicine and Advanced Technology Research Center, U.S. Army Medical and Materiel Command, and Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc. under Cooperative Agreement (W81XWH‐11‐2‐0201)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computerized random number generator produced the randomization table." |
| Allocation concealment (selection bias) | Low risk | Quote: "Participants opened presealed envelopes labeled with the sequential enrollment number containing group assignment." |
| Blinding of participants | High risk | Not blinded. |
| Blinding of personnel/providers | High risk | Not blinded. |
| Blinding of outcome assessors | High risk | Comment: participants could not be blinded and outcomes based on self‐report. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: attrition different (although low) in 2 groups and reasons not given. |
| Selective reporting (reporting bias) | Low risk | Comment: clinical trial registration listed pain scores – DVPRS 2.0 (weekly for 6 weeks) as primary outcome and this was consistent with report. Secondary outcome of RMDQ was also included in registration. The additional outcome measurements for the primary outcome at 3‐ and 6‐months do not seem unreasonable. |
| Group similarity at baseline | Low risk | Quote: "At baseline, treatment groups did not differ significantly in sex …, military status …, age …, past 24‐hour pain …, radiating back pain …, bilateral back pain …; PZ.61), or constant back pain …, leg/foot weakness …, disability …, or symptom burden … Therefore, sex and pain laterality were considered for inclusion in GLMMs [generalized linear mixed model] if they improved model fit." |
| Co‐interventions | Unclear risk | Quote: "Treatment as usual was specific to the participant on the basis of his or her provider's treatment planning and recommendations. This may include pain medications, physical therapy, chiropractic care, injections, acupuncture, massage, supplements, or other therapies." Comment: no mention of co‐interventions in yoga group or reporting of any monitoring of changes. |
| Compliance | Low risk | Quote: "Lastly, 38% of RESTORE [yoga] participants completed all 12 yoga sessions and 47% completed 9 to 11 sessions, with only 14% completing <9 sessions (Fig 1)." |
| ITT analysis | Low risk | Quote: "To compare treatment group effectiveness, an intention‐to‐treat approach using generalized linear mixed models (GLMMs) examined longitudinal patterns in the primary (past 24‐hour pain) and then secondary (disability, physical functioning, symptom burden) outcomes from baseline through 6‐month follow‐up." |
| Timing of outcome assessments | Low risk | Quote: "Follow‐up assessments for all participants occurred at the end of week 4 (midtreatment) and week 8 (posttreatment), as well as at week 13 (3‐mo follow‐up) and week 26 (6‐mo follow‐up)." |
| Other bias | Low risk | No other biases identified. |
Jacobs 2004.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 52 participants with chronic non‐specific LBP. Settings: setting for trial and location of yoga intervention delivery not described. Country: USA. Recruitment: self‐referral through flyers and posters in inner‐city primary care clinics and advertisements in newsletters for university and medical employees, and healthcare practitioner referrals from clinic conferences of large inner‐city clinics. Inclusion criteria: men and women aged 18–65 years who had made ≥ 3 visits to a health provider for non‐specific mechanical LBP in the previous 12 months, have had pain symptoms for ≥ 6 months and score ≥ 3 out of 10 on the VAS Pain Scale for pain over past week. Exclusion criteria: back pain secondary to malignancy, infectious disease, inflammatory spondyloarthropathies, vertebral fracture or dislocation, acute radicular syndrome, or severe neurologic signs, systemic or visceral causes of pain, any severe concurrent illness, pregnancy, back‐related compensation or litigation, history of back surgery, regular participation (> 1/week) in iyengar yoga for past 3 months, plans to move out of study region within next 9 months, life expectancy ≤ 9 months. |
|
| Interventions |
Yoga group: (n = 28) 90‐min iyengar yoga classes held twice a week for 12 weeks. Yoga consisted of predefined set of postures from which yoga teacher selected individual poses in varying sequences for each of 23 yoga classes. 28 asanas (postures) selected, including mandatory poses to be practiced daily. Home practice: prescribed for 30 min on 5 days/week. Participants were provided an illustrated pamphlet explaining the poses and a yoga mat, block, belts, and blankets. Waiting list group: (n = 24) group received a "back pain educational booklet" not otherwise specified. Common interventions: usual care continued for both groups. Co‐interventions: no mention of permitted or restricted co‐interventions. Duration and follow‐up: interventions provided for 12 weeks and there was an additional follow‐up at 6 months. |
|
| Outcomes | Back‐specific function (RMDQ) at 3 months (unpublished data). Back‐specific function (Oswestry Disability Index) at 3 months (unpublished data). Pain. Depression (CES – Depression) at 3 months (unpublished data). Quality of life – mental (SF‐36 Emotional Well‐Being) at 3 months (unpublished data). Quality of life – physical (SF‐36 Physical Functioning) at 3 months (unpublished data). Other outcomes collected (unpublished data): bothersomeness of back pain during past 4 weeks, mean LBP over past 4 weeks, worst back pain over last 4 weeks, best back pain over last 4 weeks, insomnia, PANAS‐PA, PANAS‐NA, STAIS, STAIT, SF‐36 Physical Role Limitations, SF‐36 Emotional Role Limitations, SF‐36 Energy/Fatigue, SF‐36 Social Functioning, SF‐36 Pain, SF‐36 General Health, biologic markers, healthcare utilization, drug usage. |
|
| Notes | Adverse events: no discussion of safety or adverse events. Measurement of expectations or treatment preferences at baseline: (quote) "To better ascertain how clinical response is modulated by baseline expectation, we ascertained baseline expectation of improvement from yoga and found no differences between groups [at baseline] (Table 6)." Unpublished data: Dr Michael Acree e‐mailed a spreadsheet of endpoint data for completers to LSW on 27 April 2015. Funding: not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used random number generator. |
| Allocation concealment (selection bias) | Low risk | Allocation by co‐ordinator according to a pre‐established randomization list. |
| Blinding of participants | High risk | No blinding as waiting list control used; outcomes based on self‐assessment. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | Participants were not blinded and self‐reported the outcomes. No mention of blinding of those who collected the information on outcomes from the participants. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Total attrition 16% and only completers analysis done. Reasons for attrition not given although attrition was similar across intervention groups. |
| Selective reporting (reporting bias) | High risk | Outcome data never published. We obtained all retrievable summary data directly from the analysis file by request of the study authors. Some primary and secondary outcomes were mentioned in the study report and not included in the outcome file (e.g. pharmaceutical drug usage for back pain, biologic markers of stress, and healthcare utilization). |
| Group similarity at baseline | Low risk | Matched on most important factors. |
| Co‐interventions | Unclear risk | Not possible to assess. |
| Compliance | Low risk | Quote: "Overall, 64% of participants assigned to receive the immediate yoga intervention attended yoga classes throughout the 3 month intervention period. On average, these participants attended 15 (66%) classes over the 3‐month trial period." |
| ITT analysis | Unclear risk | Details of analysis not reported. |
| Timing of outcome assessments | Low risk | Outcome assessment at set points. |
| Other bias | Low risk | No other biases identified. |
Kuvacic 2018.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 30 participants with chronic LBP. Settings: authors were affiliated with multiple universities and it is unclear which university or universities were the base of the study. Location of yoga classes unclear. Country: Croatia (location of first author) and possibly also Italy or Israel (other author affiliations). Recruitment: not described. Inclusion criteria: pervasive chronic LBP, aged > 18 years, presence of depression and anxiety according to Zung questionnaires. Exclusion criteria: acute LBP (including recent thoracic‐lumbar trauma); specific causes of LBP (lumbar stenosis, disk hernia, spinal deformity, fracture, spondylosis, osteoporosis of the spine); current or pre‐existing neurologic, oncologic, or psychiatric conditions (e.g. dementia, Parkinson disease, congenital central nervous system malformations, multiple sclerosis, tumors, schizophrenia, head trauma); any previous experience in mindfulness, meditation, or yoga practice; people with recent cerebrovascular accidents and myocardial infarctions; obesity. |
|
| Interventions |
Yoga group: (n = 15) 2 × 75‐min yoga sessions per week for 8 weeks. Home practice: not mentioned. Education group: (n = 15) an initial pamphlet with recommendations for posture, movement, and breathing followed by a twice‐weekly newsletter. Common interventions: none described. Co‐interventions: no mention of included or excluded co‐interventions. Duration and follow‐up: interventions provided for 8 weeks and follow‐up finished at end of intervention. |
|
| Outcomes | Back‐specific function (Oswestry Disability Index) at 8 weeks. Pain (numeric rating scale for pain 0–10) at 8 weeks. Depression (Zung self‐rating depression scale) at 8 weeks. Other outcomes collected: Zung self‐rating anxiety scale. |
|
| Notes | Adverse events: no mention of assessment of adverse events. Measurement of expectations or treatment preferences at baseline: none. Funding: not mentioned. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No mention of how sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation procedures. |
| Blinding of participants | High risk | Not blinded. |
| Blinding of personnel/providers | High risk | Not blinded. |
| Blinding of outcome assessors | High risk | Participants not blinded and outcomes based on self‐report. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no mention of whether any participants were lost to follow‐up (or not). However, there appeared to be no attrition. |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol or trial registration. |
| Group similarity at baseline | Unclear risk | Comment: no presentation or discussion of baseline characteristics by group, only for total sample. |
| Co‐interventions | Unclear risk | Comment: no mention of co‐interventions. |
| Compliance | Unclear risk | Comment: no mention of compliance with interventions. |
| ITT analysis | Unclear risk | Comment: no mention of ITT analysis. |
| Timing of outcome assessments | Low risk | Quote: "Participants from both the YG [yoga] and PG [education] received the second questionnaire at the same session (the first meeting), so that they could evaluate pain through the NRS [numerical rating scale] 0–10 scale. The post‐psychological assessment was performed one week after the end of the study through an online version of questionnaires." |
| Other bias | Low risk | No other biases identified. |
Nambi 2014.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 60 participants with chronic non‐specific LBP. Settings: based at outpatient department of a physiotherapy college. Location of yoga intervention delivery appeared to be the outpatient department as no other settings were described. Country: India. Recruitment: self‐referral and healthcare practitioner referral through pamphlets and flyers. Inclusion criteria: men and women aged ≥ 18 years who were ambulatory and had a history of non‐specific LBP persisting for ≥ 3 months. Exclusion criteria: LBP due to nerve root compression, disk prolapse, spinal stenosis, tumor, spinal infection, ankylosing spondylosis, spondylolisthesis, kyphosis or structural scoliosis, or a widespread neurologic disorder; surgical candidacy; back‐related litigation or compensation; cardiopulmonary problems; pregnancy; BMI > 35; major depression; substance abuse; yoga practice. |
|
| Interventions |
Yoga group: (n = 30) weekly 60‐min iyengar yoga classes for 4 weeks. Used a series of 29 postures, including forward bends, twists, and inversions but excluding back bends. Poses progressed from simpler to more challenging over time. Used a range of props including sticks, mats, belts, blocks, chairs, wall ropes, benches, boxes, stools, trestle, and weights. Home practice: requested 30 min, 5 days/week during intervention. Exercise group: (n = 30) participants asked to practice individually prescribed exercises for strengthening and stretching the abdominal or back muscles (or both) for 4 weeks, beginning with 5 repetitions for 3 days/week and increasing to 15 repetitions for 5 days/week. Exercise sessions were preceded by warm‐up exercises consisting of stretching and relaxation. Common interventions: both groups received 1‐hour lecture and handouts on physical therapy for chronic LBP 2 weeks before beginning of intervention. Co‐interventions: exercise group participants were asked not to participate in other exercises for their low back. Duration and follow‐up: interventions provided for 4 weeks and additional follow‐up at 6 months after program completion (7 months after randomization). |
|
| Outcomes | Current pain (10‐cm VAS scale) at 4 weeks and 7 months. Mean days of mental distress in previous 30 days at 4 weeks and 7 months. Mean days of physical distress in previous 30 days at 4 weeks and 7 months. Other outcomes collected: days of mental distress and physical distress dichotomized into frequent (≥ 14 days) and infrequent (< 14 days) distress at 4 weeks and 7 months; days of activity limitations (how many days did poor physical or mental health keep you from doing your usual activities, such as self‐care, work, or recreation?) assessed for previous 30 days at 4 weeks and 6 months and dichotomized into frequent (≥ 14 days) and infrequent (< 14 days) limitations. |
|
| Notes | Adverse events: no specific discussion of overall safety or adverse events. However, it mentioned that 1 person withdrew from the yoga group due to a herniated disk, and 2 people withdrew from yoga group due to fears that yoga would aggravate symptomatic osteoarthritis. Measurement of expectations or treatment preferences at baseline: none. Funding: authors declared no funding. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used random number generating table. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding of participants | High risk | No blinding as control was exercise; outcomes based on self‐assessment. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | Quote: "Data collectors were blind to the subject's treatment status." Comment: however, participants were not blinded and self‐reported all outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Low attrition rates but reasons for withdrawal in yoga group possibly related to outcome. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. |
| Group similarity at baseline | Unclear risk | Limited demographic data reported. |
| Co‐interventions | Unclear risk | Not mentioned in inclusion/exclusion criteria or results. |
| Compliance | Unclear risk | 4 yoga participants did not complete the trial but there was no information about class participation. |
| ITT analysis | Unclear risk | No mention of ITT. |
| Timing of outcome assessments | Low risk | Outcome assessment at set points. |
| Other bias | Low risk | No other biases identified. |
Neyaz 2019.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 70 participants with chronic non‐specific LBP. Settings: Department of Physical Medicine and Rehabilitation and Centre for Integrative Medicine and Research of a tertiary care hospital. Location of yoga intervention delivery: Center for Integrative Medicine and Research. Country: India. Recruitment: outpatient clinics. Inclusion criteria: men and women aged 18–55 years who complained of non‐specific LBP persisting for ≥ 12 weeks and had a pain rating ≥ 4 on a rating scale from 0 (no pain) to 10. Exclusion criteria: back pain due to severe scoliosis, sciatica, previous back surgery, or diagnosed spinal stenosis, potentially attributable to specific underlying diseases or conditions (e.g. pregnancy, meta‐static cancer, spondylolisthesis, fractured bones or dislocated joints, large herniated disk, sciatica pain ≥ back pain) or minimal pain (rating of > 4 on a 0–10 numerical rating scale; conditions overlapping with symptoms of back pain or confound treatment effects (rheumatoid arthritis, spondyloarthropathy, and severe fibromyalgia); currently receiving other back pain treatments or had participated in yoga or conventional therapeutic exercise training for back pain; unstable medical or severe psychiatric conditions or dementia; contraindications (e.g. progressive neurologic deficits) or schedules that precluded class participation; history of active substance or alcohol abuse; unwilling to practice at home; plans to move out of the area in next 1 month. |
|
| Interventions |
Yoga group: (n = 35) weekly 35‐min integrated yoga therapy classes for 6 weeks. Home practice: participants asked to practice for 30 minutes at home on non‐class days and during the 6‐week follow‐up period. Exercise group: (n = 35) weekly 35‐min conventional therapeutic exercise classes for 6 weeks. Home practice: participants asked to practice for 30 minutes at home on non‐class days and during the 6‐week follow‐up period. Common interventions: both groups received education on 'postural care' for chronic non‐specific LBP. Co‐interventions: none mentioned. Duration and follow‐up: interventions provided for 6 weeks and an additional follow‐up at 12 weeks. |
|
| Outcomes | Current pain (0–10 scale) reported on the DVPRS at 6 and 12 weeks. Back‐related function reported on RMDQ at 6 and 12 weeks. Patient‐perceived recovery rated on a 7‐point Likert scale ranging from 'very large improvement' to 'very much worse', at 6 and 12 weeks. Other outcomes collected: weekly consumption of pain medication. |
|
| Notes | We contacted the author in November 2019 for further information on the study data, including means and standard deviations, and were provided the full dataset by e‐mail. We analyzed the data and then extracted it into Covidence and then Review Manager 5. Adverse events: no serious adverse events but 3 participants had minor adverse events mostly related to increased pain. We contacted the author to find out which group or groups the 3 people experiencing adverse events belonged to. He replied that this was 1 in the exercise group and 2 in yoga group, and we incorporated this information into our analyses. Measurement of expectations or treatment preferences at baseline: none. Funding: authors did not specify whether or not there was funding. Quote: "No competing financial interests exist." Trial registration ID: CTRI/2017/08/009572. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomized using a pregenerated randomized sequence." |
| Allocation concealment (selection bias) | Low risk | Quote: "Opaque sealed envelopes were used to conceal the allocation." |
| Blinding of participants | High risk | No blinding as control was exercise; outcomes based on self‐assessment. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | No blinding and outcomes based on self‐assessment. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | A high percentage of participants were lost to follow‐up at both outcome points. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported as prespecified in the registration. |
| Group similarity at baseline | Low risk | Baseline characteristics relevant to disease were comparable between groups, and exceptions were consistent with the relatively small sample size, indicating that randomization was not subverted. |
| Co‐interventions | Low risk | No mention of co‐interventions that were either allowed or forbidden; however, both groups received postural education and concomitant medication use in both groups was tracked. Quote: "Questions were asked to determine the weekly consumption of pain medication 12 for CNLBP [chronic non‐specific low back pain] management before the intervention. Changes in weekly drug consumption were recorded in both the groups at 6‐week postintervention and 12‐week follow‐up compared to baseline." |
| Compliance | Low risk | There were 6 weekly classes, and good adherence was defined as attending ≥ 4 classes. 47/70 participants attained this. |
| ITT analysis | Low risk | An ITT analysis was provided. |
| Timing of outcome assessments | Low risk | All participants followed at 6‐ and 12‐weeks. |
| Other bias | Low risk | No other biases identified. |
Patil 2018.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 88 nurses with chronic LBP of whom 82% had non‐specific LBP. Settings: tertiary care teaching hospital (the workplace of the nurses). Location of yoga classes not described. Country: India. Recruitment: "nurses were screened and referred by the orthopedician" however flow chart (Figure 1) stated "self and physician referred [sic]." Inclusion criteria: female nurses with diagnosis of non‐specific LBP, lumbar spondylosis, or intervertebral disk prolapse; LBP for ≥ 3 months as diagnosed by an orthopedician and knowledge of English, Hindi, and Kannada language. Exclusion criteria: pain due to organic causes such as infective and inflammatory conditions, metabolic disorders, and post‐traumatic condition; degenerative disorders of muscles; comorbid cardiac or neuropsychiatric illness; history of major surgery or injury; pregnant women; neurologic complications of chronic LBP. |
|
| Interventions |
Yoga group: (n = 44) 6 weeks of 60‐min yoga classes provided 5 days/week. Home practice: not mentioned. Exercise group: (n = 44) 6 weeks of 60‐min physical exercises provided 5 days/week. Common interventions: none described. Co‐interventions: no mention of included or excluded co‐interventions. Duration and follow‐up: interventions provided for 6 weeks and follow‐up finished at end of intervention. |
|
| Outcomes | Quality of life – mental (Psychological health scale of WHOQOL‐BREF questionnaire English and Keralan version at 6 weeks. Quality of life – physical (physical health scale of the WHOQOL‐BREF) at 6 weeks. Other outcomes collected: Social Relationships scale of the WHOQOL‐BREF, Environmental Health scale of the WHOQOL‐BREF. |
|
| Notes | Adverse events: no mention of assessment of adverse events. Measurement of expectations or treatment preferences at baseline: none. Funding: report stated there was no financial support or sponsorship. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: used random number generator (www.randomizer.org). |
| Allocation concealment (selection bias) | Unclear risk | Comment: no mention of allocation concealment. |
| Blinding of participants | High risk | No blinding. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | Comment: participants not blinded and outcomes based on self‐report. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "There were no dropouts in the study." |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol available. |
| Group similarity at baseline | Low risk | Quote: "Participants in the two groups did not differ much in relation to their age, education, or duration of illness between the groups as shown in Table 1." Quote: "There was a no significant difference between the yoga and control groups at the baseline for all the four domains of WHOQOLBREF: (a) physical (P = 0.296), (b) psychological (P = 0.987), (c) social (P = 0.661), and (d) environmental (P = 0.904) as shown in Table 5." |
| Co‐interventions | Unclear risk | Comment: no mention of medication use at baseline, or any permitted or disallowed co‐interventions during study. |
| Compliance | Unclear risk | Comment: no mention of compliance or adherence. |
| ITT analysis | Unclear risk | Comment: no mention of ITT analysis. |
| Timing of outcome assessments | Low risk | Quote: "Data were taken at the same time of the day on the 1 and 43 day. Orientation to yoga program was given to the participants for 3 days, and then on the next day, predata collection was done after satisfactory performance. WHOQOLBREF assessments were done on day 1 and day 43 (after 6 weeks)." |
| Other bias | Low risk | No other biases identified. |
Saper 2009.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 30 participants with moderate‐to‐severe chronic non‐specific LBP. Setting: study run from 2 community health centers. Yoga classes held at 1 of 2 community health centers. Country: USA. Recruitment: self‐referral and healthcare practitioner referral through flyers in the health centers and surrounding community, radio, and newspaper advertisements, and presentations and e‐mails to healthcare providers. Letters sent by providers to participants identified from community health center electronic medical records as seen in last 2 years with an LBP diagnosis. Inclusion criteria: men and women aged 18–64 years with current LBP persisting for ≥ 12 weeks, and mean LBP intensity for 2 weeks before enrolment rated ≥ 4 on a 0‐ to 10‐rating scale; sufficient understanding of English to follow class instructions and complete surveys. Exclusion criteria: yoga use in previous year; new pain medicine or other LBP treatments started within the previous month or anticipated to begin in next 6 months; pregnancy; back surgery in previous 3 years; non‐muscular pathologies (e.g. spinal canal stenosis, spondylolisthesis, infection, malignancy, fracture); severe or progressive neurologic deficits; sciatica pain ≥ back pain; active substance or alcohol abuse; serious systemic disease, medical, or psychiatric comorbidities precluding yoga practice; active or planned worker's compensation, disability, or personal injury claims; inability to attend classes at times and location offered. |
|
| Interventions |
Yoga group: (n = 15) 12 weekly 75‐min hatha yoga classes divided into 4 × 3‐week themed segments followed a standardized protocol in which each class began and ended with Savasana relaxation and breathing exercises, and included a selection from 22 or 23 other yoga postures depending on class. Home practice: 30 min/day strongly encouraged. Provided participants with audio CD of protocol; portable CD player; handbook describing and depicting the exercises; and yoga mat, strap, and block. Usual care group: (n = 15) participants continued usual care and were offered the yoga intervention after the 26‐week follow‐up. Common interventions: both groups continued to receive usual medical care and medications, and received a copy of The Back Pain Helpbook (Moore 1999). Co‐interventions: both groups were discouraged from beginning any new back pain treatments during study. Duration and follow‐up: interventions provided for 12 weeks and there was an additional follow‐up at 26 weeks. |
|
| Outcomes | Back‐specific function (RMDQ) at 6, 12, and 26 weeks. Mean pain for the previous week (0 = no pain to 10 = worst possible pain) at 6, 12, and 26 weeks. Global improvement (dichotomized into improved vs no change or worse) at 12 weeks. Other outcomes collected: SF‐36 Mental Health component (not reported in results); SF‐36 Physical Health component (not reported in results); changes in medication use at 6 and 12 months. |
|
| Notes | Adverse events: 1 yoga participant reported transient worsening of LBP that improved after discontinuing yoga. No other significant adverse events reported. Measurement of expectations or treatment preferences at baseline: none. Unpublished data: Dr Robert Saper e‐mailed endpoint data for pain and back‐related function at 6 weeks to LSW on 4 November 2014. Funding: US NIH. Quote: "Dr Saper is supported by a Career Development Award (K07 AT002915‐04) from the National Center for Complementary and Alternative Medicine (NCCAM), National Institutes of Health (NIH), Bethesda, Maryland. Dr Phillips is supported by a Mid‐career Investigator Award (5K24AT000589‐08) from NCCAM, NIH. NCCAM had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript for submission." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used computer‐generated permuted block to generate sequence. |
| Allocation concealment (selection bias) | Low risk | Opaque, sequentially numbered envelopes prepared by a biostatistician with no contact with participants. |
| Blinding of participants | High risk | No blinding as used waiting list control; outcomes based on self‐assessment. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | Quote: "All study participants met in person with unblinded research staff members to complete paper questionnaires at baseline, 6, and 12 weeks." Comment: participants were not blinded and self‐reported the outcomes, with the assistance of unblinded study staff. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Low attrition rates (3% at 12 weeks; 23% at 26 weeks) but reasons unclear and rate differed between groups. |
| Selective reporting (reporting bias) | Unclear risk | Outcomes reported as per protocol on ClinicalTrials.gov. However, SF‐36 was in protocol and in paper methods, but only lack of statistical significance was reported in results. |
| Group similarity at baseline | Low risk | Groups matched on most important indicators. |
| Co‐interventions | Low risk | Use of non‐study treatments by yoga group was 27% and control group was 40% (P = 0.7) up to 12 weeks and by yoga group was 87% and control group 100% between 12 and 26 weeks. |
| Compliance | Low risk | Quote: "Yoga participants attended a median of 8 classes (range 0–12)." |
| ITT analysis | Low risk | All randomized participants were analyzed in the group to which they were randomized and an ITT analysis with LOCF imputation for 1 missing yoga participant was carried out at 12 weeks and 7 missing yoga participants at 26 weeks. |
| Timing of outcome assessments | Low risk | Outcome assessment at set time points. |
| Other bias | Low risk | No other biases identified. |
Saper 2017.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 320 predominantly low‐income, racially diverse adults with non‐specific chronic LBP. Settings: 1 large academic safety‐net hospital and 7 affiliated, federally qualified community health centers located in diverse neighborhoods. Yoga classes held at community health centers. 8 physical therapists delivered the physical therapy intervention in 1 hospital‐based and 2 community‐based physical therapy clinics. Country: USA. Recruitment: recruited through the sites with multiple strategies including recruitment letters and flyers to patients with an electronic medical record diagnosis of LBP, study flyers in clinic waiting rooms and surrounding neighborhoods, contacts with health providers and clinic staff, and newspaper adverts. Inclusion criteria: aged 18–64 years; current non‐specific LBP persisting ≥ 12 weeks; mean LBP intensity for previous week ≥ 4 on a 0 to 10 numerical rating scale (where 10 was highest pain); English fluency sufficient to follow treatment instructions and answer survey questions; willingness to list comprehensive contact information for ≥ 1 friend, family member, or work colleague who will always know how to contact the participant. Exclusion criteria: significant participation in yoga or physical therapy for back pain or had read The Back Pain Helpbook or The Back Book in previous 6 months; known pregnancy; active or planned worker's compensation, disability, or personal injury claims; rheumatoid arthritis; severe fibromyalgia; plans to move out of area in next 12 months; perceived religious conflict with the yoga intervention; spinal canal stenosis, severe scoliosis, spondylolisthesis (> grade I), ankylosing spondylitis, large herniated disk, sciatica pain ≥ back pain, previous back surgery; history of vertebral fracture; active or recent malignancy; active or recent constitutional symptoms; back pain possibly due to specific disease/condition(s); severe or progressive neurologic deficits; active substance or alcohol abuse; cervical radiculopathy; other severe disabling chronic medical or psychiatric comorbidities (or both) deemed by principal investigator on a case‐by‐case basis to prevent safe or adequate (or both) participation in study (e.g. severe disabling heart failure or lung disease, active treatment for hepatitis, psychosis). |
|
| Interventions |
Yoga group: (n = 127) 12 weekly 75‐min hatha yoga classes followed by randomization to drop‐in classes or home practice in a maintenance phase until week 52. Home practice: strongly encouraged to do yoga home practice for 30 min/day on days that they did not attend yoga class. To facilitate home practice, participants received DVD of protocol; guidebook describing and depicting the protocol (Additional file 1); and a yoga mat, strap, and block. Physical therapy group: (n = 129) 15 × 60‐min appointments over 12 weeks, followed by randomization to booster sessions (advice to see the therapist at 4, 6, 8, 10, and 12 months) or no booster sessions during maintenance phase until week 52. Home practice: participants received written materials and supplies (strap, mat) for home practice and were recommended to exercise at home for 30 min on days when there was no physical therapy session. Usual care group: (n = 64) The Back Pain Helpbook (Moore 1999), reading schedule, and newsletters over 12 weeks, followed by brief check‐in calls every 6 weeks to encourage continued review of the book until 52 weeks. Common interventions: all groups continued to receive their usual medical care and medications. Co‐interventions: both groups were discouraged from beginning any new back pain treatments during study. Duration and follow‐up: interventions were provided for 12 weeks, there was re‐randomization of the yoga and physical therapy participants to different intensities of maintenance treatment until week 52, and the final follow‐up was at 52 weeks. |
|
| Outcomes | Back‐specific function (RMDQ) at 6, 12, 26, 40, and 52 weeks. Mean pain for the previous week (0 = no pain to 10 = worst possible pain) at 6, 12, 26, 40, and 52 weeks. Global improvement – 0‐ to 6‐point Likert scale, where 0 indicated extremely worsened, 3 indicated no change, and 6 indicated extremely improved. Participants who reported a 5 or 6 were considered improved at 12 weeks. Health‐related quality of life – physical (SF‐36 Physical Health component) at 12 weeks. Health‐related quality of life – mental (SF‐36 Mental Health component) at 12 weeks. Other outcomes collected: self‐reported pain medication use in previous week (yes or no), patient satisfaction with interventions (5‐point scale from very dissatisfied to very satisfied), work productivity. Also planned to report data on other exploratory measures (e.g. fear‐avoidance beliefs, pain self‐efficacy, depression, anxiety, and sleep. |
|
| Notes | Adverse events: mostly mild self‐limited joint and back pain reported in 9 yoga, 14 physical therapy, and 1 education participants. Measurement of expectations or treatment preferences at baseline: none. Unpublished data: none. Funding: government (National Center for Complementary and Integrative Health). Study name: 'Back to Health.' Trial registration: NCT01343927. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Staff entered participants into StudyTRAX (ScienceTrax), a data management platform. StudyTRAX generated a randomization sequence using permuted block randomization with varying block sizes and a 2:2:1 ratio of yoga, PT, and education." |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not clearly described. Quote: "After participants completed baseline surveys, un‐masked staff informed them of their treatment assignments." |
| Blinding of participants | High risk | No blinding possible. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | Blinding not possible and outcomes based on self‐report. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "To comply with the journal editors' recommendations for handling missing data in our primary outcome analyses, we present findings based on multiple imputation using regression modeling in SAS PROC MI." "The PT group had disproportionate loss to follow‐up." Comment: although multiple imputation was used to account for missing data, the number of participants dropping out of the physical therapy group was very high (n = 15) compared to the yoga and education groups (n = 2 and n = 3). We considered the risk of attrition bias for the comparison between yoga and education to be low risk, and the risk of attrition bias for the comparison between yoga and physical therapy to be high risk. |
| Selective reporting (reporting bias) | Low risk | Employment status was a secondary outcome in the protocol but was not reported. In Supplement 1 to the main publication, the authors noted that it will be reported in a future publication. Furthermore, Supplement 1 states: "Satisfaction and global improvement were unintentionally omitted from the clinicaltrials.gov listing when it was created in 2011." |
| Group similarity at baseline | Unclear risk | Quote: "Baseline mean between‐group differences were present for RMDQ, sex, and body mass index (P = 0.032, 0.088, and 0.099, respectively)." |
| Co‐interventions | Low risk | Quote: "At 12 weeks, yoga and PT [physical therapy] participants were 21 and 22 percentage points, respectively, less likely than education participants to use any pain medication (Table 6). Although PT participants were less likely than education participants to use acetaminophen [paracetamol], there were no other significant differences in medication sub‐groups." Comment: medication use was similar at baseline and was a secondary outcome. |
| Compliance | High risk | The protocol predefined adherence: (quote) "For the 12‐week Treatment Phase, adherence is defined as follows: ≥75% attendance to recommended yoga classes (i.e., 9 or more); ≥73% attendance to PT sessions (i.e., 11 or more); self‐reported completion of three‐fourths or more of assigned educational materials." In the trial report, it was stated that (quote) "During the treatment phase, median yoga attendance was 7 classes (interquartile range, 3 to 10)." and "Fewer than half of the participants met adherence criteria: 56 yoga (44%), 46 PT (36%), and 28 education (44%) participants." Comment: although it is possible that 50% of participants attended ≥ 50% of classes, it is not clear from study report and so we rated compliance as high risk because study authors identified it as a concern. |
| ITT analysis | Low risk | Used recommended process for dealing with missing data. |
| Timing of outcome assessments | Low risk | Outcome assessment at set time points. |
| Other bias | Low risk | No other biases identified. |
Sherman 2005.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 101 participants with chronic non‐specific LBP. Setting: trial run through an integrated healthcare system. Yoga classes held at health system facilities (number of facilities not stated). Country: USA. Recruitment: invitations describing study sent by researchers to people with primary care provider visits between 3 and 15 months before the study for treatment of back pain. Self‐referral through advertisements in a health plan consumer magazine. Inclusion criteria: men and women aged 20–64 years with recent primary care visit for LBP. Exclusion criteria: back pain that was complicated (e.g. sciatica); potentially attributable to underlying disease or conditions (e.g. pregnancy); minimal (rating < 3 on a 'bothersomeness' scale of 0 to 10); had been treated with yoga or exercise in past year; currently treated with other interventions; possible disincentive to improve (e.g. were receiving worker's compensation); had severe or unstable medical or psychiatric conditions or dementia; had contraindications to the intervention (e.g. symptoms consistent with severe disk disease), unable to participate in classes or unwilling to practice at home; unable to speak or understand English. Duration and follow‐up: interventions provided for 12 weeks with additional follow‐up at 26 weeks. |
|
| Interventions |
Yoga group: (n = 36) 12 weekly 75‐min viniyoga classes, each with a specific focus: (quotes) "relaxation; strength building, flexibility, and large‐muscle movement; asymmetric poses; strengthening the hip muscles; lateral bending; integration; and customizing a personal practice." "[A]ll the sessions emphasized use of postures and breathing for managing low back symptoms…" "[P]ostures were selected from a core of 17 relatively simple postures…" "Each class included a question‐and‐answer period, an initial and final breathing exercise, 5–12 postures, and a guided deep relaxation." Home practice: daily home practice encouraged and yoga participants received CDs to guide them through the postures with the appropriate mental focus. Exercise group: (n = 35) 12 weekly 75‐min exercise classes. Intervention designed by a physiotherapist and was likely different from previous physiotherapy. Exercise sessions began with an educational talk, then simple warm‐ups and a series of 7 aerobic exercises and 10 strengthening exercises, ending with stretching exercises and a short, unguided period of deep breathing. Home practice: encouraged and exercise participants received a handout to assist them. Self‐care group: (n = 30) a copy of an evidence‐based book of self‐care strategies was mailed to participants (Moore 1999). Common interventions: all participants continued to have access to all medical care provided by their insurance plan. Co‐interventions: no specific mention of allowed or restricted co‐interventions. |
|
| Outcomes | Back‐specific function (RMDQ) at 6, 12, and 26 weeks. Other outcomes collected: bothersomeness of pain during the previous week (0 = 'not at all bothersome' and 10 = 'extremely bothersome'); SF‐36 Mental Health component (not reported in results); SF‐36 Physical Health component (not reported in results); changes in medication use at 6 and 12 months. |
|
| Notes | Adverse events: no serious adverse events reported. 1 participant discontinued yoga classes because postures that required her to move her head below her heart precipitated her migraine headaches. 1 participant in exercise class strained her back during class and sought care from a chiropractor. Measurement of expectations or treatment preferences at baseline: participants were asked to describe their current pain and to rate their expectations for each intervention. Table 1 of the publication showed median expectation of helpfulness for each treatment in each group: median of 8 for exercise and yoga in both the exercise and yoga groups, median of 8.5 for exercise and 9 for yoga in the self‐care group, and median of 4 or 5 for self‐care in each intervention group. Preferred treatment was exercise for 26–33%, yoga for 27–44%, and other for 28–40%. Reported similar expectations of helpfulness from yoga or exercise but had lower expectations for the book. Unpublished data: Dr Karen Sherman e‐mailed LSW on 23 November 2015 that she did not have group means and standard deviations available from her trial. Funding: US National Institutes of Health (NIH). Quote: "Grant Support: By the National Center for Complementary and Alternative Medicine (grant R21AT 001215) and the National Institute for Arthritis and Musculoskeletal and Skin Diseases (grant P60AR48093). Potential Financial Conflicts of Interest: None disclosed." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used computer‐generated random assignments. |
| Allocation concealment (selection bias) | Low risk | A researcher not involved in participant recruitment or randomization placed assignments in opaque sequentially numbered envelopes. |
| Blinding of participants | High risk | No blinding as control interventions were conventional exercise or self‐care book; outcomes based on self‐assessment. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | Quote: "Interviewers who were masked to the treatment assignments conducted telephone interviews at baseline and at 6, 12, and 26 weeks after randomization." Comment: however, participants were not blinded and self‐reported the outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Very low attrition rates (total 6% at 26 weeks) although there was no description of how missing data were managed. |
| Selective reporting (reporting bias) | Unclear risk | Clinical outcomes reported as per description on ClinicalTrials.gov, where there was not a formal statement of primary and secondary outcomes but a statement that the trial will report (quote) "symptoms, function, quality of life, and utilization and costs of back pain related care." However, utilization and costs were not mentioned in the study report. |
| Group similarity at baseline | Low risk | Groups matched on most important indicators. |
| Co‐interventions | Low risk | Use of non‐study treatments matched initially and reduced in yoga group compared with control groups. |
| Compliance | Low risk | 36/36 yoga participants attended ≥ 1 class and the median number attended was 9 out of a possible 12. For exercise, 33/35 participants attended ≥ 1 class and the median number attended was 8. Class attendance was similar for yoga and exercise groups. |
| ITT analysis | Low risk | All randomized participants were stated to be analyzed in the group to which they were randomized. |
| Timing of outcome assessments | Low risk | Outcome assessment at set time points. |
| Other bias | Low risk | No other biases identified. |
Sherman 2011.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 228 participants with chronic non‐specific LBP. Setting: trial run through an integrated healthcare system. 7 cohorts of classes were held in 6 different cities. Yoga classes were held at the health system facilities (exact number of facilities not stated). Country: USA. Recruitment: invitations mailed to people with primary care visits for back pain, advertisements in a health plan consumer magazine, and direct‐mail postcards. For 4 cohorts, augmentation of recruitment through outreach to general population (methods not described). Inclusion criteria: men and women aged 20–64 years with LBP. Exclusion criteria: people with back pain that was attributable to a specific cause (e.g. spondylolisthesis), or an underlying condition (e.g. pregnancy), complex (e.g. sciatica), minimally painful (i.e. rating of < 3 on a 'bothersomeness' scale of 0 to 10), or not chronic (i.e. duration < 3 months); had contraindications to the interventions (e.g. severe disc disease); had major depression; were unable to give informed consent or participate in interviews owing to mental or medical issues (e.g. dementia) or an inability to speak English; or were unable to participate in classes or unwilling to practice at home. Duration and follow‐up: interventions were provided for 12 weeks and there was an additional follow‐up at 26 weeks. |
|
| Interventions |
Yoga group: (n = 92) 12 weekly 75‐min viniyoga classes. The viniyoga intervention was the same as that used in an earlier trial (Sherman 2005). Classes included breathing exercises, a set of 5–11 postures, and guided deep relaxation. 6 distinct and progressive classes were taught in pairs. Home practice: encouraged for 20 min on non‐class days. Yoga participants received a handout and CD to assist them in home practice. Exercise group: (n = 91) 12 weekly 75‐min exercise classes. The exercise intervention was adapted from the intervention used in an earlier trial (Sherman 2005). Classes included aerobic exercises, stretches, and strengthening exercises. Home practice: encouraged for 20 min on non‐class days. Exercise participants received a handout and DVD to assist them in home practice. Self‐care group: (n = 45) participants received a copy of The Back Pain Helpbook providing information on causes of back pain and advice on how to manage pain (Moore 1999). Common interventions: all intervention groups continued to have access to medical care provided by their insurance plan. Co‐interventions: no specific mention of allowed or restricted co‐interventions. |
|
| Outcomes | Back‐specific function (RMDQ) at 6, 12, and 26 weeks. Clinical improvement (dichotomous variable measuring whether LBP was improved, yes/no) at 6, 12, and 26 weeks. Other outcomes collected: bothersomeness of pain during the previous week (0 = 'not at all bothersome' and 10 = 'extremely bothersome'); 30% improvement in outcomes; 50% improvement in outcomes; very satisfied with overall care for lower back pain; days of activity restriction (not presented in study results); days in bed (not presented in study results); work loss (not presented in study results). |
|
| Notes | Adverse events: of the 87 yoga and 75 stretching class attendees, 13 in each group reported a mild or moderate adverse experience possibly related to treatment (mostly increased back pain), and 1 yoga attendee experienced a herniated disk. 1/45 participants randomized to self‐care reported increased pain after doing recommended exercises. Measurement of expectations or treatment preferences at baseline: before randomization, information on sociodemographic characteristics, back pain history, and treatment‐related beliefs collected. Table 1 of publication showed the median expectation of helpfulness for each treatment in each group: it was a median of 8 for yoga and exercise for all groups, and a median of 4 for self‐care for all groups. Preferred treatment was yoga for 26–32%, exercise for 17–22%, and other for 51–53% in intervention groups. Funding: US NIH. Quote: "Financial Disclosure: None reported. Funding/Support: This study was funded by Cooperative Agreement Number U01 AT003208 from the National Center for Complementary and Alternative Medicine (NCCAM). Discussions with several NCCAM staff influenced the study design." Additional notes: we extracted data from the online supplement to the Annals 2011 publication, choosing the adjusted 2‐step imputed data from eTable 4 for the primary analysis, and the adjusted complete‐case analysis from eTable 4 for the complete‐case sensitivity analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization used. |
| Allocation concealment (selection bias) | Low risk | Randomization schedule generated by statistician; inaccessible to staff. |
| Blinding of participants | High risk | No blinding as control interventions were conventional exercise or self‐care book; outcomes based on self‐assessment. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | Quote: "Telephone interviews were conducted by masked interviewers at baseline and at 6, 12, and 26 weeks after randomization." Comment: however, participants were not blinded and self‐reported the outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rates; authors also conducted a secondary analysis using a single imputation method to assess the sensitivity of the complete‐case results to loss to follow‐up. The sensitivity analysis was provided online and was consistent with the primary outcomes. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported as per published trial protocol. Note: several mediating variables mentioned in protocol not reported in primary publication. |
| Group similarity at baseline | Unclear risk | Groups matched on most important indicators except that yoga group had greater back pain dysfunction. |
| Co‐interventions | Low risk | No between‐group differences in back pain‐related healthcare visits; medication use matched initially and decreased in yoga and exercise (active intervention) groups. |
| Compliance | Low risk | 95% of yoga participants attended ≥ 1 class and they attended a median of 8 out of a possible 12 classes. 82% of exercise participants attended ≥ 1 class and they attended a median of 9 classes. 65% (yoga) and 59% (exercise) attended ≥ 8 classes. |
| ITT analysis | Low risk | Statement that ITT analysis was carried out. |
| Timing of outcome assessments | Low risk | Outcome assessment at set time points. |
| Other bias | Low risk | No other biases identified. |
Tekur 2008.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 80 participants with chronic non‐specific LBP. Setting: trial run through a residential holistic health center. Yoga classes held at the health center. Country: India. Recruitment: by advertisements, newsletters, self‐referrals, word‐of‐mouth, or referrals by medical practitioners. Inclusion criteria: men and women aged 18–60 years with LBP (with or without pain radiating to the legs) ≥ 3 months in duration. Exclusion criteria: back pain attributable to organic spinal pathology (e.g. malignancy) or chronic spinal infection (checked by x‐ray); severe obesity or critical illness. Duration and follow‐up: interventions were provided for 7 days and follow‐up ended on the final day of the intervention. |
|
| Interventions |
Yoga group: (n = 40) intensive 1‐week residential yoga program. Practices consisted of asanas for back pain (yoga postures), pranayama, relaxation techniques, meditation, and lectures on yogic lifestyle, devotional sessions and stress management through yogic counseling. Intervention provided throughout the day for 7 consecutive days, and included approximately 2 hours/day of yoga postures as well as yogic meditation, breathing, chanting, and lectures. No home practice: none. Exercise group: (n = 40) intensive 1‐week residential program of non‐yogic physical exercises. Practices consisted of a set of physical movements, non‐yogic safe breathing exercises, and lectures on scientific information. Classes supervised by the trained physiatrist. Intervention was provided throughout the day for 7 consecutive days, and included approximately 2 hours/day of exercise practices. Home practice: none. Common interventions: no other interventions in common. Co‐interventions: no specific mention of allowed or restricted co‐interventions. |
|
| Outcomes | Back‐specific function (Oswestry Disability Index, range 0–100) at 1 week. Pain (Horizontal 10‐cm straight line on a white sheet, range 0–10) at 1 week. Quality of life – physical (WHOQOL‐BREF Physical Health domain (7 items), range of scores 4–20 for each domain) at 1 week. Quality of life – mental (WHOQOL‐BREF Psychological Health domain (6 items), range of scores 4–20 for each domain) at 1 week. Other outcomes collected: spinal mobility, STAI, Beck's Depression Inventory, sit and reach measures, perceived stress, straight leg raising test, and WHOQOL‐BREF Social and Environmental area domains. |
|
| Notes | Adverse events: 0 in either group. Measurement of expectations or treatment preferences at baseline: none. Funding: Swami Vivekananda Yoga Research Foundation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used computer‐generated random numbers. |
| Allocation concealment (selection bias) | Low risk | Containers used to conceal the sequence until interventions were assigned. |
| Blinding of participants | High risk | No blinding as control was exercise; pain, functioning, and quality of life were self‐assessed. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | Quote: "The statistician who did the randomization and analysis of data and the researcher who enrolled the subjects, assigned them to groups, and carried out the assessments were blinded to the subjects' treatment status." Comment: however, participants were not blinded, and outcomes were self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate among participants randomized (13% per group) was prior to beginning of treatment and there was no attrition among participants who began treatment; reasons for dropout similar and not related to outcome. |
| Selective reporting (reporting bias) | Unclear risk | Protocol unavailable. |
| Group similarity at baseline | Low risk | Groups matched on most important indicators. |
| Co‐interventions | Low risk | Quote: "Both groups had the same daily routine with matched interventions." |
| Compliance | Unclear risk | Daily sessions under supervision but no numbers of attendees reported. |
| ITT analysis | Unclear risk | No reason to suspect participants were not analyzed in the groups they were assigned to; however, this was not explicitly stated. |
| Timing of outcome assessments | Low risk | Outcome assessment at set time points. |
| Other bias | Low risk | No other biases identified. |
Teut 2016.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 176 adults aged ≥ 65 years with chronic LBP. Settings: based at a university and the yoga classes were held either at the university or retirement homes. Country: Germany. Recruitment: distribution of brochures and handouts, holding information events in retirement homes, and advertising in newspapers. Planned half of participants would live on their own and half would live in retirement homes. Participants in retirement homes were recruited directly at the retirement homes to ensure that they could participate. Inclusion criteria: adults ≥ 65 years, chronic LBP for ≥ 6 months; intensity of back pain according to pain item of the Functional Rating Index ≥ 2 over past 7 days; providing written informed consent. Exclusion criteria: acute disk prolapse or protrusion with acute neurologic symptoms within past 3 months; severe organic or psychiatric disease precluding participation in trial; pain due to cancerous effects on bones; use of pain medication that works through the central nervous system (e.g. opioids); drug or alcohol addiction (or both); participation in another clinical trial within past 6 months; participation in yoga or qigong training within past 12 months; preplanned start of a physiotherapy within study duration. |
|
| Interventions |
Yoga group: (n = 61) 24 × 45‐min viniyoga yoga classes over 3 months. Home practice: none. Qigong group: (n = 58) 12 × 90‐min qigong classes provided over 3 months. Home practice: none. Waiting list group: (n = 57) no specific intervention and were allowed to participate in either yoga or qigong at end of follow‐up (6 months). Common interventions: all groups continued to receive their usual medical care and medications. Co‐interventions: all groups were allowed concomitant health care except for physiotherapy and central nervous system pain medication. Duration and follow‐up: interventions provided for 3 months and follow‐up ended at 6 months. |
|
| Outcomes | Back‐specific function (Hannover Functional Ability Questionnaire for measuring back pain‐related disability) at 3 and 6 months. Back pain (mean pain for the previous 7 days on a 100 mm VAS) at 3 and 6 months. Health‐related quality of life – physical (SF‐36 Physical Health component) at 3 and 6 months. Health‐related quality of life – mental (SF‐36 Mental Health component) at 3 and 6 months. Depression (Geriatric Depression Scale) at 3 and 6 months. Other outcomes collected: mean pain intensity over past 7 days on the Functional Rating Index, pain medication, frequency of falls, risk of falls measured using the Tinetti Test, body self‐efficacy, the handgrip strength test, credibility and treatment satisfaction. |
|
| Notes | Adverse events: reported to be assessed in the methods section but the occurrence of adverse effects was not mentioned in the results or discussion sections. Measurement of expectations or treatment preferences at baseline: expectations of yoga and qigong were assessed at baseline. Unpublished data: none. Funding: non‐profit. Quote: "This study was performed as part of the grant for the professorship for complementary medicine funded by the Karl and Veronica Carstens‐Foundation. The Yoga intervention was funded by Berliner Yoga Zentrum." Clinical trial registration: NCT01303588. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was carried out using the random function of SAS software (version 9.1; SAS Inc, Cary, NC). The allocation ratio of yoga:qigong:control group was 1:1:1. The randomization was stratified according to the participant housing situation (living in a retirement home or living alone) and blocked with a fixed block length, which was unknown to the study staff." |
| Allocation concealment (selection bias) | Low risk | Quote: "The randomization list was transferred to a generated Microsoft Access 2003 (Microsoft Corp, Redmond, CA) secured database, where it was hidden in the background and was not accessible to anyone involved in randomization or treatment to ensure allocation concealment." Quote: "Patients who fulfilled the eligibility criteria and provided informed consent were registered in the preface of the database and randomized by clicking on a button. The group allocation was then revealed to the participants. The group allocation could not be changed or deleted, which ensured allocation concealment." |
| Blinding of participants | High risk | No blinding. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | Participants not blinded and outcomes based on self‐report. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: proportion missing from follow‐up was not high, did not differ substantially between groups, and reasons for loss to follow‐up were given. |
| Selective reporting (reporting bias) | Low risk | Comment: all primary and secondary outcomes corresponded to those in the trial registration. |
| Group similarity at baseline | Low risk | Quote: "Table 1 [of publication] shows the sociodemographic and clinical characteristics of the patients at baseline. The mean age was similar in all groups. Furthermore, most of the participants were women. The mean duration of the back pain was between 18 and 20 years for all groups, and >60% of the patients used pain medication. In the yoga class, there was a lower percentage of patients with >10 years of education (24.6% compared with 43.1% and 43.9%). In the qigong group, there was a lower percentage of single households (59.9% compared with 78.0% and 71.4%). In the control group, the period elapsed since the last physical therapy session was shorter than the period in either of the intervention groups (1.1 ± 2.4 years for the control group compared with 2.2 ± 3.7 years for the yoga group and 2.7 ± 4.8 years for the qigong group). All other baseline data measurements and clinical outcomes were nearly equally distributed among the groups." Comment: almost all demographic characteristics matched. A sensitivity analysis for period since last physical therapy session did not change the results. |
| Co‐interventions | Low risk | Quote: "Participants in both groups were allowed to use concomitant health care, but the use of physiotherapy and the intake of pain medication that works over the central nervous system (e.g., opioids) were not permitted." Comment: mean medication use at baseline was similar between groups, and restriction of physiotherapy and opioids during the trial is mentioned. |
| Compliance | Low risk | Quote: "Of all patients in the yoga group, 74.1% participated in more than 75% of the yoga lessons, another 12.9% in 50 to 75% of the lessons. From 58 patients allocated to the qigong group 3 refused further participation (medical reasons: n = 1, lack of time: n = 1, unknown reasons: n = 1). Of the patients in the qigong group, 72.7% participated in more than 75% of the classes, and another 18.2% participated in 50 to 75% of the classes." |
| ITT analysis | Low risk | Quote: "Outcomes were analyzed for the full analysis set, on the basis of the intention‐to‐treat principle. The full analysis set includes each randomized patient regardless of whether he or she adhered to the assigned treatment, complied with the protocol, or provided a complete set of all data. If any outcome data were missing, these values were not imputed. Thus, for each outcome the respective available cases were used in the analysis." |
| Timing of outcome assessments | Low risk | Timing of outcome assessment appeared to be the same for all groups. |
| Other bias | Low risk | No other biases identified. |
Tilbrook 2011.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 313 participants with chronic non‐specific LBP. Setting: 39 general practices. Yoga classes were held in 13 non‐National Health Service premises in 5 geographic areas. Country: UK. Recruitment: participating general medical practices searched patient databases and mailed out an invitation pack to all individuals aged 18–65 years who had visited for LBP in past 18 months; database searches were undertaken in 2 waves. In addition, during the second wave of recruitment, advertisements were placed in local media. Inclusion criteria: men and women aged 18–65 years with LBP (i.e. musculoskeletal pain bounded by the lowest ribs and gluteal folds) in previous 18 months, score ≥ 4 on RMDQ, and ability to attend ≥ 1 yoga classes. Exclusion criteria: did not return a baseline questionnaire (second recruitment wave only); had performed yoga in previous 6 months; could not get up off the floor unaided; could not use stairs; pregnant; had life‐threatening comorbid conditions; had previously undergone spinal surgery; had severe documented psychiatric problems or alcohol dependency; had indications of serious spinal neurologic abnormality (≥ 1 of difficulty passing urine; numbness around anus, genitals, or inner thighs; numbness, pins and needles, or weakness in both legs; or unsteadiness on feet). Duration and follow‐up: interventions provided for 12 weeks and additional follow‐up at 12 months. |
|
| Interventions |
Yoga group: (n = 156) 12 weekly 75‐min yoga classes consisting of an introduction to the weekly theme; pain‐relieving or settling‐in relaxing poses; program of seated, standing, prone, and supine poses; educative postural advice; and 5–15 min of relaxation. Home practice: encouraged to undertake yoga for 30 min daily or to practice ≥ 2 times per week, and use the relaxation CD. Usual care group: (n = 157) participants received a copy of The Back Book on managing LBP (Burton 2002), and continued to receive usual care. Common interventions: both groups received a copy of The Back Book (Burton 2002), and continued to receive usual care. Co‐interventions: no specific mention of included or excluded co‐interventions. |
|
| Outcomes | Back‐specific function (RMDQ) at 3, 6, and 12 months. Back pain (Aberdeen Back Pain Scale) at 3, 6, and 12 months. Quality of life – mental (SF‐12 Mental Component score) at 3, 6, and 12 months. Quality of life – physical (SF‐12 Physical Component score) at 3, 6, and 12 months. Other outcomes collected: self‐efficacy scores on the Pain Self‐Efficacy Questionnaire, ratings on the EQ‐5D Health Index, number of days spent in bed and number of days with restricted activity, and economic data including medication use over the previous 4 weeks and other healthcare use. |
|
| Notes | Adverse events: 12/156 (8%) yoga participants and 2/157 (1%) usual care participants reported adverse events. In yoga group, authors classified 1 adverse event as serious and possibly or probably related to yoga (participant experienced severe pain but had a history of severe pain after any physical activity); remaining 11 were non‐serious and mostly related to increased pain. In usual care group, there were 2 serious adverse events. Measurement of expectations or treatment preferences at baseline: Table 1 of publication showed that expectation that yoga works was 57% in yoga group and 55% in usual care group. Belief that yoga works was 60% in yoga group and 52% in usual care group. Intervention preference was 72% yoga, 3% usual care, and 25% indifferent in yoga group, and 61% yoga, 4% usual care, and 35% indifferent in usual care. For primary outcome of back‐related function, the effect of treatment did not vary by baseline intervention preference (P for interaction = 0.39). Unpublished data: Dr Helen Tilbrook and Dr Catherine Hewitt clarified the numbers of participants for analyses in an e‐mail to LSW on 3 March 2015 and sent endpoint values for back‐related function, pain, physical quality of life, and mental quality of life to LSW by e‐mail on 21 December 2015. Funding: Arthritis Research UK and sponsored by University of York. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used computer‐generated randomization. |
| Allocation concealment (selection bias) | Low risk | Used computer‐generated randomization. Participant details entered into randomization database by trial co‐ordinators and secretary who were blinded to the allocation sequence. |
| Blinding of participants | High risk | No blinding as comparison was usual care; outcomes based on self‐assessment. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | Quote: "The statistician was blinded to randomized group." Comment: however, participants were not blinded, and outcomes were self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate, reasons stated, and sensitivity analyses for best/worst‐case scenarios were carried out. |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes as per published trial protocol. |
| Group similarity at baseline | Low risk | Groups matched on main prognostic indicators and co‐interventions at baseline. |
| Co‐interventions | Unclear risk | No details of co‐interventions during intervention period. |
| Compliance | Low risk | Quote: "Ninety‐three (60%) participants attended at least 3 of the first 6 classes and at least any other 3 classes (adhered)." |
| ITT analysis | Low risk | ITT analysis carried out and best/worst‐case analyses used for missing data. |
| Timing of outcome assessments | Low risk | Outcome assessment at set time points. |
| Other bias | Low risk | No other biases identified. |
Wattamwar 2013.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 24 participants with chronic non‐specific LBP. Setting: setting of trial not described. Yoga classes held at an iyengar yoga center. Country: India. Recruitment: not described. Inclusion criteria: ambulatory men and women aged 20–50 years with history of LBP and symptom duration > 3 months. Exclusion criteria: LBP attributable to any pathology; history of trauma or any neurologic condition. Duration and follow‐up: interventions provided for 10 weeks and no additional follow‐up. |
|
| Interventions |
Yoga plus occupational therapy group: (n = 12) 1 × 45‐ to 60‐min session of iyengar‐based yoga – using props – per week for 10 weeks. 2 × 45‐ to 60‐min occupational therapy sessions were also received each week. This was the same as the occupational therapy received by the control group, except that some simple asanas and pranayamas were added to the occupational therapy sessions for the yoga group. Home practice: back exercises with additional simple asanas and pranayamas was suggested. Frequency and duration of this home practice not described. Occupational therapy group: (n = 12) 3 × 45‐ to 60‐min occupational therapy sessions each week for 10 weeks. The therapy was described as mostly back school therapy and consisted of education, mat exercises, and Swiss ball exercises. Home practice: home program of back exercises suggested. Common interventions: no additional interventions. Co‐interventions: no specific mention of included or excluded co‐interventions. |
|
| Outcomes | Back‐specific function (Oswestry Disability Index) at 10 weeks (10 questions each rated on a 0 to 5 scale (higher score is worse function)) obtained from the Oswestry Low Back Pain Disability Questionnaire. Usually the individual scores are summed and multiplied by 2 to produce an overall rating on a 0 to 100 scale. Study authors provided individual mean differences and an overall mean difference for each group. Based on these data, it appeared that the study authors did not multiply the total by 2 and the reported Oswestry total was on a scale of 0 to 50. Therefore, we multiplied the totals by 2 for data entry in this review. Back pain (Pain Intensity subscore of the Oswestry Disability Index, scale 0–5; higher values indicated greater pain) at 10 weeks. Other outcomes collected: RMDQ (outcome not extractable), changes in range of motion of thoraco‐lumbar spine, and change in muscle strength of abdominals and back extensors. |
|
| Notes | Adverse events: no discussion of overall safety or adverse events. Measurement of expectations or treatment preferences at baseline: none. Unpublished data: we contacted Dr Ravi Wattamwar to clarify sample size and standard deviations of change or confidence interval for RMDQ on 2 April 2015. He replied to the e‐mail but did not forward the information. Therefore, we used the Oswestry Disability Index, which was completely reported, for the review. Funding: not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization by lottery method with replacement. |
| Allocation concealment (selection bias) | Unclear risk | No details of allocation process. |
| Blinding of participants | High risk | No blinding as comparison was occupational therapy without adjuvant yoga; outcomes based on self‐assessment. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | No mention of blinding for those who collected the outcomes. Participants were not blinded, and outcomes were self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition. |
| Selective reporting (reporting bias) | High risk | RMDQ was incompletely reported. Protocol not available. |
| Group similarity at baseline | Unclear risk | Limited demographic data reported. |
| Co‐interventions | Unclear risk | No details of co‐interventions. |
| Compliance | Unclear risk | No information on class attendance. |
| ITT analysis | Unclear risk | No attrition and no suspicion that participants were not analyzed in the groups they were assigned to; however, this was not explicitly stated. |
| Timing of outcome assessments | Low risk | Outcome assessment at set time points. |
| Other bias | Low risk | No other biases identified. |
Williams 2005.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 60 participants with chronic non‐specific LBP. Setting: setting of trial not described. Yoga delivered in a community yoga studio. Country: USA. Recruitment: physician and self‐referral. Local physicians were informed about the study through lectures and mailed announcements. Project was announced to the public through flyers, public radio, and local university list serve for faculty and staff. Inclusion criteria: ambulatory English‐speaking men and women aged > 18 years with history of LBP and symptom duration > 3 months. Exclusion criteria: LBP attributable to nerve root compression, disk prolapse, spinal stenosis, tumor, spinal infection, alkylosing spondylosis, spondylolisthesis, kyphosis or structural scoliosis, or a widespread neurologic disorder; presurgical candidates; involved in litigation or compensation; displayed a compromised cardiopulmonary system; pregnant; BMI > 35; experiencing major depression or substance abuse; practitioners of yoga; did not agree to "forgo other forms of CAM [Complementary Alternative Medicine] during the study." Duration and follow‐up: interventions provided for 16 weeks and an additional follow‐up at 3 months after end of treatment (7 months after randomization). |
|
| Interventions |
Yoga group: (n = 30) 1 × 90‐min iyengar yoga class per week for 16 weeks. Classes used supine, seated, and standing poses; forward bends, twists, and inversions; and progressed from simple to more challenging poses. Used a range of props. Yoga group also received 16 weekly newsletters, written by physiotherapy students, on back care. Home practice: encouraged to practice at home for 30 min/day, 5 days/week. Education group: (n = 30) 16 weekly newsletters, written by physiotherapy students, on back care. Common interventions: all participants could continue usual medical care for LBP. 2 weeks before beginning of 16‐week study period, both groups received 2 × 1‐hour lectures on LBP and were given instructional handouts. Co‐interventions: participants were only eligible for the study if they agreed to "forgo other forms of CAM during the study." |
|
| Outcomes | Back‐specific function (Pain Disability Index) at 16 weeks and 7 months. Back pain (VAS from Short Form‐McGill Pain Questionnaire) at 16 weeks and 7 months. Other outcomes collected: pain‐related fears to movement, beliefs associated with adjustment to chronic pain, coping strategies, perception of self‐efficacy, spinal range of motion, and changes from baseline in medications reported at baseline. |
|
| Notes | Adverse events: 1 adverse event in the yoga group, quotes: "a subject with symptomatic osteoarthritis who was diagnosed with a herniated disc during the study…" "Review of the adverse event by a medical panel summoned by the Institutional Review Board determined that it was unrelated to the performance of yoga postures." 1 older participant in the educational control group died. Measurement of expectations or treatment preferences at baseline: none. Funding; university funding. Quote: "This project was funded by the Clinical Studies request for proposals at West Virginia University." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization by random number generating program. |
| Allocation concealment (selection bias) | Unclear risk | No details of allocation process. |
| Blinding of participants | High risk | No blinding as comparison was an educational intervention; outcome based on self‐assessment. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | Participants were not blinded, and outcomes were self‐reported. Quote: "Data collectors were blind to the subject's treatment status." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition 20% in control group and 33% in yoga group at 16 weeks; 2 withdrawals linked to yoga intervention. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. |
| Group similarity at baseline | Unclear risk | Quote: "Higher functional ability on the BPSES [Back Pain Self‐Efficacy Scale] (P=0.005), lower catastrophizing as a coping strategy (P=0.007), and less perceived disability (P=0.002) and harm (P=0.02) on the SOPA [Survey of Pain Attitudes] by the yoga group compared to the control group." |
| Co‐interventions | Low risk | No difference in medication use at baseline; drug use in yoga group reduced; postintervention assessment showed non‐significant differences in medical or non‐medical treatment, or lifestyle changes. |
| Compliance | Low risk | Quote: "Of the 20 subjects completing the yoga intervention [out of 30 randomized], an attendance rate of 91.9% was achieved for the 16‐week protocol." |
| ITT analysis | Unclear risk | No mention of ITT; non‐completers compared with completers. |
| Timing of outcome assessments | Low risk | Outcome assessment at set time points. |
| Other bias | Low risk | No other biases identified. |
Williams 2009.
| Study characteristics | ||
| Methods | Randomized controlled parallel‐group trial. | |
| Participants | 90 participants with chronic non‐specific LBP. Setting: setting not described. Yoga delivered in a yoga studio. Country: USA. Recruitment: self‐referral. Details of recruitment not described. Inclusion criteria: English‐speaking men and women aged 18–70 years with history of LBP and symptom duration > 3 months; lived within a 1‐hour drive of study site; insured by a participating provider; BMI < 37; able to get up and down from the floor and rise to a standing position without assistance. Back pain‐related eligibility criteria were a score 10–60 on the Oswestry Disability Index and score of 3–8 cm on VAS scale. Participants were required to agree not to participate in chiropractic, massage, Pilates, acupuncture, or any other yoga treatment during study. Participants were required to agree that if they were randomized to yoga therapy they would attend a minimum number of yoga classes and practice at home. Exclusion criteria: LBP attributable to spinal stenosis with pseudoclaudication, abdominal or spine tumors, spinal infection, osteoporosis with vertebral fractures, ankylosing spondylitis, spondylolisthesis with/without radiculopathy, structural kyphosis or scoliosis, radicular pain with weakness or loss of reflexes, failed back syndrome; presurgical candidates; pregnant; undergoing cancer treatment; had confirmed fibromyalgia, abdominal hernia, compromised cardiopulmonary system, major depression, widespread neurologic disorder, or substance abuse issues; currently involved in back‐related litigation or a workers' compensation case; had practiced yoga once per week for ≥ 3 months within the last year. Duration and follow‐up: interventions provided for 24 weeks and additional follow‐up at 24 weeks after end of treatment (48 weeks after randomization). |
|
| Interventions |
Yoga group: (n = 43) 2 × 90‐min iyengar yoga classes per week for 24 weeks. Home practice: participants directed to practice 30 minutes of yoga at home on non‐class days and were supplied with props, a DVD, and an iyengar yoga instruction manual with photographs and instructions. Self‐directed standard medical care group: (n = 47) usual medical care. Common interventions: none. Co‐interventions: participants were only eligible for the study if they agreed to forgo chiropractic, massage, Pilates, acupuncture, or any other yoga treatment during study. |
|
| Outcomes | Back‐specific function (Oswestry Disability Index) at 12, 24, and 48 weeks. Back pain (VAS 0–100) at 12, 24, and 48 weeks. Depression (Beck Depression Inventory) at 12, 24, and 48 weeks. Other outcomes collected: self‐reported medication usage. |
|
| Notes | Adverse events: 1 adverse event reported during 6‐month follow‐up in association with physical therapy, not the yoga intervention. Unclear which group this adverse event occurred in. Figure 1 of publication also showed that 1 yoga participant discontinued because yoga exacerbated LBP. Measurement of expectations or treatment preferences at baseline: in Table 3 of publication the mean of treatment expectancy for yoga on an 11‐point scale was 7.8 (SEM 0.23) for the yoga group and 8.1 (SEM 0.21) for the standard medical care group, and the mean of treatment expectancy for standard medical care were 4.8 (SEM 0.32) for the yoga group and 4.7 (SEM 0.24) for the standard medical group (all scores were prerandomization but postrandomization scores were also given). The study authors reported that (quote) "dropouts had lower post randomization expectation for [standard medical care] treatment (P= 0.016) than completers." Note: 12 yoga participants and 4 standard medical care participants dropped out. Funding: US National Institutes of Health. Quotes: "Federal funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript." "Supported by the National Institutes of Health's National Center for Complementary and Alternative Medicine (NIH‐NCCAM), grant (no.1 R21 AT001679‐01A2)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random sequence generation methods not reported; 3 of those randomized declined and were replaced. |
| Allocation concealment (selection bias) | Unclear risk | Eligible participants given envelopes with allocation but unclear who prepared these, who gave them to participants, and whether the envelopes were sealed and opaque. |
| Blinding of participants | High risk | No blinding as comparison was standard medical care; outcome measures based on self‐assessment. |
| Blinding of personnel/providers | High risk | No blinding. |
| Blinding of outcome assessors | High risk | Participants completed "assessment instruments with a research assistant blinded to the participants' group assignment." However, participants were not blinded, and outcomes were self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Missing outcome data were high in yoga group (20% at 12 weeks and 28% at 24 weeks) but low in usual care group (4% at 12 weeks and 9% at 24 weeks). |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. |
| Group similarity at baseline | Unclear risk | Groups were similar on indicators other than duration of LBP (control group had longer duration of LBP). |
| Co‐interventions | Low risk | Co‐interventions were allowed and there were no statistically significant differences between groups in use of medications at baseline. |
| Compliance | Low risk | Quote: "On average, yoga completers (n=31 [of 43 randomized]) attended 42.5 ± 0.4 of 48 classes (88.5%)…" |
| ITT analysis | Low risk | Quote: "For intention‐to‐treat analyses, missing baseline data were replaced by group means while missing data at 12 and 24 weeks were replaced using the last observation carried forward." |
| Timing of outcome assessments | Low risk | Outcome assessment at set time points. |
| Other bias | Low risk | No other biases identified. |
BMI: body mass index; CES: Center for Epidemiologic Studies; DVPRS: Defense and Veterans Pain Rating Scale; EQ‐5D: EuroQol‐5D; GP: general practitioner; ITT: intention to treat; LBP: low back pain; LOCF: last observation carried forward; min: minute; n: number; NIH: National Institutes of Health; PANAS‐PA: Positive and Negative Affect Schedule‐Positive Affect; PANAS‐NA: Positive and Negative Affect Schedule‐Negative Affect; PROMIS‐29: 29‐item Patient‐Reported Outcomes Measurement Information System; RMDQ: Roland‐Morris Disability Questionnaire; SEM: standardized error of the mean; SF‐12: 12‐item Short Form; SF‐36: 36‐item Short Form; STAI: State‐Trait Anxiety Inventory; STAIS: State‐Trait Anxiety Inventory – State Anxiety; STAIT: State‐Trait Anxiety Inventory – Trait Anxiety; VA: Veterans Affairs; VAS: visual analog scale; WHOQOL‐BREF: World Health Organization Quality of Life – Brief Questionnaire.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Anon 2006 | Not an original study report. |
| Anon 2009 | Not an original study report. |
| Anon 2017 | Not an original study report. |
| Biggs 2012 | Participants appeared to have a mix of subacute and chronic low back pain, numbers unclear; study author did not respond to request for clarification after several e‐mail attempts to contact author and institution. Wrong study population. |
| Bindal 2007 | Participants had back pain but type and duration was unclear; study author did not respond to request for clarification. Wrong study population. |
| Borg‐Olivier 2005 | Not an original study report. |
| CTRI/2012/11/003094 | Wrong study population. |
| CTRI/2017/02/007783 | Wrong intervention. |
| CTRI/2018/01/011098 | Wrong intervention. |
| De Giorgio 2018 | Wrong comparator (both study groups assigned to yoga). |
| Ford 2017 | Not an original study report. |
| Graves 2004 | Not an original study report. |
| Groessl 2012 | Not a randomized controlled trial. |
| Groessl 2021 | Wrong comparison. |
| Haldavnekar 2014 | Wrong comparison. |
| Hartfiel 2012 | Wrong study population. |
| Holden 2016 | Wrong patient population (pregnant women). |
| Horng 2006 | Not an original study report. |
| Jacob 2017 | Wrong study design (not randomized). |
| Kim 2014 | Several attempts to contact multiple authors to clarify study population were unsuccessful. Unable to establish eligible study population. |
| Kumar 2011 | Contacted multiple times but was unable to clarify study population. |
| Lee 2014 | Not a randomized controlled trial. |
| Manik 2017 | Wrong study population. |
| Michalsen 2012 | Participants had back pain but type and duration was unclear; study author did not respond to request for clarification. Wrong study population. |
| Monro 2015 | Wrong study population. |
| Namdar 2021 | Wrong patient population (pregnant women, not chronic low back pain) |
| NCT02806323 | Wrong study design (no comparison group). |
| NCT03324659 | Wrong intervention. |
| NCT03504085 | Wrong comparator (both study groups assigned to yoga). |
| NCT03840304 | Wrong population. |
| NCT04074109 | Wrong comparator. |
| NCT04089618 | Wrong intervention. |
| NCT04113460 | Wrong patient population. |
| NCT04281238 | Wrong patient population. |
| NCT04296344 | Wrong study design. |
| NCT04773743 | Wrong study design. |
| Patil 2015 | Not a randomized controlled trial. |
| Pushpika Attanayake 2010 | Participants had back pain but type and duration was unclear; study author did not respond to requests for clarification. Wrong study population. |
| Sakuma 2012 | Participants had back pain but type and duration was unclear; multiple attempts to contact study authors for clarification were unsuccessful. Wrong study population. |
| Saper 2013 | Wrong comparison. |
| Schmid 2019 | Wrong patient population. |
| Selfridge 2012 | Not an original study report. |
| Sharma 2019 | Wrong patient population. |
| Telles 2009 | Wrong study population. |
| Telles 2016 | Wrong study population. |
| Uebelacker 2019 | Wrong patient population. |
| Whitehead 2018 | Not an original study report. |
Characteristics of studies awaiting classification [ordered by study ID]
CTRI/2018/01/011243.
| Methods | RCT. |
| Participants | Chronic LBP. |
| Interventions | Yoga‐based advanced relaxation technique vs walking. |
| Outcomes | Disability (Oswestry Low Back Pain Disability Questionnaire); behavioral response (Sustained Attention to Response Task); quality of life; intensity of pain using VAS. |
| Notes | Based on timing described in study registration this trial should be completed. However, it is unclear based on information in trial registration whether the yoga‐based program should be classified as yoga, and we are attempting to contact the study investigator for further information. |
Hartfiel 2017.
| Methods | RCT. |
| Participants | Participants with and without back pain. |
| Interventions | Yoga vs usual care. |
| Outcomes | Disability (Roland‐Morris Disability Questionnaire) and the Keele STarT Back Screening Tool. |
| Notes | Unclear from publication whether the study population is eligible. We are attempting to contact the study authors for further information. |
IRCT20150531022498N27.
| Methods | RCT. |
| Participants | Women with chronic mechanical LBP. |
| Interventions | Yoga vs Pilates exercise training. |
| Outcomes | Physical fitness, LBP, functional disability, quality of life, body composition. |
| Notes | According to the trial registration, ethics approval was obtained in 2017 and the trial was retrospectively registered in 2018; therefore, it is likely that this trial has been completed. We are seeking any publications to verify eligibility. |
Krishna 2020.
| Methods | RCT. |
| Participants | Men aged 30–50 years diagnosed by a physician as having LBP for > 3 months. |
| Interventions | Yoga vs usual care. |
| Outcomes | Behavioral response (Sustained Attention to Response Task) and disability (Oswestry Low Back Pain Disability Questionnaire). |
| Notes | Full publication retrieved August 2021. Will assess at next review update. |
Krokhmal 2017.
| Methods | Unclear. |
| Participants | Chronic non‐specific lower back pain. |
| Interventions | Yoga vs usual care. |
| Outcomes | Pain, anxiety, depression, sleep disturbances. |
| Notes | Study reported in abstract format and eligibility of study is not clear. Seeking full publication for assessment of eligibility. |
Lalkate 2020.
| Methods | RCT. |
| Participants | Adults aged 25–45 years with mechanical LBP for > 7 weeks. |
| Interventions | Yoga vs physiotherapy. |
| Outcomes | Numerical pain rating scale, lumbar range of flexion by Modified Schober's test, transversus abdominis endurance by prone test with pressure biofeedback, disability level by Modified Oswestry Disability Index. |
| Notes | Attempting to contact authors to determine eligibility. |
Michalson 2021.
| Methods | RCT. |
| Participants | Chronic LBP. |
| Interventions | Yoga vs eurythmy therapy vs physiotherapeutic exercise. |
| Outcomes | Disability (Roland‐Morris Disability Questionnaire Score), intensity of pain by VAS, quality of life (Brief Multidimensional Life Satisfaction Scale, Perceived Stress Scale, Inner Correspondence with the Practices questionnaire, Freiburg Mindfulness Questionnaire, General Self‐Efficacy Scale, self‐regulation questionnaire, Internal Coherence Scale), pain diary (registering the need of analgesic medication), and questionnaire on the participants' expectations that the interventions will be effective in reducing pain and how strong this reduction might be. |
| Notes | An abstract has been published without outcome data. Full publication retrieved August 2021. Will assess at next review update. |
NCT02552992.
| Methods | RCT. |
| Participants | Adults with chronic LBP lasting > 6 months. |
| Interventions | Yoga vs self‐directed mind body education. |
| Outcomes | Primary outcome is back‐related function. |
| Notes | According to trial registration (NCT02552992) the study began in 2015 and the estimated completion date was December 2016; therefore, the study is most likely completed. We are attempting to contact the primary investigator for more information. |
NCT03432169.
| Methods | RCT. |
| Participants | Adult veterans aged 18–89 years, with lower back pain > 12 weeks. |
| Interventions | Yoga vs stretching. |
| Outcomes | Feasibility, PROMIS Global Health Scale, Pain, Engagement and General activity (a measure of pain). |
| Notes | Estimated completion date is December 2018 according to trial registration. Unclear whether the trial has been completed or not. We are attempting to contact the primary investigator. |
Rae 2020.
| Methods | RCT. |
| Participants | Veterans aged 18–89 years with lower back pain for > 12 weeks. |
| Interventions | Yoga vs stretching. |
| Outcomes | Pain (PEG), quality of life (PROMIS Global Health Survey), self‐efficacy (2‐item questionnaire), fear avoidance belief, catastrophizing, and social engagement in addition to qualitative clinician open ended questions postintervention. |
| Notes | Full publication retrieved August 2021. Will assess at next review update. |
Saper 2016.
| Methods | RCT. |
| Participants | Veteran of any branch of military service. |
| Interventions | Yoga vs education. |
| Outcomes | Primary outcomes are pain and back‐related function. |
| Notes | NCT02224183. LSW contacted Saper in October 2019 and verified that the study results have not yet been published and are not available. A further request in December 2021 produced no response to date. |
LBP: low back pain; PEG: pain intensity (P), enjoyment of life (E), general activity (G); PROMIS: Patient‐Reported Outcomes Measurement Information System; RCT: randomized controlled trial; VAS: visual analog scale.
Characteristics of ongoing studies [ordered by study ID]
CTRI/2018/09/015851.
| Study name | To study the effectiveness of yoga in back pain. |
| Methods | RCT. |
| Participants | Adults with chronic low back pain and mean back pain intensity ≥ 3 for the previous 7 days on a 0–10 numerical rating scale. |
| Interventions | Yoga vs conventional treatment including advice and regular walking. |
| Outcomes | Pain using Numerical Pain Rating score, disability using Oswestry Disability Index, lumbo pelvic rhythm, core muscle function by latency of core muscles tested by electromyography, morphology of multifidus by cross‐sectional area using magnetic resonance imaging, adverse events. |
| Starting date | 1 October 2018 according to trial registration; expected duration 2 years. |
| Contact information | Vandana Phadke; biomechanics.research@isiconline.org. |
| Notes | Official title: 'To study the effectiveness of yoga postures in the management of chronic non specific low back pain.' |
CTRI/2018/10/016132.
| Study name | A study to compare the effect of yoga and back school exercise for the treatment of low back pain in school teachers. |
| Methods | RCT. |
| Participants | Adults aged 25–50 years, with back pain ≥ 3 months of duration. |
| Interventions | Yoga vs back school vs control. |
| Outcomes | Numerical pain rating scale 0–10, disability (Roland‐Morris Disability Questionnaire), and trunk flexion range of motion. |
| Starting date | 3 November 2018 per trial registration. Expected completion date not given. |
| Contact information | Swati Dhrangu; sdhrangu248@rku.ac.in. |
| Notes | Official title: 'Effectiveness of back school exercise versus yogasana among school teachers with chronic low back pain: a randomized controlled trial.' |
CTRI/2020/04/024951.
| Study name | Yoga therapy for management of chronic low back pain. |
| Methods | RCT. |
| Participants | Adults indicative of low back pain with or without leg pain for > 3 months. |
| Interventions | Yoga vs usual care. |
| Outcomes | Functional disability (Modified Oswestry Disability Index); pain (verbal numeric rating scale, Douleur neuropathic‐4 questionnaire, and PCS), mental health (HADS); quality of life (EuroQol), fear of movement (i.e. kinesiophobia) using TAMPA Scale and Patient Global Impression Clinical Improvement to measure of the overall clinical benefit from the treatment; potential pain biomarkers. |
| Starting date | Not yet recruiting. |
| Contact information | Babita Ghai or Spoorthi Poojari; ghaibabita1@gmail.com. |
| Notes | Official title: 'Effectiveness of integrated approach of yoga therapy (IAYT) versus usual care in management on chronic low back pain patients: a randomized controlled pilot study.' |
CTRI/2020/05/025396.
| Study name | Yoga therapy versus usual care for chronic low back pain. |
| Methods | RCT. |
| Participants | Adults indicative of low back pain with or without leg pain for more than 3 months. |
| Interventions | Yoga vs usual care. |
| Outcomes | Functional disability (using MODQ) and pain (using verbal numeric rating scale), pain biomarkers, mental health (using HADS), and quality of life (using EuroQol), pain catastrophizing (using PCS) and kinesiophobia (using TAMPA Scale). |
| Starting date | Not yet recruiting. |
| Contact information | Babita Ghai; ghaibabita1@gmail.com. |
| Notes | Official title: 'Effectiveness of integrated approach of yoga therapy (IAYT) versus usual care in management on chronic low back pain patients: a randomized controlled trial.' |
CTRI/2020/12/029944.
| Study name | Effectiveness of yoga and mindfulness meditation on low back pain in computer users. |
| Methods | RCT. |
| Participants | Non‐specific low back pain persisting > 12 weeks. |
| Interventions | Yoga and mindfulness vs physical therapy. |
| Outcomes | Disability (Oswestry Disability Index); pain (Numerical Rating Scale); quality of life (Depression Anxiety Stress Scale; World Health Organization Quality of Life Scale Brief Questionnaire; Mindful Attention Awareness Scale; The Five Facet Mindfulness Questionnaire); objective measures of spinal mobility (Sit and Reach, Straight Leg Raising test, spinal flexibility using a dial type goniometer); psychological variables (Pittsburgh Sleep Quality Index, Locus of Control; resilience Scale, Fear‐Avoidance Beliefs Questionnaire). |
| Starting date | Date of first enrollment: 25 December 2020; not yet recruiting. |
| Contact information | Satyaprakash Purohit; satyaprakash.purohit@svyasa.edu.in. |
| Notes | Official title: 'Effect of yoga and mindfulness meditation on chronic low back pain in computer users: a randomized control trial.' |
CTRI/2021/03/031733.
| Study name | Effectiveness of yoga therapy versus Pilates exercises in school teachers with non‐specific chronic low back pain. |
| Methods | RCT. |
| Participants | Male school teachers aged 30–60 years, chronic (> 3 months) LBP and 4–8 pain intensity using VAS. |
| Interventions | Yoga vs Pilates. |
| Outcomes | VAS, range of motion, functional disability, muscle cross‐sectional area, quality of life. |
| Starting date | Date of first enrollment: 10 March 2021. |
| Contact information | Gopal Nambi; physio_gopal@rediffmail.com. |
| Notes | Official title: 'Clinical outcomes and psychosocial effectiveness of yoga therapy versus Pilates exercises in school teachers with non‐specific chronic low back pain: a randomized controlled trial.' |
CTRI/2021/03/031735.
| Study name | An additional effect of yoga therapy in bank employees with chronic low back pain. |
| Methods | RCT. |
| Participants | Male bank employees aged 30–60 years, chronic (> 3 months) LBP and 4–8 pain intensity using VAS. |
| Interventions | Yoga vs global postural re‐education exercises. |
| Outcomes | VAS, range of motion, functional disability, muscle cross‐sectional area, quality of life. |
| Starting date | Date of first enrolment: 10 March 2021. |
| Contact information | Gopal Nambi; physio_gopal@rediffmail.com. |
| Notes | Official title: 'An additional effect of yoga therapy with global postural reeducation exercises in bank employees with non‐specific chronic low back pain – a randomized controlled trial.' |
CTRI/2021/03/031736.
| Study name | Effects of yoga therapy in university professors with chronic low back pain. |
| Methods | RCT. |
| Participants | Male university professors aged 30–60 years, chronic (> 3 months) LBP and 4–8 pain intensity using VAS. |
| Interventions | Yoga vs proprioceptive neuromuscular facilitation exercise. |
| Outcomes | VAS, range of motion, functional disability, muscle cross‐sectional area, quality of life. |
| Starting date | Date of first enrolment: 10 March 2021. |
| Contact information | Gopal Nambi; physio_gopal@rediffmail.com. |
| Notes | Official title: 'Comparative effects of yoga therapy and proprioceptive neuromuscular training on clinical outcomes and psychosocial effects in university professors with chronic low back pain: a randomized controlled trial.' |
NCT03816007.
| Study name | Yoga and mantram for chronic pain and PTSD. |
| Methods | RCT. |
| Participants | People with PTSD and chronic low back pain or chronic neck pain, or both. |
| Interventions | Yoga and mantram repetition vs veteran calm (an enhanced relaxation program). |
| Outcomes | Back function, pain, PTSD, insomnia, quality of life, medication use. |
| Starting date | Estimated start date 1 December 2019 per trial registration. |
| Contact information | Erik J Groessl, PhD BA BS; Erik.Groessl@va.gov. |
| Notes | Official title: 'An enhanced mind–body intervention to reduce disability and pain in veterans with PTSD.' Estimated study completion date 31 May 2021 per trial registration. |
NCT04000685.
| Study name | The effects of different exercise approaches in patients with chronic low back pain. |
| Methods | RCT. |
| Participants | People with chronic low back pain. |
| Interventions | Yoga exercise program vs spinal stabilization exercise program vs aerobic walking program. |
| Outcomes | Pain, function, quality of life, gait, metabolic capacity, cognitive level, alexithymia, kinesiophobia, back awareness. |
| Starting date | 30 December 2019 per trial registration. |
| Contact information | Müzeyyen Öz, MSc; oz_muzeyyen@hotmail.com; Özlem Ülger; professor ozlemulger@yahoo.com. |
| Notes | Estimated study completion date: September 2021 per trial registration. |
NCT04142177.
| Study name | Sequential and Comparative Evaluation of Pain Treatment Effectiveness Response (SCEPTER). |
| Methods | RCT. |
| Participants | Chronic low back pain current and present for ≥ 6 months. |
| Interventions | Yoga vs Internet‐based pain self‐management program vs enhanced physical therapy vs continued care and active monitoring vs spinal manipulation therapy. |
| Outcomes | Pain (Brief Pain Inventory Interference scale). |
| Starting date | Estimated start date: 4 October 2021. |
| Contact information | Colleen M Fitzsimmons; Colleen.Fitzsimmons@va.gov. |
| Notes |
NCT04203888.
| Study name | Re‐engineering precision therapeutics through N‐of‐1 trials. |
| Methods | RCT. |
| Participants | Chronic low back pain. |
| Interventions | Swedish massage vs yoga vs usual care. |
| Outcomes | System usability score, participant satisfaction, pain, fatigue, stress, medication use, daily steps, nightly sleep. |
| Starting date | 20 November 2019 per trial registration. |
| Contact information | Karina W Davidson, PhD, MASc Northwell Health. |
| Notes | Estimated study completion date: September 2020 per trial registration. |
NCT04270617.
| Study name | A prospective, randomized‐controlled study to evaluate the effect of a standardized yoga practice on chronic back pain. |
| Methods | RCT. |
| Participants | People with chronic back pain. |
| Interventions | Yoga program vs usual care. |
| Outcomes | Disability (Oswestry Disability Index), quality of life (36‐item Short Form, VAS). |
| Starting date | 1 December 2019 per trial registration. |
| Contact information | Erich Anderer, MD; erich.anderer@nyulangone.org. |
| Notes | Estimated study completion date: January 2023 per trial registration. |
NCT04721639.
| Study name | To observe the effect of sphinx pose (Salamba Bhujangasana) among health care providers with chronic low back pain. |
| Methods | RCT. |
| Participants | Adults aged 25–45 years, score ≥ 2 for pain intensity in last week, on Numerical Pain Rating scale (0–10). |
| Interventions | Sphinx yoga therapy vs usual care. |
| Outcomes | Extent of disability, pain score, substance P, beta‐endorphins, cortisol, quality of life score, physical stress – stress score. |
| Starting date | Estimated start date: 30 January 2021. |
| Contact information | Yusra Saleem, MSc; yusrasaleem18@gmail.com; Sadaf Ahmed, PhD; sadafa@uok.edu.pk. |
| Notes |
NCT04723225.
| Study name | Effectiveness of cat‐cow yoga in managing chronic low back pain. |
| Methods | RCT. |
| Participants | Adults aged 25–45 years with low back pain constantly or on most days for the last 3 months. |
| Interventions | Cat‐cow yoga vs usual care. |
| Outcomes | Pain score, extent of disability, substance P, beta‐endorphins, stress score, cortisol, quality of life score. |
| Starting date | Estimated start date: 30 January 2021. |
| Contact information | Farah Batool MSc; farahbatool97@gmail.com; Sadaf Ahmed PhD; Sadafa@uok.edu.pk. |
| Notes | Official title: 'To observe the effectiveness of cat‐cow yoga in the pain management of chronic low back pain in health care professionals.' |
NCT04787094.
| Study name | The effect of yoga and stabilization exercises in individuals with chronic low back pain. |
| Methods | Cross‐over RCT. |
| Participants | Adults aged 25–65 years with chronic non‐specific low back pain diagnosis, pain for ≥ 12 weeks. |
| Interventions | Yoga vs spinal stabilization exercises. |
| Outcomes | Pain intensity, disability severity, functional performance, deep muscle activation, kinesiophobia, sleep quality, metabolic capacity. |
| Starting date | Actual start date: 1 December 2020. |
| Contact information | Ozlem Ulger, Professor, Physiotherapist, Hacettepe University. |
| Notes | Official title: 'The effect of yoga and stabilization exercises on pain, functional status, metabolic capacity and sleep quality in individuals with chronic low back pain: a randomized, crossover study.' |
NCT04824547.
| Study name | Evaluation of long‐term continuity of exercises in low back pain individuals. |
| Methods | RCT. |
| Participants | Adults aged 18–60 years with low back pain for ≥3 months, VAS rating ≥ 3. |
| Interventions | Yoga vs stabilization exercise. |
| Outcomes | Changes in pain severity, functional status, quality of life, exercise compliance, gait. |
| Starting date | Estimated start date: 30 May 2021. |
| Contact information | Muzeyyen OZ, MSc; oz_muzeyyen@hotmail.com. |
| Notes | Official title: Bel Ağrılı Bireylerde Egzersizlerin Uzun Dönem Devamlılığının Değerlendirilmesi. |
PACTR202001829834757.
| Study name | Physical activity effectiveness for chronic non‐specific low back pain treatment in Burundi. |
| Methods | RCT. |
| Participants | Adults aged 18–65 years with chronic (≥ 3 months) or recurrent (≥ 3 episodes in previous 12 months) LBP of mechanical origin. |
| Interventions | Group‐based yoga plus graded walking vs individual physical therapy. |
| Outcomes | Activity limitations (Roland‐Morris Disability Questionnaire), pain intensity (numerical rating scale), muscular endurance (Shirado test, Sorensen test), depression (Beck Depression Inventory), patient beliefs (Fear‐Avoidance Beliefs Questionnaire), physical fitness (Borg Rating of Perceived Exertion scale, resting heart rate), self‐perception of performance (Canadian occupational performance measure), participation (5‐Item Pain Disability Index). |
| Starting date | 17 February 2020. |
| Contact information | Principle investigator: Ildephonse Nduwimana; ilwimana@gmail.com; scientific inquiries: Jean Louis Thonnard; jeanLouis.Thonnard@uclouvain.be; public inquiries: Oyene Kossi; oyene.kossi@gmail.com. |
| Notes | Official title: 'Physical activity in chronic low back pain: a randomized controlled clinical trial comparing group‐based walking plus yoga versus individual physical therapy.' |
HADS: Hospital Anxiety and Depression Scale; MODQ: Modified Oswestry Disability Questionnaire; PCS: Physical Component scale; PTSD: post‐traumatic stress disorder; RCT: randomized controlled trial.
Differences between protocol and review
Difference between the previous review and this update
We added yoga versus sham yoga as the primary comparison based upon Cochrane Back and Neck requirements issued in 2022.
In the first version of the review we used the risk difference (RD) to report adverse events. In the current version, we use the RR and additionally express the absolute and relative percent differences and NNTH.
In the first version of the review, we conducted generic inverse variance sensitivity analyses using mean differences (MDs) and confidence intervals (CIs), when such data were available, to test the robustness of analyses carried out using endpoint data extracted from figures and standard deviations (SDs) estimated from baseline SDs. In the first version of the review, this was a useful comparison when we had only two studies in an analysis, and one of those studies relied upon data extracted from figures and SDs estimated from baseline SDs. In the original review, there was no difference between primary and sensitivity analyses, and in the update, those same analyses have more studies, and the importance of the single study with figure‐extracted data is smaller. Therefore, we omitted this sensitivity analysis from this version.
In the first version of the review, we used both the SMD and the original scale to report the MD for results for each result reported in the summary of findings tables, using the control arm SD from a representative study to re‐express the SMD in MD units of a familiar scale for all treatment effects that were based on analyses of different scales. In the update, we used a weighted mean of the SDs from both arms of all studies using a familiar scale in an analysis to re‐express the SMD in MD units, and we did this for each result reported in the results in addition to the results reported in the summary of findings tables.
In the first version of the review, we prepared summary of findings tables for the primary outcomes and adverse events at all time points. Current guidance requires us to choose only the most important comparisons for summary of findings tables and we chose yoga versus no exercise and yoga versus other exercise (not including the intensive residential comparison). We are also required to select the single most important time point for the summary of findings tables and chose the short–intermediate term (three to four months) as we believe it is the earliest clinically significant time point for observing outcomes in people with a chronic condition. However, we reported the summary of adverse events as of the longest available time point from each study, as we wished to capture all such events.
In the first version of this review, we reported depression as one of the outcomes under quality of life but did not list it as a separate outcome in the methods. In this version we have explicitly added depression as an additional outcome.
CR D'Adamo left the review team and S Harbin joined the review team.
Contributions of authors
Study concept and design: LSW, NS, KP, SH.
Development of search strategy: SH.
Searching for studies: SH.
Study selection: LSW, NS, SH, RV.
Data extraction: LSW, NS, KP.
Data analysis: LSW.
Drafting the manuscript: LSW.
Providing final approval of the final version: all authors.
Sources of support
Internal sources
-
None, Other
No internal sources of support.
External sources
-
NIH National Center for Complementary and Integrative Medicine, R24 AT001293, USA
Research reported in this publication was supported by the National Center for Complementary and Integrative Health of the National Institutes of Health under award number R24 AT001293. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declarations of interest
LSW: none.
NS: none.
KP: none.
SH was Managing Editor of the Cochrane Back and Neck review group until April 2020. She was not involved in the editorial decisions for this review.
RV is a volunteer researcher with Yoga Sangeeta, a non‐profit organization that promotes music for meditation and healing.
BB: none.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Bramberg 2017 {published and unpublished data}
- Aboagye E, Karlsson ML, Hagberg J, Jensen I. Cost-effectiveness of early interventions for non-specific low back pain: a randomized controlled study investigating medical yoga, exercise therapy and self-care advice. Journal of Rehabilitation Medicine 2015;47(2):167-73. [DOI] [PubMed] [Google Scholar]
- Bramberg EB, Bergstrom G, Jensen I, Hagberg J, Kwak L. Effects of yoga, strength training and advice on back pain: a randomized controlled trial. BMC Musculoskeletal Disorders 2017;18(1):132. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01653782. Cost effectiveness of medical yoga therapy on low back pain (MYTH) [Cost effectiveness of early interventions for non-specific low back pain: a randomized controlled study investigating medical yoga, exercise therapy and evidence based advice]. clinicaltrials.gov/ct2/show/NCT01653782 (first received 31 July 2012).
Cox 2010 {published and unpublished data}
- Cox H, Tilbrook H, Aplin J, Semlyen A, Torgerson D, Trewhela A, et al. A randomised controlled trial of yoga for the treatment of chronic low back pain: results of a pilot study. Complementary Therapies in Clinical Practice 2010;16(4):187-93. [PMID: ] [DOI] [PubMed] [Google Scholar]
Demirel 2019 {published data only}
- Demirel A, Oz M, Ozel YA, Cetin H, Ulger O. Stabilization exercise versus yoga exercise in non-specific low back pain: pain, disability, quality of life, performance: a randomized controlled trial. Complementary Therapies in Clinical Practice 2019;35:102-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Galantino 2004 {published data only}
- Galantino ML, Bzdewka TM, Eissler-Russo JL, Holbrook ML, Mogck EP, Geigle P, et al. The impact of modified hatha yoga on chronic low back pain: a pilot study. Alternative Therapies in Health and Medicine 2004;10(2):56-9. [PMID: ] [PubMed] [Google Scholar]
Groessl 2017 {published and unpublished data}
- Groessl EJ, Liu L, Chang DG, Wetherell JL, Bormann JE, Atkinson JH, et al. Yoga for military veterans with chronic low back pain: a randomized clinical trial. American Journal of Preventive Medicine 2017;53(5):599-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groessl EJ, Liu L, Richard EL, Tally SR. Cost-effectiveness of yoga for chronic low back pain in veterans. Medical Care 2020;58(Suppl 2):S142-8. [DOI] [PubMed] [Google Scholar]
- Groessl EJ, Liu L, Schmalzl L, Chang DG, McCarthy A, Chun WI, et al. Secondary outcomes from a randomized controlled trial of yoga for veterans with chronic low-back pain. International Journal of Yoga Therapy 2020;30(1):69-76. [DOI: 10.17761/2020-D-19-00036] [PMID: ] [DOI] [PMC free article] [PubMed]
- Groessl EJ, Schmalzl L, Maiya M, Liu L, Goodman D, Chang DG, et al. Yoga for veterans with chronic low back pain: design and methods of a randomized clinical trial. Contemporary Clinical Trials 2016;48:110-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Hernandez R, McCarthy A, Casteel D, Groessl E, Hafey C. The association of intervention attendance with changes in pain severity in a clinical trial of yoga for veterans with CLBP. Global Advances in Health and Medicine 2021;10:45-6. [Google Scholar]
- Liu L, Schmalzl L, Groessl, EJ. A cost-effectiveness analysis of yoga for chronic low back pain. Global Advances in Health and Medicine 2018;7:1151. [Google Scholar]
- McCarthy A, Groessl E, Liu L. Sociodemographic analysis of yoga for chronic low back pain. Global Advances in Health and Medicine 2020;9:114. [Google Scholar]
- NCT02524158. Yoga therapy to improve function among veterans with chronic low back pain. clinicaltrials.gov/ct2/show/NCT02524158 (first received 10 August 2015).
Highland 2018 {published data only}
- Highland KB, Schoomaker A, Rojas W, Suen J, Ahmed A, Zhang Z, et al. Benefits of the restorative exercise and strength training for operational resilience and excellence yoga program for chronic low back pain in service members: a pilot randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2018;99(1):91-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Highland KB, Schoomaker A, Rojas W, Suen J, Ahmed A, Zhang Z, et al. Erratum: benefits of the restorative exercise and strength training for operational resilience and excellence yoga program for chronic low back pain in service members: a pilot randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2018;99(4):777. [PMID: ] [DOI] [PubMed] [Google Scholar]
Jacobs 2004 {published and unpublished data}
- Jacobs BP, Mehling W, Avins AI, Goldberg HA, Acree M, Lasater JH, et al. Erratum: feasibility of conducting a clinical trial on hatha yoga for chronic low back pain: methodological lessons. Alternative Therapies in Health and Medicine 2014;10(3):48. [PubMed] [Google Scholar]
- Jacobs BP, Mehling W, Avins AL, Goldberg HA, Acree M, Lasater JH, et al. Feasibility of conducting a clinical trial on hatha yoga for chronic low back pain: methodological lessons. Alternative Therapies in Health and Medicine 2004;10(2):80-3. [PMID: ] [PubMed] [Google Scholar]
Kuvacic 2018 {published data only}
- Kuvacic G, Fratini P, Padulo J, Antonio DI, De Giorgio A. Effectiveness of yoga and educational intervention on disability, anxiety, depression, and pain in people with CLBP: a randomized controlled trial. Complementary Therapies in Clinical Practice 2018;31:262-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nambi 2014 {published data only}
- Cho I, Jeon C, Lee S, Lee D, Hwangbo G. Effects of lumbar stabilization exercise on functional disability and lumbar lordosis angle in patients with chronic low back pain. Journal of Physical Therapy Science 2015;27(6):1983-5. [doi: 10.1589/jpts.27.1983] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inani SB, Selkar SP. Effect of core stabilization exercises versus conventional exercises on pain and functional status in patients with non-specific low back pain: a randomized clinical trial. Journal of Back and Musculoskeletal Rehabilitation 2013;26(1):37-43. [doi: 10.3233/BMR-2012-0348] [DOI] [PubMed] [Google Scholar]
- Nambi GS, Inbasekaran D, Khuman R, Devi S, Shanmugananth, Jagannathan K. Changes in pain intensity and health related quality of life with iyengar yoga in nonspecific chronic low back pain: a randomized controlled study. International Journal of Yoga 2014;7(1):48-53. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT03676062. The effect of yoga and stabilization exercise in patients with chronic low back pain [Kronik bel ağrılı bireylerde yoga ve spinal stabilizasyon egzersizlerinin ağrı, fonksiyon ve stres uzerine etkisinin karşılaştırılması]. clinicaltrials.gov/ct2/show/NCT03676062 (first received 28 September 2018).
- Shirado O, Doi T, Akai M, Hoshino Y, Fujino K, Hayashi K, et al. Multicenter randomized controlled trial to evaluate the effect of home-based exercise on patients with chronic low back pain: the Japan low back pain exercise therapy study. Spine 2010;35(17):E811-9. [doi: 10.1097/BRS.0b013e3181d7a4d2.] [DOI] [PubMed] [Google Scholar]
Neyaz 2019 {published and unpublished data}
- CTRI/2017/08/009572. Comparing effectiveness of yoga vs exercises for old low back pain [To compare the effectiveness of conventional therapeutic exercises with yoga for chronic nonspecific low back pain: a randomized comparative trial]. www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=176462017 (first received 31 August 2017).
- Neyaz O, Sumila L, Nanda S, Wadhwa S. Effectiveness of hatha yoga versus conventional therapeutic exercises for chronic nonspecific low-back pain. Journal of Alternative and Complementary Medicine 2019;25(9):938-45. [PMID: ] [DOI] [PubMed] [Google Scholar]
Patil 2018 {published data only}
- Patil NJ, Nagaratna R, Tekur P, Manohar PV, Bhargav H, Patil D. A randomized trial comparing effect of yoga and exercises on quality of life in among nursing population with chronic low back pain. International Journal of Yoga 2018;11(3):208-14. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Saper 2009 {published and unpublished data}
- Saper RB, Sherman KJ, Cullum-Dugan D, Davis RB, Phillips RS, Culpepper L. Yoga for chronic low back pain in a predominantly minority population: a pilot randomized controlled trial. Alternative Therapies in Health and Medicine 2009;15(6):18-27. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Saper 2017 {published data only}
- Berlowitz J, Hall DL, Joyce C, Fredman L, Sherman KJ, Saper RB, et al. Changes in perceived stress after yoga, physical therapy, and education interventions for chronic low back pain: a secondary analysis of a randomized controlled trial. Pain Medicine 2020;21(10):2529-37. [DOI: 10.1093/pm/pnaa150] [DOI] [PMC free article] [PubMed]
- Do D, Saper R. Impact of yoga on depression and anxiety. Journal of Alternative and Complementary Medicine 2014;20(5):A55. [Google Scholar]
- Egan S, Saper R. Predictors of adherence to treatment for chronic low back pain in a 12-week RCT comparing yoga, physical therapy, and education. Journal of Alternative and Complementary Medicine 2014;20(5):A56. [Google Scholar]
- Femia A, Lemaster C, Bertisch S, Saper R. Change in sleep quality in a randomized controlled trial of yoga, physical therapy, and education for low-income minorities with chronic low back pain. Journal of Alternative and Complementary Medicine 2016;22(6):A74-5. [Google Scholar]
- Joyce C, Roseen EJ, Keysor JJ, Gross KD, Culpepper L, Saper RB. Can yoga or physical therapy for chronic low back pain improve depression and anxiety among adults from a racially diverse, low-income community? A secondary analysis of a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2021;102(6):1049-58. [DOI: 10.1016/j.apmr.2021.01.072] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemaster C, Keosaian J, Dorman E, Paris R, Saper R. Qualitative study in a randomized trial comparing yoga, physical therapy, and education for low back pain in a predominantly minority population. Journal of Alternative and Complementary Medicine 2014;20(5):A59. [Google Scholar]
- Marshall A, Joyce CT, Tseng B, Gerlovin H, Yeh GY, Sherman KJ, et al. Changes in pain self-efficacy, coping skills and fear avoidance beliefs in a randomized controlled trial of yoga, physical therapy, and education for chronic low back pain. Pain Medicine 2021;23(4):834-43. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01343927. Yoga vs. physical therapy vs. education for chronic low back pain in minority populations (Back to Health). clinicaltrials.gov/ct2/show/NCT01343927 (first received 20 April 2011).
- Roseen E, Saper RB, Delitto A, Sherman HK, Gerlovin MA. Which chronic low back pain patients respond favorably to yoga? Responder analyses from a large randomized controlled trial. Global Advances in Health and Medicine 2018;7:144-5. [Google Scholar]
- Roseen EJ, Gerlovin H, Felson DT, Delitto A, Sherman KJ, Saper RB. Which chronic low back pain patients respond favorably to yoga, physical therapy, and a self-care Book? Responder analyses from a randomized controlled trial. Pain Medicine 2021;22(1):165-80. [DOI: 10.1093/pm/pnaa153] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roseen EJ, Gerlovin H, Femia A, Cho J, Bertisch S, Redline S, et al. Yoga, physical therapy, and back pain education for sleep quality in low-income racially diverse adults with chronic low back pain: a secondary analysis of a randomized controlled trial. Journal of General Internal Medicine 2020;35(1):167-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saper R, Herman P, Roseen E, Lemaster C. Yoga versus physical therapy versus education for chronic low back pain: a randomized non-inferiority trial in an underserved community-based population. Spine Journal 2016;16(Suppl 1):S291. [Google Scholar]
- Saper R, Weinberg J, Delitto A, Lemaster C, Herman P, Sherman K. Yoga versus physical therapy versus education for chronic low back pain: a randomized non-inferiority trial in an underserved community-based population. Journal of Alternative and Complementary Medicine 2016;22(6):A6. [Google Scholar]
- Saper R, Weinburg J, Delitto A, Lemaster C, Herman P, Sherman K. A randomized controlled trial comparing yoga, physical, therapy, and education for chronic low back pain in predominantly low income minorities. Integrative Medicine Research 2015;4(1):24. [Google Scholar]
- Saper RB, Lemaster C, Delitto A, Sherman KJ, Herman PM, Sadikova E, et al. Yoga, physical therapy, or education for chronic low back pain: a randomized noninferiority trial. Annals of Internal Medicine 2017;167(2):85-94. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saper RB, Roseen E, Femia A, Cho J, Bertisch S, Redline S. Yoga, physical therapy, and education for sleep quality in adults with chronic low back pain: a secondary analysis of a randomized controlled trial. Global Advances in Health and Medicine 2018;7:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saper RB, Sherman KJ, Delitto A, Herman PM, Stevans J, Paris R, et al. Yoga vs. physical therapy vs. education for chronic low back pain in predominantly minority populations: study protocol for a randomized controlled trial. Trials 2014;15:67. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sherman 2005 {published data only (unpublished sought but not used)}
- Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA. Comparing yoga, exercise, and a self-care book for chronic low back pain: a randomized, controlled trial. Annals of Internal Medicine 2005;143(12):849-56. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sherman 2011 {published data only}
- Sherman K, Wellman R, Cook A, Cherkin D. Mediators of the effects of yoga and stretching on chronic low back pain (cLBP) outcomes: results from the YES RCT. BMC Complementary and Alternative Medicine 2012;12(Suppl 1):O43. [Google Scholar]
- Sherman KJ, Cherkin DC, Cook AJ, Hawkes RJ, Deyo RA, Wellman R, et al. Comparison of yoga versus stretching for chronic low back pain: protocol for the Yoga Exercise Self-care (YES) trial. Trials 2010;11:36. [NCT00447668] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman KJ, Cherkin DC, Wellman RD, Cook AJ, Hawkes RJ, Delaney K, et al. A randomized trial comparing yoga, stretching, and a self-care book for chronic low back pain. Archives of Internal Medicine 2011;171(22):2019-26. [NCT00447668] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman KJ, Wellman RD, Cook AJ, Cherkin DC, Ceballos RM. Mediators of yoga and stretching for chronic low back pain. Evidence-based Complementary and Alternative Medicine 2013;2013:130818. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tekur 2008 {published data only}
- Tekur P, Chametcha S, Hongasandra RN, Raghuram N. Effect of yoga on quality of life of CLBP patients: a randomized control study. International Journal of Yoga 2010;3(1):10-7. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tekur P, Nagarathna R, Chametcha S, Hankey A, Nagendra HR. A comprehensive yoga programs improves pain, anxiety and depression in chronic low back pain patients more than exercise: an RCT. Complementary Therapies in Medicine 2012;20(3):107-18. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Tekur P, Singphow C, Nagendra HR, Raghuram N. Effect of short-term intensive yoga program on pain, functional disability and spinal flexibility in chronic low back pain: a randomized control study. Journal of Alternative and Complementary Medicine 2008;14(6):637-44. [PMID: ] [DOI] [PubMed] [Google Scholar]
Teut 2016 {published data only}
- NCT01303588. Yoga and qigong for elderly patients with chronic low back pain. clinicaltrials.gov/ct2/show/NCT01303588 (first received 24 February 2011).
- Teut M, Knilli J, Daus D, Roll S, Witt CM. Qigong or yoga versus no intervention in older adults with chronic low back pain: a randomized controlled trial. Journal of Pain 2016;17(7):796-805. [DOI] [PubMed] [Google Scholar]
Tilbrook 2011 {published and unpublished data}
- Chuang LH, Soares MO, Tilbrook H, Cox H, Hewitt CE, Aplin J, et al. A pragmatic multicentered randomized controlled trial of yoga for chronic low back pain: economic evaluation. Spine 2012;37(18):1593-601. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Cox H, Tilbrook H, Aplin J, Chuang LH, Hewitt C, Jayakody S, et al. A pragmatic multi-centred randomised controlled trial of yoga for chronic low back pain: trial protocol. Complementary Therapies in Clinical Practice 2010;16(2):76-80. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilbrook HE, Cox H, Hewitt CE, Kang'ombe AR, Chuang LH, Jayakody S, et al. Yoga for chronic low back pain: a randomized trial. Annals of Internal Medicine 2011;155(9):569-78. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Tilbrook HE, Hewitt CE, Aplin JD, Semlyen A, Trewhela A, Watt I, et al. Compliance effects in a randomised controlled trial of yoga for chronic low back pain: a methodological study. Physiotherapy 2014;100(3):256-62. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wattamwar 2013 {published data only (unpublished sought but not used)}
- Wattamwar RB, Nadkarni K. Effect of conventional occupational therapy and yoga in chronic low back pain. Indian Journal of Occupational Therapy 2013;45(3):13-20. [Google Scholar]
Williams 2005 {published data only}
- Williams KA, Petronis J, Smith D, Goodrich D, Wu J, Ravi N, et al. Effect of iyengar yoga therapy for chronic low back pain. Pain 2005;115(1-2):107-17. [PMID: ] [DOI] [PubMed] [Google Scholar]
Williams 2009 {published data only}
- Williams K, Abildso C, Steinberg L, Doyle E, Epstein B, Smith D, et al. Evaluation of the effectiveness and efficacy of iyengar yoga therapy on chronic low back pain. Spine 2009;34(19):2066-76. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Anon 2006 {published data only}
- Anon. Yoga effective for back pain. Journal of Family Practice 2006;55(3):186. [PMID: ] [PubMed] [Google Scholar]
Anon 2009 {published data only}
- Anon. Yoga better for chronic back pain and associated depression. Backcare Journal 2009;Winter:4. [Google Scholar]
Anon 2017 {published data only}
- Anon. Yoga eases moderate-to-severe chronic low back pain. Home Healthcare Now 2017;35(9):473-6. [Google Scholar]
Biggs 2012 {published data only (unpublished sought but not used)}
- Biggs C, Swait G, Hunnisett A, Cunliffe C. Chiropractic and yoga as an effective combination therapy for the treatment of low back pain: a randomised controlled trial. Chiropractic Evidence 2012;15(2):85. [DOI: 10.1016/j.clch.2012.06.008] [DOI] [Google Scholar]
Bindal 2007 {published data only (unpublished sought but not used)}
- Bindal VD, Ghai GD. Comparative efficacy of selected physiotherapy treatment and yogic asanas on low back pain among male physical education students. Journal of Exercise Science and Physiotherapy 2007;3(2):160-4. [Google Scholar]
Borg‐Olivier 2005 {published data only}
- Borg-Olivier S, Machliss B. Yoga for low-back pain. Complementary Medicine 2005;Nov/Dec:33-6. [Google Scholar]
CTRI/2012/11/003094 {published data only}
- CTRI/2012/11/003094. Yoga therapy for low back pain: different responses of disc extrusions and bulges. www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=5112 (first received 8 November 2012). [CTRI/2012/11/003094]
CTRI/2017/02/007783 {published data only}
- CTRI/2017/02/007783. Impact of two non medicinal therapies on low back pain among women employees of University [Correlates of impact of two intervention packages on occurrence and severity of low back pain among women employees of Panjab University Chandigarh: a randomized controlled trial – LBPCARE]. apps.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2017/02/007783 (first received 6 February 2019).
CTRI/2018/01/011098 {published data only}
- CTRI/2018/01/011098. To compare effect of two basti (medicated enema) with some herbal drug in the management of sciatica [A comparative clinical study on the effect of ksheerbala taila matra basti and erandmooladi yoga basti followed by rasna guggulu in the management of gridhrasi (sciatica)]. apps.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2018/01/011098 (first received 2 January 2018).
De Giorgio 2018 {published data only}
- De Giorgio A, Padulo J, Kuvačić G. Effectiveness of yoga combined with back school program on anxiety, kinesiophobia and pain in people with non-specific chronic low back pain: a prospective randomized trial. Muscles, Ligaments and Tendons Journal 2018;8(1):104-12. [Google Scholar]
Ford 2017 {published data only}
- Ford S. Yoga 'may' aid patients with chronic nonspecific lower back pain. Nursing Times 2017;13(1):1-3. [Google Scholar]
Graves 2004 {published data only}
- Graves N, Krepcho M, Mayo HG. Does yoga speed healing for patients with low back pain? Journal of Family Practice 2004;53(8):661-2. [PubMed] [Google Scholar]
Groessl 2012 {published data only}
- Groessl EJ, Weingart KR, Johnson N, Baxi S. The benefits of yoga for women veterans with chronic low back pain. Journal of Alternative and Complementary Medicine 2012;18(9):832-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Groessl 2021 {published data only}
- Groessl E, McCarthy A, Casteel D, McKinnon S. Feasibility of yoga for chronic low back and neck pain in military personnel. Global Advances in Health and Medicine 2021;10:16-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Haldavnekar 2014 {published data only}
- Haldavnekar RV, Tekur P, Nagarathna R, Nagendra HR. Effect of yogic colon cleansing (laghu sankhaprakshalana kriya) on pain, spinal flexibility, disability and state anxiety in chronic low back pain. International Journal of Yoga 2014;7(2):111-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hartfiel 2012 {published data only}
- Hartfiel N, Burton C, Rycroft-Malone J, Clarke G, Havenhand J, Khalsa SB, et al. Yoga for reducing perceived stress and back pain at work. Occupational Medicine (Oxford, England) 2012;62(8):606-12. [PMID: ] [DOI] [PubMed] [Google Scholar]
Holden 2016 {published data only}
- Holden S, Davis R, Manor B, Zera C, Yeh G. Yoga for pregnancy related back pain. Journal of Alternative and Complementary Medicine 2016;22(6):A772016. [Google Scholar]
- NCT03651232. Prenatal yoga for pregnancy related back pain. clinicaltrials.gov/ct2/show/NCT03651232 (first received 29 August 2018).
Horng 2006 {published data only}
- Horng MS. Yoga improves function in patients with chronic low back pain. Journal of Clinical Outcomes Management 2006;13(3):140-1. [Google Scholar]
Jacob 2017 {published data only}
- Jacob AM, Kathyayani BV. A study to assess the effectiveness of yogic postures on back pain among beedi rolling women in a selected rural area at Mangalore. International Journal of Nursing Education 2017;9(2):1-5. [Google Scholar]
Kim 2014 {published data only}
- Kim SS, Min WK, Kim JH, Lee BH. The effects of VR-based Wii Fit yoga on physical function in middle-aged female LBP patients. Journal of Physical Therapy Science 2014;26(4):549-52. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kumar 2011 {published data only}
- Kumar A, Telles S, Balkrishna A. A follow up study with back pain patients. Indian Journal of Physiology and Pharmacology 2011;55:70-1. [Google Scholar]
Lee 2014 {published data only}
- Lee M, Moon W, Kim J. Effect of yoga on pain, brain-derived neurotrophic factor, and serotonin in premenopausal women with chronic low back pain. Evidence-based Complementary and Alternative Medicine 2014;2014:203173. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Manik 2017 {published data only}
- Manik RK, Mahapatra AK, Gartia R, Bansal S, Patnaik A. Effect of selected yogic practices on pain and disability in patients with lumbar spondylitis. International Journal of Yoga 2017;10(2):81-7. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Michalsen 2012 {published data only}
- Michalsen A, Jeitler M, Brunnhuber S, Ludtke R, Bussing A, Musial F, et al. Iyengar yoga for distressed women: a 3-armed randomized controlled trial. Evidence-based Complementary and Alternative Medicine 2012;2012:408727. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Monro 2015 {published data only}
- Monro R, Bhardwaj AK, Gupta RK, Telles S, Allen B, Little P. Disc extrusions and bulges in nonspecific low back pain and sciatica: exploratory randomised controlled trial comparing yoga therapy and normal medical treatment. Journal of Back and Musculoskeletal Rehabilitation 2015;28(2):383-92. [PMID: ] [DOI] [PubMed] [Google Scholar]
Namdar 2021 {published data only}
- Namdar P, Hoseini N, Dehghankar L, Yekefallah L, Noorian S, Golestaneh F, et al. The effect of hatha yoga on low back pain and sleep quality on nulliparus pregnant women: a clinical trial study. Practising Midwife 2021;24(7):24-30. [Google Scholar]
NCT02806323 {published data only}
- NCT02806323. Individually tailored yoga program for the treatment of chronic neck and back pain [An individually tailored yoga program for the treatment of chronic neck and back pain in a low-income population: a feasibility study]. clinicaltrials.gov/ct2/show/NCT02806323 (first received 20 June 2016).
NCT03324659 {published data only}
- NCT03324659. Meditation and exercise to treat chronic back pain (MedExT) [Combined meditation and exercise as a treatment for patients with chronic back pain]. clinicaltrials.gov/ct2/show/NCT03324659 (first received 30 October 2017).
NCT03504085 {published data only}
- NCT03504085. Overcoming pain through yoga in the military (OPTYM) [Mind/body interventions for chronic low back and neck pain in military personnel]. clinicaltrials.gov/ct2/show/NCT03504085 (first received 20 April 2018).
NCT03840304 {published data only}
- NCT03840304. Effectiveness of Yoga@Work program [Effectiveness of Yoga@Work program on neck and shoulder pain in Information Technology (IT) employees]. clinicaltrials.gov/ct2/show/NCT03840304 (first received 15 February 2019).
NCT04074109 {published data only}
- NCT04074109. Feasibility of at-home telehealth yoga for treating chronic pain. clinicaltrials.gov/ct2/show/NCT04074109 (first received 29 August 2019).
NCT04089618 {published data only}
- NCT04089618. Meditation based lifestyle modification in chronic pain (MBLM-P). clinicaltrials.gov/ct2/show/nct04089618 (first received 13 September 2019).
NCT04113460 {published data only}
- NCT04113460. The effectiveness yoga@work among office workers with chronic nonspecific neck pain (CNNP) [The effectiveness yoga@work among office workers with chronic nonspecific neck pain (CNNP): a randomised controlled trial]. clinicaltrials.gov/ct2/show/NCT04113460 (first received 2 October 2019).
NCT04281238 {published data only}
- NCT04281238. The effects of yoga training in ankylosing spondylitis patients. clinicaltrials.gov/ct2/show/NCT04281238 (first received 24 February 2020).
NCT04296344 {published data only}
- NCT04296344. Group acupuncture therapy with modified yoga (GAPYOGA) [Group acupuncture therapy with modified yoga for chronic neck, low back and OA pain in safety net setting for an underserved population (GAPYOGA)]. clinicaltrials.gov/ct2/show/NCT04296344 (first received 5 March 2020).
NCT04773743 {published data only}
- NCT04773743. Remotely delivered yoga program for chronic low back pain. clinicaltrials.gov/show/NCT04773743 First received 26 February 2021.
Patil 2015 {published data only}
- Patil NJ, Nagarathna R, Tekur P, Patil DN, Nagendra HR, Subramanya P. Designing, validation, and feasibility of integrated yoga therapy module for chronic low back pain. International Journal of Yoga 2015;8(2):103-8. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pushpika Attanayake 2010 {published data only}
- Pushpika Attanayake AM, Somarathna KI, Vyas GH, Dash SC. Clinical evaluation of selected Yogic procedures in individuals with low back pain. AYU 2010;31(2):245-50. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sakuma 2012 {published data only}
- Sakuma Y, Sasaki-Otomaru A, Ishida S, Kanoya Y, Arakawa C, Mochizuki Y, et al. Effect of a home-based simple yoga program in child-care workers: a randomized controlled trial. Journal of Alternative and Complementary Medicine 2012;18(8):769-76. [PMID: ] [DOI] [PubMed] [Google Scholar]
Saper 2013 {published data only}
- Boah A, Kwong L, Weinberg J, Sherman K, Saper R. Characteristics of treatment adherence in low-income minority participants in a yoga dosing study for chronic low back pain. BMC Complementary and Alternative Medicine 2012;12(Suppl 1):116. [DOI: 10.1186/1472-6882-12-S1-P116] [DOI] [Google Scholar]
- Cerrada C, Weinberg J, Dresner D, Boah A, Sherman K, Saper R. Comparison of paper surveys and computer-assisted telephone interviews in a randomized controlled trial of yoga for low back pain. BMC Complementary and Alternative Medicine 2012;12(Suppl 1):370. [DOI: 10.1186/1472-6882-12-S1-P370] [DOI] [Google Scholar]
- Cerrada CJ, Weinberg J, Sherman KJ, Saper RB. Inter-method reliability of paper surveys and computer assisted telephone interviews in a randomized controlled trial of yoga for low back pain. BMC Research Notes 2014;7:227. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keosaian J, Dresner D, Cerrada C, Kwong L, Goodman N, Tam M, et al. Recruitment strategies for community-based yoga research in a predominant minority population. BMC Complementary and Alternative Medicine 2012;12(Suppl 1):183. [DOI: 10.1186/1472-6882-12-S1-P183] [DOI] [Google Scholar]
- Keosaian JE, Lemaster CM, Dresner D, Godersky ME, Paris R, Sherman KJ, et al. "We're all in this together": a qualitative study of predominantly low income minority participants in a yoga trial for chronic low back pain. Complementary Therapies in Medicine 2016;24:34-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saper R, Boah A, Keosaian J, Weinberg J, Sherman K. The Yoga Dosing Study: comparing once vs. twice per week yoga classes for chronic low back pain in predominantly low income minority populations. BMC Complementary and Alternative Medicine 2012;12(Suppl 1):O37. [DOI: 10.1186/1472-6882-12-S1-O37] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saper RB, Boah AR, Keosaian J, Cerrada C, Weinberg J, Sherman KJ. Comparing once- versus twice-weekly yoga classes for chronic low back pain in predominantly low income minorities: a randomized dosing trial. Evidence-based Complementary and Alternative Medicine 2013;2013:658030. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein KM, Weinberg J, Sherman KJ, Lemaster CM, Saper R. Participant characteristics associated with symptomatic improvement from yoga for chronic low back pain. Journal of Yoga & Physical Therapy 2014;4(1):151. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran HH, Weinberg J, Sherman KJ, Saper RB. Preference and expectation for treatment assignment in a randomized controlled trial of once- vs twice-weekly yoga for chronic low back pain. Global Advances in Health and Medicine 2015;4(1):34-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schmid 2019 {published data only}
- Schmid AA, Fruhauf CA, Sharp JL, Puymbroeck M, Bair MJ, Portz JD. Yoga for people with chronic pain in a community-based setting: a feasibility and pilot RCT. Journal of Evidence-Based Integrative Medicine 2019;24:2515690X19863763. [DOI: 10.1177/2515690X19863763] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmid AA, Puymbroeck M, Fruhauf CA, Bair MJ, Portz JD. Yoga improves occupational performance, depression, and daily activities for people with chronic pain. Work 2019;63(2):181-9. [DOI: 10.3233/WOR-192919] [PMID: ] [DOI] [PubMed] [Google Scholar]
Selfridge 2012 {published data only}
- Selfridge N. Yay yoga! More evidence for helping low back pain. Alternative Medicine Alert 2012;15(3):33-5. [Google Scholar]
Sharma 2019 {published data only}
- Sharma N, John PJ, Meghwal N, Owen A, Mishra V. Effect of yoga therapy on patients with chronic musculoskeletal pain: a prospective randomised wait list-controlled trial. Clinical Medicine 2019;19(3):s87. [Google Scholar]
Telles 2009 {published data only}
- Telles S, Dash M, Naveen KV. Effect of yoga on musculoskeletal discomfort and motor functions in professional computer users. Work 2009;33(3):297-306. [PMID: ] [DOI] [PubMed] [Google Scholar]
Telles 2016 {published data only}
- Telles S, Bhardwaj AK, Gupta RK, Sharma SK, Monro R, Balkrishna A. A randomized controlled trial to assess pain and magnetic resonance imaging-based (MRI-based) structural spine changes in low back pain patients after yoga practice. Medical Science Monitor 2016;22:3228-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telles S, Sharma SK, Gupta RK, Bhardwaj AK, Balkrishna A. Heart rate variability in chronic low back pain patients randomized to yoga or standard care. BMC Complementary and Alternative Medicine 2016;16(1):279. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Uebelacker 2019 {published data only}
- Uebelacker LA, Noppen D, Tremont G, Bailey G, Abrantes A, Stein M. A pilot study assessing acceptability and feasibility of hatha yoga for chronic pain in people receiving opioid agonist therapy for opioid use disorder. Journal of Substance Abuse Treatment 2019;105:19-27. [DOI: 10.1016/j.jsat.2019.07.015] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Whitehead 2018 {published data only}
- Whitehead PB. The effect of yoga on chronic nonspecific low back pain. American Journal of Nursing 2018;118(2):64. [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
CTRI/2018/01/011243 {published data only}
- CTRI/2018/01/011243. Effect of yoga based relaxation technique on sustained attention in chronic low back pain (CLBP) patients: a randomized controlled trial. apps.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2018/01/011243 (first received 10 January 2018).
Hartfiel 2017 {published data only}
- Hartfiel N, Clarke G, Havenhand J, Phillips C, Edwards RT. Cost-effectiveness of yoga for managing musculoskeletal conditions in the workplace. Occupational Medicine 2017;67:687–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
IRCT20150531022498N27 {published data only}
- IRCT20150531022498N27. Comparison of two methods of yoga and pilates exercise training in women with chronic mechanical low back pain [Comparison of two methods of yoga and pilates exercise training on pain and selected indicators of physical fitness, body composition and disability in women with chronic mechanical low back pain]. en.irct.ir/trial/34662 (first received 5 November 2018).
Krishna 2020 {published data only}
- Krishna D, Deepeshwar S, Devi B. Yoga-based relaxation technique facilitates sustained attention in patients with low back pain: a pilot study. Advances in Mind-Body Medicine 2020;34(3):11-7. [PMID: ] [PubMed] [Google Scholar]
Krokhmal 2017 {published data only}
- Krokhmal S, Vyshlova I, Karpov S. New approach of correction anxiety, depression and sleep disturbances in patients with chronic non-specific lower back pain. Journal of the Neurological Sciences 2017;381(Suppl 1):978. [Google Scholar]
Lalkate 2020 {published data only}
- Lalkate S, Agrawal R, Agashe GK. A comparative study effectiveness of conventional physiotherapy versus yoga therapy on pain, core muscle endurance, lumbar flexion range of motion and functional disability in patients with chronic mechanical low back pain. Indian Journal of Physiotherapy & Occupational Therapy 2020;14(4):177-82. [Google Scholar]
Michalson 2021 {published data only}
- Bussing A, Jung S, Lotzke D, Recchia DR, Robens S, Ostermann T, et al. Randomized clinical trial to treat patients with chronic back pain: a comparison of the efficacy of yoga, eurythmy therapy and standard physiotherapy. BMC Complementary and Alternative Medicine 2017;17(Suppl 1):P27. [Google Scholar]
- Bussing A, Poier D, Ostermann T, Kroz M, Michalsen A. Treatment of chronic lower back pain: study protocol of a comparative effectiveness study on yoga, eurythmy therapy, and physiotherapeutic exercises [2018]. Complementary Medicine Research 2018;25(1):24-9. [DOI] [PubMed] [Google Scholar]
- Michalsen A, Jeitler M, Kessler CS, Steckhan N, Robens S, Ostermann T, et al. Yoga, eurythmy therapy and standard physiotherapy (YES-Trial) for patients with chronic non-specific low back pain: a three-armed randomized controlled trial. Journal of Pain 2021;22(10):1233-45. [DOI: 10.1016/j.jpain.2021.03.154] [PMID: ] [DOI] [PubMed]
NCT02552992 {published data only}
- NCT02552992. Yoga for chronic low back pain and its mechanism of action: impact of strength and stretch (YoMA II). clinicaltrials.gov/ct2/show/NCT02552992 (first received 18 August 2015).
NCT03432169 {published data only}
- NCT03432169. Yoga vs stretching in veterans with chronic lower back pain: does mindfulness matter? clinicaltrials.gov/ct2/show/NCT03432169 (first received 14 February 2018).
Rae 2020 {published data only}
- Rae L, Dougherty P, Evertz N. Yoga vs stretching in veterans with chronic lower back pain and the role of mindfulness: a pilot randomized controlled trial. Journal of Chiropractic Medicine 2020;19(2):101-10. [DOI: 10.1016/j.jcm.2019.10.005] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Saper 2016 {published data only}
- Lemaster C, Plumb D, Wang S, Femia A, Elwy AR, Saper R. Recruitment of veterans for a yoga research study for chronic low back pain. Journal of Alternative and Complementary Medicine 22;6:A80. [Google Scholar]
- NCT02224183. Veterans Back to Health: a study comparing yoga and education for veterans with chronic low back pain. clinicaltrials.gov/ct2/show/NCT02224183 (first received: 20 August 2014).
- Saper RB, Lemaster CM, Elwy AR, Paris R, Herman PM, Plumb DN, et al. Yoga versus education for veterans with chronic low back pain: study protocol for a randomized controlled trial. Trials 2016;17(1):224. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
CTRI/2018/09/015851 {published data only}
- CTRI/2018/09/015851. To study the effectiveness of yoga in back pain [To study the effectiveness of yoga postures in the management of chronic non specific low back pain]. www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=28388 (first received 26 September 2018).
CTRI/2018/10/016132 {published data only}
- CTRI/2018/10/016132. A study to compare the effect of yoga and back school exercise for the treatment of low back pain in school teachers [Effectiveness of back school exercise versus yogasana among school teachers with chronic low back pain: a randomized controlled trial]. www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=28760 (first received 24 October 2018).
CTRI/2020/04/024951 {published data only}
- CTRI/2020/04/024951. Yoga therapy for management of chronic low back pain. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2020/04/024951 (first received 30 April 2020).
CTRI/2020/05/025396 {published data only}
- CTRI/2020/05/025396. Yoga therapy versus usual care for chronic low back pain. www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=42949 (first received 27 May 2020).
CTRI/2020/12/029944 {published data only}
- CTRI/2020/12/029944. Effectiveness of yoga and mindfulness meditation on low back pain in computer users. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2020/12/029944 (first received 21 December 2020).
CTRI/2021/03/031733 {published data only}
- CTRI/2021/03/031733. Effectiveness of yoga therapy versus Pilates exercises in school teachers with non-specific chronic low back pain. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2021/03/031733 (first received 5 March 2021).
CTRI/2021/03/031735 {published data only}
- CTRI/2021/03/031735. An additional effect of yoga therapy in bank employees with chronic low back pain. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2021/03/031735 (first received 5 March 2021).
CTRI/2021/03/031736 {published data only}
- CTRI/2021/03/031736. Effects of yoga therapy in university professors with chronic low back pain. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2021/03/031736 (first received 5 March 2021).
NCT03816007 {published data only}
- NCT03816007. Yoga and mantram for chronic pain and PTSD [An enhanced mind-body intervention to reduce disability and pain in veterans with PTSD]. clinicaltrials.gov/ct2/show/NCT03816007 (first received 25 January 2019).
NCT04000685 {published data only}
- NCT04000685. The effects of different exercise approaches in patients with chronic low back pain [The effects of different exercise approaches on physical and cognitive variables in patients with chronic low back pain]. clinicaltrials.gov/ct2/show/nct04000685 (first received 27 June 2019).
NCT04142177 {published data only}
- NCT04142177. Sequential and Comparative Evaluation of Pain Treatment Effectiveness Response (SCEPTER). clinicaltrials.gov/show/NCT04142177 (first received 29 October 2019).
NCT04203888 {published data only}
- NCT04203888. Personalized trial for chronic lower back pain [Re-engineering precision therapeutics through N-of-1 trials]. clinicaltrials.gov/ct2/show/NCT04203888 (first received 18 December 2019).
NCT04270617 {published data only}
- NCT04270617. The effect of yoga practice on chronic back pain [A prospective, randomized-controlled study to evaluate the effect of a standardized yoga practice on chronic back pain]. clinicaltrials.gov/ct2/show/NCT04270617 (first received 17 February 2020).
NCT04721639 {published data only}
- NCT04721639. To observe the effect of Sphinx Pose (Salamba Bhujangasana) among health care providers with chronic low back pain. clinicaltrials.gov/show/NCT04721639 (first received 22 January 2021).
NCT04723225 {published data only}
- NCT04723225. Effectiveness of cat-cow yoga in managing chronic low back pain. clinicaltrials.gov/show/NCT04723225 (first received 25 January 2021).
NCT04787094 {published data only}
- NCT04787094. The effect of yoga and stabilization exercises in individuals with chronic low back pain. clinicaltrials.gov/show/NCT04787094 (first received 8 March 2021).
NCT04824547 {published data only}
- NCT04824547. Evaluation of long-term continuity of exercises in low back pain individuals. clinicaltrials.gov/show/NCT04824547 (first received 1 April 2021).
PACTR202001829834757 {published data only}
- PACTR202001829834757. Physical activity effectiveness for chronic non-specific low back pain treatment in Burundi. pactr.samrc.ac.za/TrialDisplay.aspx?TrialID=9580 (first received 27 January 2020).
Additional references
Airaksinen 2006
- Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. European Spine Journal 2006;15(Suppl 2):S192-300. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Axén 2013
- Axén I, Leboeuf-Yde C. Trajectories of low back pain. Best Practice & Research. Clinical Rheumatology 2013;27(5):601-12. [PMID: ] [DOI] [PubMed] [Google Scholar]
Balague 2012
- Balague F, Mannion AF, Pellise F, Cedraschi C. Non-specific low back pain. Lancet 2012;379(9814):482-91. [PMID: ] [DOI] [PubMed] [Google Scholar]
Barnes 2008
- Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. National Health Statistics Reports 2008;(12):1-23. [PMID: ] [PubMed]
Birdee 2008
- Birdee GS, Legedza AT, Saper RB, Bertisch SM, Eisenberg DM, Phillips RS. Characteristics of yoga users: results of a national survey. Journal of General Internal Medicine 2008;23(10):1653-8. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Buchbinder 2012
- Buchbinder R, Underwood M. Prognosis in people with back pain. Canadian Medical Association Journal 2012;184(11):1229-30. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Burton 2002
- Burton K, Klaber-Moffett J, Main C, Roland M, Waddell G. The Back Book. Norwich (UK): TSO Publishers, 2002. [Google Scholar]
Bussing 2012
- Bussing A, Ostermann T, Ludtke R, Michalsen A. Effects of yoga interventions on pain and pain-associated disability: a meta-analysis. Journal of Pain 2012;13(1):1-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chou 2007
- Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr, Shekelle P, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Annals of Internal Medicine 2007;147(7):478-91. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chou 2010
- Chou R, Shekelle P. Will this patient develop persistent disabling low back pain? JAMA 2010;303(13):1295-302. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chou 2017
- Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al. Nonpharmacologic therapies for low back pain: a systematic review for an American College of Physicians Clinical Practice guideline. Annals of Internal Medicine 2017;166(7):493-505. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chung 2017
- Chung AS, Copay AG, Olmscheid N, Campbell D, Walker JB, Chutkan N. Minimum clinically important difference: current trends in the spine literature. Spine 2017;42(14):1096-105. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cohen 1988
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd edition. Hillsdale (NJ): Lawrence Erlbaum Associates, 1988. [Google Scholar]
Costa 2012
- Costa Ld, Maher CG, Hancock MJ, McAuley JH, Herbert RD, Costa LO. The prognosis of acute and persistent low-back pain: a meta-analysis. Canadian Medical Association Journal 2012;184(11):E613-24. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cramer 2013
- Cramer H, Lauche R, Haller H, Dobos G. A systematic review and meta-analysis of yoga for low back pain. Clinical Journal of Pain 2013;29(5):450-60. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cramer 2015a
- Cramer H, Lauche R, Langhorst J, Dobos G. Are Indian yoga trials more likely to be positive than those from other countries? A systematic review of randomized controlled trials. Contemporary Clinical Trials 2015;41:269-72. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cramer 2015b
- Cramer H, Ward L, Saper R, Fishbein D, Dobos G, Lauche R. The safety of yoga: a systematic review and meta-analysis of randomized controlled trials. American Journal of Epidemiology 2015;182(4):281-93. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cramer 2016a
- Cramer H, Ward L, Steel A, Lauche R, Dobos G, Zhang Y. Prevalence, patterns, and predictors of yoga use: results of a U.S. nationally representative survey. American Journal of Preventive Medicine 2016;50(2):230-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cramer 2016b
- Cramer H, Lauche R, Langhorst J, Dobos G. Is one yoga style better than another? A systematic review of associations of yoga style and conclusions in randomized yoga trials. Complementary Therapies in Medicine 2016;25:178-87. [PMID: ] [DOI] [PubMed] [Google Scholar]
Crow 2015
- Crow EM, Jeannot E, Trewhela A. Effectiveness of iyengar yoga in treating spinal (back and neck) pain: a systematic review. International Journal of Yoga 2015;8(1):3-14. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dagenais 2008
- Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine Journal 2008;8(1):8-20. [PMID: ] [DOI] [PubMed] [Google Scholar]
Daubenmier 2012
- Daubenmier J, Mehling W, Price C, Bartmess-Levasseur E, Acree M, Stewart A. Exploration of body awareness and pain and emotion regulation among yoga and meditation practitioners: does type of mind–body practice matter? BMC Complementary & Alternative Medicine 2012;12(Suppl 1):O54. [Google Scholar]
Deeks 2001
- Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Davey Smith G, Altman DG, editors(s). Systematic Reviews in Health Care: Meta-analysis in Context. London (UK): BMJ Publication Group, 2001. [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JP, Altman DG. Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Dutmer 2019
- Dutmer AL, Schiphorst Preuper HR, Soer R, Brouwer S, Bültmann U, Dijkstra PU, et al. Personal and societal impact of low back pain: the Groningen Spine Cohort. Spine 2019;44(24):E1443-51. [PMID: ] [DOI] [PubMed] [Google Scholar]
Foster 2018
- Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet 2018;391(10137):2368-83. [PMID: ] [DOI] [PubMed] [Google Scholar]
Furlan 2015a
- Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, et al. 2015 Updated method guideline for systematic reviews in the Cochrane Back and Neck Group. Spine 2015;40(21):1660-73. [PMID: ] [DOI] [PubMed] [Google Scholar]
Furlan 2015b
- Furlan AD, Giraldo M, Baskwill A, Irvin E, Imamura M. Massage for low-back pain. Cochrane Database of Systematic Reviews 2015, Issue 9. Art. No: CD001929. [DOI: 10.1002/14651858.CD001929.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
GBD 2017
- GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390(10100):1211-59. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
GBD 2020
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396(10258):1204-22. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Version accessed 25 October 2020. Hamilton (ON): McMaster University (developed by Evidence Prime, Inc.), 2020. Available at gradepro.org.
Guyatt 2011
- Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence – imprecision. Journal of Clinical Epidemiology 2011;64(12):1283-93. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hayden 2021
- Hayden JA, Ellis J, Ogilvie R, Malmivaara A, Tulder MW. Exercise therapy for chronic low back pain. Cochrane Database of Systematic Reviews 2021, Issue 9. Art. No: CD009790. [DOI: 10.1002/14651858.CD009790.pub2] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hayes 2010
- Hayes M, Chase S. Prescribing yoga. Primary Care: Clinics in Office Practice 2010;37:31-47. [DOI] [PubMed] [Google Scholar]
Heuch 2013
- Heuch I, Foss IS. Acute low back usually resolves quickly but persistent low back pain often persists. Journal of Physiotherapy 2013;59(2):127. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hewitt 2001
- Hewitt J. The Complete Yoga Book. New York (NY): Schocken Books Inc, 2001. [Google Scholar]
Higgins 2011a
- Higgins JP, Altman DG, Sterne JA. Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Higgins 2011b
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Higgins 2017
- Higgins JP, Altman DG, Sterne JA. Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s), Cochrane Handbook for Systematic Reviews of Interventions Version 5.2.0 (updated June 2017), The Cochrane Collaboration, 2017. Available from training.cochrane.org/handbook/archive/v5.2/:205-28.
Hill 2013
- Hill C. Is yoga an effective treatment in the management of patients with chronic low back pain compared with other care modalities – a systematic review. Journal of Complementary & Integrative Medicine 2013;10(1):211-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Holtzman 2013
- Holtzman S, Beggs RT. Yoga for chronic low back pain: a meta-analysis of randomized controlled trials. Pain Research & Management 2013;18(5):267-72. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
IAYT 2016
- International Association of Yoga Therapists (IAYT). Contemporary definitions of yoga therapy. www.iayt.org/?page=ContemporaryDefiniti (accessed 13 December 2016).
Jelicic Kadic 2016
- Jelicic Kadic A, Vucic K, Dosenovic S, Sapunar D, Puljak L. Extracting data from figures with software was faster, with higher interrater reliability than manual extraction. Journal of Clinical Epidemiology 2016;74:119-23. [PMID: ] [DOI] [PubMed] [Google Scholar]
Jordan 2006
- Jordan K, Dunn KM, Lewis M, Croft P. A minimal clinically important difference was derived for the Roland-Morris Disability Questionnaire for low back pain. Journal of Clinical Epidemiology 2006;59(1):45-52. [PMID: ] [DOI] [PubMed] [Google Scholar]
Koes 2006
- Koes BW, Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ (Clinical Research Ed.) 2006;332(7555):1430-4. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kongsted 2016
- Kongsted A, Kent P, Axen I, Downie AS, Dunn KM. What have we learned from ten years of trajectory research in low back pain? BMC Musculoskeletal Disorders 2016;17:220. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Lo 2020
- Lo J, Chan L, Flynn S. A systematic review of the incidence, prevalence, costs, and activity and work limitations of amputation, osteoarthritis, rheumatoid arthritis, back pain, multiple sclerosis, spinal cord injury, stroke, and traumatic brain injury in the United States: a 2019 update. Archives of Physical Medicine and Rehabilitation 2020;102(1):115-31. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Luckhaupt 2019
- Luckhaupt SE, Dahlhamer JM, Gonzales GT, Lu ML, Groenewold M, Sweeney MH, et al. Prevalence, recognition of work-relatedness, and effect on work of low back pain among U.S. workers. Annals of Internal Medicine 2019;171(4):301-4. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Luo 2004
- Luo X, Pietrobon R, Sun SX, Liu GG, Hey L. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine 2004;29(1):79-86. [PMID: ] [DOI] [PubMed] [Google Scholar]
Machado 2017
- Machado GC, Maher CG, Ferreira PH, Latimer J, Koes BW, Steffens D, et al. Can recurrence after an acute episode of low back pain be predicted? Physical Therapy 2017;97(9):889-95. [PMID: ] [DOI] [PubMed] [Google Scholar]
McCall 2007
- McCall T. Yoga as Medicine. New York (NY): Bantam Dell, 2007. [Google Scholar]
McPherson 1997
- McPherson K, Britton AR, Wennberg JE. Are randomized controlled trials controlled? Patient preferences and unblind trials. Journal of the Royal Society of Medicine 1997;90(12):652-6. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moore 1999
- Moore J, Lorig K, Korff M, Gonzalez VM, Laurent DD. The Back Pain Helpbook. Reading (MA): Perseus, 1999. [Google Scholar]
Nascimento 2019
- Nascimento PR, Costa LO, Araujo AC, Poitras S, Bilodeau M. Effectiveness of interventions for non-specific low back pain in older adults a systematic review and meta-analysis. Physiotherapy 2019;105(2):147-62. [PMID: ] [DOI] [PubMed] [Google Scholar]
NHIS 2018
- National Center for Health Statistics. Crude percentages of pain in lower back for adults aged 18 and over (standard errors), United States, 2015–2018. National Health Interview Survey, 2015–2018). Generated interactively at www.cdc.gov/nchs/nhis/ADULTS/www/index.htm (5 January 2021).
NICE 2016
- National Collaborating Centre for Chronic Conditions (UK). Low back pain and sciatica in over 16s: assessment and management, 2016 (last updated 11 December 2020). www.nice.org.uk/guidance/NG59 (accessed 5 January 2021).
Oliveira 2018
- Oliveira CB, Maher CG, Pinto RZ, Traeger AC, Lin CC, Chenot JF, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. European Spine Journal 2018;27(11):2791-803. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ostelo 2008
- Ostelo RW, Deyo RA, Stratford P, Waddell G, Croft P, Korff M, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine 2008;33(1):90-4. [PMID: ] [DOI] [PubMed] [Google Scholar]
Pengel 2003
- Pengel LH, Herbert RD, Maher CG, Refshauge KM. Acute low back pain: systematic review of its prognosis. BMJ (Clinical Research Ed.) 2003;327(7410):323. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Posadzki 2011
- Posadzki P, Ernst E. Yoga for low back pain: a systematic review of randomized clinical trials. Clinical Rheumatology 2011;30(9):1257-62. [PMID: ] [DOI] [PubMed] [Google Scholar]
Preference Collaborative Review Group 2008
- Preference Collaborative Review Group. Patients' preferences within randomised trials: systematic review and patient level meta-analysis. BMJ (Clinical Research Ed.) 2008;337:a1864. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Review Manager 5. Version 5.4. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Ryan 2016
- Ryan R, Hill S, Cochrane Consumers and Communication Group. How to GRADE the quality of the evidence. cccrg.cochrane.org/author-resources (accessed 8 December 2016).
Saper 2004
- Saper RB, Eisenberg DM, Davis RB, Culpepper L, Phillips RS. Prevalence and patterns of adult yoga use in the United States: results of a national survey. Alternative Therapies in Health and Medicine 2004;10(2):44-9. [PMID: ] [PubMed] [Google Scholar]
Schünemann 2019
- Schünemann HJ, Vist GE, Higgins JP, Santesso N, Deeks JJ, Glasziou P, et al. Chapter 15: Interpreting results and drawing conclusions. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (updated July 2019). 2nd edition. Chichester (UK): John Wiley & Sons, 2019:403-28. [Google Scholar]
Sherman 2010
- Sherman KJ, Cherkin DC, Cook AJ, Hawkes RJ, Deyo RA, Wellman R, et al. Comparison of yoga versus stretching for chronic low back pain: protocol for the Yoga Exercise Self-care (YES) trial. Trials 2010;11:36. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shmagel 2016
- Shmagel A, Foley R, Ibrahim H. Epidemiology of chronic low back pain in US adults: data from the 2009–2010 National Health and Nutrition Examination Survey. Arthritis Care & Research 2016;68(11):1688-94. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Skelly 2018
- Skelly AC, Chou R, Dettori JR, Turner JA, Friedly JL, Rundell SD, et al. Noninvasive nonpharmacological treatment for chronic pain: a systematic review [internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2018 Jun. Report No.: 18-EHC013-EF. [PMID: ] [PubMed]
Sorosky 2008
- Sorosky S, Stilp S, Akuthota V. Yoga and pilates in the management of low back pain. Current Reviews in Musculoskeletal Medicine 2008;1(1):39-47. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stanton 2008
- Stanton TR, Henschke N, Maher CG, Refshauge KM, Latimer J, McAuley JH. After an episode of acute low back pain, recurrence is unpredictable and not as common as previously thought. Spine 2008;33(26):2923-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Tran 2015
- Tran HH, Weinberg J, Sherman KJ, Saper RB. Preference and expectation for treatment assignment in a randomized controlled trial of once- vs twice-weekly yoga for chronic low back pain. Global Advances in Health and Medicine 2015;4(1):34-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
van Tulder 2006
- Tulder M, Koes B. Chronic low back pain. American Family Physician 2006;74(9):1577-9. [PMID: ] [PubMed] [Google Scholar]
Ward 2013
- Ward L, Stebbings S, Cherkin D, Baxter GD. Yoga for functional ability, pain and psychosocial outcomes in musculoskeletal conditions: a systematic review and meta-analysis. Musculoskeletal Care 2013;11(4):203-17. [PMID: ] [DOI] [PubMed] [Google Scholar]
Will 2018
- Will JS, Bury DC, Miller JA. Mechanical Low Back Pain. American Family Physician 2018;98(7):421-8. [PMID: ] [PubMed] [Google Scholar]
Wolsko 2003
- Wolsko PM, Eisenberg DM, Davis RB, Kessler R, Phillips RS. Patterns and perceptions of care for treatment of back and neck pain: results of a national survey. Spine 2003;28(3):292-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Wren 2011
- Wren AA, Wright MA, Carson JW, Keefe FJ. Yoga for persistent pain: new findings and directions for an ancient practice. Pain 2011;152(3):477-80. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Wieland 2013
- Wieland LS, Skoetz N, Manheimer E, Pilkington K, Vempati R, Berman BM. Yoga treatment for chronic non-specific low back pain. Cochrane Database of Systematic Reviews 2013, Issue 7. Art. No: CD010671. [DOI: 10.1002/14651858.CD010671] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wieland 2017
- Wieland LS, Skoetz N, Pilkington K, Vempati R, D'Adamo CR, Berman BM. Yoga treatment for chronic non-specific low back pain. Cochrane Database of Systematic Reviews 2017, Issue 1. Art. No: CD010671. [DOI: 10.1002/14651858.CD010671.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


