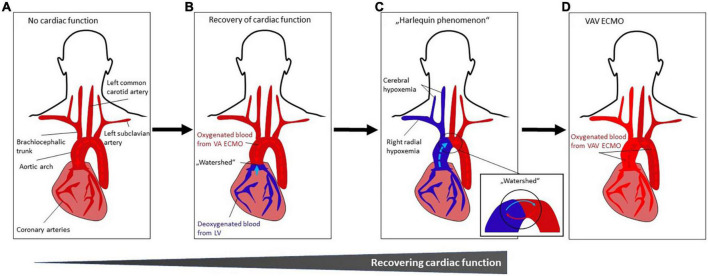
FIGURE 4.
(A–D) Occurrence and treatment of differential hypoxemia during VA ECMO treatment. (A) No cardiac function. Systemic perfusion with oxygenated blood (indicated by dark red color) is solely dependent from VA ECMO flow which is infused retrogradely toward the heart. (B) Recovery of cardiac function with impaired pulmonary gas exchange. The LV starts ejecting poorly oxygenated blood from the pulmonary circulation (indicated by blue color) that mixes with oxygenated blood from the VA ECMO (“watershed” or “mixing cloud”). The location of the “watershed” depends on the LV function and the VA ECMO flow. With severe myocardial dysfunction (e.g., due to cardiac arrest), the watershed is close to or at (if asystolic patient) the aortic valve. (C) Harlequin phenomenon. With improving LV function, the “watershed” may move more distally in the aortic arch. As a result, given impaired pulmonary function, poorly oxygenated blood from the LV is ejected into the aortic arch, coronary and cerebral arteries, resulting in ischemia and cyanosis of the upper body (in this case, right upper body), while the lower body is sufficiently oxygenated by the VA ECMO circuit. This phenomenon is known as differential hypoxemia, watershed phenomenon, two-circulation syndrome or Harlequin phenomenon. (D) VAV ECMO. The Harlequin phenomenon (Figure 3C) can be treated by converting VA ECMO to VAV ECMO. Thus, ECMO-oxygenated blood (indicated by lighter red color) is infused from a third ECMO cannula via the jugular or subclavian vein through and the pulmonary circulation into the LV and upper body (see Figure 1C). Abbreviations: left ventricle (LV); veno-arterial extracorporeal membrane oxygenation (VA ECMO); veno-arterio-venous ECMO (VAV ECMO).