Abstract
Purpose:
This article focuses on the transition to adult health care in youth with spina bifida (SB) from the perspective of theory, measurement, and interventions.
Methods:
The purpose of this article is to discuss (a) a theory of linkages between the transfer of medical responsibility from parent to child and the transition from pediatric to adult health care, as mediated by transition readiness; (b) measurement issues in the study of self-management and the transition to adult health care; and (c) U.S.-based and international interventions focused on the transition to adult health care in young adults with SB.
Findings:
Individuals with SB must adhere to a complex multicomponent treatment regimen while at the same time managing a unique array of cognitive and psychosocial challenges and comorbidities that hinder self-management, medical adherence, and the transition to adult health care. Moreover, such youth endure multiple transitions to adult health care (e.g., in the areas of urology, orthopedics, neurosurgery, and primary care) that may unfold across different time frames. Finally, three transition-related constructs need to be assessed, namely, transition readiness, transition completion, and transition success.
Conclusions:
SB provides an important exemplar that highlights the complexities of conducting research on the transition to adult health care in youth with chronic health conditions. Many transition trajectories are possible, depending on the functioning level of the child and a host of other factors. Also, no single transition pathway is optimal for all patients with SB.
Clinical Relevance:
The success of the process by which a child with SB transitions from pediatric to adult health care can have life-sustaining implications for the patient.
Keywords: Adolescence, adult health care, chronic illness/chronic disease, quality improvement of care, symptom management
Spina bifida (SB) is a relatively common congenital birth defect that is caused by an incomplete closure of the neural tube during the early stages of pregnancy (Copp et al., 2015). Hispanic or Latino youth demonstrate the highest rates, followed by non-Hispanic European Americans, and African Americans (Boulet et al., 2008). The severity of the disability in SB is linked with the level of the spinal lesion, with higher levels causing more impairment. Those with SB often have shunted hydrocephalus and a Chiari II malformation as well as motor difficulties, neurogenic bladder and bowel, and pressure injuries (Copp et al., 2015). They also exhibit cognitive difficulties in the areas of executive functioning and attention (Dennis & Barnes, 2010), which places them at risk for academic problems as well as difficulties in managing their medically complex treatment regimen. Moreover, they are at risk for depression, social problems, obesity, lower levels of quality of life, and difficulties achieving the milestones of early adulthood such as employment, education, and involvement in romantic relationships (Holmbeck et al., 2010; Murray et al., 2015; Sawin & Bellin, 2010; Zukerman, Devine, & Holmbeck, 2011).
Importantly, the transfer of medical responsibility from parent to child is very challenging for most families of youth with SB (Psihogios, Kolbuck, & Holmbeck, 2015). Moreover, the manner in which this transfer process is managed may have downstream effects on other important condition-related milestones, such as the transition from pediatric to adult health care (Reed-Knight, Blount, & Gilleland, 2014). In this article, the term transfer will refer to the transfer of medical responsibility from parent to child (e.g., where the child begins to manage the steps of the catheterization process), and the term transition will refer to the transition from pediatric to adult health care (e.g., the child begins to see a urologist who cares for adults and stops seeing a pediatric urologist). More specifically, the transition to adult health care has been described as a dynamic process wherein an individual moves from pediatric, family-oriented health care to adult, individual-oriented health care, with the goal being the provision of high-quality, developmentally appropriate, uninterrupted healthcare services (American Academy of Pediatrics, 2002). Unfortunately, there is a dearth of research on how this gradual transition process unfolds over time in populations with chronic health conditions, including youth with SB (Betz, Smith, Van Speybroeck, Hernandez, & Jacobs, 2016; Binks, Barden, Burke, & Young, 2007; Sawyer & Macnee, 2010). Similar to other pediatric health conditions, pediatric care for SB often occurs in the context of a single, multidisciplinary clinic (Liptak & El Samra, 2010), with many young adults continuing to be followed in these settings well past the age of 18 years. Unlike pediatric settings, the adult healthcare system is fragmented and often requires individuals with SB to make separate appointments with multiple specialists across multiple settings (e.g., urologists, orthopedists, neurologists; Kaufman, Terbrock, Winters, Klosterman, & Park, 1994; Liptak & El Samra, 2010). Clearly, empirical evidence is needed on factors that contribute to a successful transition to adult-centered healthcare services in this population, given that many youths with SB experience general health declines during this period. In fact, it has been reported that renal damage occurs in over 30% of young adults with SB and pressure injuries occur in over 50% (Liptak, Kennedy, & Dosa, 2010; Roach, Short, & Saltzman, 2011). Such complications are likely caused, at least in part, by difficulties encountered during the transition process. Similarly, in Canada, Young and colleagues (2006) examined the transition of children with cerebral palsy, SB, and acquired brain injury and reported that adults with SB reported the worst self-rated health across all three of these groups.
The purpose of the discussion that follows is to review (a) a theory of linkages between the transfer of medical responsibility from parent to child and the transition from pediatric to adult health care; (b) measurement issues related to the assessment of self-management and this transition; and (c) U.S.-based and international interventions focused on the transition to adult health care in young adults with SB. We conclude with a discussion of implications for nursing practice and recommendations for future research on the transition to adult health care.
Theories: Self-Management and the Transition to Adult Health Care
Based on earlier models of self-management and transition readiness (Grey, Schulman-Green, Knafl, & Reynolds, 2015; Modi et al., 2012; Reed-Knight et al., 2014; Sawin, 2017; Schwartz et al., 2013), as well as interviews of youth, young adults, parents, and healthcare professionals, we propose a two-part model of self-management and the transition to adult health care in youth with SB (Figure 1). The first part of the model (top of Figure 1) includes predictors of self-management (i.e., demographic, condition-related, individual, family, peer), dimensions and mediators of self-management (i.e., readiness and self-efficacy to self-manage, skills to execute self-management behaviors, and the degree to which the youth is responsible for self-management), as well as adherence outcomes and health complications. The bottom part of Figure 1 extends the model by including self-management as the starting point and as a precursor to the transition to adult health care. Specifically, this second part of the model links the successful transfer of medical responsibility (from parent to child) to the successful transition to adult health care via transition readiness. In other words, the degree to which youth take on responsibility for their own self-management is expected to make them more “ready” to transition to adult health care, which is, in turn, expected to make it more likely that they will experience a successful transition.
Figure 1.
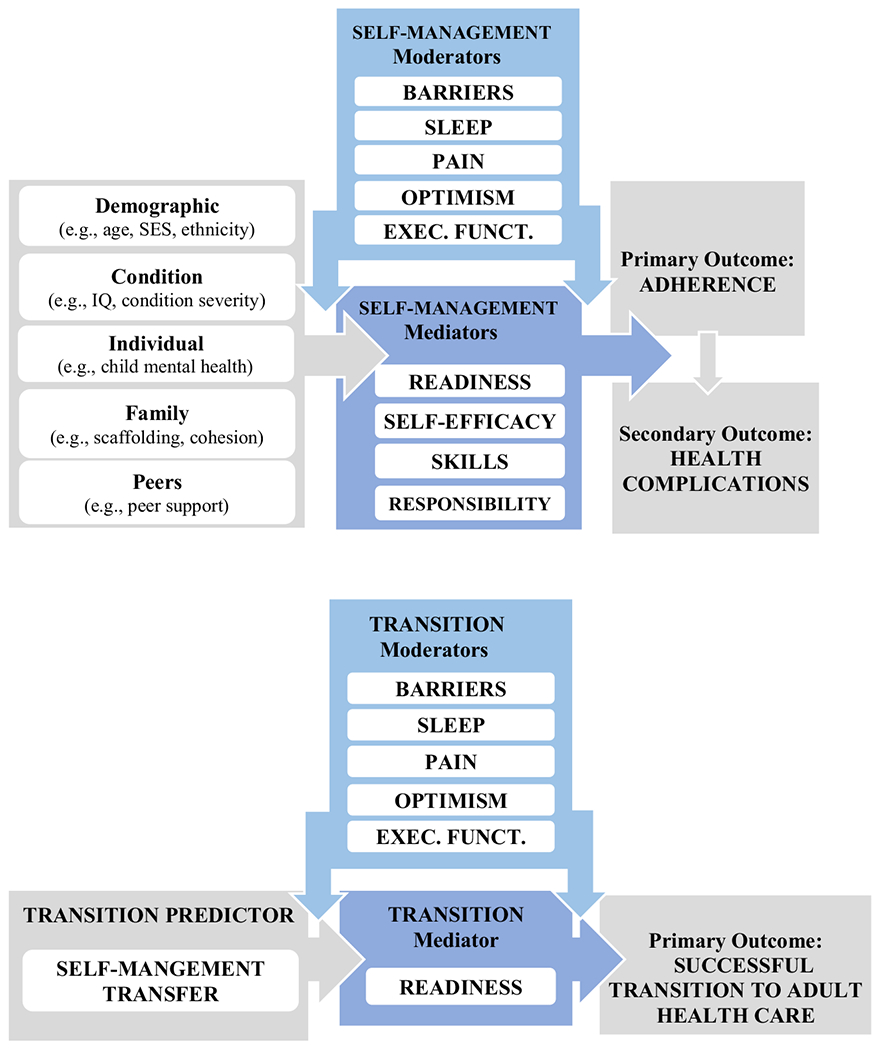
Models of self-management and the transition to adult health care in youth with spina bifida. Parental scaffolding is the process by which a parent aids their child in skill acquisition and eventual independence by gradually removing supports as the child becomes increasingly responsible (Wood, Bruner, & Ross, 1976); Cohesion represents shared affection, support, helpfulness, and caring among family members (Moos, 1974). Mediator variables specify how (or the mechanism by which) a given effect occurs (Holmbeck, 1997). Moderator variables specify the conditions under which a given effect occurs, as well as the conditions under which the direction or strength of an effect varies (Holmbeck, 1997). We expect that the strength of the mediational pathways in the model will vary depending on the presence of certain barriers or facilitators (i.e., moderators). EXEC. FUNCT. = executive functioning; IQ = intelligence quotient; SES = socioeconomic status. [Colour figure can be viewed at wileyonlinelibrary.com]
To what degree have past research findings supported this theoretical model? Although links between the transfer of medical responsibility and the transition to adult health care have not been examined, some of our findings support specific components of these models. For example, Kayle, Chu, Stern, Pan, and Holmbeck (2020) found that the transfer of responsibility from parent to child does not unfold in the same manner across all youth with SB. Instead, Kayle and colleagues found that roughly two thirds of youth with SB assume increasing responsibility over time (a high increasing trajectory), with most of these youth having more responsibility than do their parents beginning at ages 12 to 13 years. The other one third of the sample assume only limited amounts of responsibility (a low increasing trajectory), with parents having more responsibility than do youth throughout the adolescent years. Participants in the high increasing trajectory were more likely to have a higher IQ, be female, and come from homes with less familial stress related to having a child with SB. Such findings have potential implications for the transition to adult health care. For example, we would expect that those who move along the high increasing trajectory are more likely to have a smooth transition to adult health care than those on the low increasing trajectory. Of course, the findings for IQ suggest that some youth with SB are cognitively lower functioning and are unable to take over significant levels of self-management responsibility; in these cases, favorable transition outcomes may still be possible if such youth have skilled caregivers who can responsibly manage and sustain this transition process.
Measurement: Self-Management and the Transition to Adult Health Care
The measurement of the self-management process as well as the transition to adult health care is complicated by several factors, most of which relate to the complexities of SB (Table 1). Importantly, individuals with SB can assume different levels of responsibility for self-management across each of the medical regimen tasks (e.g., catheterization, bowel program, medication, skin care). Also, the process by which an individual develops increasing levels of self-management unfolds across multiple dimensions (see Figure 1 and Table 1; e.g., responsibility, skills, self-efficacy; Psihogios et al., 2015). For example, two children with SB who are the same age may exhibit different levels of responsibility for their medical care. Or, two children may have the same amount of responsibility but exhibit very different levels of skills to take on such responsibility. Also, two youth may have acquired the same amount of responsibility and skills, but exhibit different levels of adherence to what is prescribed by the medical professional. Youth with SB may also vary in their experiences of different types of barriers (e.g., differing levels of executive functioning) that may make self-management or adherence more difficult. Finally, and given different levels of responsibility, skills, adherence, and barriers, youth with SB may differ in the types and severity of health complications that they experience. And, as noted above, all of these self-management dimensions may be exhibited differently across each of the medical regimen tasks.
Table 1.
The Transfer and Transition Processes: Tasks, Providers, and Dimensions
| Transfer of medical responsibility from parent to child | Transition from pediatric to adult health care |
|---|---|
|
Tasks to be transferred Catheterization Bowel program Skin care Medication Exercise Setting up healthcare appointments |
Providers to be transitioned Neurosurgery/neurology Urology Orthopedics Primary care Other healthcare providers |
|
Dimensions/mediators/outcomes of transfer Responsibility Skills Transfer readiness Self-efficacy Adherence Health complications |
Dimensions/mediators/outcomes of transition Transition readiness Transition completion Transition success |
Prior work on the transfer process has noted that a successful transfer of responsibility from parent to child typically occurs gradually rather than abruptly and often involves continued parental involvement over the course of adolescence (Helgeson, Reynolds, Siminerio, Escobar, & Becker, 2008; Psihogios & Holmbeck, 2013; Reed-Knight et al., 2014; Wysocki et al., 1996). If the transfer is initiated prematurely with limited parental oversight, nonadherence and health complications may result. It is also possible that parental involvement could become excessive and possibly undermine the unfolding of the self-management process (Campbell et al., 2019). Thus, given different levels of skills and barriers, the task of finding the right mix of medical responsibilities that results in an optimal level of adherence is a difficult one for every parent who has a child with SB.
The measurement of the transition to adult health care is no less complicated than the measurement of self-management and its various dimensions (see Table 1). Unlike most other chronic conditions, youth with SB must endure multiple transitions to adult health care because they have multiple healthcare providers. As noted above, the medical regimen for youth with SB is made up of several tasks involving various recommendations from different healthcare professionals. When a child is young, each of these providers is typically part of a pediatric multidisciplinary treatment team. When youth with SB approach young adulthood, they must navigate multiple transitions to adult health care across any or all of the following providers: neurosurgery/neurology, urology, orthopedics, primary care, and other healthcare providers (see Table 1). The demands of multiple transitions are particularly challenging for this population because of the cognitive and psychological challenges and comorbidities noted earlier.
In addition to managing multiple transitions, there are several transition-related constructs that should be assessed. Specifically, transition readiness, transition completion, and the success of the transition can be assessed across each type of healthcare provider. With respect to transition readiness, one useful measurement option is the SB version of the Transition Readiness Assessment Questionnaire (TRAQ-SB; Wood, Rocque, Hopson, Barnes, & Johnson, 2019), which has been shown to have adequate criterion-related validity and internal consistency reliability. For a comprehensive review of self-management and transition readiness instruments, the reader is referred to Sawin and colleagues’ (2020) review of instruments reported in the literature over the past 10 years. With respect to transition completion, our research team has begun developing a coding system for each type of healthcare provider based on the reliable coding of a combination of questionnaire and interview data. As can be seen in Table 2, the success of the transition is assessed separately for each provider, is based on an assessment of whether or not the youth has experienced transition-related meetings and discussions with pediatric or adult providers, and includes an assessment of each youth’s subjective opinion regarding their transition status. Finally, the success of the transition is assessed by examining how they manage health-related complications. These dimensions of “management of SB complications” in Table 2 (i.e., autonomy, urgency, action, anticipation, and prevention) align with key outcomes established for transition success, including patient knowledge, understanding characteristics of condition and complications, and avoidance of unnecessary hospitalizations (Fair et al., 2016).
Table 2.
Measuring Transition Success
| Aspect of transition | Description | Lowest score | Highest score |
|---|---|---|---|
| Providers | Do they see adult providers and specialists? | 100% are pediatric providers | 100% are adult providers |
| Transition meeting/discussion | Did they meet with their providers to discuss transition? |
No meeting or discussion | Discussion of transition with two or more providers |
| Subjective opinion | Do they report that they believe they have transitioned? | Self-reports that they have not transitioned | Self-reports that they have fully transitioned |
| Management of complications | Are they able to manage issues such as a UTI, headache, etc.? | None of the following: Autonomy Urgency Action Anticipation Prevention |
Endorses the following: Autonomy Urgency Action Anticipation Prevention |
U.S.-Based and International Interventions: The Transition to Adult Health Care
There are a relatively small number of randomized controlled trials examining the effectiveness of transition interventions for adolescents across chronic conditions, highlighting the need for more robust research evidence for transitional care interventions (Campbell, Aldiss, & Biggs, 2020). Betz and colleagues provide an overview of healthcare transition practice and research, emphasizing the role of nursing (Betz, in press), as well as exemplars of nursing research investigations conducted during the healthcare transition (Grady, Rehm, & Betz, in press). Further, researchers have worked to establish international and interdisciplinary consensus on priority outcomes in healthcare transition studies, including optimal quality of life, self-management of condition, understanding characteristics of conditions and complications, among others (Fair et al., 2016).
In terms of the SB-specific transition, a small number of transition interventions have emerged. Two studies have described programs in the United States specifically aimed at helping youth with SB transition to adult healthcare services. First, the Spina Bifida Transition Project (SBTP) involved a pretransition orientation visit with a nurse at a children’s hospital, a summary of health problems and treatment, a tour of the adult care setting, transfer of medical records, and transition visits to adult clinics (Sawin et al., 2015). Investigators found that 82% of SBTP participants had a positive experience, even when encountering difficulties with engaging or establishing rapport with new providers. Another paradigm is the Movin’ On Up program, which includes a healthcare transition (HCT) nursing specialist, interdisciplinary healthcare transition plans, an interdisciplinary HCT team, direct HCT services provided in a weekly SB clinic, and telephone follow-ups with patients, families, and providers. Investigators reported that 210 adolescents and emerging adults with SB have been enrolled in the program (Betz et al., 2016).
Additionally, there have been efforts to bolster transition readiness. The Transition Preparation Training Program included a 2-day workshop, culminating in an adolescent-centered transition plan based on the personalized goals of the adolescent with SB (Betz, Smith, & Macias, 2010). Workshop elements included identification of goals, resources, and referrals and practicing strategies for obtaining services. While no treatment effects were observed in a prospective randomized controlled trial (RCT) of this program, investigators highlighted issues that may have undermined the ability to detect intervention effects, namely, the small dose of the intervention, lack of condition-specific knowledge, low level of transition readiness among participants, and low adherence, specifically in terms of workshop attendance and transition plan follow-through (Betz et al., 2010). Other research targeting transition readiness reported on a quality improvement pilot study that restructured the clinical roles of six nursing care coordinators (Seeley & Lindeke, 2017). These nurses collaborated with families to develop individualized family-centered plans focused on improving self-management and readiness for transition. Results from 14 youth–parent pairs suggest that families perceived improved transition readiness following the program (Seeley & Lindeke, 2017). Similarly, Hopson, Alford, Zimmerman, Blount, and Rocque (2019) developed individualized transition plans for adolescents with SB that focused on five goals: maximizing education, bowel continence, and goals set by the SB clinic coordinator, parent or caregiver, and patient. Preliminary results suggest that the program was well received by families and may promote adherence with care plans (Hopson et al., 2019).
Although considerable work has been done with other chronic health conditions across several other countries (Betz & Coyne, 2020), transition interventions for individuals with SB have only been evaluated in Australia, Canada, and the United Kingdom. In a prospective study of the development of an SB adult service, West, Brodie, Dicker, and Steinbeck (2011) outlined both a local clinic option and a state-wide option in Australia, and described the establishment of the Spina Bifida Adult Resource Team, which provided clinical consultation, education, support, and preventative health strategies to adults with SB. In an interagency program in Canada, a pediatric hospital partnered with an adult community healthcare center (CHC) to provide coordinated, continuous care for individuals with SB (Lindsay et al., 2016). The program established a transition team that consisted of a cross-appointed nurse practitioner and life skills coach who provided services at the pediatric hospital and adult CHC, and an adolescent medicine specialist at the pediatric hospital. These team members collaborated with other staff at both sites to coordinate referrals to adult health care and provide youth with adult medical and life skills. Parents and youth reported feeling supported when participating in this program. By comparison, those who did not participate reported experiencing some gaps in the continuity of their care (Lindsay et al., 2016). Finally, focus group sessions and a survey of members of the Scottish Spina Bifida Association (ages 12 to 26 years) revealed that most participants in the 12- to 18-year-old age range had not yet started their transition process. While participants described pediatric care as attentive and comprehensive, they noted that adult specialist services were limited, and adult providers tended to lack knowledge and were less likely to demonstrate respect for young people with special needs (Levy, Wynd, & Carachi, 2014).
Implications for Nursing Practice
As others have acknowledged (Betz, 2017; Coyne & Betz, 2020), nurses are ideally situated to assist with the transition from pediatric to adult health care given their long-term relationships and frequent contact with patients, expertise in care coordination, and core competences that emphasize the role of nursing in transition services (International Family Nursing Association, 2015). Nurses have an important role in educating patients and their families, preparing them for transition, providing support, monitoring readiness, and promoting important skills related to self-care and self-management (Coyne & Betz, 2020). While all nurses can engage in phases of the transition process, specialized nursing roles such as transition coordinators or case managers are dedicated to the process. Advanced practice registered nurses engage in interprofessional care coordination and collaboration, develop and implement evidence-based transition programs, and engage in continuous quality monitoring and improvement (Lestishock, Disabato, & Daley, 2020).
The model proposed here has implications for nursing practice, education, and research. First, in terms of practice, nurses should consider the contextual and mediational factors presented in Figure 1 in their comprehensive assessments of self-management and readiness. For example, the model suggests that individuals with better executive functioning, higher levels of self-management skills, and appropriate self-management responsibility will have the most favorable adherence outcomes and the lowest number of health complications. Alternatively, when nurses identify vulnerability factors (e.g., low socio-economic status, poor child mental health), these risk factors may indicate that additional assessments and interventions are warranted. Identification of these vulnerability factors can, in turn, inform nurse-led educational programs. In fact, Coyne and Betz (2020) pointed out that there is evidence supporting the use of such programs for adolescents and their families with other conditions. Additionally, our model can guide a developmentally appropriate and comprehensive approach to educating adolescents with SB and their families about key factors related to adherence and health-related complications. Finally, in terms of research, our model can facilitate more outcome-focused research (Coyne & Betz, 2020) while also accounting for the complexity of SB and the assessment of the transition to adult health care. The coding system that we are developing (see earlier section on “Measurement: Self-Management and the Transition to Adult Health Care”) considers the various outcomes associated with a successful transition to adult healthcare in SB and allows for variability in one’s transition status across providers. As such, this type of coding system takes into account the complexity of the transition.
Directions for Future Research
SB is an ideal population in which to study the transfer and transition processes, given the complexity of both of these processes for youth with this chronic health condition. Specifically, youth must manage the transfer of multiple tasks (rather than just one), and they must also manage the transition to adult health care across multiple healthcare providers (rather than just one)—and they must do all of this while enduring numerous cognitive and psychological comorbidities. Additionally, the process is further complicated for youth who are cognitively low functioning and rely more heavily on caregivers throughout these processes. Also, as indicated in Table 1, each process is composed of several dimensions that would need to be assessed to provide a complete picture of what an individual is experiencing during the transfer and transition processes. Finally, we have also made the case that it is likely that there are important linkages between the transfer process and the transition process.
Clearly, we need more research on both the transfer process and the transition process and the longitudinal linkages between the two. Also, intervention development is in its infancy regarding the transition to adult health care in this population. In the future, we need more RCTs that focus on potentially efficacious transition interventions that can facilitate an effective and smooth transition with minimal health complications. We also need more work on how these important medically related processes (i.e., transfer and transition) interact with other important independence-related developmental milestones, such as living independently or obtaining employment or postsecondary education.
Clinical Resources.
Child Neurology Foundation. Eight common principles to assist with the transition of care. https://www.childneurologyfoundation.org/wp-content/uploads/2017/08/CNF_8_Principles_Inforgraphic_v5a.pdf
Got Transition. https://www.gottransition.org/
Pacer Center. Pacer’s National Parent Center on Transition and Employment. https://www.pacer.org/transition/
Spina Bifida Association. Guidelines for the care of people with spina bifida. https://www.spinabifidaassociation.org/guidelines/
Spina Bifida Association. National Resource Center. https://www.spinabifidaassociation.org/national-resource-center/
Acknowledgments
Portions of this article were presented at the 2020 National Nursing Research Roundtable (“Care Transitions from Pediatric to Adult Care: Planning and Interventions for Adolescents and Youth Adults with Chronic Illness”), in Bethesda, MD, March 5–6, 2020. This work was supported in part by research grants from the National Institute of Nursing Research (No. R01 NR016235), the National Institute of Child Health and Human Development (No. R01 HD048629), and the March of Dimes Birth Defects Foundation (No. 12-FY13-271). The authors thank the Illinois Spina Bifida Association as well as staff of the spina bifida clinics at Ann & Robert H. Lurie Children’s Hospital of Chicago and Loyola University Medical Center. They also thank the numerous undergraduate and graduate research assistants who helped with data collection and data entry. Finally, they thank the parents, children, teachers, and health professionals who have participated in the Chicago Healthy Adolescent Transition Study (CHATS).
References
- American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians-American Society of Internal Medicine. (2002). A consensus statement on health care transitions for young adults with special health care needs. Pediatrics, 10(6 Pt. 2), 1304–1306. [PubMed] [Google Scholar]
- Betz CL (2017). SPN position statement: Transition of pediatric patients into adult care. Journal of Pediatric Nursing, 35, 160–164. 10.1016/j.pedn.2017.05.003 [DOI] [PubMed] [Google Scholar]
- Betz CL (in press). Nursing’s influence on the evolution of the field of health care transition and future implications. Manuscript submitted for publication. [DOI] [PubMed] [Google Scholar]
- Betz CL, & Coyne IT (Eds.). (2020). Transition from pediatric to adult health care services for adolescents and young adults with long-term conditions: An international perspective on nurse’s roles and interventions. Cham, Switzerland: Springer Nature Switzerland AG. [Google Scholar]
- Betz CL, Smith K, & Macias K (2010). Testing the transition preparation training program: A randomized controlled trial. International Journal of Child and Adolescent Health, 3(4), 595–607. [PMC free article] [PubMed] [Google Scholar]
- Betz CL, Smith KA, Van Speybroeck A, Hernandez FV, & Jacobs RA (2016). Movin’ on up: An innovative nurse-led interdisciplinary health care transition program. Journal of Pediatric Health Care, 30(4), 323–338. [DOI] [PubMed] [Google Scholar]
- Binks JA, Barden WS, Burke TA, & Young NL (2007). What do we really know about the transition to adult-centered health care? A focus on cerebral palsy and spina bifida. Archives of Physical Medicine and Rehabilitation, 88(8), 1064–1073. [DOI] [PubMed] [Google Scholar]
- Boulet SL, Yang Q, Mai C, Kirby RS, Collins JS, Robbins JM, … National Birth Defects Prevention Network. (2008). Trends in the postfortification prevalence of spina bifida and anencephaly in the United States. Birth Defects Research, 82(7), 527–532. 10.1002/bdra.20468 [DOI] [PubMed] [Google Scholar]
- Campbell F, Aldiss S, & Biggs K (2020). Transition of care for adolescents from child to adult health services: A systematic review. In Betz CL & Coyne IT (Eds.). Transition from pediatric to adult healthcare services for adolescents and young adults with long-term conditions (pp. 147–169). Cham, Switzerland: Springer. [Google Scholar]
- Campbell MS, Wang J, Cheng Y, Cogen FR, Streisand R, & Monaghan M (2019). Diabetes-specific family conflict and responsibility among emerging adults with type 1 diabetes. Journal of Family Psychology, 33, 788–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copp AJ, Adzick NS, Chitty LS, Fletcher JM, Holmbeck GN, & Shaw GM (2015). Spina bifida. Nature Reviews Disease Primers, 1, 155007. 10.1038/nrdp.2015.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne IT, & Betz CL (2020). Nursing initiatives and future directions for transition practice and research. In Betz CL & Coyne IT (Eds.), Transition from pediatric to adult healthcare services for adolescents and young adults with long-term conditions (pp. 319–336). Cham, Switzerland: Springer. [Google Scholar]
- Dennis M, & Barnes MA (2010). The cognitive phenotype of spina bifida meningomyelocele. Developmental Disabilities Research Reviews, 16(1), 31–39. 10.1002/ddrr.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fair C, Cuttance J, Sharma N, Maslow G, Wiener L, Betz C, … Naranjo D (2016). International and interdisciplinary identification of health care transition outcomes. JAMA Pediatrics, 170, 205–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grady K, Rehm R, & Betz CL (in press). Understanding the phenomenon of health care transition: Theoretical underpinnings, exemplars of nursing contributions, and research implications. Journal of Pediatric Health Care. [DOI] [PubMed] [Google Scholar]
- Grey M, Schulman-Green D, Knafl K, & Reynolds NR (2015). A revised self- and family management framework. Nursing Outlook, 63, 162–170. [DOI] [PubMed] [Google Scholar]
- Helgeson VS, Reynolds KA, Siminerio L, Escobar O, & Becker D (2008). Parent and adolescent distribution of responsibility for diabetes self-care: Links to health outcomes. Journal of Pediatric Psychology, 33(5), 497–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmbeck GN (1997). Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: Examples from the child-clinical and pediatric psychology literatures. Journal of Consulting and Clinical Psychology, 65, 599–610. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN, DeLucia C, Essner BS, Kelly L, Zebracki K, Friedman D, & Jandasek B (2010). Trajectories of psychosocial adjustment in adolescents with spina bifida: A 6-year, four-wave longitudinal follow-up. Journal of Consulting and Clinical Psychology, 78(4), 511–525. 10.1037/a0019599 [DOI] [PubMed] [Google Scholar]
- Hopson B, Alford EN, Zimmerman K, Blount JP, & Rocque BG (2019). Development of an evidence-based individualized transition plan for spina bifida. Neurosurgical Focus, 47(4). Retrieved from https://thejns.org/focus/view/journals/neurosurg-focus/47/4/article-pE17.xml [DOI] [PubMed] [Google Scholar]
- International Family Nursing Association. (2015). IFNA position statement on generalist competencies for family nursing practice. Retrieved from https://internationalfamilynursing.org/2015/07/31/ifna-position-statement-on-generalist-competencies-for-family-nursing-practice/
- Kaufman BA, Terbrock A, Winters N, Klosterman A, & Park TS (1994). Disbanding a multidisciplinary clinic: Effects on the health care of myelomeningocele patients. Pediatric Neurosurgery, 21(1), 36–44. [DOI] [PubMed] [Google Scholar]
- Kayle M, Chu DI, Stern A, Pan W, & Holmbeck GN (2020). Trajectories of self-management in youth with spina bifida: Condition-related, parental, and family systems predictors of medical responsibility. Journal of Pediatric Psychology, 45, 1153–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lestishock L, Disabato J, & Daley AM (2020). NAPNAP position statement on supporting the transition from pediatric to adult-focused health care. Journal of Pediatric Health Care, 34, 390–394. [Google Scholar]
- Levy S, Wynd AH, & Carachi R (2014). Transition into adult healthcare services in Scotland: Findings from a study concerning service users at the Scottish Spina Bifida Association. Scottish Medical Journal, 59(4), 209–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay S, Fellin M, Cruickshank H, McPherson A, & Maxwell J (2016). Youth and parents’ experiences of a new inter-agency transition model for spina bifida compared to youth who did not take part in the model. Disability and Health Journal, 9(4), 705–712. [DOI] [PubMed] [Google Scholar]
- Liptak GS, & El Samra A (2010). Optimizing health care for children with spina bifida. Developmental Disabilities Research Reviews, 16(1), 66–75. 10.1002/ddrr.91 [DOI] [PubMed] [Google Scholar]
- Liptak GS, Kennedy JA, & Dosa NP (2010). Youth with spina bifida and transitions: Health and social participation in a nationally representative sample. Journal of Pediatrics, 157(4), 585–588. 10.1016/j.jpeds.2010.04.004 [DOI] [PubMed] [Google Scholar]
- Modi AC, Pai AL, Hommel KA, Hood KK, Cortina S, Hilliard ME, … Drotar D (2012). Pediatric self-management: A framework for research, practice, and policy. Pediatrics, 129(2), e473–e485. 10.1542/peds.2011-1635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH (1974). The social climate scales. Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Murray CB, Holmbeck GN, Ros AM, Flores DM, Mir SA, & Varni JW (2015). A longitudinal examination of health-related quality of life in children and adolescents with spina bifida. Journal of Pediatric Psychology, 40(4), 19–30. 10.1093/jpepsy/jsu098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psihogios AM, & Holmbeck GN (2013). Discrepancies in mother and child perceptions of spina bifida medical responsibilities during the transition to adolescence: Associations with family conflict and medical adherence. Journal of Pediatric Psychology, 38, 859–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psihogios AM, Kolbuck V, & Holmbeck GN (2015). Disease self-management in pediatric spina bifida: A longitudinal investigation of medical adherence, responsibility-sharing, and independence skills. Journal of Pediatric Psychology, 40, 790–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed-Knight B, Blount RL, & Gilleland J (2014). The transition of health care responsibility from parents to youth diagnosed with chronic illness: A developmental systems perspective. Families, Systems, & Health, 32(2), 219–234. 10.1037/fsh0000039 [DOI] [PubMed] [Google Scholar]
- Roach JW, Short BF, & Saltzman HM (2011). Adult consequences of spina bifida: A cohort study. Clinical Orthopaedics and Related Research, 469(5), 1246–1252. 10.1007/s11999-010-1594-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawin KJ (2017). Definitions, frameworks, and theoretical issues in self-management. Journal of Pediatric Rehabilitation, 10, 169–176. [Google Scholar]
- Sawin KJ, & Bellin MH (2010). Quality of life in individuals with spina bifida: A research update. Developmental Disabilities Research Reviews, 16(1), 47–59. 10.1002/ddrr.96 [DOI] [PubMed] [Google Scholar]
- Sawin KJ, Margolis R, Bookman JRM, Bellin MH, Logan LR, Woodward J, & Brei TJ (2020). Analysis of self-management and transition readiness instruments for clinical practice. In Betz CL & Coyne IT (Eds.), Transition from pediatric to adult healthcare services for adolescents and young adults with long-term conditions (pp. 71–109). Cham, Switzerland: Springer. [Google Scholar]
- Sawin KJ, Rauen K, Bartelt T, Wilson A, O’Connor RC, Waring WP III, & Orr M (2015). Transitioning adolescents and young adults with spina bifida to adult healthcare: Initial findings from a model program. Rehabilitation Nursing, 40(1), 3–11. [DOI] [PubMed] [Google Scholar]
- Sawyer SM, & Macnee S (2010). Transition to adult health care for adolescents with spina bifida: Research issues. Developmental Disabilities Research Reviews, 16(1), 60–65. 10.1002/ddrr.98 [DOI] [PubMed] [Google Scholar]
- Schwartz LA, Brumley LD, Tuchman LK, Barakat LP, Hobbie WL, Ginsberg JP, … Deatrick JA (2013). Stakeholder validation of a model of readiness for transition to adult health care. JAMA Pediatrics, 167, 939–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeley A, & Lindeke L (2017). Developing a transition care coordination program for youth with spina bifida. Journal of Pediatric Health Care, 31(6), 627–633. [DOI] [PubMed] [Google Scholar]
- West C, Brodie L, Dicker J, & Steinbeck K (2011). Development of health support services for adults with spina bifida. Disability and Rehabilitation, 33(22–23), 2381–2388. [DOI] [PubMed] [Google Scholar]
- Wood D, Bruner JS, & Ross G (1976). The role of tutoring in problem solving. Journal of Child Psychology and Psychiatry, 17, 89–100. [DOI] [PubMed] [Google Scholar]
- Wood D, Rocque B, Hopson B, Barnes K, & Johnson KR (2019). Transition Readiness Assessment Questionnaire Spina Bifida (TRAQ-SB): Specific module and its association with clinical outcomes among youth and youth adults with spina bifida. Journal of Pediatric Rehabilitation Medicine, 12, 405–413. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Taylor A, Hough BS, Linscheid TR, Yeates KO, & Naglieri JA (1996). Deviation from developmentally appropriate self-care autonomy. Association with diabetes outcomes. Diabetes Care, 19(2), 119–125. [DOI] [PubMed] [Google Scholar]
- Young NL, Wedge J, McCormick A, Fehlings D, Mills W, Mukherjee S, … Law M (2006). The transition study: A look at youth and adults with cerebral palsy, spina bifida, and acquired brain injury. Physical & Occupational Therapy in Pediatrics, 26(4), 25–45. [PubMed] [Google Scholar]
- Zukerman JM, Devine KA, & Holmbeck GN (2011). Adolescent predictors of emerging adulthood milestones in youth with spina bifida. Journal of Pediatric Psychology, 36(3), 265–276. 10.1093/jpepsy/jsq075 [DOI] [PMC free article] [PubMed] [Google Scholar]


