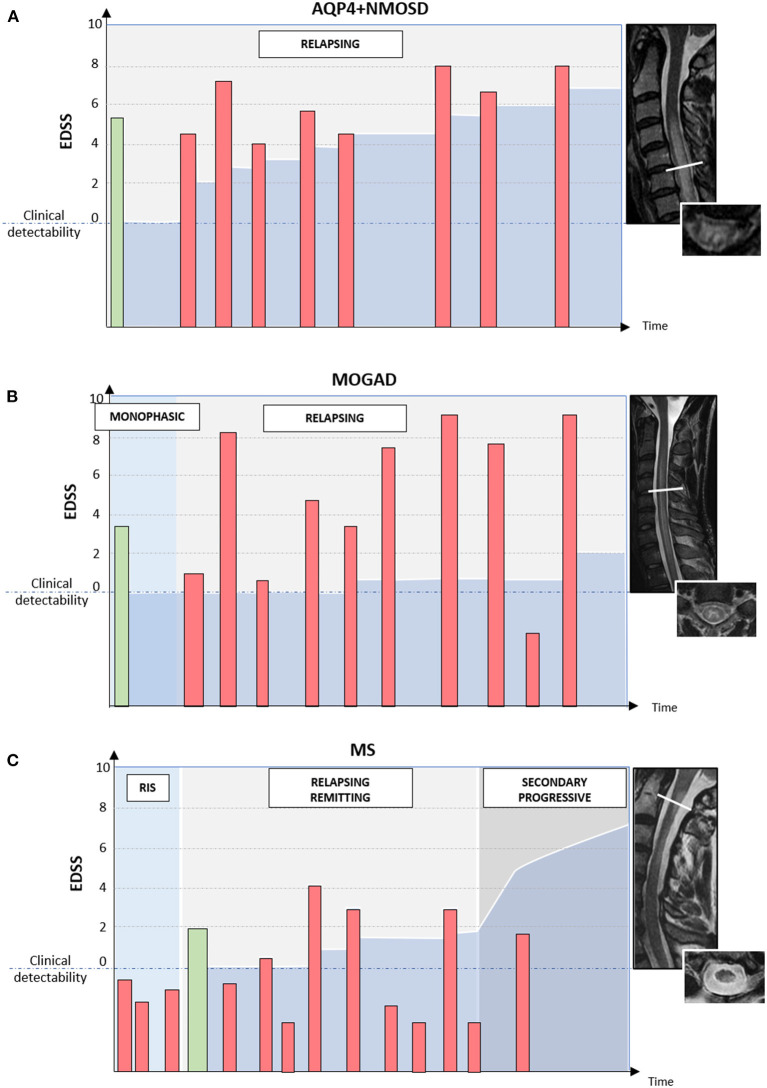
Figure 4.
Different disease courses and patterns of disability accrual in AQP4-IgG-positive neuromyelitis optica spectrum disorder (AQP4+NMOSD), MOG-IgG-associated disease (MOGAD), and multiple sclerosis (MS). Red bars = disease relapses; green bars = first clinical attack; darker blue area in the bottom half of each diagram = accumulated disability. In patients with AQP4+NMOSD (A) disease relapses are almost always clinically manifested with severe disability and often incomplete recovery between attacks. Disability accumulates in a stepwise fashion. In patients with MOGAD (B) disease attacks are similarly severe to those observed in NMOSD but post-attack recovery is generally complete or nearly complete. Long-term outcomes in MOGAD are often favorable with less disability accumulation (B). Lastly, in patients with MS (C) disease relapses are typically of mild-moderate severity and often do not cross the threshold for clinical detectability. For this reason, the first clinical attack often occurs in patients with MRI evidence of prior asymptomatic lesions. When these lesions are detected incidentally during the diagnostic workup for other disorders (e.g., headache), before the presenting MS attack, a radiologically isolated syndrome (RIS) can be diagnosed. When clinically manifested, MS attacks tend to result in complete or nearly complete clinical recovery in most cases (relapsing-remitting MS); while progressive disability accumulation can be seen in a minority of cases either from disease onset (primary progressive MS) or after an initially relapsing-remitting course (secondary progressive MS). Progressive disability generally occurs in the form of progressive motor impairment in MS, which often coincides with the development of focally atrophic lesions in the spinal cord lateral columns.