Figure 3. Possible mechanisms of chemotherapy resistance in the testes.
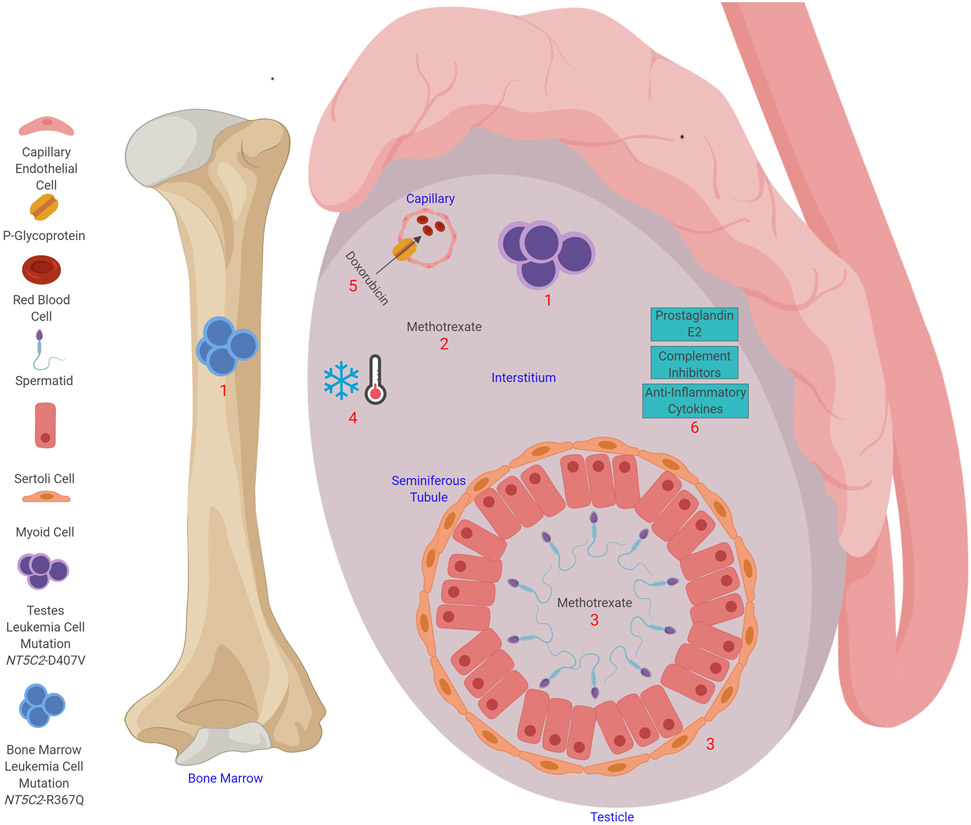
Testicular leukemia relapse is considered to occur as a result of insufficient exposure to chemotherapy. (1) Leukemia relapse in the testes can develop from a clone that is independent of the one seen in the bone marrow relapse; in a patient with relapsed ALL, the testicular leukemia cells were found to have an NT5C2-D407V mutation, whereas the bone marrow cells had an NT5C2-R367Q mutation. (2) The chemotherapy concentration can be reduced in the interstitium; for example, methotrexate levels in the interstitium are lower than those in the serum by a factor of two to four. (3) Tight junctions between the myoid cells and Sertoli cells prevent the entry of large molecules into the seminiferous tubule. Methotrexate levels in seminiferous tubule are lower than those in the serum by a factor of 18 to 50. (4) The testes are 2.5°C colder than the body temperature, which could decrease the efficacy of chemotherapy. (5) P-glycoprotein can export chemotherapy agents (e.g., doxorubicin) from the testes into capillaries. (6) Prostaglandin E2, anti-inflammatory cytokines, and complement inhibitors in the testes help to make the testes an immune-privileged site.
