Abstract
Cracked tooth is a common dental hard tissue disease.The involvement of cracks directly affects the selection of treatment and restoration of the affected teeth.It is helpful to choose more appropriate treatment options and evaluate the prognosis of the affected tooth accurately to determine the actual involvement of the crack.However, it is often difficult to accurately and quantitatively assess the scope of cracks at present.So it is necessary to find a real method of early quantitative and non-destructive crack detection.This article reviews the current clinical detection methods and research progress of cracked tooth in order to provide a reference for finding a clinical detection method for cracked tooth.
Keywords: Cracked tooth, Quantitative detection, Nondestructive, Diagnosis
1. Introduction
Referring to the standards of American Association of Endodontists (AAE),the classification of cracked teeth:(1)Craze lines,the crack is visible which only involves enamel.(2)Fractured cusp, the crack originating from the crown extending to the dentin and terminating at the cervical region.(3)Cracked tooth,the crack extending from the occlusal to the apical direction. (4)Split tooth,the crack that completely splits along the mesial and distal direction and extends to the marginal ridge of the tooth (5)Vertical root fracture(VRF) [1]. Among them, cracked tooth is a common dental hard tissue disease.The crack is the way for bacteria to invade the dental pulp.And the deeper the bacteria are colonized in the crack, the more serious the inflammatory reaction of the dental pulp is[2]. Subgingival cracks may lead to isolated narrow, deep periodontal pockets that can act as a pathway for bacterial invasion and may also lead to tooth loss[3]. Therefore,cracked tooth is the third major cause of tooth loss after caries and periodontal disease[4], [5]. Its etiology mainly includes large and complex fillings, defective cavity design,developmental defect of fossa and groove, abrasion, dental erosion and caries, excessive occlusal force, bruxism and occlusal trauma. The clinical symptoms of teeth are usually related to the depth and direction of cracks[6]. Nevertheless,whether the diagnosis,the treatment or the prognosis evaluation of affected teeth has always been a challenge for clinicians[7], [8]. The evaluation method of cracked tooth has even become the primary research topic according to American Association of Endodontists Foundation[9].
For patients with cracked tooth,if the condition is not controlled in time,the gradual deepening of crack may cause pulpitis and periodontal lesions.Therefore timely and appropriate diagnosis and treatment are essential in order that preserving the affected teeth and reducing the pain of the patients[10]. However, due to the concealment of cracked tooth in the early stage and the complex manifestations after combined with pulpitis or periodontal lesions,the cracked tooth is easy to be confused with other diseases, resulting in difficulties in clinical diagnosis and treatment. Therefore, how to effectively diagnose and treat cracked tooth has always been a hot and tough issue concerned by many clinical workers[11].
2. Diagnosis of cracked tooth
Clinically, the diagnosis of cracked tooth is often diagnosed by combining the patient's medical history to assist clinical examination and auxiliary examination results.Currently, the particular examination methods for cracked teeth include bite tests,dye tests and transillumination,etc.
2.1. Probing
Probing may be used to explore the suspected area of a cracked tooth. Patients often feel sharp pain when probing is applied to the crack[12].
2.2. Bite test
Bite test is also important, in which patients may show severe pain when they bite a cotton roll or cotton swab with the affected tooth. Severe pain caused by the release of occlusal pressure is the typical feature of cracked tooth.The location, direction and depth of the crack determine the mode of occlusal pain[13], [14]. It should be emphasized that the bite tests may not be able to distinguish pain between maxillary and mandibular origin. Moreover,the application of force is risky to the affected tooth and may cause further crack propagation, so it is sometimes not recommended[15], [16], [17].
2.3. Vitality test
The sensitivity to temperature stimulation usually indicates that proximal or near-pulp cracks.The high sensitivity to cold stimulation and the positive of bite test can diagnose cracked tooth [14], [18]. Kim et al. [19] believed that root canal therapy should be performed when there is obvious cold stimulation pain in cracked tooth.
2.4. Dye test
Dyes can be used to dye cracks in order to see cracks clearly. Commonly used dyes include methylene blue, iodine tincture and gentian violet.However,this method may take several days to see the effect,or even require wearing a temporary crown[18]. Furthermore, the dye test can only detect the location of the crack but have difficulty in assessing progress. Besides,when bacteria enter the crack,the decay is easy to be colored but the dye is difficult to remove, that will affect aesthetics and repair.The toxicological effect of dyes is unknown which limits its application[20], [21].
2.5. Transillumination
Transillumination refers to the use of light guide fibers to illuminate the tooth surface and the light perpendicular to the crack will be diffracted, thereby locating the crack[22]. The yellow light is more capable to diagnose cracks[15]. Some scholars have specially designed a crack detection lamp with appropriate brightness which can not only refract at the crack but also facilitate the observation of clinicians[23]. Other studies have also shown that 810 nm diode laser or 1300–1310 nm near infrared laser has good targeting ability for cracks[24], [25], [26]. If there is a large area of filling in the affected tooth, the original filling should first be removed to assess the degree of cracking, the condition of the pulp, and the remaining tooth tissue structure[18].
2.6. Microscope detection
It is difficult to detect on naked-eye visual inspection when the crack width is less than 18 µm, and dental surgery microscope can be used to assist in locating cracks[5], [27], [28].
2.7. Periodontal probing
The presence of separate, narrow, deep periodontal pockets at a site of the suspicious tooth may indicate a hidden crack extending subgingival.The depth of the periodontal pocket may mediately reflect the extension of the crack to the subgingival indirectly.Due to the deep periodontal pocket could also be used as a bacterial invasion route to infect the pulp.Studies have shown that the rate of pulp necrosis is higher for affected teeth with periodontal probing depth greater than 4 mm caused by cracks.Moreover,when the depth of narrow deep periodontal pocket was more than 4 mm caused by cracks, that may have a unfavourable prognosis.[3], [19].
2.8. Others
2.8.1. Auxiliary diagnosis band
When the above methods still fail to diagnose, a stainless steel orthodontic band can also be worn on the suspicious teeth.If the clinical symptoms of the patients are relieved after 2–4 weeks, the diagnosis is correct.In addition,the band can be used to fix the cleft teeth as external splint[29], [30].
2.8.2. Quantitative percussion diagnostics
Quantitative percussion diagnostics (QPD) are commonly used to detect peri-implant osteointegration.And due to the presence of cracks, the tooth tissue on both sides of the crack can be slightly moved under the action of QPD[31], so QPD can be used to detect hidden cracks and locate the presence of cracks that cannot be detected by light transmission,for instance,the cracks where were interproximal or beneath the gingival/bone complex[32], [33].
2.9. Imageological examination
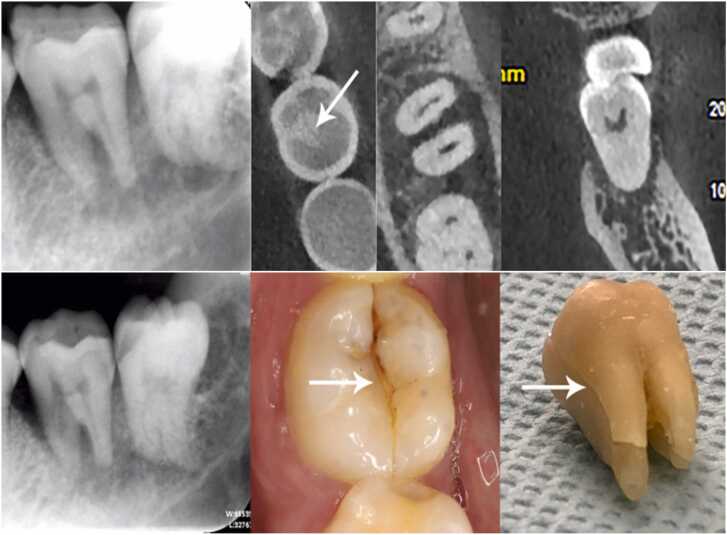
Periapical films are commonly used for dental clinical examination, but their ability to identify tooth cracks is not ideal. Cracks can be mediately judged by the situation of periodontal or periapical bone (as shown in Fig. 1)[34]. As a clinical quantitative analysis method at present, Cone Beam Computed Tomography(CBCT) is not ideal for the identification of cracks.Some literatures have pointed out that CBCT is still difficult to identify cracked tooth with a width of less than 50 µm even under appropriate parameters[35]. Guo XL et al. [36] scanned artificial root cracks by combining different voxel parameters with different CBCT units and the experimental results showed that the selected parameters of CBCT affected the identification of root cracks. However, due to the different parameters of each machine and the difficulty of clinicians to adjust the parameters,CBCT is not clinically effective in diagnosing cracked tooth.In addition,studies have shown that cracks are easily secondary to the filling[37], and the filling is generally high-density under CBCT. The influence of filling artifacts makes it more difficult to identify cracked tooth under CBCT[38], [39], [40].
Fig. 1.
There was no obvious crack image on the apical film, but there was obvious bone destruction around the root of the affected tooth. Extensive bone destruction surrounding the root can serve as a diagnostic reference for root-involving fractures[41].
3. Quantitative evaluation of cracked tooth
The choice of treatment plan for cracked tooth depends on the stage of the development of the disease, however, the clinical examination methods available at this stage are still arduous to judge the extent of cracks,the relationship between crack and dental pulp,and the subgingival extension.For clinicians, the diagnosis and treatment implementation are difficult problems. Frankly speaking,the judgment of the condition of cracked tooth mostly depends on the subjective analysis of dentists, which will inevitably cause patients' doubts and misjudgment. The diagnosis and judgment of cracked tooth have always been a long-standing problem[42]. Delay in treatment leads to crack propagation, bacterial invasion leads to pulp infection, and finally causing serious pulp and periodontal disease,which becomes the main cause of tooth loss [43], [44], [45], [46], [47]. Therefore, the early diagnosis and treatment of cracked tooth are very important in relieving pain, restoring the function of the affected teeth and improving prognosis. Early detection and diagnosis are important to limit crack propagation [10], [48]. It is essential to find a method that can be used for clinical quantitative evaluation of cracked tooth.
3.1. MicroCT
MicroCT has a high recognition rate,which can locate cracks with a width of a few tenths to tens of microns and identify enamel and dentin accurately[49], [50]. Generally, it is used as the gold standard for crack detection in cracked teeth research. However,because of its high restrictions on the volume of the detection sample and the long detection time, it is generally only used in researches[51], [52]. Moreover, MicroCT is not considered as suitable method for diagnosis of tooth crack in routine clinical practice because of the high radiation doses which violates the concept"as low as reasonably achievable"(ALARA)[53], [54].
3.2. OCT/SS-OCT
Optical coherence tomography (OCT) is a noninvasive imaging method, which can provide high-resolution cross-sectional images of biological internal tissues[55]. It uses infrared light wave to reflect internal microstructure, which is similar to ultrasonic pulse echo in principle[56], [57]. At present, it has been applied in several clinical departments such as ophthalmology, cardiology and dermatology[58], [59], [60]. As one of the derivatives of OCT, swept-source optical coherence tomography (SS-OCT) is an ideal scheme that can break through the speed bottleneck of OCT. SS-OCT uses a longer wavelength for imaging deeper biological tissue penetration.In addition, the swept frequency light source has high transient coherence so that it can achieve a deeper longitudinal imaging range.Moreover,SS-OCT system can provide extremely high imaging speed[61]. Studies have shown that SS-OCT has high sensitivity and specificity in detecting caries and cracked tooth, especially at near-infrared wavelengths of 1310 nm[62], [63]. Both in vivo and in vitro experiments have proved the possibility of SS-OCT for the detection of cracked tooth [63], [64], [65]. Although the main experimental subjects were cracks in the enamel layer, the experimental results of Imai K showed that SS-OCT has the ability to recognize the enamel and dentin layer and can identify cracks in the dentin layer.Due to its shallow penetrating depth of about 3 mm, the use of SS-OCT is limited [62]. The ability of SS-OCT to identify full-thickness cracks in tooth hard tissue remains to be promoted [66]. OCT and SS-OCT is difficult to image root crack at sub-gingival zone.In addition, the long detection time, the difficulty of avoiding motion artifacts, limited penetration depth and scanning range,the influence of the special optical characteristics of tooth hard tissue on the detection results and the high cost of equipment are all the difficulties faced by SS-OCT in the detection of cracked teeth [62], [67], [68], [69]. At the same time, the contrivance of adaptive probe is necessary with the objective to ensure the operability of oral clinic[70].
3.3. Magnetic resonance imaging
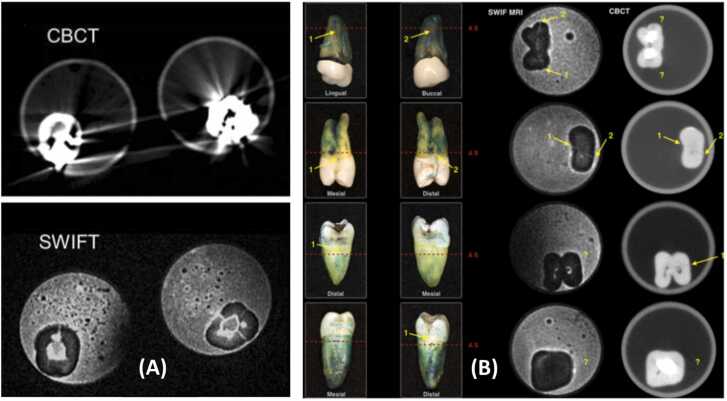
Magnetic Resonance Imaging (MRI) is a common method of soft tissue examination, which is often used to diagnose temporomandibular diseases and maxillofacial tumors in oral clinics [71]. In recent years, it has also been applied to the diagnosis of dental diseases [72], [73], [74]. However, the hard tissue of the tooth has low hydrogen density, less binding water, and short relaxation time cause the low signal dental hard tissue shows in MRI,which is difficult to capture.Some scholars use ultrashort echo capture time technology to display the mineralized tissue of tooth, such as sweep image with fourier transformation (Swift) to obtain the clearer signal of tooth hard tissue [75]. In terms of the diagnosis of cracked tooth,the presence of water in the crack produces positive contrast enhancement through two mechanisms:First, the concentration of water in the crack is at least five times higher than that of dentin[76];Second, the lateral relaxation rate of active water in the crack (=1/t2) is much smaller than the water component confined in the dentin pore, which makes the signal of water in the crack less ambiguous [77]. TylerJ. Schuurmans [78] concluded by comparing the MRI and CBCT's detection results of root cracks in excised teeth after root filling that MRI is better than CBCT in identifying partial hidden cracks and root filling or crown filling has little effect on MRI imaging(as shown in Fig. 2). Djat Idiyatullin et al. [79] used gradient recalled echo (GRE) and SWIFT MRI to detect two tooth cracks in vitro, and the results showed that SWIFT MRI could detect the cracks as small as 20 µm.Generally, MRI examination takes a long time. When examining small volume tissues, routine scanning is prone to artifacts due to patient movement. The research results of Djaudat team also show that the scanning time of SWIFT MRI for cracked tooth can be controlled at about 10 min, which creates a possibility for its practical application in the clinical detection of cracked tooth [80]. Therefore, MRI is expected to become a detection method of tooth cracked tooth but the detection sensitivity of MRI needs to be improved and high price for a tooth examination needs to be considered.
Fig. 2.
(A) MRI can identify some hidden cracks and is less affected by filler artifacts, (B) but the ability to identify hidden cracks is unstable.[78,79].
3.4. Contrast medium-assisted imaging
Contrast medium is a commonly used imaging auxiliary means,the principle of which is to inject contrast medium into demic tissues or organs to improve the imaging contrast for the sake of achieving the observation purpose [81]. Commonly used contrast include gastrointestinal barium, indocyanine green for retinography and iodine reagent for angiography,etc.This provides a new direction for dental radiography. Theoretically, after the contrast medium is introduced into the crack, the crack is easier to identify when the transmission density under X-ray is higher than that of tooth hard tissue(as shown in Fig. 3). Matthew DL [50] et al. soaked 10 human molars in barium chloride solution and sodium sulfate solution for three days respectively to form BaSO4 precipitate and immerse them in the teeth cracks. The microCT`s ability of identification of cracked tooth after introduction to the contrast medium was improved. Additionally,the results showed that some cracks which could not be detected by ordinary scanning could be detected after dyeing. The results showed that the cracks only involving the enamel could not be identified after BaSO4 staining.It may be acceptable for barium chloride and sodium sulfate to be contained in the mouth.But the excised teeth need to be soaked in the solution for three days in this experiment, otherwise the dye can not completely immerse in the crack or reach the recognition concentration,so it is difficult to meet the identification conditions clinically.Based on the previous experiment [82], [83]. Li Z et al. used indocyanine green-assisted near-infrared dental imaging to quantitatively detect cracked tooth.The experimental results showed that when using a preestablished detection system and the projection light transilluminates the crack at a vertical angle, the crack depth obtained by analyzing the size of the dark area behind the crack is almost equal to the actual crack depth[84]. Ioversol was also used to assist CBCT in imaging cracks. The results showed that with the aid of Ioversol, CBCT's ability to identify cracks is significantly improved. This imaging method can only mark the length of crack in the direction of the long axis of the tooth, and the distribution and direction of crack are usually irregular, which reduces the accuracy of the detection results [85]. Yuan M et al. [86] used meglumine diatrizoate(MD) as contrast medium to thoroughly soak 24 excised teeth with artificial cracks, and scanned the isolated tooth model with conventional and enhanced CBCT respectively.The results showed that MD enhanced CBCT could significantly improve the identification ability of cracks. Meanwhile,the team simulated a model of periodontal tissue in vitro. The team pointed out that due to the blocking of periodontal tissue, the contrast agent cannot be immersed into the root cracks, so this method is not suitable for the detection of subgingival cracked teeth.Furthermore, the team also pointed out that how to ensure that the contrast agent is immersed in the crack is also a difficult problem for the technology.Considering that the permeability and fluidity of the contrast medium directly affect the ability of the medium to penetrate the crack, and the saliva environment will affect the concentration of the water-soluble contrast medium as well [86], [87]. Team of Hu further selected the NaI+DMSO combination which has better permeability.Comparing the identification ability of cracks under CBCT between the new contrast medium combintion and previously MD in the saliva environment, it is concluded that the new combination with better permeability has stronger ability to identify crack in the saliva environment [87].
Fig. 3.
Contrast medium can enhance the ability of CBCT to identify cracked teeth, so that CBCT can recognize some previously undetectable cracks[86].
3.5. Nondestructive testing technology
As an essential technology to ensure product quality and equipment safety, non-destructive testing has been widely used in aviation, aerospace, military industry, railway, nuclear power, metallurgy, special equipment, automobile manufacturing, petrochemical and other fields. Conventional nondestructive testing includes X-ray testing, ultrasonic testing, magnetic particle testing, penetration testing, eddy current testing as well as acoustic emission testing, infrared testing and so on [88]. Some scholars tried to apply these nondestructive testing techniques to the detection of tooth hard tissue(The results of some nondestructive testing for cracked tooth are shown in Fig. 4).
Fig. 4.
A variety of nondestructive testing methods have been tried to quantify the cracked teeth.(A)(B)(C) separately show that the identification of optical polarization imaging system,Vibrothermography and X-ray dark field tomography of carcked tooth[101], [106], [108].
3.5.1. Ultrasonic testing technology
Ultrasonic testing technology is a nondestructive testing method, which has the characteristics of wave length, high resolution and no danger. It is expected to be used in the detection of human teeth[89], [90], [91]. Ultrasonic has the ability to penetrate the hard structure and it is very effective in detecting physical discontinuities. It can even detect cracks more narrow than the wavelength, which lays a theoretical foundation for ultrasonic wave to detect cracked teeth.Culjat MO et al. simulated a set of ultrasonic detection system that can be used to detect cracked tooth, which provided a theoretical basis for the application of ultrasonic testing in cracked tooth detection [92]. However, the traditional ultrasonic technology is a contact measurement method, which needs couplant mediated contact. Due to the small dimension of human teeth and the tiny operation space in the mouth, traditional ultrasonic testing is not suitable for tooth testing [93].
3.5.2. Laser ultrasonic technology
Laser ultrasonic (LU) technology is a new nondestructive testing method, which uses pulsed laser to generate ultrasonic and describes the defect characteristics by detecting the reflection, scattering and attenuation of ultrasonic signals [94], [95], [96]. The laser can focus on small objects with complex shapes in a non-contact way which solves the problem of insufficient operating space.The laser energy of LU can be kept at a low level to ensure lossless thermoelastic operation that making it appropriate for crack detection [93]. Kaihua S [97] preliminarily applied laser ultrasonic nondestructive testing to the detection of cracked tooth, and his team constructed a set of laser ultrasonic testing system which can be used to detect human teeth.They successfully measured the depth of cracks involving the enamel layer on the labial surface of two anterior teeth and the feasibility of the application of LU testing in the detection of cracked tooth was verified by using a three-dimensional finite element model. However, the hard tissue of the tooth is not a single structure and has special optical properties.It is still difficult to successfully establish a complete LU detection system for cracked teeth.In addition, when using LU detection system, we should pay attention to the influence of laser on tooth hard tissue, dental pulp and periodontal tissue.It has been pointed out that some patients may feel pain when locating cracked teeth with semiconductor laser of 810 nm, and the pain of individual patients can last for one second in spite of there is no evidence that the pulp inflammation of individual teeth after several years is directly related to laser irradiation [24]. In addition, laser irradiation can also cause structural damage to tooth hard tissue [98], [99]. At the same time, whether the vibration of tooth hard tissue caused by irradiation will extend the crack range needs to be further verified [93].
3.5.3. Optical polarization imaging system
Based on the optical birefringence characteristics of the tooth surface [100],Tien YH et al. [101] constructed an optical polarization imaging system and used this system to detect the excised teeth with cracks.The results show that the system can preliminarily detect the cracks,but the detection results are not completely consistent with the actual depth on the tissue section.
3.5.4. Quantitative light induced fluorescence
Quantitative light induced fluorescence (QLF) is a new optical technology for the diagnosis of dental caries and the detection of dental plaque [102]. Some researches have tried to use it in cracked tooth detection, and the improved system considers using the maximum fluorescence loss value to preliminarily evaluate depth of crack.The results showed that the maximum fluorescence loss value increases with the increase of crack depth, and there is a close correlation between the crack depth and the maximum fluorescence loss value. The clinical test results show that the improved system is expected to be used in enamel crack detection [103], [104].
3.5.5. Photoacoustic tomography
Photoacoustic tomography (PAT) is a new non-destructive and noninvasive biomedical imaging technology, which has been used in enamel crack detection [105].
3.5.6. Anisotropic X-ray dark field tomography
The research of anisotropic X-ray dark field tomography (XDT) provides a theoretical basis for XDT in the detection of tooth cracked teeth[106].
3.5.7. Digital image processing system
In addition,Chunliangzhang[107] et al. established a set of digital image processing system to simulate the stress change of cracked teeth during chewing, which provides a new reference method for clinical diagnosis of cracked teeth.
3.5.8. Vibrothermography
The principle of Vibrothermography (VibroIR) is that the defect generates heat by friction under ultrasonic vibration.And the defect is detected by the temperature change,moreover,the smaller the crack width is the more obvious the temperature change is.Matsushita TM[108] et al. tried to detect artificially created cracks extending to the root with different parameters of VibroIR.The experimental results show that the depth of dentin crack can be detected by using VibroIR under appropriate parameters.However, whether vibration will increase the crack range and its effect on dental pulp needs to be considered.
The application of nondestructive testing technology in industry and other fields is becoming more and more mature, and extending it to more disciplines will be the direction that related majors should strive for.
4. Conclusion
Since the quantitative detection of tooth crack can be classified as the nondestructive detection of cracks in hard tissue.The methods that can be used for nondestructive and quantitative detection of cracks could equally apply to cracked tooth.And the special physical and chemical properties of tooth can also be considered as the direction of detection.However,it is due to the special properties of teeth, the multi-layer structure of dental hard tissue, the non-solid structure of dentin and the limited space and time for clinical operation that have brought great difficulties to the detection.In addition,whether routine non-destructive testing is truly non-destructive to teeth, whether the detection will affect the health of the pulp, whether it restricts or affects periodontal tissue, and whether cracks deepen as a result of testing are all questions that should be considered in researches.Therefore, after trying to detect cracks in vitro, it should be used with caution when it is really used clinically.
Conflicts of Interest
The authors declare no conflict of interest.
Acknowledgements
The financial support from the Science and technology Project of the Jilin Provincial Department of Finance, China (JCSZ2021893-26) , is gratefully acknowledged.
Footnotes
Jilin Scientific and Technological Development Program.Award Number: jcsz2021893–26 | Recipient: YuYan Liu
References
- 1.American association of endodontists.cracking the cracked tooth code, Endodontics: Colleagues for Excellence , 1997.
- 2.Kahler B., Moule A., Stenzel D. Bacterial contamination of cracks in symptomatic vital teeth. Aust Endod J. 2000;26:115–118. doi: 10.1111/j.1747-4477.2000.tb00296.x. [DOI] [PubMed] [Google Scholar]
- 3.Yang S.E., Jo A.R., Lee H.J., Kim S.Y. Analysis of the characteristics of cracked teeth and evaluation of pulp status according to periodontal probing depth. BMC Oral Health. 2017;17:135. doi: 10.1186/s12903-017-0434-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.W. Geurtsen, T. Schwarze, H. Gunay, Diagn, Ther, Prev Crack tooth Syndr Quintessence Int, 34, 2003, pp. 409–417. [PubMed]
- 5.Mamoun J.S., Napoletano D. Cracked tooth diagnosis and treatment: an alternative paradigm. Eur J Dent. 2015;9:293–303. doi: 10.4103/1305-7456.156840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li L., Luo X. Research progress in diagnosis and treatment of cracked teeth. J Clin Stomatol. 2017;33:372–374. [Google Scholar]
- 7.Sim I.G., Lim T.S., Krishnaswamy G., Chen N.N. Decision making for retention of endodontically treated posterior cracked teeth: a 5-year follow-up study. J Endod. 2016;42:225–229. doi: 10.1016/j.joen.2015.11.011. [DOI] [PubMed] [Google Scholar]
- 8.Kang S.H., Kim B.S. Cracked teeth: distribution and survival at 6 months, 1 year and 2 years after treatment. J Formos Med Assoc. 2016;42:557–562. doi: 10.1016/j.jfma.2021.03.020. [DOI] [PubMed] [Google Scholar]
- 9.Foundation AAOE, Endodontic research guidelines, in: Chicago IAAO (Ed.), 2004.
- 10.Ellis S.G. Incomplete tooth fracture--proposal for a new definition. Br Dent J. 2001;190:424–428. doi: 10.1038/sj.bdj.4800992. [DOI] [PubMed] [Google Scholar]
- 11.Zhao J. Research progress in clinical diagnosis and treatment of cracked teeth with pulpitis. Electron J Gen Stomatol. 2019;6:12–15. [Google Scholar]
- 12.Sadasiva K., Ramalingam S., Rajaram K., Meiyappan A. Cracked tooth syndrome: a report of three cases. J Pharm Bioallied Sci. 2015;7:S700–S703. doi: 10.4103/0975-7406.163482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mathew S., Thangavel B., Mathew C.A., Kailasam S., Kumaravadivel K., Das A. Diagnosis of cracked tooth syndrome. J Pharm Bioallied Sci. 2012;4:S242–S244. doi: 10.4103/0975-7406.100219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.E.B. Lubisich, T.J. Hilton, J. Ferracane, Crack teeth: a Rev Lit J Esthet Restor Dent, 22, 2010, pp. 158–167. [DOI] [PMC free article] [PubMed]
- 15.Banerji S., Mehta S.B., Millar B.J. The management of cracked tooth syndrome in dental practice. Br Dent J. 2017;222:659–666. doi: 10.1038/sj.bdj.2017.398. [DOI] [PubMed] [Google Scholar]
- 16.Seo D.G., Yi Y.A., Shin S.J., Park J.W. Analysis of factors associated with cracked teeth. J Endod. 2012;38:288–292. doi: 10.1016/j.joen.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 17.Y. Yang, G. Chen, F. Hua, Q. Yu, W. Yang, Biting Pain Reprod tooth slooth: aid Early Diagn Crack tooth Quintessence Int, 50, 2019, pp. 82–87. [DOI] [PubMed]
- 18.Banerji S., Mehta S.B., Millar B.J. Cracked tooth syndrome: Part 1: aetiology and diagnosis. Br Dent J. 2010;208:459–463. doi: 10.1038/sj.bdj.2010.449. [DOI] [PubMed] [Google Scholar]
- 19.Kim S.Y., Kim S.H., Cho S.B., Lee G.O., Yang S.E. Different treatment protocols for different pulpal and periapical diagnoses of 72 cracked teeth. J Endod. 2013;39:449–452. doi: 10.1016/j.joen.2012.11.052. [DOI] [PubMed] [Google Scholar]
- 20.Hasan S., Singh K., Salati N. Crack tooth syndrome: overview of literature. Int J Appl Basic Med Res. 2015;5:164–168. doi: 10.4103/2229-516X.165376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pai S. Diagnosis and management of cracked tooth- decision analysis. Biosci Biotechnol Res Commun. 2020;13:457–463. [Google Scholar]
- 22.Bhanderi S. Facts about cracks in teeth. Prim Dent J. 2021;10:20–27. doi: 10.1177/2050168420980987. [DOI] [PubMed] [Google Scholar]
- 23.Liewehr F.R. An inexpensive device for transillumination. J Endodont. 2001;27:130–131. doi: 10.1097/00004770-200102000-00019. [DOI] [PubMed] [Google Scholar]
- 24.Sapra A., Darbar A., George R. Laser-assisted diagnosis of symptomatic cracks in teeth with cracked tooth: a 4-year in-vivo follow-up study. Aust Endod J. 2020;46:197–203. doi: 10.1111/aej.12391. [DOI] [PubMed] [Google Scholar]
- 25.Fried W.A., Simon J.C., Lucas S., Chan K.H., Darling C.L., Staninec M., et al. Near-ir imaging of cracks in teeth. Proc SPIE Int Soc Opt Eng. 2014;8929:89290Q. doi: 10.1117/12.2045686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Staninec M., Lee C., Darling C.L., Fried D. In vivo near-ir imaging of approximal dental decay at 1,310 nm. Lasers Surg Med. 2010;42:292–298. doi: 10.1002/lsm.20913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clark D.J., Sheets C.G., Paquette J.M. Definitive diagnosis of early enamel and dentin cracks based on microscopic evaluation. J Esthet Restor Dent. 2003;15(391–401):401. doi: 10.1111/j.1708-8240.2003.tb00963.x. [DOI] [PubMed] [Google Scholar]
- 28.Hu H., Liu J., Zhang H. Application of operating microscope in diagnosis and treatment of cracked teeth. J Clin Stomatol. 2010;26:410–411. [Google Scholar]
- 29.S. Banerji, S.B. Mehta, B.J. Millar, Cracked tooth syndrome Part 2: Restor Options Manag Crack tooth Syndr Br Dent J, 208, 2010, pp. 503–514. [DOI] [PubMed]
- 30.Batalha-Silva S., Gondo R., Stolf S.C., Baratieri L.N. Cracked tooth syndrome in an unrestored maxillary premolar: a case report. Oper Dent. 2014;39:460–468. doi: 10.2341/13-257. [DOI] [PubMed] [Google Scholar]
- 31.Poveromo S.L. Quantitative percussion diagnostics for evaluating bond integrity between composite laminates. [University of California, Irvine].
- 32.Sheets C.G.D., Stewart D.L.D., Wu J.C.D., Earthman J.C.P. An in vitro comparison of quantitative percussion diagnostics with a standard technique for determining the presence of cracks in natural teeth. J Prosthet Dent. 2014;112:267–275. doi: 10.1016/j.prosdent.2014.02.020. [DOI] [PubMed] [Google Scholar]
- 33.Sheets C.G., Wu J.C., Earthman J.C. Quantitative percussion diagnostics as an indicator of the level of the structural pathology of teeth: retrospective follow-up investigation of high-risk sites that remained pathological after restorative treatment. J Prosthet Dent. 2018;119:928–934. doi: 10.1016/j.prosdent.2017.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.J.O.A.L.A.F. Andreasen Textbook and color atlas of dental trauma Beijing People’s Med Publ House 2012.
- 35.Brady E., Mannocci F., Brown J., Wilson R., Patel S. A comparison of cone beam computed tomography and periapical radiography for the detection of vertical root fractures in nonendodontically treated teeth. Int Endod J. 2014;47:735–746. doi: 10.1111/iej.12209. [DOI] [PubMed] [Google Scholar]
- 36.Guo X.L., Li G., Zheng J.Q., Ma R.H., Liu F.C., Yuan F.S., et al. Accuracy of detecting vertical root fractures in non-root filled teeth using cone beam computed tomography: effect of voxel size and fracture width. Int Endod J. 2019;52:887–898. doi: 10.1111/iej.13076. [DOI] [PubMed] [Google Scholar]
- 37.Hilton T.J., Funkhouser E., Ferracane J.L., Gordan V.V., Huff K.D., Barna J., et al. Associations of types of pain with crack-level, tooth-level and patient-level characteristics in posterior teeth with visible cracks: findings from the national dental practice-based research network. J Dent. 2018;70:67–73. doi: 10.1016/j.jdent.2017.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khedmat S., Rouhi N., Drage N., Shokouhinejad N., Nekoofar M.H. Evaluation of three imaging techniques for the detection of vertical root fractures in the absence and presence of gutta-percha root fillings. Int Endod J. 2012;45:1004–1009. doi: 10.1111/j.1365-2591.2012.02062.x. [DOI] [PubMed] [Google Scholar]
- 39.Lofthag-Hansen S., Huumonen S., Grondahl K., Grondahl H.G. Limited cone-beam ct and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radio Endod. 2007;103:114–119. doi: 10.1016/j.tripleo.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 40.Moudi E., Haghanifar S., Madani Z., Alhavaz A., Bijani A., Bagheri M. Assess Vert root Fract Using cone-beam Comput Tomogr Imaging Sci Dent. 2014;44:37–41. doi: 10.5624/isd.2014.44.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gao A., Cao D., Lin Z. Diagnosis of cracked teeth using cone-beam computed tomography: literature review and clinical experience. Dentomaxillofac Radiol. 2021;50 doi: 10.1259/dmfr.20200407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Snyder D.E. The cracked-tooth syndrome and fractured posterior cusp. Oral Surg Oral Med Oral Pathol. 1976;41:698–704. doi: 10.1016/0030-4220(76)90181-x. [DOI] [PubMed] [Google Scholar]
- 43.Ricucci D., Siqueira J.J., Loghin S., Berman L.H. The cracked tooth: histopathologic and histobacteriologic aspects. J Endod. 2015;41:343–352. doi: 10.1016/j.joen.2014.09.021. [DOI] [PubMed] [Google Scholar]
- 44.Cohen S., Blanco L., Berman L. Vertical root fractures: clinical and radiographic diagnosis. J Am Dent Assoc. 2003;134:434–441. doi: 10.14219/jada.archive.2003.0192. [DOI] [PubMed] [Google Scholar]
- 45.Turp J.C., Gobetti J.P. The cracked tooth syndrome: an elusive diagnosis. J Am Dent Assoc. 1996;127:1502–1507. doi: 10.14219/jada.archive.1996.0060. [DOI] [PubMed] [Google Scholar]
- 46.Walton R.E., Michelich R.J., Smith G.N. The histopathogenesis of vertical root fractures. J Endod. 1984;10:48–56. doi: 10.1016/S0099-2399(84)80037-0. [DOI] [PubMed] [Google Scholar]
- 47.Lustig J.P., Tamse A., Fuss Z. Pattern of bone resorption in vertically fractured, endodontically treated teeth. Oral Surg Oral Med Oral Pathol Oral Radio Endod. 2000;90:224–227. doi: 10.1067/moe.2000.107445. [DOI] [PubMed] [Google Scholar]
- 48.CAMERON C.E. Cracked-tooth syndrome. J Am Dent Assoc. 1964;68:405–411. doi: 10.14219/jada.archive.1964.0108. [DOI] [PubMed] [Google Scholar]
- 49.Dumbryte I., Vailionis A., Skliutas E., Juodkazis S., Malinauskas M. Three-dimensional non-destructive visualization of teeth enamel microcracks using x-ray micro-computed tomography. Sci Rep. 2021;11:14810. doi: 10.1038/s41598-021-94303-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Landrigan M.D., Flatley J.C., Turnbull T.L., Kruzic J.J., Ferracane J.L., Hilton T.J., et al. Detection of dentinal cracks using contrast-enhanced micro-computed tomography. J Mech Behav Biomed Mater. 2010;3:223–227. doi: 10.1016/j.jmbbm.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 51.De-Deus G., Belladonna F.G., Silva E., Souza E.M., Carvalhal J., Perez R., et al. Micro-ct assessment of dentinal micro-cracks after root canal filling procedures. Int Endod J. 2017;50:895–901. doi: 10.1111/iej.12706. [DOI] [PubMed] [Google Scholar]
- 52.de Oliveira B.P., Camara A.C., Duarte D.A., Gomes A., Heck R.J., Antonino A., et al. Detection of apical root cracks using spectral domain and swept-source optical coherence tomography. J Endod. 2017;43:1148–1151. doi: 10.1016/j.joen.2017.01.019. [DOI] [PubMed] [Google Scholar]
- 53.Gabriella Lopes De Rezende Barbosa L.A.P.S. Micro-ct evaluation of the radioprotective effect of resveratrol on the mandibular incisors of irradiated rats. Braz Oral Res. 2016;30 doi: 10.1590/1807-3107BOR-2016.vol30.0168. S1806-83242016000100229. [DOI] [PubMed] [Google Scholar]
- 54.Frane N., Bitterman A. Radiat Saf Prot. 2022 [Google Scholar]
- 55.Yu Y., Wang H., Sun H., Zhang Y., Chen P., Liang R. Optical coherence tomography in fingertip biometrics. Opt Laser Eng. 2022;151 [Google Scholar]
- 56.Hajizadeh F.K.R. Introd Opt Coherence Tomogr. 2018 [Google Scholar]
- 57.Fujimoto J.G.D.W. Introduction to optical coherence tomography. Opt Coherence Tomogr. 2008:1–45. [Google Scholar]
- 58.Lavinsky F., Lavinsky D. Novel perspectives on swept-source optical coherence tomography. Int J Retin Vitr. 2016;2:25. doi: 10.1186/s40942-016-0050-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Su M.I., Chen C.Y., Yeh H.I., Wang K.T. Concise review of optical coherence tomography in clinical practice. Acta Cardiol Sin. 2016;32:381–386. doi: 10.6515/ACS20151026A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cao T., Tey H.L. High-definition optical coherence tomography - an aid to clinical practice and research in dermatology. J Dtsch Dermatol Ges. 2015;13:886–890. doi: 10.1111/ddg.12768. [DOI] [PubMed] [Google Scholar]
- 61.Huang Z., Hu Y., Zhou C., Lu Y., Ren Q., Liu G. Diagnosis and evaluation of early caries and cracked teeth by laser surface acoustic wave. Eye Sci. 2021;36:55–65. [Google Scholar]
- 62.Hsieh Y.S., Ho Y.C., Lee S.Y., Chuang C.C., Tsai J.C., Lin K.F., et al. Dental optical coherence tomography. Sensors. 2013;13:8928–8949. doi: 10.3390/s130708928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shimada Y., Sadr A., Sumi Y., Tagami J. Application of optical coherence tomography (oct) for diagnosis of caries, cracks, and defects of restorations. Curr Oral Health Rep. 2015;2:73–80. doi: 10.1007/s40496-015-0045-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lee S.H., Lee J.J., Chung H.J., Park J.T., Kim H.J. Dental optical coherence tomography: new potential diagnostic system for cracked-tooth syndrome. Surg Radio Anat. 2016;38:49–54. doi: 10.1007/s00276-015-1514-8. [DOI] [PubMed] [Google Scholar]
- 65.Kim J.M., Kang S.R., Yi W.J. Automatic detection of tooth cracks in optical coherence tomography images. J Periodontal Implant Sci. 2017;47:41–50. doi: 10.5051/jpis.2017.47.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Imai K., Shimada Y., Sadr A., Sumi Y., Tagami J. Noninvasive cross-sectional visualization of enamel cracks by optical coherence tomography in vitro. J Endod. 2012;38:1269–1274. doi: 10.1016/j.joen.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 67.Stanga P.E., Tsamis E., Papayannis A., Stringa F., Cole T., Jalil A. Swept-source optical coherence tomography angio (topcon corp, japan): technology review. Dev Ophthalmol. 2016;56:13–17. doi: 10.1159/000442771. [DOI] [PubMed] [Google Scholar]
- 68.Machoy M., Seeliger J., Szyszka-Sommerfeld L., Koprowski R., Gedrange T., Wozniak K. The use of optical coherence tomography in dental diagnostics: a state-of-the-art review. J Health Eng. 2017;2017:7560645. doi: 10.1155/2017/7560645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hoyos AZOB, An efficient estimation algorithm for the calibration of low-cost ss-oct systems, IEEE International Symposium on Biomedical Imaging, IEEE, 2017.
- 70.Qi L., Chen C., Jiang L., Li J., Liang Y. Establishment of swept-frequency optical coherence tomography endoscopic imaging system for root canal and its application in the diagnosis of root fissures. J Peking Univ Health Sci. 2019;51:753–757. doi: 10.19723/j.issn.1671-167X.2019.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lü C.X.C.S. Correlation between clinical diagnosis and magnetic resonance imaging findings of temporomandibular joint disorder. Int J Stomatol. 2016;43:47–51. [Google Scholar]
- 72.Sedlacik J., Kutzner D., Khokale A., Schulze D., Fiehler J., Celik T., et al. Optimized 14 + 1 receive coil array and position system for 3d high-resolution mri of dental and maxillomandibular structures. Dentomaxillofac Radiol. 2016;45 doi: 10.1259/dmfr.20150177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bracher A.K., Hofmann C., Bornstedt A., Hell E., Janke F., Ulrici J., et al. Ultrashort echo time (ute) mri for the assessment of caries lesions. Dentomaxillofac Radiol. 2013;42 doi: 10.1259/dmfr.20120321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fujita M., Matsuzaki H., Yanagi Y., Hara M., Katase N., Hisatomi M., et al. Diagnostic value of mri for odontogenic tumours. Dentomaxillofac Radiol. 2013;42 doi: 10.1259/dmfr.20120265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Liu T., Ke X., Yang J. Magnetic resonance imaging and its application in endodontics. Int J Stomatol. 2019;46:693–698. [Google Scholar]
- 76.Pasteris J.D., Wopenka B., Valsami-Jones E. Bone and tooth mineralization: why apatite. Elements. 2008;4:97–104. [Google Scholar]
- 77.Schreiner L.J., Cameron I.G., Funduk N., Miljkovic L., Pintar M.M., Kydon D.N. Proton nmr spin grouping and exchange in dentin. Biophys J. 1991;59:629–639. doi: 10.1016/S0006-3495(91)82278-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Schuurmans T.J., Nixdorf D.R., Idiyatullin D.S., Law A.S., Barsness B.D., Roach S.H., et al. Accuracy and reliability of root crack and fracture detection in teeth using magnetic resonance imaging. J Endod. 2019;45:750–755. doi: 10.1016/j.joen.2019.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Idiyatullin D., Garwood M., Gaalaas L., Nixdorf D.R. Role of mri for detecting micro cracks in teeth. Dentomaxillofac Radiol. 2016;45 doi: 10.1259/dmfr.20160150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Idiyatullin D., Corum C., Moeller S., Prasad H.S., Garwood M., Nixdorf D.R. Dental magnetic resonance imaging: making the invisible visible. J Endod. 2011;37:745–752. doi: 10.1016/j.joen.2011.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Miao S., Yang H., Huang Y., Gong R., Shao X. RBI progress in photoacoustic imaging research. Chin J Opt. 2015;8:699–713. [Google Scholar]
- 82.Li Z., Hartzler T., Ramos A., Osborn M.L., Li Y., Yao S., et al. Optimal imaging windows of indocyanine green-assisted near-infrared dental imaging with rat model and its comparison to x-ray imaging. J Biophotonics. 2020;13 doi: 10.1002/jbio.201960232. [DOI] [PubMed] [Google Scholar]
- 83.Li Z., Zaid W., Hartzler T., Ramos A., Osborn M.L., Li Y., et al. Indocyanine green-assisted dental imaging in the first and second near-infrared windows as compared with x-ray imaging. Ann N Y Acad Sci. 2019;1448:42–51. doi: 10.1111/nyas.14086. [DOI] [PubMed] [Google Scholar]
- 84.Li Z., Holamoge Y.V., Li Z., Zaid W., Osborn M.L., Ramos A., et al. Detection and analysis of enamel cracks by icg-nir fluorescence dental imaging. Ann N Y Acad Sci. 2020;1475:52–63. doi: 10.1111/nyas.14374. [DOI] [PubMed] [Google Scholar]
- 85.Zhou J., Fu J., Xiao M., Qiao F., Fu T., Lv Y., et al. New technique for detecting cracked teeth and evaluating the crack depth by contrast-enhanced cone beam computed tomography: an in vitro study. BMC Oral Health. 2022;22:48. doi: 10.1186/s12903-022-02085-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yuan M., Gao A.T., Wang T.M., Liang J.H., Aihemati G.B., Cao Y., et al. Using meglumine diatrizoate to improve the accuracy of diagnosis of cracked teeth on cone-beam ct images. Int Endod J. 2020;53:709–714. doi: 10.1111/iej.13270. [DOI] [PubMed] [Google Scholar]
- 87.Hu Z., Wang T., Pan X., Cao D., Liang J., Gao A., et al. Comparison of diagnosis of cracked tooth using contrast-enhanced cbct and micro-ct. Dentomaxillofac Radiol. 2021;50:20210003. doi: 10.1259/dmfr.20210003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Liu L., Qiang C., Ni P., Pan F., Guo M. Status and prospect of laboratory accreditation for new technology capability of nondestructive testing. Nondestruct Test. 2021;43:39–44. [Google Scholar]
- 89.Peck S.D., Rowe J.M., Briggs G.A. Studies on sound and carious enamel with the quantitative acoustic microscope. J Dent Res. 1989;68:107–112. doi: 10.1177/00220345890680020201. [DOI] [PubMed] [Google Scholar]
- 90.Brandt K.R.J., High frequency acoustic dispersion of surface waves using time-resolved broadband microscopy,”inieee symposium onultrasonics, Ultrasonics, 2003 IEEE Symposium on, IEEE, 2003, pp. 799–802.
- 91.Raum K., Kempf K., Hein H., Schubert J., Maurer P. Preservation of microelastic properties of dentin and tooth enamel in vitro—a scanning acoustic microscopy study. Dent Mater. 2007;23:1221–1228. doi: 10.1016/j.dental.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 92.Culjat M.O., Singh R.S., Brown E.R., Neurgaonkar R.R., Yoon D.C., White S.N. Ultrasound crack detection in a simulated human tooth. Dento-maxillo-Facial Radiol. 2005;34:80. doi: 10.1259/dmfr/12901010. [DOI] [PubMed] [Google Scholar]
- 93.Sun K., Yuan L., Shen Z., Xu Z., Zhu Q., Ni X., et al. Scanning laser-line source technique for nondestructive evaluation of cracks in human teeth. Appl Opt. 2014;53:2366–2374. doi: 10.1364/AO.53.002366. [DOI] [PubMed] [Google Scholar]
- 94.Feng G., Huang G.B., Lin Q., Gay R. Error minimized extreme learning machine with growth of hidden nodes and incremental learning. IEEE Trans Neural Netw. 2009;20:1352–1357. doi: 10.1109/TNN.2009.2024147. [DOI] [PubMed] [Google Scholar]
- 95.Hu T., Gao L., Yang H. Application of laser ultrasonic technology in nondestructive testing of aerospace composites. Aeronaut Manuf Technol. 2018;61:50–57. [Google Scholar]
- 96.Zhao Y., Guo R., Song J., Ma J., Liu S., Sun J., et al. Research on non-contact non-destructive detection of metal internal defects by laser-emat method. Laser Technol. 2013;37:277–280. [Google Scholar]
- 97.Sun K.. Diagnosis and evaluation of early caries and cracked teeth by laser surface acoustic wave. [PH.D]:Nanjing University of Science and Technology; 2014.
- 98.Aljdaimi A., Devlin H., Dickinson M., Burnett T., Slater T. Micron-scale crack propagation in laser-irradiated enamel and dentine studied with nano-CT. Clin Oral Investig. 2019;23:2279–2285. doi: 10.1007/s00784-018-2654-0. [DOI] [PubMed] [Google Scholar]
- 99.Staninec M., Meshkin N., Manesh S.K., Ritchie R.O., Fried D. Weakening of dentin from cracks resulting from laser irradiation. Dent Mater. 2009;25:520–525. doi: 10.1016/j.dental.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Carlstrom D., Glas J.E. Studies on the ultrastructure of dental enamel. III. The birefringence of human enamel. J Ultrastruct Res. 1963;8:1–11. doi: 10.1016/s0022-5320(63)80016-7. [DOI] [PubMed] [Google Scholar]
- 101.Hsiao T., Lee S., Sun C. Optical polarimetric detection for dental hard tissue diseases characterization. Sensors. 2019;19:4971. doi: 10.3390/s19224971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tatano R., Berkels B., Ehrlich E.E., Deserno T.M., Fritz U.B. Spatial agreement of demineralized areas in quantitative light-induced fluorescence images and digital photographs. Dentomaxillofac Radiol. 2018;47:20180099. doi: 10.1259/dmfr.20180099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Jun M.K., Ku H.M., Kim E., Kim H.E., Kwon H.K., Kim B.I. Detection and analysis of enamel cracks by quantitative light-induced fluorescence technology. J Endod. 2016;42:500–504. doi: 10.1016/j.joen.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 104.Jun M.K., Park S.W., Lee E.S., Kim B.R., Kim B.I. Diagnosis and management of cracked tooth by quantitative light-induced fluorescence technology. Photodiagn. Photodyn. Ther. 2019;26:324–326. doi: 10.1016/j.pdpdt.2019.04.025. [DOI] [PubMed] [Google Scholar]
- 105.Cheng R., Shao J., Gao X., Tao C., Ge J., Liu X. Noninvasive assess early dent lesion using a dual-contrast photoacoust tomography. Sci Rep. 2016;6:21798. doi: 10.1038/srep21798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Jud C., Sharma Y., Gunther B., Weitz J., Pfeiffer F., Pfeiffer D. X-ray dark-field tomography reveals tooth cracks. Sci Rep. 2021:14017. doi: 10.1038/s41598-021-93393-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zhang C., Mo D., Guo J., Wang W., Long S., Zhu H., et al. A method of crack detection based on digital image correlation for simulated cracked tooth. BMC Oral Health. 2021;21:539. doi: 10.1186/s12903-021-01897-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Matsushita-Tokugawa M., Miura J., Iwami Y., Sakagami T., Izumi Y., Mori N., et al. Detection of dentinal microcracks using infrared thermography. J Endod. 2013;39:88–91. doi: 10.1016/j.joen.2012.06.033. [DOI] [PubMed] [Google Scholar]