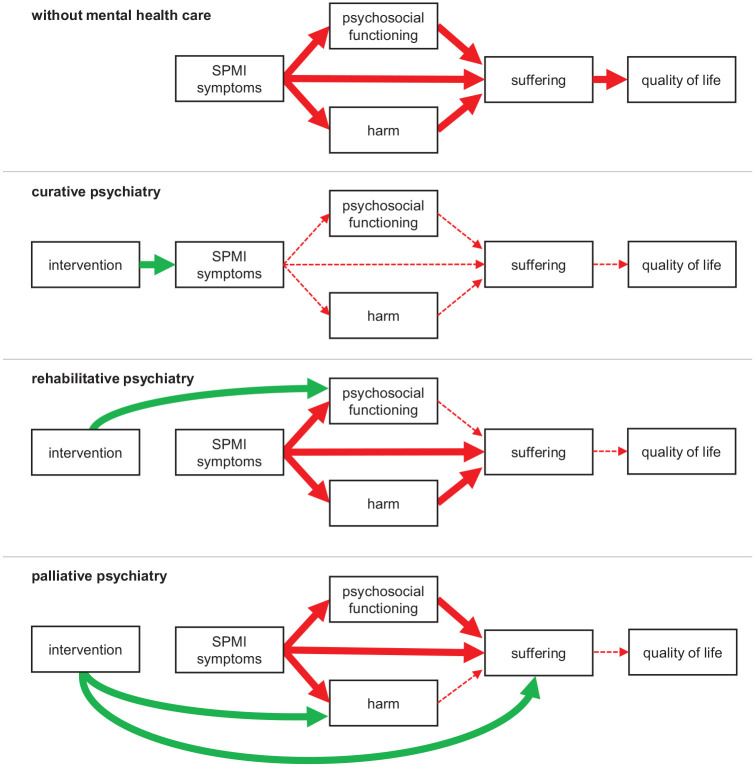
Figure 1.
Conceptual overview of different approaches to mental health care.
Harmful effects in red and beneficial effects in green. While many more associations between the depicted constructs are conceivable, for reasons of clarity, we only show the associations most important for clarifying the conceptual differences between subdisciplines of psychiatry. ‘SPMI symptoms’ refer to the core symptoms of the respective SPMI, such as fear of gaining weight in anorexia nervosa. ‘Harm’ refers to negative consequences of the SPMI and can be biological, psychological, social or economic. ‘Suffering’ is the felt quality of unfulfilled basic needs threatening the existence or integrity of the person. All subdisciplines of psychiatry ultimately aim at improving patients’ quality of life, but differ in the strategies they employ in this pursuit. Traditional curative psychiatry uses interventions aiming at symptom remission (or at least reduction), which – if successful – indirectly reduces harm and suffering associated with the SPMI, improves psychosocial functioning and ultimately quality of life. When SPMI symptoms are most likely irremediable, rehabilitative and palliative psychiatry offer alternative care approaches. Rather than at symptom reduction, rehabilitative psychiatry aims directly at improved psychosocial functioning, and palliative psychiatry aims directly at harm reduction (e.g. supplying patients with sterile injection equipment to prevent infections; prescribing calcium and vitamin D for osteopenia in anorexia nervosa to prevent fractures) and/or relief of suffering (e.g. prescribing diazepam to relieve anxiety induced by therapy-refractory persecutory delusions). Often, palliative psychiatry interventions will aim at both harm reduction and relief of suffering (e.g. supervised injectable heroin treatment to reduce the risk of overdoses and alleviate craving). While palliative psychiatry in a broad sense refers to any approaches aiming at reducing harm and relieving suffering by means other than reduction of SPMI symptoms or improvement of psychosocial functioning, palliative psychiatry in a narrow sense refers to such approaches in patients likely to die of their SPMI in the near future.