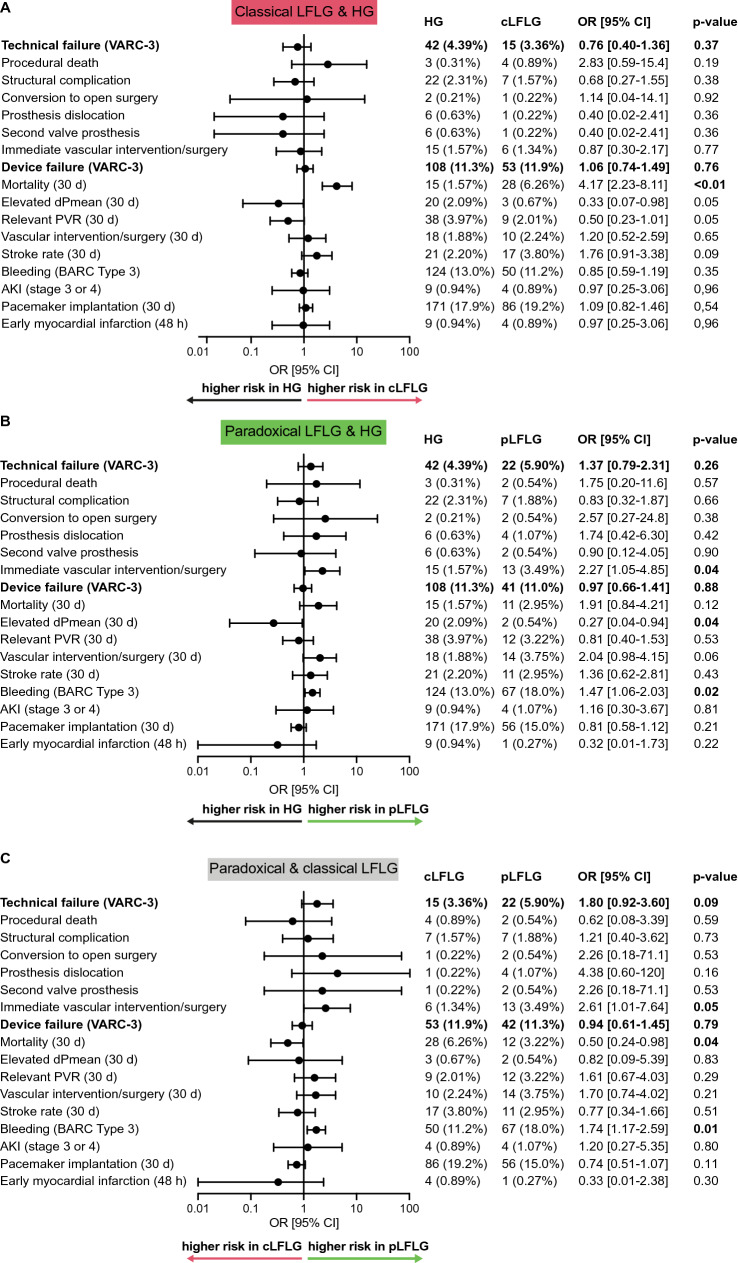
Fig. 2.
Technical and clinical outcomes Short-term outcomes (up to 30 days) for the two LFLG groups were compared to HG and compared to each other according to Valve Academic Research Consortium-3 (VARC-3) endpoints. The composite endpoints of a technical failure (consisting of procedural death, structural cardiac complications, conversion to open surgery, prosthesis dislocation, the use of a second valve prosthesis, or immediate vascular intervention or surgery) or device failure at 30 days (consisting of the composite endpoint technical failure, 30-day mortality, elevated pressure gradients or relevant paravalvular regurgitation on echocardiography, or vascular surgery/intervention at 30 days, stroke, relevant bleeding, acute kidney injury (AKI) and permanent pacemaker implantation) occurred at similar frequencies. However, there were differences in single components. a The 30-day mortality was significantly higher in cLFLG compared to HG. b For pLFLG patients, the risk of relevant bleeding or the necessity for vascular interventions were significantly increased in comparison to HG patients. c While pLFLG patients had a higher risk for bleeding and vascular intervention/surgery, cLFLG patients had a higher 30-day mortality. OR denotes odds ratio. AKI acute kidney injury, cLFLG classical low-flow low-gradient, dPmean, mean transvalvular pressure gradients, HG high gradient, pLFLG paradoxical low-flow low-gradient, VARC-3 valve academic research consortium-3