Abstract
Simple Summary
The reported incidence of thrombotic events (TE) in non-promyelocytic acute myeloid leukemia (AML) patients varies in the literature from 2% to 13%. The aim of our retrospective study was to assess the incidence of TE in a real-word population of AML patients to determine the impact of TE on survival and to recognize risk factors for early venous thromboembolism (VTE). We observed a TE incidence of 14.6% among 300 patients with newly diagnosed AML. Arterial TE but not VTE was associated with a poorer OS. Furthermore, we observed a higher relapse rate among patients experiencing a VTE. We recognized platelets count >50 × 109/L, presence of comorbidities and a previous history of TE as risk factors for early VTE development. Accordingly, we proposed a score combining these factors that may help in implementing strategies to manage patients at higher risk of early thrombotic complications.
Abstract
Information regarding the incidence and the prognostic impact of thrombotic events (TE) in non-promyelocytic acute myeloid leukemia (AML) is sparse. Although several risk factors associated with an increased risk of TE development have been recognized, we still lack universally approved guidelines for identification and management of these complications. We retrospectively analyzed 300 consecutive patients with newly diagnosed AML. Reporting the incidence of venous TE (VTE) and arterial TE (ATE) was the primary endpoint. Secondarily, we evaluated baseline patient- and disease-related characteristics with a possible influence of VTE-occurrence probability. Finally, we evaluated the impact of TE on survival. Overall, the VTE incidence was 12.3% and ATE incidence was 2.3%. We identified three independent predictors associated with early-VTE: comorbidities (p = 0.006), platelets count >50 × 109/L (p = 0.006), and a previous history of VTE (p = 0.003). Assigning 1 point to each variable, we observed an overall cumulative incidence of VTE of 18.4% in the high-risk group (≥2 points) versus 6.4% in the low-risk group (0–1 point), log-rank = 0.002. Overall, ATE, but not VTE, was associated with poor prognosis (p < 0.001). In conclusion, TE incidence in AML patients is not negligible. We proposed an early-VTE risk score that could be useful for a proper management of VTE prophylaxis.
Keywords: acute myeloid leukemia, thrombosis, venous thromboembolism, thrombosis risk score, survival
1. Introduction
The association between cancer and thrombotic events (TE) has been well-known for more than a century, as it was firstly reported by Jean Baptiste Bouillaud in 1823 [1]. Since then, several studies have described this complication of patients with solid tumors, who are estimated to have a seven-fold increased risk of developing TE as compared to the general population [2,3]. In these patients, TE correlate with a worse prognosis in terms of both overall (OS) and relapse-free survival (RFS) [4,5], representing the second leading cause of death [6].
In patients with hematological malignancies (HM), treatment-related morbidity and mortality are presumed to be almost exclusively related to infection and bleeding, given the common condition of thrombocytopenia and neutropenia at diagnosis and during the course of the disease. Conversely, in such a setting TE has been considered rare and has not received a great deal of attention. However, recent studies indicate a non-negligible risk of thrombosis in HM patients, similar or even higher than in subjects with solid cancers [7,8]. The incidence of TE is well known in some HM such as myeloma (up to 25% without thromboprophylaxis and during therapy with thalidomide) [9], non-Hodgkin lymphoma (6.5%), and Hodgkin disease (4.7%) [10]. Furthermore, the frequency of arterial thrombotic events (ATE) and venous thromboses (VTE) is approximately 11–25% in essential thrombocythemia, 12–39% in polycythemia vera and 10% in acute promyelocytic leukemia (APL) [11,12,13].
Available information about thrombosis in non-promyelocytic acute myeloid leukemia (AML) is scarce, with a reported incidence of TE ranging from 2% to 13% [14,15,16,17]. In such a scenario, the pathogenesis of TE is multifactorial with leukemia cells exerting a prothrombotic effect through the release of fibrinolytic and proteolytic factors, inflammatory cytokines and over-expression of tissue factor on the cell surface of leukemic cells [18,19,20]. Active therapy represents a further predisposing element. Indeed, chemotherapy-induced cell lysis results in a massive release of these procoagulants which, together with the hemodynamic changes and CVC-related vessel injuries, may explain the reported increased rate of TE also in AML patients, in whom the common occurrence of thrombocytopenia may lead to underestimation of this complication [21]. Moreover, patients with AML often present with a hypercoagulable state or chronic disseminated intravascular coagulation (DIC), even in the absence of active thrombosis [22,23]. Therefore, an accurate estimate of an individual patient’s TE risk is essential to decide whether anticoagulation is needed, and to balance the benefit of thromboprophylaxis against the hemorrhagic risk due to the underlying disease- and chemotherapy-induced thrombocytopenia.
The primary aim of our study is: (1) to assess the incidence of TE in a real-word population of non-promyelocytic AML patients; (2) to assess the association between baseline disease and patients’ characteristics and TE; (3) to generate a clinical score predicting the risk of VTE; (4) to determine the impact of TE on survival.
2. Materials and Methods
2.1. Patients’ Characteristics
We reviewed the records of 300 consecutive newly diagnosed adult patients (≥18 years of age) with non-promyelocytic AML, admitted between January 2010 and December 2020 to the Hematology Department of our institution. Baseline characteristics included in the analysis were date of AML diagnosis, age, gender, body mass-index (BMI), genetics/cytogenetics, blood count and serum chemistry. Information about chemo-therapeutic regimens, date of complete remission (CR)/resistance, date of relapse, date of death or last follow-up, comorbidities, date of TE diagnosis and treatment and TE characteristics were also collected. Comorbidities were defined as the simultaneous presence of one or more diseases or medical conditions, not related to the underlying AML. Routine blood tests, including hemoglobin, white blood cell (WBC) and platelet count (PLTc), were carried out on ethylenediaminetetra-acetic acid (EDTA)-anticoagulated blood samples. Assessment of the coagulation parameters, such as prothrombin time (PT), activated partial thromboplastin time (APTT), fibrinogen (Clauss method) and D-dimer (immuno-turbidimetric method) coagulation tests were performed on citrated plasma tubes. The presence of DIC was assessed according to the 2018 revision of the International Society of Thrombosis and Haemostasis (ISTH) scoring system for DIC [24] as follows: platelet count (≥100 × 109/L = 0; 50–99.999 × 109/L = 1; <50 × 109/L = 2), fibrinogen level (≥100 mg/dL = 0; <100 mg/dL = 1), PT prolongation above upper limit of normal (ULN) (<3 s = 0, 3–6 s = 1, >6 s = 2), and D-dimer (<3000 ng/mL = 0, 3000–7000 ng/mL = 2, >7000 ng/mL = 3). A score sum ≥4 denotes the presence of an overt DIC. Patients were stratified according to the ELN 2017 genetic/cytogenetic risk assessment [25]. Depending on age, performance status or availability of clinical trials for the treatment of AML, patients received intensive chemotherapy (mostly “7 + 3”-like schedule or fludarabine based regimens), non-intensive chemotherapy (such as low dose of cytarabine or hypomethylating agents) or supportive therapy [26]. The study was approved by the Internal Review Board of our Institution and conducted in accordance with the regulations set forth by the Declaration of Helsinki.
2.2. Thrombotic Events Diagnosis and Management
TE were defined as a composite of first VTE (not including superficial vein thrombosis) or ATE at any site. VTE were diagnosed by Doppler ultrasonography, computed tomography, or magnetic resonance imaging. Myocardial infarction (MI) was diagnosed according to clinical, enzymatic and electrocardiographic criteria as per well established guidelines [27]. The diagnosis of ATE other than MI was made by computed tomography. Patients with VTE and PLTc ≥30 × 109/L were treated with low-molecular-weight heparin (LMWH) for 3 to 6 months [28,29]. The dose of LMWH was reduced by 50% if PLTc was between 30 and 50 × 109/L and discontinued or not initiated when PLTc was <30 × 109/L. Patients with a previous history of MI were prophylactically treated with antiplatelet drugs if PLTc >50 × 109/L [30].
2.3. Statistical Analyses
Comparisons between groups were performed to assess differences in biological and clinical data using the Chi-squared test or Fisher’s exact test for categorical data and Mann-Whitney and Kruskal-Wallis test in case of continuous variables. Risk factors associated with the development of VTE or ATE were analyzed by logistic regression models. Patients who presented with a TE before chemotherapy initiation were considered to belong to the group receiving supportive therapy. We dichotomized potentially significant continuous variables at an optimal cut-off point identified with ROC analysis and the Youden index. Hosmer and Lemeshow’s stepwise strategies were applied for model building: potential independent variables with p-value < 0.25 were included in the initial full model. All tests were 2-sided, accepting p < 0.05 as a statistically significant value. Statistically significant variables (p < 0.05) were included in the final model. The model was evaluated using Hosmer–Lemeshow tests and pseudo-R2 measures. The final prediction score was derived based on weighed variables in the final model and compared using Kaplan–Meier survival analysis with log- rank tests to assess differences in identified categories. Internal validation was conducted using nonparametric bootstrapping methods, obtaining estimates of the variability of the β-coefficients for the parameters in the regression equations. To evaluate the predictive accuracy of the model, a Harrell’s statistics was performed and a C-index was calculated. OS was defined as the time from the diagnosis to death from any cause, and in patients with TE as the time from TE diagnosis to death from any cause. RFS was defined as the time from the achievement of CR after induction therapy to disease-relapse or death from any cause, whichever came first. Probabilities of OS and RFS were calculated using the Kaplan-Meier method. All statistical analyses were performed using SPSS v28.
3. Results
Overall, the median age at AML diagnosis was 64 years (range 21–90), with a slight male predominance (61%, n = 178). Among the 300 patients, 69% had de novo AML, 19% had secondary AML, and 12% had therapy-related AML. According to the ELN 2017 risk stratification, 17.3% of the cases were classified as favorable, 41.4% intermediate and 28.3% adverse risk, whereas 13% were not classifiable. At least one comorbidity was present in 67.7% of the patients, including hypertension (41%), autoimmune disorders (15%) and diabetes (10.7%). Two or more cardiovascular comorbidities were observed in 24.7% of the patients with 6.7% reporting previous coronary diseases or myocardial infarction and, therefore, receiving antiplatelets medication. An additional 4.3% of patients were receiving anticoagulation for other indications (atrial fibrillation, chronic VTE, cerebrovascular ischemia, or heart failure). At baseline, 20% of cases showed an ISTH-DIC score ≥4. As to treatments, 58.3% received intensive chemotherapy, 19.7% non-intensive strategies and 22% only supportive care. The demographic and disease characteristics of the study cohort are summarized in Table 1.
Table 1.
Baseline patient’s characteristics.
| No TE n = 264 | TE n = 36 | p | VTE, n = 30 | p | ATE, n = 6 | p | |
|---|---|---|---|---|---|---|---|
| Sex M/F | 159/105 | 24/12 | 0.585 | 18/12 | 1 | 6/0 | 0.085 |
| Median Age (interval) | 64 (21–90) | 64 (30–82) | 0.998 | 64 (30–82) | 0.708 | 66 (53–77) | 0.584 |
| AML Classification | |||||||
| de Novo AML | 183 | 24 | 0.203 | 20 | 0.137 | 4 | 0.59 |
| Treatment-related AML | 35 | 2 | 0.219 | 1 | 0.195 | 1 | 0.318 |
| Secondary-AML | 46 | 10 | 0.152 | 9 | 0.179 | 1 | 0.876 |
| ELN 2017-risk stratification | |||||||
| Favorable | 46 | 6 | 0.908 | 5 | 0.919 | 1 | 0.93 |
| Intermediate | 108 | 16 | 0.803 | 13 | 0.862 | 2 | 0.885 |
| Adverse | 73 | 12 | 0.665 | 10 | 0.696 | 2 | 0.868 |
| Non-Classifiable | 37 | 2 | 2 | 1 | |||
| FLT3 | 49 | 8 | 0.652 | 7 | 0.621 | 1 | 1 |
| NPM1 | 54 | 5 | 0.379 | 4 | 0.467 | 1 | 1 |
| Comorbidities ≥ 1 | 171 | 32 | 0.004 | 27 | 0.006 | 6 | 0.182 |
| Cardiovascular comorbidities ≥ 2 | 58 | 16 | 0.006 | 10 | 0.266 | 6 | <0.001 |
| BMI ≥ 1 | 24 | 5 | 0.367 | 4 | 0.511 | 1 | 0.46 |
| ISTH-DIC score ≥ 4 | 56 | 5 | 0.382 | 5 | 0.811 | 0 | 0.605 |
| Smokers | 107 | 18 | 0.286 | 15 | 0.337 | 3 | 0.696 |
| History of VTE | 7 | 5 | 0.008 | 5 | 0.003 | 0 | |
| Central Venous Catheter | 221 | 31 | 0.813 | 25 | 1 | 6 | |
| Hemoglobin Count g/dL | 8.55 (3.5–13.8) | 8.95 (5.2–13.9) | 0.371 | 8.7 (5.2–11.7) | 0.939 | 9.7 (8.4–13.9) | 0.059 |
| Leukocyte Count × 109/L | 9.11 (10–472.3) | 8.77 (0.47–200) | 0.614 | 7.83 (0.47–200) | 0.708 | 6.93 (0.82–26) | 0.286 |
| Platelet Count × 109/L | 44.5 (3–1130) | 71 (5–597) | 0.032 | 76 (5–597) | 0.05 | 44.5 (29–95) | 0.998 |
| Serum LDH level, U/L | 350 (70–4000) | 300 (120–1687) | 0.425 | 292 (120–1687) | 0.262 | 364 (234–811) | 0.707 |
| Serum Fibrinogen level mg/dL | 364 (63–2878) | 373 (82–1025) | 0.842 | 364 (82–1025) | 0.677 | 506 (332–872) | 0.027 |
| ATIII, % | 92 (25–142) | 97.3 (70–125) | 0.147 | 97.3 (71–125) | 0.2 | 88.3 (70–115) | 0.727 |
| PT, seconds | 14.6 (11.1–29.6) | 14.5 (11.4–20.4) | 0.439 | 14.85 (11.4–20.4) | 0.66 | 14.7 (12.4–16.5) | 0.981 |
| aPTT, ratio | 0.980 (0.59–1.86) | 0.925 (0.68–2.01) | 0.136 | 0.935 (0.68–2.01) | 0.379 | 0.950 (0.8–0.94) | 0.076 |
| Serum D-Dimer level ng/mL | 834 (52–121,450) | 886 (77–48,065) | 0.936 | 999 (77–48,065) | 0.948 | 1279 (532–20,650) | 0.324 |
All data are the median value (range) unless otherwise indicated. AML, acute myeloid leukemia; ELN. European Leukemia Net; BMI, body mass index; ISTH-DIC score, International Society of Thrombosis and Haemostasis- disseminated intravascular coagulation score; VTE, venous thromboembolism; ATE, arterial thrombosis; LDH, Lactate Dehydrogenase; ATIII, Antithrombin; PT, Prothrombin Time; aPTT, activated Partial Thromboplastin Time. Statistically.
During the overall study period (median follow-up 30 months, range 2–126 months), a total of 44/300 patients (14.6%) experienced a TE, the majority of which (12.3%) were VTE, with 2.3% being ATE. We observed 28 CVC-related thromboses (CRT), 5 PE (2 occurring in the context of deep vein thrombosis of the lower extremities and 1 of the arm), 2 deep vein thromboses of the lower extremities without pulmonary embolism, 2 hepatic veins thrombosis, 6 MI, and 1 peripheral arterial thrombosis. Patients suffering from TE had a median age at AML diagnosis of 71.5 years (range 30–82). None of the 44 patients had received anticoagulant prophylaxis in the two weeks preceding TE occurrence. Overall, the cumulative incidence of VTE at 45 days, 3 months, 6 months, and 2 years from AML presentation was 9.2%, 11.1%, 13.8% and 15%, respectively, while the cumulative incidence of ATE was 2.8%, 3.3%, and 4.8%. The majority of TE (82%, 30 VTE and 6 ATE) occurred within 45 days from AML presentation (median 25 days, range 1–40 days), 58% of which (19 VTE and 2 ATE) before starting AML-therapy. The characteristics of TE are detailed in Table 2. Eight patients developed TE after 45 days from AML presentation: 3 VTE and 1 ATE at AML relapse, 2 VTE after of HSCT and 2 VTE under hypomethylating agents. These patients were excluded from the analysis because of potential bias, related to a myriad of factors treatment- and not-treatment related.
Table 2.
Characteristics of thrombotic events occurred within 45 days from acute myeloid leukemia diagnosis.
| Age | Sex | Type of TE | Onset from AML Diagnosis (Days) | History of VTE | n° of Comorbidities | TE Pre/Post AML-Therapy | |
|---|---|---|---|---|---|---|---|
| 1 | 66 | M | hepatic veins thrombosis | 1 | no | 2 | pre |
| 2 | 47 | F | CRT | 8 | no | 2 | pre |
| 3 | 63 | M | CRT | 10 | no | 1 | post |
| 4 | 68 | M | DVT+PE | 1 | no | 3 | pre |
| 5 | 53 | M | MI | 1 | no | 2 | pre |
| 6 | 44 | F | CRT | 11 | no | 1 | post |
| 7 | 71 | F | PE | 12 | no | 2 | post |
| 8 | 63 | M | MI | 35 | no | 2 | post |
| 9 | 81 | M | CRT | 18 | no | 2 | pre |
| 10 | 70 | M | DVT | 1 | no | 2 | pre |
| 11 | 68 | M | CRT | 4 | no | 2 | pre |
| 12 | 49 | F | CRT | 11 | no | 2 | post |
| 13 | 64 | F | CRT | 10 | no | 1 | pre |
| 14 | 30 | M | CRT | 8 | no | 0 | pre |
| 15 | 58 | M | CRT | 5 | no | 2 | pre |
| 16 | 63 | F | DVT | 1 | yes | 1 | pre |
| 17 | 64 | M | DVT | 3 | no | 3 | pre |
| 18 | 76 | M | CRT | 8 | no | 3 | post |
| 19 | 61 | M | CRT | 6 | no | 1 | post |
| 20 | 73 | F | PE | 40 | no | 1 | post |
| 21 | 59 | M | CRT | 36 | yes | 1 | post |
| 22 | 40 | F | DVT+PE | 10 | no | 0 | post |
| 23 | 82 | F | CRT | 28 | no | 2 | pre |
| 24 | 41 | M | CRT | 34 | no | 0 | post |
| 25 | 55 | M | CRT | 12 | no | 1 | pre |
| 26 | 64 | M | MI | 24 | no | 2 | post |
| 27 | 75 | M | CRT | 31 | yes | 1 | post |
| 28 | 72 | M | MI | 13 | no | 1 | post |
| 29 | 69 | F | CRT | 2 | no | 1 | pre |
| 30 | 73 | M | CRT | 6 | yes | 1 | pre |
| 31 | 48 | F | hepatic veins thrombosis | 1 | no | 0 | pre |
| 32 | 72 | M | CRT | 3 | no | 1 | pre |
| 33 | 55 | M | CRT | 10 | no | 3 | pre |
| 34 | 68 | M | MI | 24 | no | 2 | pre |
| 35 | 67 | F | CRT | 10 | yes | 3 | pre |
| 36 | 77 | M | MI | 25 | no | 4 | post |
TE, thrombotic event; AML, acute myeloid leukemia; VTE, venous thrombotic event; M, male; F, female; CRT, catheter-related thrombosis; MI, myocardial infarction; DVT deep-venous thrombosis; PE, pulmonary embolism.
The presence of one or more comorbidities (OR: 4.729; 95% CI 1.398–16.000; p = 0.006), a previous history of VTE (OR: 7.514; 95% CI 2.221–25.420; p = 0.003) and a PLTc at diagnosis higher than 50 × 109/L (OR: 3.287; 95% CI 1.413–7.643; p = 0.006) were associated with an increased risk of VTE, within 45 days from AML diagnosis. Age, sex, BMI, leucocyte count, hemoglobin level, an ISTH-DIC score ≥4, ELN risk stratification and cytogenetic and genetic abnormalities were not associated with an increased risk of VTE development. No difference in VTE rate was observed in patients with or without CVC (n = 25/252, 10% vs. 5/48, 10% respectively, p = 1). Once resolved, no recurrence of VTE was recorded in any of the patients. With the limitation of the small sample size, ATE were associated with the presence of two or more cardiovascular comorbidities (i.e., hypertension, previous IM or ischemic stroke, peripheral arterial disease, atrial fibrillation etc.), (p < 0.001). Despite the cardiovascular comorbidities, it must be noted that 3 patients had normal cardiac function (of which, 2 were given intensive chemotherapy, 1 non-intensive), 1 died soon thereafter AML diagnosis (thereby cardiac function was not evaluated), 2 had existing cardiac impairment. Excluding patients developing TE prior to AML therapy initiation, no difference in TE rates was seen in patients receiving intensive chemotherapy (12/161, 7.5%) vs. non-intensive therapy (3/54, 5.6%; OR 0.730, 95% CI 0.198–2.69; p = 0.869).
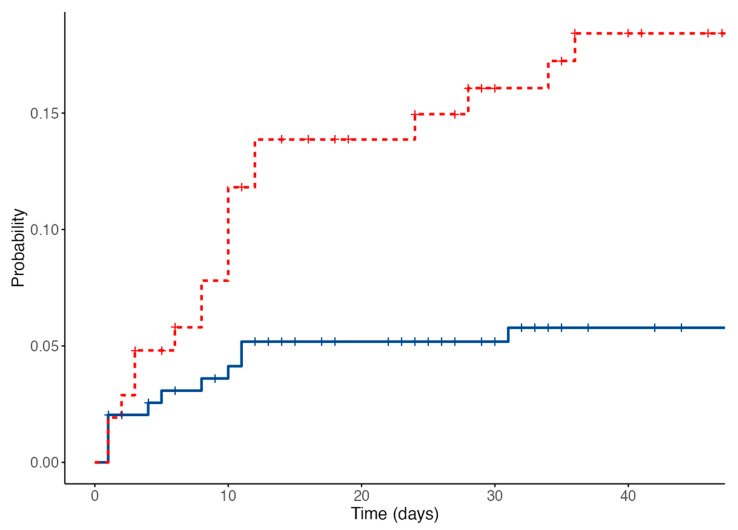
3.1. Development of Venous Thromboembolism Prediction Score
In the attempt to identify patients at higher risk of TE, amenable to early interventions, we built a practice prediction model using 22 potential baseline predictors. Among the risk factors considered, only 3 were included in the final model. These were a previous VTE history, presence of comorbidities, and PLTc > 50 × 109/L at the time of AML diagnosis. Non- parametric bootstrapping confirmed the significance of the selected variables (Table 3). A final prediction score was based on weighed variables assigning 1 point for each of the aforementioned variables. A score summing 2 or more defined patient at high-risk of VTE. When applying this score to our cohort, 34.7% were at high-risk for VTE. This resulted in an overall cumulative incidence of VTE within 45 days from AML presentation of 18.4% in the high-risk and 6.41% in the low-risk group (Figure 1). The Kaplan-Meier survival analysis (log-rank p = 0.002) and the C-index for the model (0.641; 95% CI: 0.534–0.747) demonstrated a significant discrimination between the two categories and an efficient predictive accuracy.
Table 3.
Logistic regression model for occurrence of venous thromboembolism within 45 days from acute myeloid leukemia diagnosis.
| Risk Factor | β-Coefficient | 95% Coefficient Interval for β-Coefficient | p-Value | p-Value (Bootstrapped) |
|---|---|---|---|---|
| Platelet count > 50 × 109/L at baseline | 3.238 | 1.361–7.704 | 0.008 | 0.004 |
| History of venous thromboembolism | 5.447 | 1.521–19.514 | 0.009 | 0.004 |
| Presence of one or more comorbidities | 3.974 | 1.150–13.734 | 0.029 | 0.021 |
Figure 1.
Overall cumulative incidence of venous thromboembolic events, low risk patients in blue, high risk patients in red.
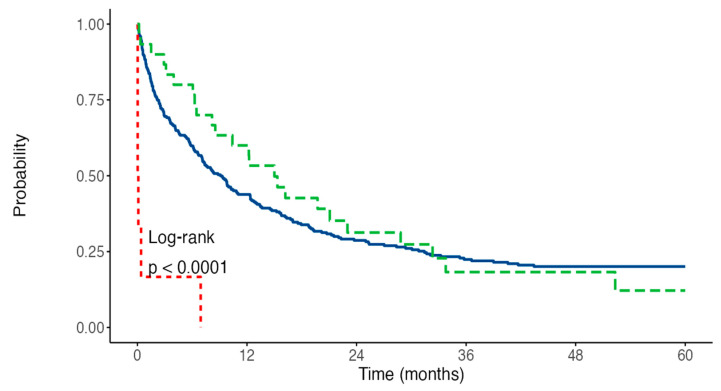
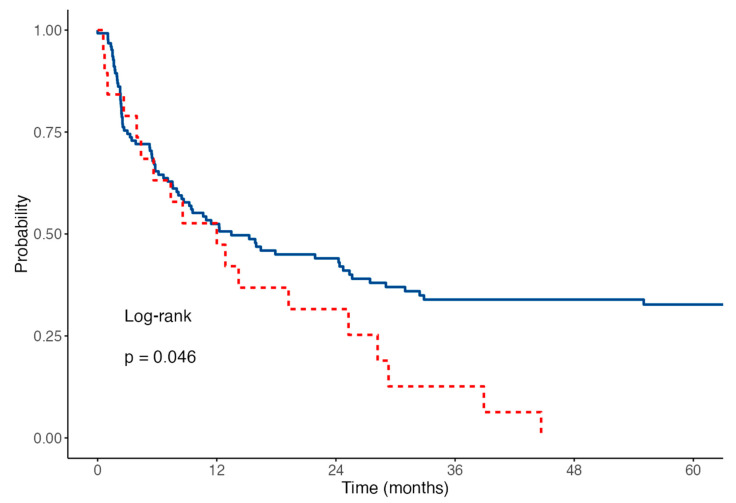
3.2. Impact of Thrombosis on Survival
We finally explored whether the occurrence of early TE would affect survival outcomes in patients with AML. With a median follow-up of 30 months, the overall OS rate was 28.4% at 2 years. No differences were observed in terms of 2-year OS (28.7% vs. 31.3%, HR 0.88 p = 0.552) rates between patients experiencing or not VTE. We did not record any VTE-related death in our series of patients. In contrast, five of six patients experiencing ATE died within 12 days from the event (HR 9.23, p < 0.001). The OS curves are shown in Figure 2. Finally, while no differences in terms of CR rates were observed between patients developing VTE or not (63% vs. 48% p = ns), we noticed that patients developing VTE had a shorter RFS (Figure 3) when compared to the non-VTE counterpart (2-years RFS 31% vs. 44%, p = 0.046). Timing of TE (prior to vs. during treatment) did not affect patients’ outcome (HR 1.26 p = 0.539).
Figure 2.
Overall Survival, patients with no TE in blue, VTE in green, ATE in red.
Figure 3.
Relapse-free survival, patients with VTE in red, no VTE in blue.
4. Discussion
The pathogenesis of thrombosis in patients with cancer is complex and involves both patient and disease-related factors. Parameters known to be associated with an increased risk of TE among AML patients include comorbidities, age, sex, use of hematopoietic growth-factors, presence of CVC, PLTc and prior history of venous thromboembolism [31]. To date, literature evidence concerning the incidence of TE in AML is limited, mostly based on small series of patients, non-homogeneously evaluated from a diagnostic point of view for TE, such as the inclusion of only symptomatic VTE, exclusion of CRT, or heterogeneity of studies population [14,15,16,32,33]. Furthermore, the frequent condition of thrombocytopenia contraindicates an adequate delivery of anticoagulant therapy and further contributes to lack of clarity when precisely assessing the thrombotic risk in such patients.
We evaluated the rate and characteristics of TE in a large cohort of patients with AML. Moreover, we included patients undergoing either intensive or less intensive treatments in order to offer a comprehensive overview of TE incidence in a real-world scenario. In line with data reported on patients with other cancer types, we observed a global rate of TE incidence of 15%, and a risk of VTE development during the early phase of the disease of 10% [7,14,15]. Having one or more comorbidities, a prior history of VTE and a PLTc higher than 50 × 109/L at AML presentation were associated with a greater risk of early VTE. Following the evidence suggested by Al-Ani et al. [34], we built a simple tool to assess the VTE risk in AML patients that categorizes patients into two discrete categories. Based on this model, we established that the overall cumulative incidence of VTE was 18.4% in the high-risk group (≥2 points) and 6.4% in the low-risk group (0–1 points).
Indeed, prior history of VTE is a well-known major risk factor for developing VTE in cancer patients [5,35]. As reported by Vu et al. [32], 7% of AML patients who developed VTE had a prior history of VTE, vs. only 2.1% in cases without previous VTE. Several studies have also identified an association between burden of comorbidities and increased risk of cancer-associated thromboses [36,37], even in AML patients [14].
PLTc has been shown to have significant association with cancer and thrombosis. The Khorana score [38], commonly used to stratify the risk of VTE in patients with cancer undergoing chemotherapy, indicates that a PLTc of 350 × 109/L is a risk factor for VTE [33]. Such a cut-off is not optimal to quantify the risk of thrombosis in AML patients since the very frequent baseline condition of thrombocytopenia precludes its applicability. Studies specifically focused on patients with acute leukemias [17,34] found that a baseline PLTc > 50 × 109/L was an independent risk factor for VTE development. Given the propensity of AML to trigger coagulopathy, Libourel et al. [16] evaluated the role of the ISTH-DIC score [39] to predict the risk of thrombosis in AML patients. The ISTH-DIC score was developed as a diagnostic algorithm for DIC for patients with a clinical suspicion of coagulative disorders (e.g., excessive bleeding in the setting of malignancy, severe infection or sepsis, obstetric complications, trauma). However, this score takes into account PLTc, fibrinogen levels, prothrombin time, and D-Dimer. Therefore, its translation into the AML scenario is someway troublesome as low PLTc (<50 × 109/L) is a very common finding and typically related to AML itself [40]. Moreover, delivery of chemotherapy contributes to alter the evaluation of the severity of DIC due to leukemic cells lysis and tissue cellular damage. For these reasons, inherently linked to the nature of the disease and to its treatment, the ISTH-DIC score fails to reliably predict risk of VTE development in AML. While Libourel showed that the occurrence of TE was significantly higher in patients with laboratory evidence of DIC (DIC score ≥ 5) prior to the initiation of treatment, other studies confirmed the limitation of ISTH-DIC score in VTE-prediction in AML patients [17]. Our study did not show a significant association between VTE and ISTH DIC score. Finally, we confirmed the absence of correlation between the presence of cytogenetic and genetic abnormalities and the development of VTE.
Despite the high number of CRT, we did not observe a statistically significant cor-relation between the presence of CVC and the incidence of VTE. The incidence of CRT observed in our cohort is comparable to that observed in the literature [41]. CRT occurring during the first few days after device insertion are to be related to the local venous injury, reduction of blood flow and deposition of fibrin on the catheter surface. On the other hand, late onset CRT may be related to blood stream infections or to disease-related coagulopathy [42].
In patients with solid tumors, TE are associated with adverse short-term and long-term prognosis [4,43]. In patients with acute leukemia, only a retrospective, registry-based study by Poh et al. [44] evaluated the effect of upper-extremity TE on survival. Analyzing 5072 patients (3252 AML and 1820 ALL) treated with intensive chemotherapy and registered in the California Cancer Registry, the authors found that upper-extremity TE was an independent predictor for increased leukemia-associated and overall mortality in both AML and ALL. The authors speculated that the higher mortality of patients with TE was a surrogate of disease severity and not only the ultimate cause of death. In our study, we did not observe VTE-related death, there was no difference in CR rate between patients with or without VTE, and VTE was not associated with a poorer OS. At the same time, we observed a higher relapse rate among patients experiencing a VTE. In agreement with Poh et al., we could speculate that ill-defined biologic factors may still contribute to thrombogenesis and that VTE could reflect a more aggressive, relapse-prone disease and serve as an additional relapse risk factor. This is different for patients suffering from ATE: 6 patients experienced a MI in the first 45 days after the diagnosis of AML, 5 of whom died within 12 days from the event. These data are consistent with the current literature [45], and could be explained by the different pathogenesis underlying ATE compared to VTE.
We acknowledge the limitations of our study such as its retrospective nature and the absence of an external validation of the proposed scoring system, potentially limiting the broad applicability of the score prior to independent validation studies. However, we believe that the homogeneity of our series, its consecutive recruitment, the management based on standardized diagnostic and therapeutic procedures and the long-term follow up, reflecting 10 years of clinical practice, constitute a valuable strength of our work.
5. Conclusions
Our study highlights that a non-negligible proportion of patients with AML can develop TE, especially of venous origin. Early identification of patients at higher risk of such a complication is challenging and represents an unmet need with potentially relevant clinical consequences. In fact, a possible great risk of TE is made ever more complicated by the AML intrinsic proclivity to bleeding, which precludes unconditionally the use of primary thromboprophylaxis. Therefore, identification of predictors of TE are mandatory for adequate clinical management. As the thrombotic risk-scoring systems used for non-HM does not apply to AML patients, we identified three independent predictors to quantify patients’ VTE risk. This score may help in implementing strategies to manage patients at higher risk of early thrombotic complications. Once could speculate as a potential approach to use higher platelet transfusion thresholds (to maintain a PLTc > 30 × 109/L) along with prophylactic doses of LMWH and/or nonpharmacologic prophylaxis in selected cases.
Further investigation and an external validation of our prediction score on larger cohorts of patients are warranted. Finally, prospective studies investigating the pathogenesis underpinning the occurrence of VTE in AML, its correlations with prognosis, and the proper management of prophylaxis and therapeutic anticoagulation in this setting of patients may shed light onto such oftentimes-neglected AML complication.
Author Contributions
G.P. and M.I.D.P. designed the study; R.P., A.S., L.G., E.B., F.M., M.R.P., V.M. and I.C., collected the data, G.P. and V.D.P. performed the statistical analyses and generated the tables; G.P., R.P. and M.I.D.P. drafted the manuscript; V.F., C.G., F.B., L.M. and A.V. corrected the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was approved by local institutional review board (Pro RS 186.19). With respect to privacy, all personal information was treated in a confidential manner, and all clinical data were anonymized.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bouillaud J., Bouillaud S. De l’obliteration des veines et de son influence sur la formation des hydropisies partielles: Consideration sur la hydropisies passive et general. Arch. Gen. Intern. Med. 1823;1:188–204. [Google Scholar]
- 2.Timp J.F., Braekkan S.K., Versteeg H.H., Cannegieter S.C. Epidemiology of cancer-associated venous thrombosis. Blood. 2013;122:1712–1723. doi: 10.1182/blood-2013-04-460121. [DOI] [PubMed] [Google Scholar]
- 3.Blom J.W., Doggen C.J.M., Osanto S., Rosendaal F.R. Malignancies, Prothrombotic Mutations, and the Risk of Venous Thrombosis. JAMA. 2005;293:715–722. doi: 10.1001/jama.293.6.715. [DOI] [PubMed] [Google Scholar]
- 4.Khorana A.A. Venous thromboembolism and prognosis in cancer. Thromb. Res. 2010;125:490–493. doi: 10.1016/j.thromres.2009.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donnellan E., Khorana A.A. Cancer and Venous Thromboembolic Disease: A Review. Oncologist. 2017;22:199–207. doi: 10.1634/theoncologist.2016-0214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khorana A.A., Francis C.W., Culakova E., Kuderer N.M., Lyman G.H. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J. Thromb. Haemost. 2007;5:632–634. doi: 10.1111/j.1538-7836.2007.02374.x. [DOI] [PubMed] [Google Scholar]
- 7.Kekre N., Connors J.M. Venous thromboembolism incidence in hematologic malignancies. Blood Rev. 2019;33:24–32. doi: 10.1016/j.blre.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 8.Colombo R., Gallipoli P., Castelli R. Thrombosis and hemostatic abnormalities in hematological malignancies. Clin. Lymphoma Myeloma Leuk. 2014;14:441–450. doi: 10.1016/j.clml.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Palumbo A., Rajkumar S.V., Dimopoulos M.A., Richardson P.G., San Miguel J., Barlogie B., Harousseau J., Zonder J.A., Cavo M., Zangari M., et al. Prevention of thalidomide-and lenalidomide-associated thrombosis in myeloma. Leukemia. 2008;22:414–423. doi: 10.1038/sj.leu.2405062. [DOI] [PubMed] [Google Scholar]
- 10.Hohaus S., Bartolomei F., Cuccaro A., Maiolo E., Alma E., D’alò F., Bellesi S., Rossi E., De Stefano V. Venous thromboembolism in lymphoma: Risk stratification and antithrombotic prophylaxis. Cancers. 2020;12:1291. doi: 10.3390/cancers12051291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Falanga A., Marchetti M. Thrombosis in myeloproliferative neoplasms. Semin. Thromb. Hemost. 2014;40:348–358. doi: 10.1055/s-0034-1370794. [DOI] [PubMed] [Google Scholar]
- 12.Montesinos P., de la Serna J., Vellenga E., Rayon C., Bergua J., Parody R., Esteve J., Gonzalez M., Brunet S., Sanz M. Incidence and Risk Factors for Thrombosis in Patients with Acute Promyelocytic Leukemia. Experience of the PETHEMA LPA96 and LPA99 Protocols. Blood. 2006;108:1503. doi: 10.1182/blood.V108.11.1503.1503. [DOI] [Google Scholar]
- 13.Gurnari C., Breccia M., Di Giuliano F., Scalzulli E., Divona M., Piciocchi A., Cicconi L., De Bellis E., Venditti A., Del Principe M.I., et al. Early intracranial haemorrhages in acute promyelocytic leukaemia: Analysis of neuroradiological and clinico-biological parameters. Br. J. Haematol. 2021;193:129–132. doi: 10.1111/bjh.17018. [DOI] [PubMed] [Google Scholar]
- 14.Ku G.H., White R.H., Chew H.K., Harvey D.J., Zhou H., Wun T. Venous thromboembolism in patients with acute leukemia: Incidence, risk factors, and effect on survival. Blood. 2009;113:3911–3917. doi: 10.1182/blood-2008-08-175745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Stefano V., Sorà F., Rossi E., Chiusolo P., Laurenti L., Fianchi L., Zini G., Pagano L., Sica S., Leone G. The risk of thrombosis in patients with acute leukemia: Occurrence of thrombosis at diagnosis and during treatment. J. Thromb. Haemost. 2005;3:1985–1992. doi: 10.1111/j.1538-7836.2005.01467.x. [DOI] [PubMed] [Google Scholar]
- 16.Libourel E.J., Klerk C.P.W., van Norden Y., de Maat M.P.M., Kruip M.J., Sonneveld P., Löwenberg B., Leebeek F.W.G. Disseminated intravascular coagulation at diagnosis is a strong predictor for thrombosis in acute myeloid leukemia. Blood. 2016;128:1854–1861. doi: 10.1182/blood-2016-02-701094. [DOI] [PubMed] [Google Scholar]
- 17.Martella F., Cerrano M., Di Cuonzo D., Secreto C., Olivi M., Apolito V., D’Ardia S., Frairia C., Giai V., Lanzarone G., et al. Frequency and risk factors for thrombosis in acute myeloid leukemia and high-risk myelodysplastic syndromes treated with intensive chemotherapy: A two centers observational study. Ann. Hematol. 2022;101:855–867. doi: 10.1007/s00277-022-04770-6. [DOI] [PubMed] [Google Scholar]
- 18.Falanga A., Barbui T., Rickles F.R. Hypercoagulability and tissue factor gene upregulation in hematologic malignancies. Semin. Thromb. Hemost. 2008;34:204–210. doi: 10.1055/s-2008-1079262. [DOI] [PubMed] [Google Scholar]
- 19.Falanga A., Schieppati F., Russo D. Cancer Tissue Procoagulant Mechanisms and the Hypercoagulable State of Patients with Cancer. Semin. Thromb. Hemost. 2015;41:756–764. doi: 10.1055/s-0035-1564040. [DOI] [PubMed] [Google Scholar]
- 20.Kwaan H.C. Double hazard of thrombophilia and bleeding in leukemia. Hematol. Am. Soc. Hematol. Educ. Program. 2007;2007:151–157. doi: 10.1182/asheducation-2007.1.151. [DOI] [PubMed] [Google Scholar]
- 21.Lyman G.H., Eckert L., Wang Y., Wang H., Cohen A. Venous Thromboembolism Risk in Patients with Cancer Receiving Chemotherapy: A Real-World Analysis. Oncologist. 2013;18:1321–1329. doi: 10.1634/theoncologist.2013-0226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Franchini M., Di Minno M.N.D., Coppola A. Disseminated intravascular coagulation in hematologic malignancies. Semin. Thromb. Hemost. 2010;36:388–403. doi: 10.1055/s-0030-1254048. [DOI] [PubMed] [Google Scholar]
- 23.Levi M., Sivapalaratnam S. Disseminated intravascular coagulation: An update on pathogenesis and diagnosis. Expert Rev. Hematol. 2018;11:663–672. doi: 10.1080/17474086.2018.1500173. [DOI] [PubMed] [Google Scholar]
- 24.Suzuki K., Wada H., Imai H., Iba T., Thachil J., Toh C.H. A re-evaluation of the D-dimer cut-off value for making a diagnosis according to the ISTH overt-DIC diagnostic criteria: Communication from the SSC of the ISTH. J. Thromb. Haemost. 2018;16:1442–1444. doi: 10.1111/jth.14134. [DOI] [PubMed] [Google Scholar]
- 25.Döhner H., Estey E., Grimwade D., Amadori S., Appelbaum F.R., Büchner T., Dombret H., Ebert B.L., Fenaux P., Larson R.A., et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–447. doi: 10.1182/blood-2016-08-733196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tallman M.S., Wang E.S., Altman J.K., Appelbaum F.R., Bhatt V.R., Bixby D., Coutre S.E., De Lima M., Fathi A.T., Fiorella M., et al. Acute Myeloid Leukemia, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2019;17:721–749. doi: 10.6004/jnccn.2019.0028. [DOI] [PubMed] [Google Scholar]
- 27.Gulati M., Levy P.D., Mukherjee D., Amsterdam E., Bhatt D.L., Birtcher K.K., Blankstein R., Boyd J., Bullock-Palmer R.P., Conejo T., et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2021;78:e187–e285. doi: 10.1016/j.jacc.2021.07.053. [DOI] [PubMed] [Google Scholar]
- 28.Napolitano M., Saccullo G., Marietta M., Carpenedo M., Castaman G., Cerchiara E., Chistolini A., Contino L., De Stefano V., Falanga A., et al. Platelet cut-off for anticoagulant therapy in thrombocytopenic patients with blood cancer and venous thromboembolism: An expert consensus. Blood Transfus. 2019;17:171–180. doi: 10.2450/2018.0143-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Napolitano M., Valore L., Malato A., Saccullo G., Vetro C., Mitra M.E., Fabbiano F., Mannina D., Casuccio A., Lucchesi A., et al. Management of venous thromboembolism in patients with acute leukemia at high bleeding risk: A multi-center study. Leuk. Lymphoma. 2016;57:116–119. doi: 10.3109/10428194.2015.1046864. [DOI] [PubMed] [Google Scholar]
- 30.Falanga A., Leader A., Ambaglio C., Bagoly Z., Castaman G., Elalamy I., Lecumberri R., Niessner A., Pabinger I., Szmit S., et al. EHA Guidelines on Management of Antithrombotic Treatments in Thrombocytopenic Patients with Cancer. HemaSphere. 2022;6:e750. doi: 10.1097/HS9.0000000000000750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Del Principe M.I., Del Principe D., Venditti A. Thrombosis in adult patients with acute leukemia. Curr. Opin. Oncol. 2017;29:448–454. doi: 10.1097/CCO.0000000000000402. [DOI] [PubMed] [Google Scholar]
- 32.Vu K., Luong N.V., Hubbard J., Zalpour A., Faderl S., Thomas D.A., Yang D., Kantarjian H., Kroll M.H. A retrospective study of venous thromboembolism in acute leukemia patients treated at the university of texas MD anderson cancer center. Cancer Med. 2015;4:27–35. doi: 10.1002/cam4.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mirza A.S., Yun S., Ali N.A., Shin H., O’Neil J.L., Elharake M., Schwartz D., Robinson K., Nowell E., Engle G., et al. Validation of the Khorana score in acute myeloid leukemia patients: A single-institution experience. Thromb. J. 2019;17:13. doi: 10.1186/s12959-019-0202-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Al-Ani F., Wang Y.P., Lazo-Langner A. Development of a Clinical Prediction Rule for Venous Thromboembolism in Patients with Acute Leukemia. Thromb. Haemost. 2020;120:322–328. doi: 10.1055/s-0039-3400303. [DOI] [PubMed] [Google Scholar]
- 35.Razak N.B.A., Jones G., Bhandari M., Berndt M.C., Metharom P. Cancer-associated thrombosis: An overview of mechanisms, risk factors, and treatment. Cancers. 2018;10:380. doi: 10.3390/cancers10100380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Connolly G.C., Khorana A.A. Emerging risk stratification approaches to cancer-associated thrombosis: Risk factors, biomarkers and a risk score. Thromb. Res. 2010;125:S1–S7. doi: 10.1016/S0049-3848(10)00227-6. [DOI] [PubMed] [Google Scholar]
- 37.Wun T., White R.H. Venous thromboembolism (VTE) in patients with cancer: Epidemiology and risk factors. Cancer Investig. 2009;27:63–74. doi: 10.1080/07357900802656681. [DOI] [PubMed] [Google Scholar]
- 38.Khorana A.A., Kuderer N.M., Culakova E., Lyman G.H., Francis C.W. Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood. 2008;111:4902–4907. doi: 10.1182/blood-2007-10-116327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levi M., Toh C.H., Thachil J., Watson H.G. Guidelines for the diagnosis and management of disseminated intravascular coagulation. Br. J. Haematol. 2009;145:24–33. doi: 10.1111/j.1365-2141.2009.07600.x. [DOI] [PubMed] [Google Scholar]
- 40.Weltermann A., Pabinger I., Geissler K., Jäger U., Gisslinger H., Knöbl P., Eichinger S., Kyrie P.A., Valent P., Speiser W., et al. Hypofibrinogenemia in non-M3 acute myeloid leukemia. Incidence, clinical and laboratory characteristics and prognosis. Leukemia. 1998;12:1182–1186. doi: 10.1038/sj.leu.2401101. [DOI] [PubMed] [Google Scholar]
- 41.Murray J., Precious E., Alikhan R. Catheter-related thrombosis in cancer patients. Br. J. Haematol. 2013;162:746–757. doi: 10.1111/bjh.12474. [DOI] [PubMed] [Google Scholar]
- 42.Geerts W. Central venous catheter-related thrombosis. Hematol. Am. Soc. Hematol. Educ. Program. 2014;1:306–311. doi: 10.1182/asheducation-2014.1.306. [DOI] [PubMed] [Google Scholar]
- 43.Grilz E., Königsbrügge O., Posch F., Schmidinger M., Pirker R., Lang I.M., Pabinger I., Ay C. Frequency, risk factors, and impact on mortality of arterial thromboembolism in patients with cancer. Haematologica. 2018;103:1549–1556. doi: 10.3324/haematol.2018.192419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Poh C., Brunson A., Keegan T., Wun T., Mahajan A. Incidence of Upper Extremity Deep Vein Thrombosis in Acute Leukemia and Effect on Mortality. TH Open. 2020;04:e309–e317. doi: 10.1055/s-0040-1718883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mohamed M.O., Lopez-Mattei J.C., Parwani P., Iliescu C.A., Bharadwaj A., Kim P.Y., Palaskas N.L., Rashid M., Potts J., Kwok C.S., et al. Management strategies and clinical outcomes of acute myocardial infarction in leukaemia patients: Nationwide insights from United States hospitalizations. Int. J. Clin. Pract. 2020;74:e13476. doi: 10.1111/ijcp.13476. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.