Abstract
Obesity is one of the major factors contributing to noncommunicable diseases (NCDs), which is associated with a high intake of a sugar-rich diet. Sugar blend (a novel combination of sugar and stevia) has half the calories of sugar with the same sweetness at recommended use and offers better compliance. A randomized controlled trial was conducted to evaluate the efficacy and safety of this sugar blend in normal to mildly overweight subjects with a body mass index (BMI) of 23–26 kg/m. Sixty subjects were categorized into Group A: Sugar group (n = 30), and Group B: Sugar blend group (n = 30). The primary outcomes evaluated were weight, waist circumference, hip circumference, waist/hip ratio, BMI, and the secondary outcomes evaluated were lipid profile, random blood sugar, and HbA1c. All these parameters were assessed at baseline, 30 days, 60 days, and 90 days. Group B showed a significantly higher weight loss (p = 0.013) at 90 days compared with Group A. A significant reduction in waist circumference (p < 0.0001) by 4.4 cm was noted at 90 days, in addition to reduction in total cholesterol (p < 0.0001), triglyceride (p = 0.006), LDL cholesterol (p = 0.0490), and VLDL cholesterol (p = 0.006) in Group B compared with the baseline. The study revealed that the sugar blend is an effective formulation in reducing weight, anthropometric factors, and other related metabolic parameters. It has been proven to be well tolerated and promotes weight loss when used in conjunction with a daily balanced diet and exercise plan.
Keywords: noncommunicable diseases (NCDs), body mass index (BMI), obesity, steviol glycosides (SGs), stevia, weight loss
1. Introduction
Obesity is caused by an increase in the consumption of high-fat, high-sugar energy-dense meals and decreased physical activity caused by the increasingly sedentary nature of many types of jobs, changing modes of transportation, and rising urbanization, as well as a lack of supportive policies in sectors such as health, agriculture, and others [1]. The consumption of sugar and sweets has been prominent in Indian culture, rituals, and religion [2]. People in India use roughly 25.17 kg of sugar per person/year, which is more than the worldwide per capita consumption of 23.7 kg per year [3]. Sweets and beverage consumption patterns among children are also changing fast [2]. A study revealed cola (sugar-sweetened beverages (SSBs)) consumption patterns among children and adolescents in urban India, with children and adolescents consuming about 1.8 cans of cola per week (540 mL/week; 1 can or 300 mL = 132 kcal and 33–40 g sugar), which might result in almost 1.3 kg of weight gain per child per year [2,4]. India’s rising sugar consumption per capita is a major problem and thus requires immediate attention [2]. The 66th round of the National Sample Survey Office (NSSO) 2009–2010 study indicated that roughly 13.2 teaspoons of white sugar were used per person/day in India in 2010 (55.3 g/day), up from 22 g/day in 2000 [5]. These values exceed the ones suggested by the National Institute of Nutrition’s Dietary Guidelines for Indians (2011), according to which healthy individuals should consume no more than 20–25 g of added sugar per day [6]. India is facing a potential healthcare crisis, owing to rising obesity rates and a significant shift in disease burden to NCDs, including cardiovascular disease (CVD), diabetes, hypertension, cancer, kidney disease, chronic respiratory disease, and nonalcoholic fatty liver disease [7,8,9]. According to the National Nutrition Monitoring Bureau (NNMB) 2016–2017 survey conducted among the urban population in India, 34% of men and 44% of women were overweight and obese. Further, about 22.3% of men and 22.4% of women had high cholesterol levels, while the overall prevalence of hypertension was found to be 31.1% and 26.1% among men and women, respectively [10]. A population-based cross-sectional study conducted in 15 states of India by the Indian Council of Medical Research–INdia DIABetes (ICMR-INDIAB) showed the overall prevalence of diabetes to be 7.3%, while that of prediabetes was 10.3% [11].
According to the World Health Organization (WHO) 2015 guidelines, free sugar intake should be decreased to less than 10% of total calorie intake in both adults and children [12]. In light of this remark, a range of measures targeted at lowering free sugar intake have been recommended, with food reformulation being one of the most notable options [13]. Regulating the calorie density of meals might be a revolutionary way to effective bodyweight loss by reducing energy consumption [14,15]. Sugar substitutes or low-calorie sweeteners (LCS) help lower the daily sugar and calorie intake. These dietary modifications can help in glycemic, weight, and cardiometabolic control [16]. Low-calorie sweeteners are employed in minute amounts to bestow the necessary degree of sweetness, while providing very little or no energy to the final product due to their strong sweetening power relative to sugars. These are simple approaches to cutting calories and sugars from our diet without compromising the enjoyment of sweet foods and beverages. Furthermore, because such calorie reductions are accomplished without a change in total dietary sweetness or palatability, such “sugar swaps” are anticipated to result in increased dietary compliance and better weight management results for individuals in the long run [14]. Natural LCS have gained immense interest in the toxicological acceptability and commercial development of steviol glycosides (SGs) [17]. Steviol glycoside, derived from Stevia rebaudiana Bertoni, provides no calories, and antioxidant properties, and is heat/pH stable [18,19,20]. When compared with sucrose, stevia is approximately 100 to 300 times sweeter [21]. Several Generally Recognized as Safe (GRAS) notices are received by the U.S. Food and Drug Administration (FDA) for the use of high-pure (at least 95% purity) SGs, among others, to which the FDA has no objection under the intended circumstances of use [22]. In addition, the acceptable daily intake (ADI) of 0–4 mg/kg BW, represented as steviol, was validated by the Joint Food and Agriculture Organization (FAO)/WHO Expert Committee on Food Additives [23].
People with conscious mindsets often try cutting down sugar or replacing sugar solely with LCS; however, compliance is the challenge. Sugar blend is a novel product manufactured with sugar and stevia combination that is 50% lower in calories when used as directed. It looks like crystal sugar and gives the same sweetness with half the amount of sugar. Stevia contributes to zero calories [17]. As a result, the use of sugar is reduced by 50%, and because it resembles sugar, it offers better compliance. This product lowers calorie consumption, which is linked to weight loss that in turn is associated with the prevention of diseases such as CVD. Moreover, it is an effective alternative for people who are habituated to high sugar intake with an insight into a healthy lifestyle, i.e., reduce calorie intake to maintain weight, yet desire the same appearance product as sugar. With this perspective, the current study was conducted to evaluate the efficacy and safety of completely replacing table sugar with sugar blend in the diet while maintaining a healthy lifestyle in healthy adults with a BMI of 23–26 kg/m2.
2. Material and Methods
2.1. Study Design
This was a randomized, open-label, two-arm, active-controlled, clinical trial.
2.2. Study Population
Over 60 subjects between the ages of 18 and 50 years were included in the study. The subjects were categorized into two groups:
Group A: Sugar group (n = 30), who consumed ordinary table sugar (sucrose) (Active, control group), and
Group B: Sugar blend group (n = 30), who substituted ordinary table sugar with half the quantity of sugar blend in their diet (Test group).
Inclusion criteria:
Normal to preobese participants (BMI = 23 kg/m2 to 26 kg/m2).
Subjects who are willing to provide written informed consent.
Those who agree to follow the general dietary, sugar intake, and exercise guidelines.
Subjects who have not taken part in a comparable study in the previous four weeks.
Exclusion criteria:
Subjects who have hypertension, renal, hepatic, or cardiac failure.
Endocrine diseases, such as hypothyroidism (if already on treatment).
Subjects with dyslipidemia or fat metabolic inborn errors.
Subjects who have postprandial glucose of more than 150 mg/dL in two tests and are considered early diabetics.
Any history of medication hypersensitivity or an adverse reaction that might affect the study.
Antidiabetic medicines such as metformin and statins, as well as nutritional supplements that may affect body weight, body fat, or blood cholesterol levels.
Women who are pregnant or lactating.
Refusal to sign an informed consent form.
2.3. Study Protocol
In the sugar group, the subjects used regular table sugar in their diet. In the sugar blend group, the subjects were asked to replace regular table sugar with a standard amount of test product, i.e., sugar blend in beverages such as tea, coffee, smoothies, milk, and other food products, and the amount consumed was noted in the subject’s diary. The spoons given to the sugar group dispensed approximately 5 g, whereas the spoons given to the sugar blend group dispensed around 2.5 g product.
Additionally, subjects were asked to restrict their daily diet to 2300 kcal/day (for women) and 2500 kcal/day (for men) and record their daily food intake in diet diaries. During follow-ups, the diet diary was checked to ensure compliance, and subjects were asked to adhere to the above kcal restriction. The subjects were asked to follow a moderate-intensity exercise routine, either 45 min of brisk walking or gym exercises daily for at least 6 days a week.
The study documentation, including the study protocol, was approved by the Institutional Ethics Committee (IEC)-Lifeline Ethics Committee in a review meeting conducted in November 2019 and again in November 2020, and is registered with the Clinical Trial Registry of India (CTRI) under the reference number CTRI/2021/02/030921.
The analysis was done within the group for all parameters at baseline, 30 days, 60 days, and 90 days. In addition, the parameters in Groups A and B were compared at baseline, 30 days, 60 days, and 90 days.
2.3.1. Exception
Any additional sugar in both groups was allowed only at the discretion of the subject, who wished to attend a function or party not exceedingly once every month. The additional sugar consumed was picked up from a tabulated diary. Small discretion during daily life was allowed if the planned sugar intake was noted and recorded. No additional sugar substitute of any other kind was allowed other than the test product.
2.3.2. Primary Outcomes
The primary outcomes analyzed were changes in weight, waist circumference, hip circumference, and waist/hip (W/H) ratio, BMI, noted at baseline, 30 days, 60 days, and 90 days, respectively.
2.3.3. Secondary Outcomes
Biochemical investigation of blood lipid profile (total cholesterol, triglyceride, low-density lipoprotein (LDL) cholesterol, and very-low-density lipoprotein (VLDL) cholesterol, high-density lipoprotein (HDL)), random blood sugar (RBS), hemoglobin A1c (HbA1c), and liver function test (serum glutamate pyruvate transaminase, serum glutamic oxaloacetic transaminase, gamma-glutamyl transferase, urea, serum creatinine) were conducted at start and end of the study. Blood lipids determination using the enzymatic colorimetry method and random sugar were measured at each visit on baseline, 30 days, 60 days, and 90 days.
2.3.4. Safety Evaluation
The safety of the test product in Group B subjects was evaluated. The clinicians (investigators, i.e., medical doctors) assessed the safety by observing if there were any adverse reactions reported by any subjects.
2.4. Statistical Analysis
Continuous variables such as age and instrumental readings were reported using descriptive statistics (mean, standard deviation (SD), number of subjects (n), median, and range), whereas categorical variables such as gender, race, and other factors were characterized using count (n) and percentage (%) of subjects. All comparisons within and between groups were performed using two-tailed paired t-tests and independent sample t-tests with a significance threshold of 5%, respectively. Correlation coefficients between the primary and secondary parameters were also computed. All statistical analyses were performed using XLSTAT—2019 by Addinsoft LLC (Paris, France).
3. Results
The baseline characteristics of both groups are listed in Table 1.
Table 1.
Baseline characteristics of both groups.
| Group A | Group B | p Value * | |
|---|---|---|---|
| Total subjects (n) | 30 | 30 | |
| Male | 18 | 17 | |
| Female | 12 | 13 | |
| Aged 30 years or below | 13 | 15 | |
| Aged between 31 and 39 years | 11 | 6 | |
| Aged 40 years and above | 6 | 9 | |
| Weight (kg) † | 64.963 ± 9.861 | 66.993 ± 8.308 | 0.392 |
| Waist (cm) † | 88.533 ± 7.637 | 88.567 ± 6.755 | 0.986 |
| Hip (cm) † | 97.333 ± 7.373 | 99.867 ± 5.07 | 0.126 |
| Waist/hip ratio † | 0.905 ± 0.058 | 0.882 ± 0.052 | 0.118 |
| BMI (kg/m2) † | 24.01 ± 2.271 | 24.673 ± 2.023 | 0.204 |
| Total cholesterol (mg/dL) † | 176.3 ± 23.476 | 187.80 ± 32.964 | 0.125 |
| Triglyceride (mg/dL) † | 159.167 ± 70.445 | 177.733 ± 84.736 | 0.360 |
| HDL cholesterol (mg/dL) † | 36.667 ± 5.862 | 38.567 ± 5.952 | 0.218 |
| LDL cholesterol (mg/dL) † | 107.867 ± 17.795 | 113.64 ± 31.73 | 0.388 |
| VLDL cholesterol (mg/dL) † | 31.833 ± 14.089 | 35.58 ± 16.929 | 0.355 |
| RBS (mg/dL) † | 95.567 ± 17.561 | 93.10 ± 14.456 | 0.555 |
| HbA1c % † | 5.53 ± 0.447 | 5.57 ± 0.462 | 0.735 |
BMI: Body mass index; HDL: High-density lipoprotein; LDL: Low-density lipoprotein; VLDL: Very-low-density lipoprotein; RBS: Random blood sugar; HbA1c: Hemoglobin A1c. † All values are presented as mean ± standard deviation. * p values significant depicting baseline comparison between Groups A and B.
3.1. Weight
Both Groups A and B had significant differences in body weight at 90 days compared with the baseline (p < 0.0001) (Table 2). In Group B, there was a significant weight reduction (p = 0.0004) at 60 days compared with the baseline (Table 3).
Table 2.
Change in weight, waist circumference (cm), hip circumference (cm), and waist/hip ratio within the group at 90 days.
| Group A | Group B | |||||
|---|---|---|---|---|---|---|
| Baseline | Day 90 | p Value | Baseline | Day 90 | p Value | |
| Weight in kg (mean ± SD) | 64.963 ± 9.861 | 63.067 ± 9.791 | <0.0001 * | 66.993 ± 8.308 | 63.600 ± 8.071 | <0.0001 * |
| Mean reduction in kg (%) | −1.897 (2.936) | −3.393 (5.037) | ||||
| Waist Circumference in cm (mean ± SD) | 88.533 ± 7.637 | 84.633 ± 9.779 | 0.001 * | 88.567 ± 6.755 | 84.167 ± 6.385 | <0.0001 * |
| Mean reduction in cm (%) | −3.90 (4.462) | −4.40 (4.931) | ||||
| Hip circumference in cm (mean ± SD) | 97.333 ± 7.373 | 94.900 ± 6.599 | <0.0001 * | 99.867 ± 5.070 | 97.133 ± 4.897 | <0.0001 * |
| Mean reduction in cm (%) | −2.433 (2.441) | - | −2.733 (2.703) | |||
| Waist/hip ratio (mean ± SD) | 0.905 ± 0.058 | 0.900 ± 0.05 | 0.495 | 0.882 ± 0.052 | 0.862 ± 0.045 | <0.0001 * |
| Mean reduction (%) | −0.005 (0.389) | −0.02 (2.24) | ||||
| BMI in kg/m2 (mean ± SD) |
24.01 ± 2.271 |
23.323 ± 2.461 | <0.0001 * | 24.673 ± 2.023 | 23.447 ± 2.301 | <0.0001 * |
SD: Standard deviation. * p values significant depicting the comparison with the baseline.
Table 3.
Change in weight (kg), waist circumference (cm), hip circumference (cm), waist/hip ratio, and body mass index between groups.
| Parameters | Baseline | Day 30 | Day 60 | Day 90 | ||||
|---|---|---|---|---|---|---|---|---|
| Group A | Group B | Group A | Group B | Group A | Group B | Group A | Group B | |
| Weight (kg) † | 64.963 ± 9.861 | 66.993 ± 8.308 | 64.250 ± 9.669 | 66.160 ± 8.460 | 63.807 ± 9.838 | 64.583 ± 8.267 | 63.067 ± 9.791 | 63.600 ± 8.071 |
|
p value (between groups) p value (within group) |
0.392 | 0.419 | 0.742 0.0004 ** |
0.819 | ||||
| Weight difference (kg) from baseline † | 0.713 ± 0.606 | 0.833 ± 1.475 | 1.157 ± 0.716 | 2.410 ± 3.313 | 1.897 ± 1.739 | 3.393 ± 2.688 | ||
| p value (between groups) | 0.682 | 0.047 * | 0.013 * | |||||
| Weight difference % † | 1.081 ± 0.922 | 1.276 ± 2.393 | 1.824 ± 1.297 | 3.540 ± 4.427 | 2.936 ± 2.771 | 5.037 ± 3.650 | ||
| p value (between groups) | 0.679 | 0.046 * | 0.015 * | |||||
| Waist circumference (cm) † | 88.533 ± 7.637 | 88.567 ± 6.755 | 87.000 ± 7.579 | 86.833 ± 6.721 | 86.200 ± 7.595 | 85.967 ± 6.392 | 84.633 ± 9.779 | 84.167 ± 6.385 |
|
p value (between groups) p value (within group) |
0.986 | 0.929 | 0.898 <0.0001 ** |
0.828 | ||||
| Waist circumference difference (cm) from baseline † | 1.533 ± 1.358 | 1.733 ± 1.946 | 2.333 ± 1.882 | 2.600 ± 2.824 | 3.900 ± 5.744 | 4.400 ± 2.283 | ||
| p value (between groups) | 0.646 | 0.668 | 0.659 | |||||
| Waist circumference difference % † | 1.724 ± 1.519 | 1.941 ± 2.150 | 2.626 ± 2.060 | 2.870 ± 3.197 | 4.462 ± 7.042 | 4.931 ± 2.432 | ||
| p value (between groups) | 0.654 | 0.727 | 0.731 | |||||
| Hip circumference (cm) † | 97.333 ± 7.373 | 99.867 ± 5.070 | 96.167 ± 6.859 | 98.567 ± 4.876 | 95.700 ± 6.737 | 97.167 ± 4.800 | 94.900 ± 6.599 | 97.133 ± 4.897 |
|
p value (between group) p value (within group) |
0.126 | 0.124 | 0.336 <0.0001 ** |
0.142 | ||||
| Hip circumference difference (cm) from baseline † | 1.167 ± 1.642 | 1.300 ± 2.020 | 1.633 ± 2.748 | 2.700 ± 2.351 | 2.433 ± 1.995 | 2.733 ± 2.703 | ||
| p value (between groups) | 0.780 | 0.112 | 0.627 | |||||
| Hip circumference difference % † | 1.156 ± 1.617 | 1.277 ± 1.983 | 1.608 ± 2.729 | 2.672 ± 2.237 | 2.441 ± 1.887 | 2.703 ± 2.588 | ||
| p value (between groups) | 0.797 | 0.104 | 0.656 | |||||
| Waist/hip ratio † | 0.905 ± 0.058 * | 0.882 ± 0.052 | 0.899 ± 0.046 | 0.878 ± 0.050 | 0.896 ± 0.053 | 0.880 ± 0.048 | 0.900 ± 0.050 | 0.862 ± 0.045 |
| p value (between groups) | 0.118 | 0.098 | 0.244 | 0.003* | ||||
| Waist/hip ratio difference from baseline † | 0.005 ± 0.034 | 0.004 ± 0.016 | 0.009 ± 0.037 | 0.002 ± 0.027 | 0.005 ± 0.037 | 0.020 ± 0.023 | ||
| p value (between groups) | 0.809 | 0.387 | 0.052 | |||||
| Waist/hip ratio difference % † | 0.456 ± 3.648 | 0.388 ± 1.785 | 0.885 ± 3.972 | 0.119 ± 3.105 | 0.389 ± 4.049 | 2.240 ± 2.524 | ||
| p value (between groups) | 0.927 | 0.409 | 0.038 * | |||||
| BMI (kg/m2) † | 24.01 ± 2.271 | 24.674 ± 2.023 | 23.751 ± 2.259 | 24.376 ± 2.283 | 23.578 ± 2.311 | 23.822 ± 2.476 | 23.323 ± 2.461 | 23.447 ± 2.301 |
| p value (between groups) | 0.24 | 0.29 | 0.69 | 0.84 | ||||
BMI: Body mass index. † All values are presented as mean ± standard deviation. * p values significant depicting the comparison between Groups A and B (between-groups independent sample t-test). ** p values significant depicting the comparison between Group B and the baseline (within Group B paired t-test).
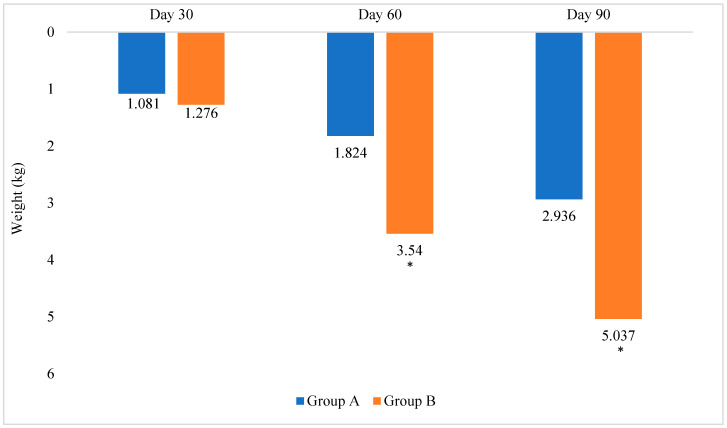
Group B showed a higher weight loss compared with Group A (p = 0.013). At 90 days, Group B lost 3.393 kg (about 5% body weight) from the baseline, while Group A lost 1.897 kg (2.9% body weight) from the baseline (Figure 1) and (Table 3).
Figure 1.
Change in weight (%) from the baseline. * p value significant depicting the comparison between Groups A and B.
Group B lost approximately 1.7 times more weight than Group A at the end of 90 days, compared with the baseline.
3.2. Waist Circumference
Within Groups A and B, a significant difference was observed in waist circumference at 90 days compared with the baseline (p = 0.001; p < 0.0001, respectively). Group B had a mean waist circumference reduction of 4.4 cm after 90 days (Table 2). In Group B, there was also a significant reduction in waist circumference (p < 0.0001) at 60 days compared with the baseline (Table 3).
However, between Groups A and B, there was no significant difference in waist circumference at 90 days (Table 3).
3.3. Hip Circumference
Within both groups, a significant difference was observed in hip circumference at 90 days compared with the baseline (p < 0.0001). In Group B, a mean hip circumference reduction of 2.7 cm was observed at 90 days (Table 2), and a significant reduction in hip circumference (p < 0.0001) was observed at 60 days compared with the baseline (Table 3).
However, between Groups A and B, there was no significant difference in hip circumference at 90 days (Table 3).
3.4. Waist/Hip Ratio
Group B had a significant change in W/H ratio from baseline 0.882 ± 0.052 to 0.862 ± 0.045 at 90 days (p < 0.0001), whereas it was nonsignificant in Group A (Table 2).
There was no significant difference in the W/H ratio from baseline between Groups A and B at 90 days (Table 3).
3.5. Body Mass Index (BMI)
Between Groups A and B, there was no significant difference in the BMI values at 90 days. Within Groups A and B, a significant reduction in the BMI was observed at 90 days when compared to baseline (Table 2).
3.6. Secondary Outcomes
In within-group analysis, Group B showed a significant reduction in total cholesterol (p < 0.0001), triglyceride (p = 0.006), LDL cholesterol (p = 0.0490), VLDL cholesterol (p = 0.006), RBS (p = 0.028), and HbA1c (p < 0.0001) at the end of 90 days compared with the baseline. Between Groups A and B, there was no significant difference in, lipid profile, RBS, or HbA1c values. These blood parameters were within the clinical reference range (Table 4).
Table 4.
Secondary outcomes.
| Parameters | Baseline | Day 30 | Day 60 | Day 90 | ||||
|---|---|---|---|---|---|---|---|---|
| Group A | Group B | Group A | Group B | Group A | Group B | Group A | Group B | |
| Total cholesterol (mg/dL) † | 176.300 ± 23.476 | 187.800 ± 32.964 | 179.900 ± 25.841 | 182.367 ± 28.695 | 175.533 ± 24.274 | 171.333 ± 35.856 | 179.667 ± 22.225 | 175.333 ± 28.585 |
|
p value (between groups) p value (within group) |
0.125 | 0.728 | 0.597 | 0.515 <0.0001 * |
||||
| Triglyceride (mg/dL) † | 159.167 ± 70.445 | 177.733 ± 84.736 | 157.100 ± 68.364 | 154.667 ± 52.341 | 150.000 ± 61.630 | 151.167 ± 48.471 | 149.533 ± 58.819 | 150.500 ± 43.793 |
|
p value (between groups) p value (within group) |
0.360 | 0.878 | 0.935 | 0.943 0.006 * |
||||
| HDL (mg/dL) † | 36.667 ± 5.862 | 38.567 ± 5.952 | 38.067 ± 5.271 | 39.267 ± 5.375 | 37.767 ± 4.439 | 39.300 ± 5.522 | 38.633 ± 4.745 | 38.300 ± 4.801 |
| p value (between groups) | 0.218 | 0.386 | 0.241 | 0.788 | ||||
| LDL (mg/dL) † | 107.867 ± 17.795 | 113.640 ± 31.730 | 110.500 ± 18.877 | 112.167 ± 26.019 | 107.633 ± 18.669 | 104.613 ± 26.833 | 110.633 ± 17.616 | 106.933 ± 25.377 |
|
p value (between groups) p value (within group) |
0.388 | 0.777 | 0.615 | 0.514 0.0490 * |
||||
| VLDL (mg/dL) † | 31.833 ± 14.089 | 35.580 ± 16.929 | 31.467 ± 13.673 | 30.933 ± 10.468 | 29.333 ± 12.337 | 31.967 ± 13.895 | 30.373 ± 11.746 | 30.167 ± 8.789 |
|
p value (between groups) p value (within group) |
0.355 | 0.866 | 0.551 | 0.939 0.006 * |
||||
| RBS (mg/dL) † | 95.567 ± 17.561 | 93.100 ± 14.456 | 90.467 ± 12.252 | 93.200 ± 16.606 | 89.333 ± 9.925 | 84.962 ± 19.622 | 89.967 ± 8.002 | 86.767 ± 16.400 |
|
p value (between groups) p value (within group) |
0.555 | 0.471 | 0.281 | 0.341 0.028 * |
||||
| HbA1c % † | 5.530 ± 0.447 | 5.570 ± 0.462 | 5.527 ± 0.376 | 5.483 ± 0.424 | 5.537 ± 0.334 | 5.377 ± 0.387 | 5.520 ± 0.350 | 5.437 ± 0.420 |
|
p value (between groups) p value (within group) |
0.735 | 0.677 | 0.092 | 0.407 <0.0001 * |
||||
HDL: High-density lipoprotein; LDL: Low-density lipoprotein; VLDL: Very-low-density lipoprotein; RBS: Random blood sugar; HbA1c: Hemoglobin A1c. † All values are presented as mean ± standard deviation. * p values significant depicting the comparison between Group B and the baseline (within Group B paired t-test).
3.7. Safety Evaluation
Overall, the sugar blend was well tolerated and there were no dropouts or complaints in the study. No adverse events were reported during the trial period, and no adverse changes in biochemical secondary parameters (blood lipid profile, blood glucose levels) were seen. Hence, the product could be considered safe.
4. Discussion
People in India are at an elevated risk of metabolic disorders owing to a higher metabolic load. It is believed that for every given level of BMI, there is a proportionally higher ratio of fat to lean mass, and as BMI rises, the metabolic load rises too. Therefore, preventing excess weight gain, abdominal obesity, and sedentary behavior, as well as a transition to low-glycemic index and lower fat diets, are necessary [24]. A diet that can self-regulate dietary energy intake can play a key role in long-term weight loss, weight maintenance, and body weight gain prevention [15].
According to World Health Organization (WHO) 2015 guidelines, free sugar intake should be kept to less than 10% of total calorie intake in both adults and children [12]. Sugar restriction while retaining natural taste and appearance in products is a revolutionary concept that sugar blend has achieved with a balanced formulation of natural sweetener stevia and sugar in a proportion to produce the same sweetness of sugar at 50% consumption as instructed. Half the quantity of sugar blend, i.e., 2.5 g of sugar blend is equivalent to 5 g of table sugar in sweetness, thereby giving 50% lesser calories. The present study was conducted to enumerate the benefits of sugar blend in healthy adults.
WHO classified stevia as a natural sweetener in its noncaloric sweetener classification (i.e., natural and artificial) [25,26]. In the United States, it is widely recognized as a natural sweetener, and imagery and “natural” phraseology are utilized in many parts of the world to communicate to customers the usage of natural-origin plant-based stevia sweeteners [25]. The Food Safety and Standard Authority of India has approved steviol glycoside intense sweetener SG (INS 960) as a sweetener. The standard for this sweetener is defined in “The Food Safety and Standards (Food Products Standards and Food Additives) Regulations, 2011, Clause 3.2.2 (1)” [27].
In India, any celebration is traditionally marked by the consumption of sweets. After every meal, any happy event, religious holiday, social gathering, etc., it is a tradition to “sweeten the tongue” [2]. Excess sugar consumption leads to the buildup of body fat and intra-abdominal fat, increased insulin resistance, excess liver fat, hypertriglyceridemia, increased free fatty acids, hyperuricemia, and diabetes among other metabolic disorders [3]. According to a recent report by the Scientific Advisory Committee on Nutrition (SACN), there is some evidence that SSBs are associated with weight gain, as well as consistent evidence that they are linked to an elevated risk of type 2 diabetes mellitus [28]. Further, obesity, like other cardiovascular risk factors, contributes to the development of CVD and associated mortality [29]. Non-nutritive sweeteners can help people cut back on added sugars, resulting in calorie reduction and weight loss/control, as well as positive impacts on metabolic parameters. Nonetheless, if there is a compensatory increase in calorie intake from other sources, these potential advantages will not be completely realized [30]. The American Heart Association (AHA) and the American Diabetes Association (ADA) issued a joint statement saying that stevia and comparable sweeteners can help patients with diabetes provided they use them correctly and do not compensate by consuming more calories later in the day [30].
Overweight and obesity are caused by an energy imbalance between calories ingested and calories burned [1]. One pound of body weight is 3500 calories. This indicates that if a person cuts (or adds) 500 calories to the daily diet, they will lose (or gain) one pound every week, i.e., 500 calories each day multiplied by seven days equals 3500 calories [31]. Therefore, at least 45 min of moderate-intensity physical activity 5 days a week is also advisable. This level of physical exercise may lower the chance of developing some chronic conditions [6].
The current study aims to understand the effect of sugar replacement with blended sugar, which gives the same sweetness in half the amount. A mere cut down in sugar kcal, without compromising the sweetness, can help in improving metabolic parameters and weight loss. Here, when sugar was substituted with sugar blend, which resulted in consumption of just 50% sugars, the weight loss was 3.393 kg (p < 0.013) compared to 1.897 kg in the sugar group, indicating that there is a calorie reduction and weight loss, as well as a healthy strategy of losing weight with better compliance. The effect of confounding factors such as physical activity was also taken into consideration. There was a weight loss in the sugar group, which could be due to dietary restrictions and a moderate physical activity routine; however, more weight loss was observed in the sugar blend group, which could be due to physical activity along with the kcal deficit.
In addition, compared with the baseline, a significant mean reduction was noted in the sugar blend group in metabolic parameters at the end of the study (90 days) owing to weight loss that is related to a reduction in calories. The HbA1c levels dropped slightly, showing that the product helped in lowering blood sugar in conjunction with calorie reduction and subsequent weight loss. An increase in these cardiometabolic parameters denotes the risk factors for diseases such as CVD, diabetes, etc., and altering these parameters would help in disease prevention.
At 90 days, the sugar blend group had a significant waist circumference reduction of 4.4 cm (p < 0.0001) and hip circumference reduction of 2.7 cm (p < 0.0001) from baseline.
This is a free-living trial; simply substituting sugar with sugar blend, a similar-looking product with half the calories in everyday life, would help people stimulate their routine, which in turn is associated with better outcomes. Better compliance offered by the product will assist people in losing weight. Sugar blend was found to reduce 1.7 times more weight than the regular table sugar (no substitution) along with physical activity, which could be attributed to the consumption of half the amount of sugar blend, thereby reducing the overall caloric intake. Reduction in calorie intake along with increasing calorie expenditure and regular exercise could lead to an energy deficit. It thus helped in weight loss, which in turn plays a remarkable role in CVD prevention.
The test product was found to be safe. In addition, the safety of stevia is established in the literature [23,32]. The Joint FAO/WHO Expert Committee has declared stevia to be safe [23].
Being an open-label, free-living community trial, there is a possibility that the results could have been influenced by the nature of the treatment and participant behavior. Although the sugar blend has a positive influence on body weight and other cardiometabolic parameters, the small sample size and possible ambiguity in the results due to participants’ personal choices necessitate further research on other metabolic parameters under a controlled environment.
5. Conclusions
Indians are at an elevated risk of metabolic disorders owing to higher metabolic load. It is believed that there is a relatively higher ratio of fat to lean mass for any given level of BMI. With an increase in BMI, the metabolic load also increases. In this clinical trial, we observed that among healthy adults, replacing regular/ordinary table sugar with novel products such as sugar blend (a combination of sugar and stevia) provides the same sweetness as sugar and better compliance. Half the quantity, e.g., 2.5 g of sugar blend is equal in sweetness to 5 g of sugar, resulting in 50% fewer calories compared with table sugar. When used in conjunction with a daily balanced diet and exercise routine, the sugar blend can help reduce weight, waist circumference, hip circumference, and other metabolic parameters. Overall, sugar blend was proven to reduce 3.39 kg weight, 4.4 cm waist circumference, and 2.7 cm hip circumference after 90 days when used as part of a daily balanced diet and regular exercise. Sugar blend, when used in conjunction with a daily balanced diet and exercise routine, helped people lose 1.7 times more weight than ordinary sugar. In addition, the product was found to be well tolerated. Such sugar blends provide a meaningful way to dietary control of metabolism and weight control, and larger population studies in the future will gather momentum to provide this for use by the population at large.
Acknowledgments
We acknowledge the Medical Writing support provided by Medicca Press Limited.
Author Contributions
Conceptualization, G.R., A.M. and A.B.; methodology, G.R. and S.A.; software, J.S.P.; validation, S.K.P. (Sunil Kumar Prabhu), R.L. and A.R.; formal analysis, R.L. and A.R.; investigation, R.L. and A.R.; resources, S.A.; data curation, S.K.P. (Shashi Kishor Pankaj); writing—original draft preparation, S.K.P. (Shashi Kishor Pankaj); writing—review and editing, G.R., A.B. and S.K.P. (Shashi Kishor Pankaj); visualization, A.B.; supervision, G.R.; project administration, S.A. and S.K.P. (Sunil Kumar Prabhu). All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study documentation, including the study protocol, was approved by the Institutional Ethics Committee (IEC)-Lifeline Ethics Committee in a review meeting conducted in November 2019 and again in November 2020, and is registered with the Clinical Trial Registry of India (CTRI) under Reference Number CTRI/2021/02/030921.
Informed Consent Statement
Written informed consent was obtained from all study participants.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare that there are no conflict of interest regarding the publication of this article.
Funding Statement
This research was funded by Zydus Wellness Products Limited, Ahmedabad, India.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization Obesity and Overweight. Jun 9, 2021. [(accessed on 3 November 2021)]. pp. 1–6. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- 2.Gulati S., Misra A. Sugar Intake, Obesity, and Diabetes in India. Nutrients. 2014;6:5955–5974. doi: 10.3390/nu6125955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gulati S., Misra A. Abdominal obesity and type 2 diabetes in Asian Indians: Dietary strategies including edible oils, cooking practices and sugar intake. Eur. J. Clin. Nutr. 2017;71:850–857. doi: 10.1038/ejcn.2017.92. [DOI] [PubMed] [Google Scholar]
- 4.Gupta N., Shah P., Goel K., Misra A., Rastogi K., Vikram N.K., Kumari V., Pandey R.M., Kondal D., Wasir J.S., et al. Imbalanced dietary profile, anthropometry, and lipids in urban Asian Indian adolescents and young adults. J. Am. Coll. Nutr. 2010;29:81–91. doi: 10.1080/07315724.2010.10719820. [DOI] [PubMed] [Google Scholar]
- 5.Mathur P., Pillai R. Overnutrition: Current scenario & combat strategies. Indian J. Med. Res. 2019;149:695–705. doi: 10.4103/ijmr.IJMR_1703_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dietary Guidelines for Indians—A Manual. National Institute of Nutrition; Hyderabad, India: 2011. [(accessed on 3 November 2021)]. pp. 18–20. Available online: https://www.nin.res.in/downloads/DietaryGuidelinesforNINwebsite.pdf. [Google Scholar]
- 7.Dhawan D., Sharma S. Abdominal Obesity, Adipokines and Non-communicable Diseases. J. Steroid Biochem. Mol. Biol. 2020;203:105737. doi: 10.1016/j.jsbmb.2020.105737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kesztyüs D., Erhardt J., Schönsteiner D., Kesztyüs T. Therapeutic Treatment for Abdominal Obesity in Adults. Dtsch. Ärzteblatt Int. 2018;115:487–493. doi: 10.3238/arztebl.2018.0487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siddiqui Z., Donato R. The dramatic rise in the prevalence of overweight and obesity in India: Obesity transition and the looming health care crisis. World Dev. 2020;134:105050. doi: 10.1016/j.worlddev.2020.105050. [DOI] [Google Scholar]
- 10.National Nutrition Monitoring Bureau . Diet and Nutritional Status of Urban Population in India and Prevalence of Obesity, Hypertension, Diabetes and Hyperlipidemia in Urban Men and Women. National Institute of Nutrition; Hyderabad, India: 2017. [(accessed on 22 September 2021)]. pp. 13–19. Available online: https://www.nin.res.in/downloads/NNMB%20Urban%20Nutrition%20Report%20-Brief%20%20%20report.pdf. [Google Scholar]
- 11.Anjana R.M., Deepa M., Pradeepa R., Mahanta J., Narain K., Das H.K., Adhikari P., Rao P.V., Saboo B., Kumar A., et al. ICMR–INDIAB Collaborative Study Group. Prevalence of diabetes and prediabetes in 15 states of India: Results from the ICMR-INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5:585–596. doi: 10.1016/S2213-8587(17)30174-2. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization . Information Note about Intake of Sugars Recommended in the WHO Guideline for Adults and Children. World Health Organization; Geneva, Switzerland: 2015. [(accessed on 3 November 2021)]. Available online: https://apps.who.int/iris/rest/bitstreams/1234140/retrieve. [Google Scholar]
- 13.Sugar Reduction: Report on Progress between 2015 and 2019. [(accessed on 3 November 2021)];2020 October; Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/984282/Sugar_reduction_progress_report_2015_to_2019-1.pdf.
- 14.Low Calorie Sweeteners: Role and Benefits a Guide to the Science of Low Calorie Sweeteners. Sep, 2018. [(accessed on 3 November 2021)]. Available online: https://www.sweeteners.org/wp-content/uploads/2020/09/isa_booklet_september_2018.pdf.
- 15.Stelmach-Mardas M., Rodacki T., Dobrowolska-Iwanek J., Brzozowska A., Walkowiak J., Wojtanowska-Krosniak A., Zagrodzki P., Bechthold A., Mardas M., Boeing H. Link between Food Energy Density and Body Weight Changes in Obese Adults. Nutrients. 2016;8:229. doi: 10.3390/nu8040229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Evert A.B., Dennison M., Gardner C.D., Garvey W.T., Lau K.H.K., MacLeod J., Mitri J., Pereira R.F., Rawlings K., Robinson S., et al. Nutrition Therapy for Adults with Diabetes or Prediabetes: A Consensus Report. Diabetes Care. 2019;42:731–754. doi: 10.2337/dci19-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fry J.C. Natural low-calorie sweeteners. In: Baines D., Seal R., editors. Natural Food Additives, Ingredients and Flavourings. Woodhead Publishing; Cambridge, UK: 2012. [(accessed on 3 November 2021)]. pp. 41–75. (Woodhead Publishing Series in Food Science, Technology and Nutrition). Available online: http://www.gbv.de/dms/tib-ub-hannover/730478742.pdf. [Google Scholar]
- 18.Asrani U., Thakur D.A. A Comprehensive Review on Uses of Stevia Rebaudiana Plant. Eur. J. Mol. Clin. Med. 2020;7:4478–4483. [Google Scholar]
- 19.Bundgaard Anker C.C., Rafiq S., Jeppesen P.B. Effect of Steviol Glycosides on Human Health with Emphasis on Type 2 Diabetic Biomarkers: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients. 2019;11:1965. doi: 10.3390/nu11091965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tandel K.R. Sugar substitutes: Health controversy over perceived benefits. J. Pharmacol. Pharmacother. 2011;2:236–243. doi: 10.4103/0976-500X.85936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pang M.D., Goossens G.H., Blaak E.E. The Impact of Artificial Sweeteners on Body Weight Control and Glucose Homeostasis. Front. Nutr. 2021;7:598340. doi: 10.3389/fnut.2020.598340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.US Food and Drug Administration Additional Information about High-Intensity Sweeteners Permitted for Use in Food in the United States. [(accessed on 24 November 2021)];2020 February 20;:3. Available online: https://www.fda.gov/food/food-additives-petitions/additional-information-about-high-intensity-sweeteners-permitted-use-food-united-states.
- 23.World Health Organization . Evaluation of Certain Food Additives—Eighty-Second Report of the Joint FAO/WHO Expert Committee on Food Additives. World Health Organization; Geneva, Switzerland: 2016. [(accessed on 24 November 2021)]. p. 152. Available online: https://apps.who.int/iris/bitstream/handle/10665/250277/9789241210003-eng.pdf?sequence=1&isAllowed=y. [Google Scholar]
- 24.Wells J.C.K., Pomeroy E., Walimbe S.R., Popkin B.M., Yajnik C.S. The Elevated Susceptibility to Diabetes in India: An Evolutionary Perspective. Front. Public Health. 2016;4:145. doi: 10.3389/fpubh.2016.00145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Samuel P., Ayoob K.T., Magnuson B.A., Wölwer-Rieck U., Jeppesen P.B., Rogers P.J., Rowland I., Mathews R. Stevia Leaf to Stevia Sweetener: Exploring Its Science, Benefits, and Future Potential. J. Nutr. 2018;148:1186S–1205S. doi: 10.1093/jn/nxy102. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization . Incentives and Disincentives for Reducing Sugar in Manufactured Foods: An Exploratory Supply Chain Analysis. World Health Organization; Geneva, Switzerland: 2017. [(accessed on 8 November 2021)]. Available online: https://www.euro.who.int/__data/assets/pdf_file/0004/355972/Sugar-report_WHO_107773_updated-and-revised-Dec-2017.pdf. [Google Scholar]
- 27.Food Safety and Standards (Food Products Standards and Food Additives) Regulations. [(accessed on 24 June 2022)];2011 :455. Available online: https://www.fssai.gov.in/upload/uploadfiles/files/Compendium_Food_Additives_Regulations_08_09_2020-compressed.pdf.
- 28.GOV.UK SACN Carbohydrates and Health Report—The Scientific Advisory Committee on Nutrition Recommendations on Carbohydrates, Including Sugars and Fibre. [(accessed on 8 November 2021)];2015 July 17;:2. Available online: https://www.gov.uk/government/publications/sacn-carbohydrates-and-health-report.
- 29.Powell-Wiley T.M., Poirier P., Burke L.E., Després J.-P., Gordon-Larsen P., Lavie C.J., Lear S.A., Ndumele C.E., Neeland I.J., Sanders P., et al. Obesity and Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation. 2021;143:e984–e1010. doi: 10.1161/CIR.0000000000000973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gardner C., Wylie-Rosett J., Gidding S.S., Steffen L.M., Johnson R.K., Reader D., Lichtenstein A.H. Nonnutritive sweeteners: Current use and health perspectives: A scientific statement from the American Heart Association and the American Diabetes Association. Circulation. 2012;126:509–519. doi: 10.1161/CIR.0b013e31825c42ee. [DOI] [PubMed] [Google Scholar]
- 31.Guth E. Healthy weight loss. JAMA. 2014;312:974. doi: 10.1001/jama.2014.10929. [DOI] [PubMed] [Google Scholar]
- 32.Barriocanal L.A., Palacios M., Benitez G., Benitez S., Jimenez J.T., Jimenez N., Rojas V. Apparent lack of pharmacological effect of steviol glycosides used as sweeteners in humans. A pilot study of repeated exposures in some normotensive and hypotensive individuals and in Type 1 and Type 2 diabetics. Regul. Toxicol. Pharmacol. 2008;51:37–41. doi: 10.1016/j.yrtph.2008.02.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.