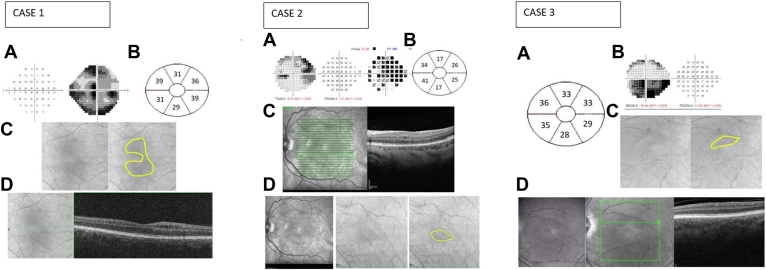
Figure 3.
Case 1. A, Visual field showing central involvement. B, Illustration of Δ ganglion cell layer (GCL) thickness. C, Cirrhus high-definition OCT (HD-OCT) fundoscopic images showing a hypointense circular distribution of the inner nuclear layer cystic change. D, En face Cirrus OCT showing microcystic macular change (case 1). Case 2. A, Visual field showing a superior altitudinal defect. B, Illustration of corresponding ΔGCL (μm) thinning between the affected eye at 6 months and the unaffected eye. C, En face Heidelberg Retina Angiograph (HRA) OCT (Heidelberg Engineering) showing microcystic macular change located in the inferior hemimacula. D, HRA infrared imaging and Cirrhus HD-OCT funduscopic imaging showing an inferior hypointense distribution of the vacuoles. Case 3. A, Illustration of corresponding ΔGCL (μm) thinning between the eye before the event and 6 months postepisode. B, Visual field showing a superior altitudinal defect. C, HD-OCT funduscopy images showing hypointense lesion corresponding to location of microcyst. D, HRA en face OCT (Heidelberg Engineering) showing inner nuclear layer microcysts in the inferior hemimacula. This cystic change develops over time, is longstanding, may be permanent, and corresponds with the ganglion cell complex thinning and visual field loss. For each patient, the distribution of cystic change was confirmed by inspection of the horizontal scans.