Abstract
Sinonasal inverting papilloma is a rare benign, locally aggressive tumour, arising from sinus and/or nasal fossa mucosa, with high recurrence rate, and risk of malignant transformation. This is a case of orbital invasive, lateral extending inverting papilloma approached via combined external and endoscopic surgery.
Keywords: Inverting papilloma, Frontal sinus, Endonasal endoscopic surgery, Sub-brow orbitotomy
Introduction
Inverting papilloma is a rare benign tumour originating from the Schneiderian’s mucosa with a global incidence approximately 4% of all sinonasal epithelial benign neoplasms and typical endofitic growth pattern. Inverting papilloma originating primarily within frontal sinus is quite rare (10%). The gold standard treatment is represented by surgical resection due to the chance of progression to squamous cell carcinoma (9% of cases). The overall recurrence rate, due to non-radical resection, is around 22.4% accordingly with the recent literature [1]. However, treating frontal sinus inverting papilloma may be still challenging, especially when pedicle is implanted on the anterior wall, upper part of the posterior wall, or if extending far lateral in the sinus, with bony remodelling of the orbit roof and/or the posterior wall of the sinus, leading to an intracranial extension.
Case Report
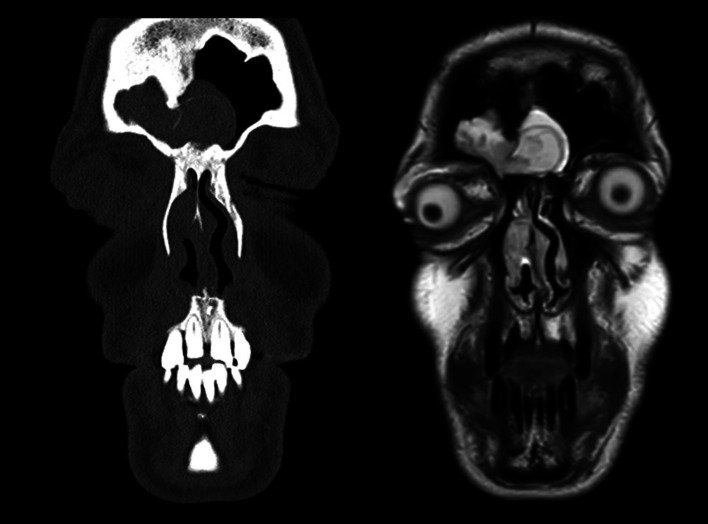
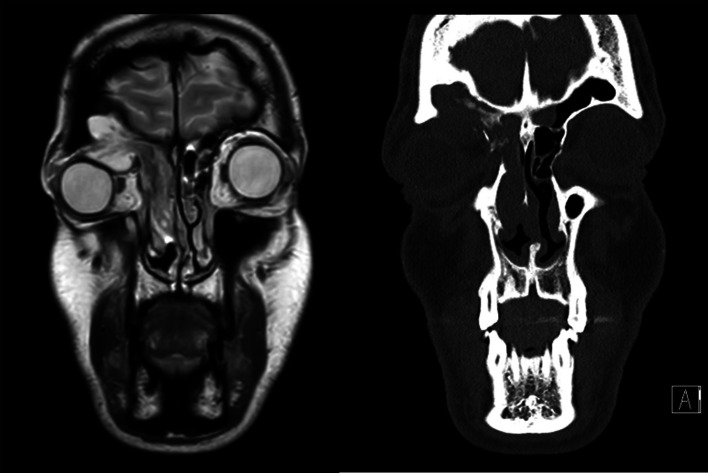
On May 2019, a 42-year-old man presented to the Unit of Maxillo-Facial Surgery of University “Federico II” of Naples with a history of recurrent headache, nasal obstruction, right orbital proptosis, limited ocular movements, and binocular diplopia, arising after a previous surgical operation for IP in right nasal fossa carried out in another hospital. On direct rhinoscopy, a mass occupied the upper nasal fossa, confirmed by the endoscopic view. CT scans highlighted a voluminous mass of mild density, except for higher density in fronto-ethmoidal area, occupying the right frontal sinus completely, partially extended to the contralateral frontal sinus, and descending in right nasal fossa. (Fig. 1) Orbit roof was eroded with a protruding mass in orbital cavity displacing the eye bulb. T2-weighted MRI scans showed a hyper-intense mass with less intense core extending in both the frontal sinuses invading the right orbit. (Fig. 2) An endoscopic incisional biopsy diagnosed a Schneiderian inverting papilloma recurrence. Due to its far lateral extension, the chosen treatment consisted in combined approach via a contemporary sub-brow orbitotomy access and endonasal endoscopic technique. The mass was endoscopically debulked, in order to proceed to inferior turbinectomy and a “Sturmann Canfield” type 2 medial maxillectomy. The frontal recess that appeared fully interested by the IP. Draf III frontal sinusotomy was performed to remove the medial part of the neoplasia occupying both frontal sinuses and to guarantee the drainage. Via a sub-brow orbitotomy access, it was possible to reach the eroded orbit roof with protruding mass from the frontal sinus. (Fig. 3) Under endoscopic view, the remaining tumour was completely removed through the orbitotomy access preserving the periorbit. The bony surfaces were blurred with endoscopic drill and Piezosurgery scalpels. There were no intraoperative complications, eye movements got better as soon as the patient woke up, and he was discharged after 4 days of hospitalization, with the indication for antibiotic and steroid therapy, and nasal washes with saline solution. On December 2019, the patient presented with a massive right periorbital oedema, right proptosis, diplopia. MRI showed a hyper-intense mass in right frontal sinus, leading to mucocele diagnosis due to neo-nasofrontal duct stenosis. The patient underwent a second surgical procedure that completely solved the complication. One year after the second surgical procedure, the patient is free from disease, asymptomatic, and in regular in-office and radiological follow-up.
Fig. 1.
MRI and CT scans showing the frontal intersinus septum distorted and partially reabsorbed by the neoplasm
Fig. 2.
MRI and CT scans showing the extension of the IP that occupyies the right nasal fossa, and invades the right orbit
Fig. 3.
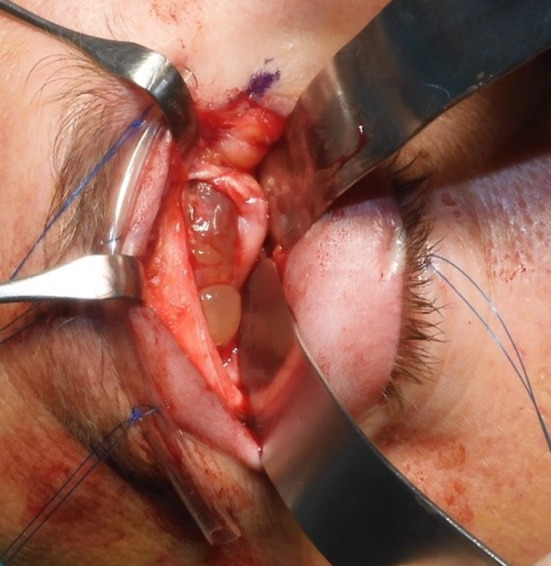
Intraoperative view of the sub-brow orbitotomy access exposing the orbit roof visibly eroded and with protruding mass from the frontal sinus
Discussion
Inverting papilloma originates from the Schneiderian’s mucosa and it is the most common benign epithelial tumour with a global incidence approximately 4%. It has a endofytic pattern of growth, cerebriform aspect at the MRI, local aggressiveness leading to bony erosions and consequent intracranial, orbital or subcutaneous invasion. It usually arises from the lateral wall of nasal cavity, invading, secondarily, the ethmoid and/or the maxillary sinuses. IP originates from frontal sinus in 10% of all cases. The gold standard treatment is surgical resection, due to the chance of progression to squamous cell carcinoma (9% of cases). The overall recurrence rate is 22.4%. [1] CT and MRI are essential to delineate the localization and extension of the tumour, the base of implant characterized by higher density and hyperostosys. MRI helps to distinguish between an IP and a mucous retention, or inflammatory disease. Even if a complete resection of frontal sinus IP is challenging, most of these can be successfully managed via exclusive endoscopic approach. In the past, frontal osteoplastic flap via coronal access was the gold standard to treat these cases [2]. Nowadays, endoscopic surgery together with practical algorithm based on localization, extension, complication, anatomy of the frontal sinuses, and eventual progression to carcinoma of the primary tumour [3], led to an easier approach for sinonasal neoplasms, with less complications and faster recovery. A brand new classification was published for IP involving the frontal sinuses based on its origin and its relationship with the plane of lamina papyracea [4]. Accordingly with this classification, the case proposed by the Author is recognizable as an F5 class (frontal IP with extrasinonasal extension) with extension to the contralateral sinus, small antero-posterior diameter and endo-orbital invasion, suggesting a combined approach, endonasal endoscopic and external, via coronal incision or direct trans-palpebral mini-orbito-frontal craniotomy or sub-brow orbitotomy. [5–8]. After “Sturmann Canfield” type 2 medial maxillectomy, anterior ethmoidectomy, the performed Draf III frontal sinusotomy allowed complete removal of the medial part of the tumour within both sinuses, and created a common drainage duct for both sinuses left patent. Particular attention blurring the underlying bone to eradicate the tumour buried in crevices of the bone, preventing recurrence. Sub-brow orbitotomy access was chosen for the existing orbit roof breach wide enough to guarantee an aggressive and complete approach to the mass, eradicating it completely from the lateral portion of the sinus, as well as the orbit cavity. This access assures aesthetic results, as well as a great exposure of the surgical field. Relative contraindication for this access is any pre-existing eye disease that may get worse. Possible complication of this
access is a retaining scar and palpebral impairment. Stenosis and/or obliteration of the sinus drainage, with consequent retention mucocele, may be a complication in approximately 30% of cases of frontal sinus and frontal recess IP [1, 9]. In our experience, a second surgical treatment, based on scar debridement and drainage duct expansion with balloon sinuplasty, can resolve the retention complications.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations
Conflict of interest
The Authors declare that they have no conflict of interest.
Ethics Approval
No general ethical approval was needed, with only a signed patient consent required by the hospital.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Walgama E, Ahn C, Batra PS. Surgical management of frontal sinus inverted papilloma: a systematic review. Laryngoscope. 2012;122:1205–1209. doi: 10.1002/lary.23275. [DOI] [PubMed] [Google Scholar]
- 2.Shohet J, Duncavage J. Management of the frontal sinus with inverted papilloma. Otolaryngol Head Neck Surg. 1996;114(4):649–52. doi: 10.1016/s0194-5998(96)70263-2. [DOI] [PubMed] [Google Scholar]
- 3.Pietrobon G, Karligkiotis A, Turri-Zanoni M, et al. Surgical management of inverted papilloma involving the frontal sinus: a practical algorithm for treatment planning. Acta Otorhinolaryngol Ital. 2019;39(1):28–39. doi: 10.14639/0392-100X-2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sham CL, van Hasselt CA, Chow SMW, et al. Frontal inverted papillomas: a 25-year study. Laryngoscope. 2020;130:1622–1628. doi: 10.1002/lary.28245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kopelovich JC, Baker MS, Potash A, et al. The hybrid lid crease approach to address lateral frontal sinus disease with orbital extension. Ann Otol Rhinol Laryngol. 2014;123(12):826–30. doi: 10.1177/0003489414538767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Albathi M, Ramanathan M, Lane AP, Boahene KDO. Combined endonasal and eyelid approach for management of extensive frontal sinus inverting papilloma. Laryngoscope. 2018;128:3–9. doi: 10.1002/lary.26552. [DOI] [PubMed] [Google Scholar]
- 7.Makary CA, Limjuco A, Nguyen J, Ramadan HH. Combined lid crease and endoscopic approach to lateral frontal sinus disease with orbital extension. Ann Otol Rhinol Laryngol. 2018;127(9):637–642. doi: 10.1177/0003489418784967. [DOI] [PubMed] [Google Scholar]
- 8.Desjarlais EB, Jovanovic N, Teo HMT, Kahana A. Surgical management of a recurrent orbit-eroding mucocele associated with frontal-ethmoidal sinus inverted papilloma. Ophthalmic Plast Reconstr Surg. 2019;35(6):e136–e138. doi: 10.1097/IOP.0000000000001465. [DOI] [PubMed] [Google Scholar]
- 9.Verillaud B, Le Clerc N, Blancal JP, et al. Mucocele formation after surgical treatment of inverted papilloma of the frontal sinus drainage pathway. Am J Rhinol Allergy. 2016;30(5):181–4. doi: 10.2500/ajra.2016.30.4351. [DOI] [PubMed] [Google Scholar]