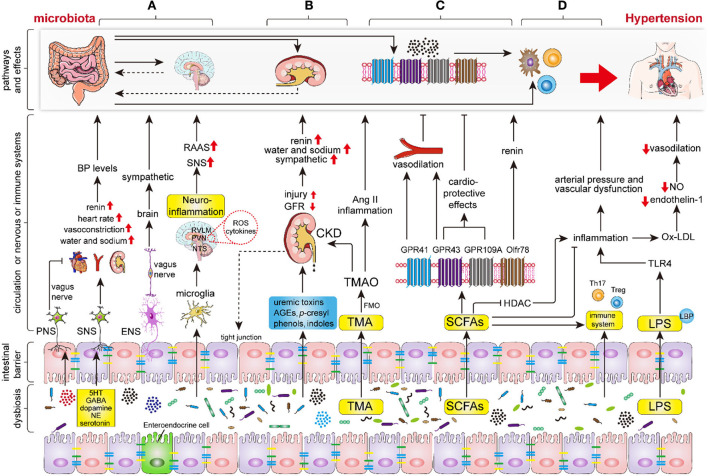
Figure 2.
The key mechanisms of intestinal microbiota in regulating the hypertension process. Intestinal dysbiosis leads to disruption of the nervous system, renal function, intestinal SCFAs, immune system, and increases LPS production and intestinal permeability, thereby aggravating the progression of hypertension. (A) Intestinal microbiota and its metabolites (mainly including GABA, dopamine, noradrenaline and 5HT) regulate hypertension by modifying sympathetic and vagal nerve activity and neuroinflammatory response through the gut-brain axis. (B) Intestinal microbiota and its metabolites regulate hypertension via renal sympathetic regulation, humoral regulation, vasoactive substances (RAAS, nitric oxide, and endothelin), and even lead to hypertension by triggering chronic kidney disease (CKD). (C) The indigestible dietary fiber was fermented into SCFAs, primarily involving acetate, propionate, and butyrate, by intestinal microbiota. Subsequently, the SCFAs regulate hypertension via binding to the specific GPCRs which mainly include GPR43, GPR41, GPR109A, and Olfr78. (D) Intestinal microbiota and endotoxins (LPS) regulate hypertension via the immune and inflammation systems. Abbreviations: BP, blood pressure; PNS, peripheral nervous system; SNS, sympathetic nervous system; ENS, enteric nervous system; RAAS, renin-angiotensin-aldosterone system; GABA, gamma-aminobutyric acid; NE, noradrenaline; 5HT, 5-hydroxytryptamine; ROS, reactive oxygen species; TMA, trimethylamine; TMAO, trimethylamine-N-oxide; FMO, flavin monooxygenases; CKD, chronic kidney disease; SCFAs, short-chain fatty acids; GPR, G protein coupled receptor; HDAC, histone deacetylase; TLR4, Toll-like receptor 4.