Abstract
Introduction
Chronic subdural hematoma (CSDH) is one of the most commonly encountered neurosurgical diseases. Middle meningeal artery embolization (MMAE) is a technique for the management of CSDH that has elicited promising results. Despite the encouraging results of MMAE, recurrence does occur. One uncommon mechanism for recurrence of CSDH is by means of neovascularization of the contralateral middle meningeal artery (MMA). We describe two cases of CSDH recurrence by means of contralateral middle meningeal artery neovascularization treated with contralateral MMAE.
Methods
We identified two cases of recurrent subdural hematoma secondary to neovascularization following treatment with contralateral MMAE.
Results
Two patients initially treated with MMAE were identified with CSDH recurrence secondary to contralateral MMA neovascularization. There was no traumatic or coagulopathic contribution to CSDH recurrence. In both cases, patients underwent contralateral MMAE. Both patients were neurologically intact with radiographic improvement of CSDH at follow up.
Conclusions
Re-accumulation of SDH following MMAE by means of contralateral MMA neovascularization is a rare subtype of subdural hematoma (SDH) recurrence following MMAE. Within the context of re-accumulation of SDH following MMAE, catheter angiography is an important diagnostic investigation to elucidate the etiology of the recurrence. Furthermore, when angiography reveals neovascularization of the contralateral MMA, embolization of the contralateral MMA achieves good clinical and radiographic result.
Keywords: Chronic subdural hematoma, middle meningeal artery embolization, embolization
Introduction
Chronic subdural hematoma (CSDH) is one of the most commonly encountered neurosurgical diseases. The incidence of CSDH has been increasing overtime due to the aging population and increased utilization of antiplatelet and anticoagulation medications. Population wide studies have described an overall incidence of 17.6 to 79.4 per 100,000 persons per year.1,2 The pathophysiology is thought to arise from interruption of the dural cell layer leading to inflammatory cascade and release of angiogenic factors. This leads to the formation of an inflammatory pseudomembrane with fragile neovessels that can lead to accumulation of exudate and blood overtime. 3 Craniotomy or burr hole irrigation is the standard of practice for the surgical management of CSDH, however the recurrence rate is as high as 30%. 4 The middle meningeal artery is one proposed target to reduce the neovascularization involved with CSDH recurrence.
Middle meningeal artery embolization (MMAE) is a technique for the management of CSDH that has elicited promising results. Early studies involving the use of MMAE describe recurrence rates as low as 0–3%.5,6 A large multicenter study examining MMAE reported >50% reduction in over 70% of patient after 90 day follow up. 7 Despite the encouraging results of MMAE, recurrence does occur. One uncommon mechanism for recurrence of CSDH is by means of neovascularization of the contralateral middle meningeal artery (MMA). We describe two cases of CSDH recurrence by means of contralateral middle meningeal artery neovascularization treated with contralateral MMAE.
Methods
Patient selection
We identified two patients with recurrent subdural hematoma secondary to neovascularization following treatment with contralateral MMAE. Data included clinical history, treatment, and review of angiographic images.
MMA embolization technique
Endovascular access was obtained by means of the radial artery. After securing access, guide catheter was placed in the proximal external carotid artery. Microcatheter was advanced into the main trunk of the MMA, where superselective angiography was performed. If the presence of dangerous collateral vessels were identified, the embolization was not performed. Onyx was utilized as the index material for MMAE in all cases. Embolization material was injected into the MMA until flow stasis occurred. Embolization was considered successful when all target MMA branches were embolized.
Illustrative cases
Case 1
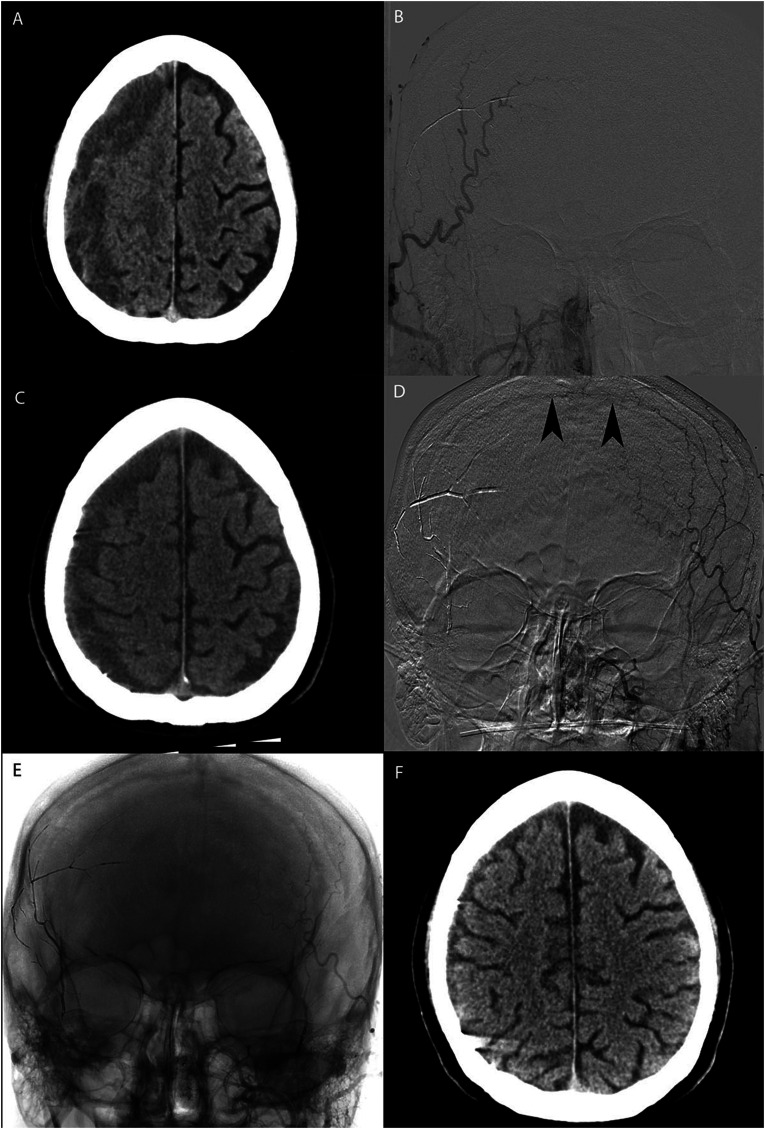
A patient with past medical history of hypertension and remote mechanical ground level fall one month prior presented after having a seizure at home. On examination, no focal neurological deficits were found. Noncontrast computed tomography (CT) of the head revealed a right subacute subdural hematoma (SDH) measuring 2.2 cm with no midline shift (Figure 1A). Right sided subdural evacuation port system (SEPS) was placed and transradial diagnostic cerebral angiography was conducted. Middle meningeal embolization of the right MMA was performed without incident (Figure 2B). The patient had an uncomplicated post-procedure course and was discharged home 6 days after presentation. The patient presented for follow up one week later with repeat noncontrasted CT head revealing decrease in the SDH. The patient presented two weeks after discharge to an outside hospital emergency department with headache. Noncontrasted head CT revealed re-accumulation of R SDH measuring 1.6 cm (Figure 2C). The patient was transferred and transradial diagnostic cerebral angiography was performed, revealing neovasculartization by means of the L MMA (Figure 2D). The MMA was embolized using a combination of coils and particles (Figure 2E). The patient was discharged home the following day. One month later, follow up noncontrasted head CT revealed no re-accumulation of SDH (Figure 2E). The patient denied any symptoms or complaints.
Figure 1.
A: Axial noncontrast CT demonstrates R CSDH. B: AP digital subtraction angiogram, R external carotid artery injection demonstrating no residual filling of the R MMA. C: Axial noncontrast CT demonstrates recurrence of R CSDH. D: AP digital subtraction angiography demonstrating contralateral MMA neovascularization. E: AP native angriogram demonstrating no residual filling of L MMA following coil/particle embolization. F: Follow up axial noncontrast CT demonstrating near resolution of R CSDH.
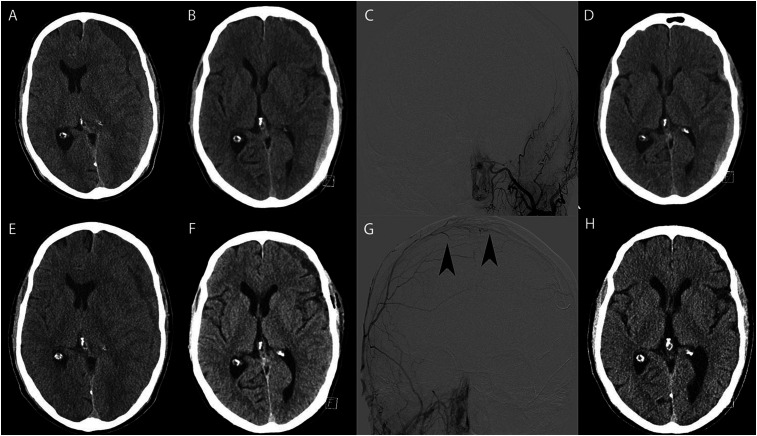
Figure 2.
A: Axial noncontrast CT demonstrates L acute on chronic SDH. B: Axial noncontrast CT demonstrates improvement of mass effect and midline shift following L SEPS placement. C: AP digital subtraction angiogram, L external carotid artery injection demonstrating no residual filling of the R MMA following oxyx embolization. D: Axial noncontrast CT demonstrates stable L acute on chronic SDH at the time of discharge. E: Axial noncontrast CT demonstrates recurrence of L CSDH. F: Axial noncontrast CT demonstrates improvement in mass effect and midline shift following craniotomy for evacuation of CSDH. G: AP digital subtraction angiography demonstrating contralateral MMA neovascularization. H: Follow up axial noncontrast CT demonstrating near resolution of L CSDH.
Case 2
A patient with past medical history of hypertension and mechanical fall three days prior presented with progressive headache and nausea. On examination, the patient was neurologically intact. Noncontrast CT of the head revealed a 2.5 cm subdural hematoma with 1.6 cm of midline shift (Figure 2A). Left sided SEPS was placed (Figure 2B) and transradial MMAE was performed without incident (Figure 2C). The patient was discharged the following day (Figure 2D). The patient presented to the ED two weeks later with gait imbalance and confusion. On examination, no focal neurological deficits were found. Noncontrast CT of the head revealed re-accumulation of the left SDH measuring 1.7 cm with 1.4 cm midline shift (Figure 2E). Left sided craniotomy for subdural evacuation was performed (Figure 2F). On postoperative day one, transradial diagnostic cerebral angiography was performed revealing neovascularization from the R MMA (Figure 2G). Right sided MMAE was performed by means of coils and particles. The patient was discharged on postoperative day four. On follow up visit six weeks later, the subdural was reduced in size (Figure 2H) and the patient was asymptomatic.
Discussion
These two cases demonstrate a rare and previously undescribed mechanism of SDH recurrence following MMAE. In both cases, subdural hematoma re-accumulation was neither due to trauma or coagulopathy. Both patients were found to have neovascularization of the contralateral MMA. Following embolization of the contralateral MMA, both patients achieved radiographic improvement by means of MMAE. Onyx was the embolization agent in the index procedure for both cases, followed by coil/particle embolization. It is unknown which embolization material if superior for MMAE.,8, 9 There are some critical differences in the two cases. In the first case, the subdural was initially treated by means of SEPS, while the second case was treated with traditional craniotomy for subdural evacuation. While some authors report comparable rates of recurrence between both modalities, it is unknown if surgery confers protective benefit in subdural recurrence in the setting of MMAE. 10 Moreover, the first patient achieved improvement of CSDH recurrence by means of contralateral MMAE alone while the second patient underwent craniotomy for evacuation followed by contralateral MMAE. The decision to undergo a second evacuation procedure is multifactorial and depends on patient specific factors including imaging and neurological examination. The cases presented demonstrate good outcome using both modalities.
One of the important limitations of this study is the short follow up interval. While both patients displayed evidence of significantly decreased subdural hematoma size, it is unclear whether this will be a lasting effect following contralateral MMAE. Moreover, some of the patients at our institution are lost to follow up, therefore the number of patients with symptomatic re-accumulation that may be attributed to neovascularization may be underestimated.
Conclusion
Re-accumulation of SDH following MMAE by means of contralateral MMA neovascularization is a rare subtype of SDH recurrence following MMAE. Catheter angiography is an important diagnostic investigation to elucidate the etiology of the recurrence. Furthermore, when angiography reveals neovascularization of the contralateral MMA, embolization of the contralateral MMA achieves good clinical and radiographic result.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
ORCID iD: Zachary S Hubbard https://orcid.org/0000-0002-5643-9480
References
- 1.Feghali J, Yang W, Huang J. Updates in chronic subdural hematoma: epidemiology, etiology, pathogenesis, treatment, and outcome. World Neurosurg 2020 Sep 1; 141: 339–345. [DOI] [PubMed] [Google Scholar]
- 2.Rauhala M, Luoto TM, Huhtala H, et al. The incidence of chronic subdural hematomas from 1990 to 2015 in a defined Finnish population. J Neurosurg 2019 Mar 22; 132: 1147–1157. [DOI] [PubMed] [Google Scholar]
- 3.Edlmann E, Giorgi-Coll S, Whitfield PCet al. et al. Pathophysiology of chronic subdural haematoma: inflammation, angiogenesis and implications for pharmacotherapy. J Neuroinflammation 2017 May 30; 14: 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Santarius T, Kirkpatrick PJ, Ganesan D, et al. Use of drains versus no drains after burr-hole evacuation of chronic subdural haematoma: a randomised controlled trial. Lancet 2009 Sep 26; 374: 1067–1073. [DOI] [PubMed] [Google Scholar]
- 5.Ban SP, Hwang G, Byoun HS, et al. Middle meningeal artery embolization for chronic subdural hematoma. Radiology 2017 Oct 10; 286: 992–999. [DOI] [PubMed] [Google Scholar]
- 6.Kim E. Embolization therapy for refractory hemorrhage in patients with chronic subdural hematomas. World Neurosurg 2017 May 1; 101: 520–527. [DOI] [PubMed] [Google Scholar]
- 7.Kan P, Maragkos GA, Srivatsan A, et al. Middle meningeal artery embolization for chronic subdural hematoma: a multi-center experience of 154 consecutive embolizations. Neurosurgery 2021 Jan 13; 88: 268–277. [DOI] [PubMed] [Google Scholar]
- 8.Medtronic Neurovascular Clinical Affairs. A Study of the Embolization of the Middle Meningeal Artery With ONYXTM Liquid Embolic System In the Treatment of Subacute and Chronic Subdural HEmatoma (EMBOLISE) [Internet]. clinicaltrials.gov; 2021 Mar [cited 2021 Mar 4]. Report No.: NCT04402632. Available from: https://clinicaltrials.gov/ct2/show/NCT04402632 (accessed 30 August 2021).
- 9.Balt USA. The SQUID Trial for the Embolization of the Middle Meningeal Artery for Treatment of Chronic Subdural Hematoma (STEM) [Internet]. clinicaltrials.gov; 2021 Feb [cited 2021 Mar 4]. Report No.: NCT04410146. Available from: https://clinicaltrials.gov/ct2/show/NCT04410146 (accessed 30 August 2021).
- 10.Singla A, Jacobsen WP, Yusupov IRet al. et al. Subdural evacuating port system (SEPS)--minimally invasive approach to the management of chronic/subacute subdural hematomas. Clin Neurol Neurosurg 2013 Apr; 115: 425–431. [DOI] [PubMed] [Google Scholar]