Abstract
The identification of tissue-resident memory T cells (TRM cells) has significantly improved our understanding of immunity. In the last decade, studies have demonstrated that TRM cells are induced after an acute T-cell response, remain in peripheral organs for several years, and contribute to both an efficient host defense and autoimmune disease. TRM cells are found in the kidneys of healthy individuals and patients with various kidney diseases. A better understanding of these cells and their therapeutic targeting might provide new treatment options for infections, autoimmune diseases, graft rejection, and cancer. In this review, we address the definition, phenotype, and developmental mechanisms of TRM cells. Then, we further discuss the current understanding of TRM cells in kidney diseases, such as infection, autoimmune disease, cancer, and graft rejection after transplantation.
Keywords: T cell, Tissue-resident memory T cell, Infection, Autoimmune kidney disease
Introduction
The kidney is a unique non-barrier organ that can be challenged by different types of immune-associated pathologies such as infections, autoimmune diseases, cancer, and graft rejection after kidney transplantation. In these conditions, different types of immune responses are involved that lead to either resolution or progression of the disease. Tissue-resident immunity can be immediately activated on the inflammation site and has important roles in the early phase of immune reactions (1). Adaptive immunity by T cells and B cells contributes to an antigen-specific and efficient immune reaction (2). However, upon the first antigen challenge, adaptive immunity takes longer to be activated as compared with the innate immune system [1, 2]. One major advantage of adaptive immunity is immune memory formation, which enables a swift response upon repeated antigen challenge [1–3]. In the last decade, tissue-resident memory T cells (TRM cells), a new immune cell population, have been characterized as an antigen-specific frontline defense in peripheral organs [4]. TRM cells can, immediately and efficiently, fight specific antigens. Most important, recent findings suggest that TRM cells not only have roles in the host defense but also in unwanted inflammation such as autoimmune disease [4].
General background of TRM cells
The protection of peripheral tissues from invading pathogens and microbes is a central function of the adaptive immune system. Upon challenge, antigens of the pathogens are taken up by dendritic cells (DC) [1]. In response to inflammatory signals, dendritic cells (DC) migrate to secondary lymphoid tissue and present processed antigens via MHC class I or II to CD8+ or CD4+ T cells, respectively. After antigen recognition, T cells become activated, start to proliferate, and differentiate into effector T cells, which migrate to the site of inflammation [1]. Ideally, this response results in the elimination of the non-self-antigen and, ultimately, resolution of the local inflammation. As a consequence, the antigen-specific T-cell population contracts. However, a subset remains as a memory T-cell population, which is responsible for an accelerated response when re-encountering the antigen.
Until recently, memory T cells were divided into two main groups, namely effector memory T cells (TEM cells) and central memory T cells (TCM cells) [3, 5]. TEM cells can enter peripheral tissues from the blood vessels, migrate via lymphatic vessels to secondary lymphoid organs, and eventually re-enter the blood stream [6]. Upon recurring antigen challenge, activated TEM cells are responsible for the accelerated T-cell response at peripheral sites. In contrast, TCM cells are mainly found in the lymphoid tissue and blood. TCM cells have a strong proliferative capacity and are thought to support and replenish TEM cells [3]. However, the concept of memory T cells has dramatically changed by the identification of TRM cells, a memory T-cell population that persists in tissue after resolution of the acute T-cell response.
The identification of TRM cells as a novel memory T-cell population was mainly achieved by innovative technical approaches, namely parabiosis and intravenous labeling. Parabiosis, the surgical connection of the blood circulation of two mice, revealed the exclusion of a population of memory T cells from the circulation and their residency in peripheral tissues for extended time periods [7, 8]. After several weeks of parabiosis, circulating T-cell populations reach an equilibrium. In contrast, a substantial memory T-cell population in peripheral tissues fails to reach this equilibrium and remains in the original tissue [7, 8]. Tissue residency of TRM cells is also observed in tissue transplantation models in which a large population of donor T cells persists in the graft tissue for months [8]. A further novel approach was the development of in vivo labeling techniques for intravascular T cells. After intravenous injection, fluorochrome-conjugated antibodies require several minutes to cross blood vessel endothelia. If antibodies are injected shortly before cell isolation, intravascular cells can be identified by the presence of antibody staining, leaving TRM cells and other extravascular T cells unstained [9, 10]. Together, these approaches allowed the isolation and in-depth characterization of TRM cells in mouse models to be performed and revealed that TRM cells significantly differ in phenotype, gene expression profile, and function from circulating memory T-cell subsets. Based on their characteristic phenotype and mRNA expression profile, TRM cells were subsequently identified in human tissues, including barrier sites and internal organs including the kidney [4, 11, 12]. The identification of donor-derived TRM cells in transplanted human tissues confirmed the long-term tissue residency of these cells and their exclusion from the recipients’ blood circulation [13, 14].
Analysis of TRM cells in the kidney
Analysis of TRM cells is usually based on flow cytometry, which requires harsh isolation procedures of cells from peripheral tissues and often results in the underestimation of TRM cell numbers. In particular, renal TRM cells are more difficult to isolate compared with intravascular T cells. The quantification of renal TRM cells using immunofluorescence microscopy revealed that the numbers were 20 times higher as compared to those determined by the use of flow cytometry-based methods [10].
Under homeostatic conditions, only a small number of memory T cells can be isolated from non-lymphoid tissues of mice. This is mainly because laboratory mice are usually kept under specific pathogen- free conditions, with very limited challenge to their immune system. When freely living feral mice or pet store mice are analyzed, significantly increased numbers of T cells can be isolated from peripheral tissues, including the kidney [15]. The number of T cells in non-lymphoid tissue increases when laboratory mice are co-housed with pet store mice, indicating an important role for the environment. Under homeostatic conditions, a small number of TRM cells can be isolated from the kidney, and a large fraction of these cells are CD8+ TRM cells [9, 16]. The number of TRM cells in mice kidney can be significantly increased using bacterial or viral infection models.
In the human healthy kidney, CD4+ TRM cells are more abundant than CD8+ TRM cells [17, 18]. Compared to barrier organs such as the intestine, the number of TRM cells in healthy kidney is low. Nevertheless, in our experience, more than 10,000 CD4+ TRM cells can be isolated from one gram of healthy human kidney tissue using fluorescence-activated cell sorting (FACS) (unpublished data).
Surface markers of TRM cells in the kidney
There are currently only a few published studies addressing the phenotype of renal TRM cells in humans. This is mainly because of limited access to healthy human tissue. In recent studies, healthy tissue from surgically removed kidneys due to tumor, or tissue from explanted renal allografts after transplant failure, was analyzed [17, 18]. Comparable to TRM cells in other human organs, or in mouse kidneys, healthy human kidneys harbor TRM cells with a similar surface phenotype.
TRM cells are generally identified by the expression of CD69, a membrane-bound, type II C-lectin receptor [9]. CD69 inhibits expression of the sphingosine-1-phosphate receptor 1 (S1PR1), which is required for the egress of T cells from peripheral tissues [19, 20]. Although CD69 was originally described as an early activation marker for T cells, resting TRM cells do not show an activated phenotype [21]. Other common markers for TRM cells are CD103 and CD49a, which are subunits of the integrins αEβ7 and α1β1, respectively. CD103 and CD49a bind to adhesion molecules commonly expressed on epithelial cells, leading to tissue adherence of T cells [22, 23]. CD103 is a marker for CD8+ TRM cells in mucosal tissues and skin [24, 25], but its expression is relatively rare in renal TRM cells [23]. In the kidney, CD49a is a more reliable TRM cell marker, especially for CD8+ T cells [22]. The chemokine receptors CXCR3 and CXCR6 are also frequently expressed on renal TRM cells, which is comparable to findings in other non-lymphoid organs [17, 18, 26, 27]. Moreover, a recent study showed that CD8+ TRM cells downregulate interleukin-18 receptor (IL-18R) during their development in the kidney [28]. Other general phenotypes of TRM cells are S1PR1low, CD44+ (memory T-cell marker), CD62L− (L-selectin, a cell adhesion molecule for homing to lymph tissue), and CCR7− (chemokine receptor for lymphoid tissue recruitment) [29].
Development of TRM cells in the kidney
An accumulation of pathogen-specific renal CD8+ TRM cells was demonstrated in several mouse infection models [10, 30–32]. Most of the used pathogens, e.g., Listeria monocytogenes or lymphocytic choriomeningitis virus (LCMV), infect the kidney, at least transiently. After clearance of the infection, pathogen-specific T cells, together with the phenotype of TRM cells, can be identified in the kidney and persist in the tissue for months. The evidence of tissue residency of these cells was also provided using parabiosis [18, 33].
CD69 expression is crucial to TRM-cell development in the kidney of mice. In CD69-deficient animals, the number of renal TRM cells is significantly decreased [34], and expression of mutant CD69 which cannot interact with S1P1 fails to rescue the poor accumulation of TRM cells in the kidney, suggesting that the interaction of CD69 with S1P1 is required for TRM-cell induction.
TGF-β induces the expression of CD103 during TRM-cell development [30, 35]. Although only a minor subset of renal CD8+ TRM cells is CD103+ [36, 37], the accumulation of renal TRM cells depends on TGF-β. In the absence of TGF-β signaling, T cells show an impaired upregulation of the P- and E-selectin ligands and reduced CXCR3 expression, which results in insufficient recruitment and transendothelial migration of T cells into the kidney [30].
IL-15 was demonstrated to be required for TRM-cell survival in tissues such as skin, lung, liver, salivary gland, and kidney, but it is dispensable for cells in the pancreas, female reproductive tract, and small intestine [38–40].
Transcription profile of TRM cells
In addition to the analyses of surface markers, TRM cells have been extensively characterized for their mRNA expression profile, and core expression signatures have been defined for both mouse and human TRM cells. The signatures define TRM cells as a unique cell population distinct from other T-cell subsets [24, 27, 41]. Furthermore, transcriptional heterogeneity exists within the TRM-cell population, which probably reflects different adaptations to the local environment, or consequences of the type of infection responsible for the formation of these cells [42].
Transcription factors regulating TRM-cell development include Hobit (encoded by the gene Znf683), Blimp-1 (encoded by Prdm1), and Runx3 [36, 43, 44]. The related transcription factors Hobit and Blimp-1 contribute to TRM-cell development in both CD4+ and CD8+ T cells. Hobit represses the expression of Klf2, which is required for tissue egress receptor S1pr1 expression. Both Hobit and Blimp-1 bind to target sequences and suppress the expression of S1PR1, CCR7, and TCF-1, which are important for tissue egress [36]. In response to the interaction with ligands on cells from the environment, the transcription factor NOTCH controls the maintenance of CD8+ TRM cells in peripheral tissue [41]. Furthermore, the transcription factor Bhlhe40 is important to facilitate the metabolic adaptation of TRM cells for the maintenance of mitochondrial fitness [45].
Tissue residency also requires metabolic adaptation to nutrients and oxygen availability in the environment. Although it is unclear how renal TRM cells adapt to the environment, previous studies showed upregulation of the hypoxia-inducible factor pathway in hepatic TRM cells [46]. Given the hypoxic environment in the kidney [47, 48], it is likely that renal TRM cells also upregulate the expression of hypoxia-responsive genes. In addition, an adaptation of the nutrient metabolism is crucial to the maintenance of TRM cells. In CD8+ TRM cells generated by viral infection in the skin, several molecules that mediate lipid uptake are highly expressed. In particular, the fatty acid binding proteins (FABP) 4 and 5 are essential to the exogenous uptake of free fatty acids (FFA), long-term survival, and even to TRM-cell functions [49].
TRM cells in clinical settings
In this part, we will discuss TRM cells in the human and mice kidney by focusing on their clinical relevance.
TRM cells in kidney infection
Infection is the key trigger for TRM-cell induction in many different organs, including the kidney. Upon infection, T cells with cognate T-cell receptor (TCR) are activated and recruited to the infection sites. Some T cells remain in the organ as TRM cells after resolution of the inflammation, working as sentinels that rapidly respond when re-encountering the pathogen. In murine model studies, the presence of TRM cells significantly reduced the pathogen burden and protects mice from lethal challenge infections [50, 51].
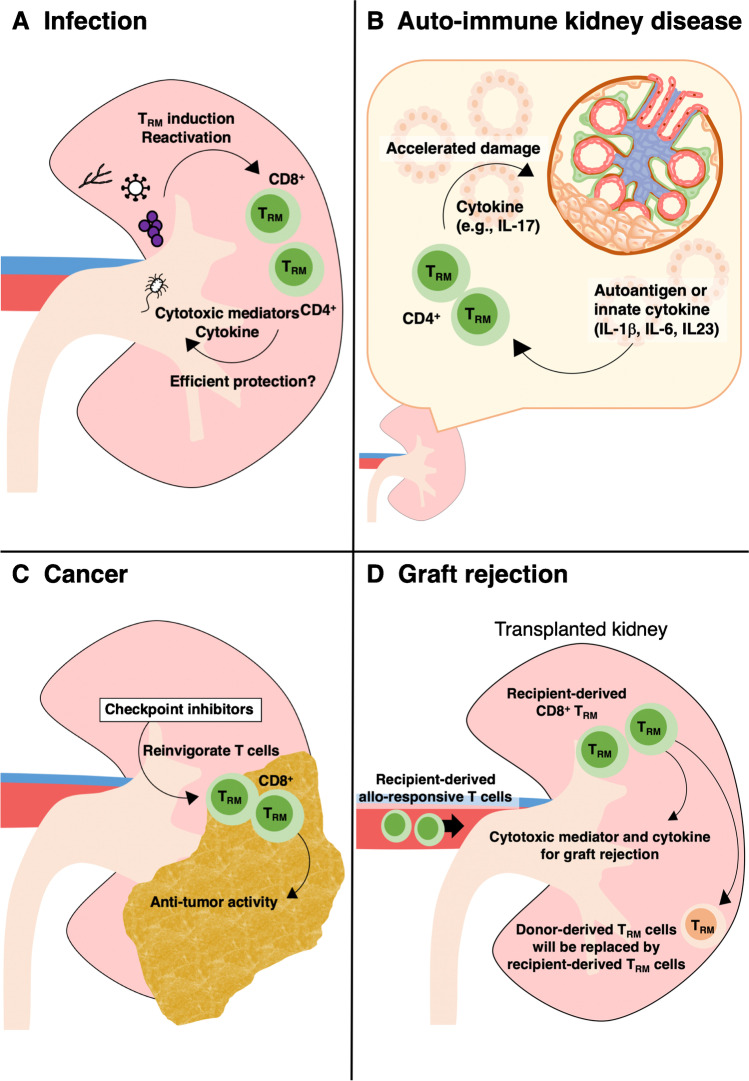
T cells can respond to peptides from pathogens [21]. One of the most common infections in the kidney is bacterial urinary tract infection, affecting young children and adults alike [52–54]. Urinary tract infection is often caused by gut bacteria. Escherichia coli is responsible for more than 80% of urinary tract infections in immunocompetent individuals [52–54]. In mouse studies, pyelonephritis induced by E. coli results in a significant increase in the number of renal TRM cells [18] (Fig. 1A). Other pathogens such as Staphylococcus aureus and Candida albicans are also clinically relevant and cause kidney infection in humans. Murine studies demonstrate that renal TRM cells are induced after infection with these pathogens [18]. TRM cells induced by either bacterial or fungal infection show hallmarks of Th17 cells, including high RORγt expression and IL-17A production upon activation. Although TRM cells can provide protection in a variety of infections [51], it is currently unclear to which extent pathogen-specific TRM cells contribute to the host defense against recurrent renal infections.
Fig. 1.
Role of TRM cells in kidney diseases. A) Infection by pathogens such as bacteria, fungi, and virus, induces CD4+ and/or CD8+ TRM cells in the kidney. They produce cytokines and cytotoxic mediators and are expected to contribute to efficient host defense. B) In autoimmune kidney disease, TRM cells are activated by autoantigen and/or innate cytokines, and aggravate disease by producing inflammatory cytokines. C) In renal cancer such as renal cell carcinoma, CD8+ T cells with TRM phenotype suppress tumor growth. Immune checkpoint inhibitors reinvigorate T cells that have lost anti-tumor activity due to immune-inhibitory signaling. D) After kidney transplantation, donor-derived TRM cells remain in the graft at least for several months. However, in case of graft rejection, recipient-derived TRM cells replace donor-derived TRM cells and damage the kidney by producing cytokines and cytotoxic molecules
Kidneys are also a target of viruses such as cytomegalovirus (CMV) or polyomaviruses. These viruses establish a latent, seemingly asymptomatic infection in immunocompetent individuals. However, in immune-compromised patients, including transplant recipients, the immune surveillance is weakened, causing reactivation of viruses and severe systemic illness. CMV infects various types of cells, occasionally also tubular epithelial cells, endothelial cells, and glomerular epithelial cells [55]. In murine CMV infection models, virus-specific TRM cells are induced in many organs but are found at high frequency in the kidney [56, 57]. Polyomavirus is another clinically relevant virus, establishing latent infection in urothelial and renal tubular epithelial cells in a vast majority of the immunocompetent population [58]. In immunosuppressed renal transplant recipients, however, these viruses are reactivated in up to 60% of patients and cause serious conditions such as polyomavirus BK (PyVBK)-associated interstitial nephritis in 10% of the reactivation cases [58, 59]. Polyomavirus-specific T cells were detected in the peripheral blood of healthy individuals [60], in kidney transplant recipients, and even in kidney allografts [59, 60]. PyVBK-specific CD8+ T cells in allograft kidney tissue expressed CD69 and CD103 in line with a TRM phenotype. In allografts affected by PyVBK-associated interstitial nephritis, virus-specific CD8+ TRM cells were significantly enriched compared with blood [59]. These findings suggest that TRM cells respond and expand after reactivation of the virus, although their activity may not be strong enough to resolve the infection in these patients. It remains unclear how PyVBK-specific TRM cells act after intermittent reactivation in immunocompetent individuals and how they contribute to the control of polyomavirus infection.
TRM cells in autoimmune kidney diseases
The efficient reactive capacity of TRM cells can be important in the development and/or recurrence of autoimmune diseases. Of note, the tissue manifestation of immune-mediated inflammatory diseases, such as psoriasis, often reoccurs in the same location upon relapse. In previous studies, the presence of TRM cells in the psoriatic skin was described, even during remission, indicating that psoriasis remission and relapse are orchestrated by TRM cells [61–63].
The kidney is a common target organ in relapsing and recurrent autoimmune diseases. In kidneys of patients with ANCA vasculitis or lupus nephritis, a significant number of T cells are observed. Here, it is important to note that the number of T cells in the kidney correlates with disease activity, as indicated by increased serum creatinine, proteinuria, and histological score in patients with lupus nephritis, anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis, anti-glomerular basement membrane (GBM) glomerulonephritis [64–66], and as demonstrated in murine lupus models [67]. T cells are found mainly in periglomerular and interstitial regions and less abundantly in intraglomerular regions of the inflamed kidney [64–66]. While CD4+ T cells dominate in number compared with CD8+ T cells in murine glomerulonephritis models, nearly equal numbers of CD4+ and CD8+ T cells in humans [64–66, 68] are reported in many studies.
Most of the renal T cells in inflammatory conditions show a tissue-resident phenotype. CD69 is widely expressed in both CD4+ and CD8+ T cells in the kidney [18, 67, 69]. There are also reports of CD103 expression by CD8+ cells in the kidneys of lupus patients and lupus-prone mice [67]. Moreover, molecules such as CCR7, which are important for the homing to lymphatics organs, were not detected in renal T cells from glomerulonephritis patients [18]. In the recent years, single-cell RNA sequencing (scRNAseq) has advanced our understanding of the cellular landscape of immune cells in the kidney. Especially, scRNAseq technology, combined with epitope measurement using barcoded antibodies [cellular indexing of transcriptomes and epitopes by sequencing (CITE-seq)], allowed single-cell transcriptome analysis with surface molecule expression information to be performed. This is of great importance to the tissue-resident immunity analysis because there can be a significant discrepancy between mRNA expression and protein expression of surface markers such as CD69 [18]. Recently, using combined scRNAseq and CITE-seq methods, we have demonstrated the presence of CD4+ TRM cells in patients with ANCA-associated glomerulonephritis (GN). In these ANCA patients, we found an increased number of TRM cells compared with healthy kidneys. In addition, transcriptome analysis showed that TRM cells from ANCA patients have a higher proliferative capacity than those isolated from healthy kidneys. The scRNAseq analysis revealed heterogeneity in the tissue-resident CD4+ TRM-cell population, showing three clusters with different transcriptomic profiles. Another study of scRNAseq analysis of CD45+ leukocytes from lupus patients’ kidneys also showed the heterogeneity of T-cell populations, with a distinct CD8+ TRM-cell cluster expressing the TRM-associated proteins Hobit and CD103 [70]. Likewise, it is noteworthy that T cells can be found in the urine of patients. Protein expression profiling of cells from lupus patients’ urine revealed the presence of T cells positive for TRM-associated molecules such as CD69 and CD38 [71], which suggests that T cells in the urine originate from TRM cells in the kidney.
In ANCA glomerulonephritis, the number of TRM cells in the kidney biopsy shows a positive correlation with impaired kidney function as indicated by serum creatinine [18]. Currently, it is unclear how autoantigen-specific TRM cells in the kidney are associated with autoimmune kidney disease development and/or relapse in humans. One possibility is that autoantigen-specific TRM cells are more clonally expanded, especially in relapsing patients, but this assumption needs to be verified by TCR specificity and clonality analysis (Fig. 2). Recently, we have shown that TRM cells induced by S. aureus infection aggravates murine crescentic glomerulonephritis [18]. The activation of these TRM cells is probably independent of TCR because they are thought to be mostly bystander TRM cells, which express polyclonal TCR non-specific to the kidney antigen. We demonstrated that the innate inflammatory cytokines IL-1β, IL-6, and IL-23 activate TRM cells, leading to cytokine production [18] (Fig. 1B). Most important, TRM-cell depletion prevented disease aggravation. These findings suggest that pathogenic TRM cells may be a potential target for the treatment of autoimmune kidney diseases. Targeting their specific survival requirements, such as metabolic reliance on free fatty acids or on IL-15, is currently explored to achieve the depletion of TRM cells [42, 72].
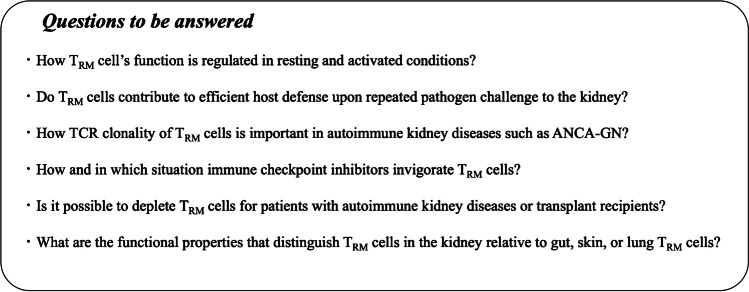
Fig. 2.
Unanswered questions about TRM cells in kidney diseases
Kidney tumors and TRM cells
The kidney is a common cancer site, and different types of cancers can develop. The most common kidney cancer, renal cell carcinoma (RCC), is an immunogenic tumor. Here, increased numbers of T cells are observed in the tumor tissue compared with those found in adjacent healthy tissue [11, 73]. In RCC tumor tissue, CD8+ T cells are more common [74]. Similar to renal T cells in other diseases, the majority of T cells detected in the tumor show a tissue-resident phenotype with CD69 expression in both CD4+ and CD8+ T cells [75], and CD103 expression mainly in CD8+ T cells [11, 76]. In a mouse renal adenocarcinoma model, most of the CD69+ T cells are protected from intravascular staining, supporting the assumption that these T cells are tissue resident.
While a high number of tumor-infiltrating T cells are usually associated with a better prognosis in many tumor types [77], the abundance of intratumoral T cells might be associated with a high tumor grade and shorter patient survival in clear cell RCC (ccRCC) [78]. However, the number of CD103+ T cells was reported to be an independent favorable prognostic factor in RCC patients [79]. Furthermore, in a mouse RCC model, CD103+-cell depletion resulted in accelerated tumor growth [79]. CD103+ T cells are able to respond to TCR reactivation by upregulating cytotoxic mediators and proliferation, suggesting that CD103+ CD8+ T cells can rapidly reactivate their effector functions [79]. Therefore, CD103+ TRM-like cells in tumors substantially contribute to immune surveillance. Their potential of immediate anti-tumor responses makes tumor-infiltrating TRM cells an attractive target for therapeutic interventions (Fig. 1C).
The regulation of intratumoral T cells is of great importance to their anti-tumor response. T-cell functionality can be regulated by immune checkpoint proteins such as PD1 and CTLA-4. T cells regulated by inhibitory molecules are unable to proliferate, or to produce cytokine or cytotoxic molecules in response to antigen recognition. The inhibitory protein PD1 was detected on tumor-infiltrating CD103+ T cells in RCC, suggesting that their anti-tumor function is actively suppressed and that these tumor-infiltrating T cells can be targeted by checkpoint inhibitors [80]. It is reported that a high proliferation rate of tumor-infiltrating CD8+ T cells is associated with prolonged survival of RCC patients. Furthermore, a murine study demonstrated the inefficacy of checkpoint inhibitors after depletion of CD103+ cells in a RCC model [79].
Immune checkpoint inhibitors have revolutionized cancer treatment. Clinical trials have provided evidence of a superior survival rate of metastatic RCC patients treated with immune checkpoint inhibitors. Therefore, immune checkpoint inhibition has become a standard of care for advanced RCC [73, 81]. Immune checkpoint inhibition therapy is thought to reinvigorate tumor-infiltrating T cells that have lost their anti-tumor activity due to immune-inhibitory signaling. However, it remains to be investigated how TRM cells in kidney tumors suppress tumor growth. In melanoma models, it is reported that the anti-tumor effect is due to the direct killing of tumor cells, in addition to the activation and recruitment of other immune cells by cytokine production [82, 83].
While many patients benefit from immune checkpoint inhibition therapy, some do not respond to it. Therefore, reliable markers are needed to predict the therapeutic response and to ensure that individuals with a good chance of response receive treatment. Expression of PDL1, a ligand for PD1, has been investigated as a marker of response. However, a clinical response to PD1 inhibition was observed even in patients with low or no PDL1 expression (73, 84). Genetic analysis as a useful predictive tool, such as tumor mutation profiling, was also reported. Accumulating mutations in tumors lead to the formation of increased neoantigens, stimulating immune responses. An analysis of five clinical trials revealed that patients with different tumors such as RCC, with microsatellite instability or deficient mismatch repair, showed a higher response to pembrolizumab, a humanized antibody targeting PD1 [85]. By contrast, another study showed that tumor mutations and neoantigen expression were not associated with progression-free survival of patients treated with anti-PD-L1 [86]. Therefore, further studies addressing the question of how tumor-infiltrating T cells are regulated need to be performed.
In addition to immune checkpoint inhibitors, another innovative approach, namely therapeutic cancer vaccination, has been developed and is being tested. It is reported that the induction of TRM cells enhances the efficacy of cancer vaccines [87]. These vaccines are evolving by the development of next-generation sequencing, which makes it possible to reveal mutations present in tumor cells. By using tumor neoantigens produced by the mutations, cancer vaccines induce T-cell responses specific to cancer cells. First clinical trials showed a robust tumor-specific immunogenicity in patients with melanoma and other cancers. This therapeutic strategy is currently being tested in combination with immune checkpoint inhibitors in a clinical trial for RCC [88].
Kidney transplantation and TRM cells
Kidney transplantation is an important treatment for patients with end-stage renal diseases. Although the transplantation outcome was significantly improved by the development of immunosuppressants, the rejection of transplanted kidneys remains a serious problem. The graft rejection is caused by T cells. Kidney allografts contain donor-derived T cells, most of which express tissue residency-associated markers such as CD69 and CD103. In the case of HLA-mismatched transplantation, donor- and recipient-derived T cells can be distinguished by HLA staining, making it possible to track T-cell chimerism in the transplanted organs. In lung transplantation, donor-derived TRM cells persist in the organ and express signature markers including CD69, CD103, and CD49a, but the number of donor-derived T cells in the blood becomes negligible at two months following transplantation. Of particular note, recipients with an increased number of donor-derived lung TRM cells have fewer adverse events such as primary graft dysfunction, or acute cellular rejection, compared with recipients with lower donor TRM-cell persistence. In kidney transplantation, it is still unclear how long donor-derived cells persist in the graft. A study analyzed transplanted kidneys from patients with graft failure and reported that donor-derived TRM cells were not detected in organs that failed > 5 months after transplantation. This suggests that recipient-derived T cells are recruited to the transplanted kidney, become TRM cells, and replace donor-derived TRM cells when graft failure occurs [12] (Fig. 1D).
Recipient-derived T cells play an important role in the rejection of a transplanted kidney. Both CD4+ and CD8+-recipient T cells are found in the graft. Based on the expression of cytotoxic molecules such as granzymes A and B, the tissue injury mechanism in T cell-mediated rejection was once thought to be direct cell damage to donor cells. However, tubulitis after allogenic transplantation was observed even in mice deficient in perforin or in the granzymes A and B [89]. Furthermore, a recent study showed that TRM cells in kidney allografts did not express higher amounts of granzyme B, or perforin, compared with circulating cells [12, 17]. Therefore, T cell-mediated rejection is considered to take place through cytotoxic and non-cytotoxic functions [90].
Allo-responsive T cells in recipients can be identified by the detection of cytokine production after stimulation with donor-derived cells. An increased frequency of allo-specific T cells in the peripheral blood of recipients prior to or during the first six months after renal transplantation was associated with an increased risk of acute rejection and inferior graft function [91, 92]. In a mouse model of kidney transplantation, graft rejection was observed only when kidney antigen-specific CD8+ T cells were transferred to recipient mice. After transplantation, both kidney antigen-specific and polyclonal T cells were recruited to the graft and differentiated into TRM cells. TRM cells proliferated locally and produced IFN-γ upon re-stimulation with allogenic donor splenocytes (93). Therefore, in kidney transplant rejection, allo-specific T cells in recipients are recruited to the graft, develop into TRM cells, and damage the kidney via production of cytokine and cytotoxic molecules. During this rejection process, host-derived TRM cells are replaced by recipient TRM cells.
Conclusions
The discovery of TRM cells has significantly advanced our understanding of immunity. Because of their tissue-residing and memory phenotypes, they can respond quickly and efficiently to invading pathogens in the affected organs. The efficient induction of TRM cells in barrier organs would be an attractive strategy for vaccine-mediated immunization against pathogens. Yet, the presence of TRM cells might cause adverse events such as autoimmune disease development and relapse, which makes the induction of TRM cells a double-edged sword. Therefore, it will be important to address the question of how TRM-cell activity is regulated and can be targeted for treatment. (Unanswered questions are listed in Fig. 2.)
Funding
Open Access funding enabled and organized by Projekt DEAL.
Declarations
Conflict of interest
The authors declare that they have no competing interests.
Footnotes
This article is a contribution to the special issue on: Heterogeneity of tissue-resident immunity across organs and in health and disease - Guest Editors: Federica Sallusto & Petra Arck
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Nariaki Asada and Pauline Ginsberg contributed equally to this work.
References
- 1.Iwasaki A, Medzhitov R. Control of adaptive immunity by the innate immune system. Nat Immunol. 2015;16:343–353. doi: 10.1038/ni.3123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Netea MG, Domínguez-Andrés J, Barreiro LB, Chavakis T, Divangahi M, Fuchs E, Joosten LAB, van der Meer JWM, Mhlanga MM, Mulder WJM, Riksen NP, Schlitzer A, Schultze JL, Stabell Benn C, Sun JC, Xavier RJ, Latz E. Defining trained immunity and its role in health and disease. Nat Rev Immunol. 2020;20:375–388. doi: 10.1038/s41577-020-0285-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sallusto F, Geginat J, Lanzavecchia A. Central memory and effector memory T cell subsets: function, generation, and maintenance. Annu Rev Immunol. 2004;22:745–763. doi: 10.1146/annurev.immunol.22.012703.104702. [DOI] [PubMed] [Google Scholar]
- 4.Park CO, Kupper TS. The emerging role of resident memory T cells in protective immunity and inflammatory disease. Nat Med. 2015;21:688–697. doi: 10.1038/nm.3883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sallusto F, Lenig D, Förster R, Lipp M, Lanzavecchia A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature. 1999;401:708–712. doi: 10.1038/44385. [DOI] [PubMed] [Google Scholar]
- 6.Schenkel JM, Masopust D. Tissue-resident memory T cells. Immunity. 2014;41:886–897. doi: 10.1016/j.immuni.2014.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gebhardt T, Wakim LM, Eidsmo L, Reading PC, Heath WR, Carbone FR. Memory T cells in nonlymphoid tissue that provide enhanced local immunity during infection with herpes simplex virus. Nat Immunol. 2009;10:524–530. doi: 10.1038/ni.1718. [DOI] [PubMed] [Google Scholar]
- 8.Masopust D, Choo D, Vezys V, Wherry EJ, Duraiswamy J, Akondy R, Wang J, Casey KA, Barber DL, Kawamura KS, Fraser KA, Webby RJ, Brinkmann V, Butcher EC, Newell KA, Ahmed R. Dynamic T cell migration program provides resident memory within intestinal epithelium. J Exp Med. 2010;207:553–564. doi: 10.1084/jem.20090858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson KG, Mayer-Barber K, Sung H, Beura L, James BR, Taylor JJ, Qunaj L, Griffith TS, Vezys V, Barber DL, Masopust D. Intravascular staining for discrimination of vascular and tissue leukocytes. Nat Protoc. 2014;9:209–222. doi: 10.1038/nprot.2014.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steinert EM, Schenkel JM, Fraser KA, Beura LK, Manlove LS, Igyártó BZ, Southern PJ, Masopust D. Quantifying Memory CD8 T Cells Reveals Regionalization of Immunosurveillance. Cell. 2015;161:737–749. doi: 10.1016/j.cell.2015.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dornieden T, Sattler A, Pascual Reguant A, Ruhm A, Thiel L, Bergmann Y, Thole L, Kohler R, Kuhl A, Hauser A, Boral S, Friedersdorff F, Kotsch K. 2021. Signatures and Specificity of Tissue-resident Lymphocytes Identified in Human Renal Peri-tumor and Tumor Tissue. J Am Soc Nephrol [DOI] [PMC free article] [PubMed]
- 12.de Leur K, Dieterich M, Hesselink DA, Corneth OBJ, Dor F, de Graav GN, Peeters AMA, Mulder A, Kimenai H, Claas FHJ, Clahsen-van Groningen MC, van der Laan LJW, Hendriks RW, Baan CC. Characterization of donor and recipient CD8+ tissue-resident memory T cells in transplant nephrectomies. Sci Rep. 2019;9:5984. doi: 10.1038/s41598-019-42401-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bartolomé-Casado R, Landsverk OJB, Chauhan SK, Richter L, Phung D, Greiff V, Risnes LF, Yao Y, Neumann RS, Yaqub S, Øyen O, Horneland R, Aandahl EM, Paulsen V, Sollid LM, Qiao SW, Baekkevold ES, Jahnsen FL. Resident memory CD8 T cells persist for years in human small intestine. J Exp Med. 2019;216:2412–2426. doi: 10.1084/jem.20190414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Snyder ME, Finlayson MO, Connors TJ, Dogra P, Senda T, Bush E, Carpenter D, Marboe C, Benvenuto L, Shah L, Robbins H, Hook JL, Sykes M, D'Ovidio F, Bacchetta M, Sonett JR, Lederer DJ, Arcasoy S, Sims PA, Farber DL. 2019. Generation and persistence of human tissue-resident memory T cells in lung transplantation. Sci Immunol 4 [DOI] [PMC free article] [PubMed]
- 15.Beura LK, Hamilton SE, Bi K, Schenkel JM, Odumade OA, Casey KA, Thompson EA, Fraser KA, Rosato PC, Filali-Mouhim A, Sekaly RP, Jenkins MK, Vezys V, Haining WN, Jameson SC, Masopust D. Normalizing the environment recapitulates adult human immune traits in laboratory mice. Nature. 2016;532:512–516. doi: 10.1038/nature17655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Turner JE, Becker M, Mittrucker HW, Panzer U. Tissue-Resident Lymphocytes in the Kidney. J Am Soc Nephrol. 2018;29:389–399. doi: 10.1681/ASN.2017060599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van der Putten C, Remmerswaal EBM, Terpstra ML, van der Bom ND, Kers J, Ten Berge IJM, Geerlings SE, van Lier RAW, Bemelman FJ, van Aalderen MC. 2021. CD8 and CD4 T Cell Populations in Human Kidneys. Cells 10 [DOI] [PMC free article] [PubMed]
- 18.Krebs CF, Reimers D, Zhao Y, Paust HJ, Bartsch P, Nunez S, Rosemblatt MV, Hellmig M, Kilian C, Borchers A, Enk LUB, Zinke M, Becker M, Schmid J, Klinge S, Wong MN, Puelles VG, Schmidt C, Bertram T, Stumpf N, Hoxha E, Meyer-Schwesinger C, Lindenmeyer MT, Cohen CD, Rink M, Kurts C, Franzenburg S, Koch-Nolte F, Turner JE, Riedel JH, Huber S, Gagliani N, Huber TB, Wiech T, Rohde H, Bono MR, Bonn S, Panzer U, Mittrucker HW. 2020. Pathogen-induced tissue-resident memory TH17 (TRM17) cells amplify autoimmune kidney disease. Sci Immunol 5 [DOI] [PubMed]
- 19.Mackay LK, Braun A, Macleod BL, Collins N, Tebartz C, Bedoui S, Carbone FR, Gebhardt T. Cutting edge: CD69 interference with sphingosine-1-phosphate receptor function regulates peripheral T cell retention. J Immunol. 2015;194:2059–2063. doi: 10.4049/jimmunol.1402256. [DOI] [PubMed] [Google Scholar]
- 20.Shiow LR, Rosen DB, Brdicková N, Xu Y, An J, Lanier LL, Cyster JG, Matloubian M. CD69 acts downstream of interferon-alpha/beta to inhibit S1P1 and lymphocyte egress from lymphoid organs. Nature. 2006;440:540–544. doi: 10.1038/nature04606. [DOI] [PubMed] [Google Scholar]
- 21.Hegazy AN, West NR, Stubbington MJT, Wendt E, Suijker KIM, Datsi A, This S, Danne C, Campion S, Duncan SH, Owens BMJ, Uhlig HH, McMichael A, Bergthaler A, Teichmann SA, Keshav S, Powrie F. Circulating and Tissue-Resident CD4(+) T Cells With Reactivity to Intestinal Microbiota Are Abundant in Healthy Individuals and Function Is Altered During Inflammation. Gastroenterology. 2017;153:1320–37.e16. doi: 10.1053/j.gastro.2017.07.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park JG, Na M, Kim MG, Park SH, Lee HJ, Kim DK, Kwak C, Kim YS, Chang S, Moon KC, Lee DS, Han SS. Immune cell composition in normal human kidneys. Sci Rep. 2020;10:15678. doi: 10.1038/s41598-020-72821-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Szabo PA, Miron M, Farber DL. 2019. Location, location, location: Tissue resident memory T cells in mice and humans. Sci Immunol 4 [DOI] [PMC free article] [PubMed]
- 24.Mackay LK, Rahimpour A, Ma JZ, Collins N, Stock AT, Hafon ML, Vega-Ramos J, Lauzurica P, Mueller SN, Stefanovic T, Tscharke DC, Heath WR, Inouye M, Carbone FR, Gebhardt T. The developmental pathway for CD103(+)CD8+ tissue-resident memory T cells of skin. Nat Immunol. 2013;14:1294–1301. doi: 10.1038/ni.2744. [DOI] [PubMed] [Google Scholar]
- 25.Zhang N, Bevan MJ. Transforming growth factor-β signaling controls the formation and maintenance of gut-resident memory T cells by regulating migration and retention. Immunity. 2013;39:687–696. doi: 10.1016/j.immuni.2013.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kunkel EJ, Boisvert J, Murphy K, Vierra MA, Genovese MC, Wardlaw AJ, Greenberg HB, Hodge MR, Wu L, Butcher EC, Campbell JJ. Expression of the chemokine receptors CCR4, CCR5, and CXCR3 by human tissue-infiltrating lymphocytes. Am J Pathol. 2002;160:347–355. doi: 10.1016/S0002-9440(10)64378-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kumar BV, Ma W, Miron M, Granot T, Guyer RS, Carpenter DJ, Senda T, Sun X, Ho SH, Lerner H, Friedman AL, Shen Y, Farber DL. Human Tissue-Resident Memory T Cells Are Defined by Core Transcriptional and Functional Signatures in Lymphoid and Mucosal Sites. Cell Rep. 2017;20:2921–2934. doi: 10.1016/j.celrep.2017.08.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liao W, Liu Y, Ma C, Wang L, Li G, Mishra S, Srinivasan S, Fan KK, Wu H, Li Q, Zhao M, Liu X, Demel EL, Zhang X, Qiu Y, Lu Q, Zhang N. 2021. The downregulation of IL-18R defines bona fide kidney-resident CD8(+) T cells. iScience 24: 101975 [DOI] [PMC free article] [PubMed]
- 29.Mueller SN, Mackay LK. Tissue-resident memory T cells: local specialists in immune defence. Nat Rev Immunol. 2016;16:79–89. doi: 10.1038/nri.2015.3. [DOI] [PubMed] [Google Scholar]
- 30.Ma C, Mishra S, Demel EL, Liu Y, Zhang N. TGF-β Controls the Formation of Kidney-Resident T Cells via Promoting Effector T Cell Extravasation. J Immunol. 2017;198:749–756. doi: 10.4049/jimmunol.1601500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beura LK, Anderson KG, Schenkel JM, Locquiao JJ, Fraser KA, Vezys V, Pepper M, Masopust D. Lymphocytic choriomeningitis virus persistence promotes effector-like memory differentiation and enhances mucosal T cell distribution. J Leukoc Biol. 2015;97:217–225. doi: 10.1189/jlb.1HI0314-154R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frost EL, Kersh AE, Evavold BD, Lukacher AE. Cutting Edge: Resident Memory CD8 T Cells Express High-Affinity TCRs. J Immunol. 2015;195:3520–3524. doi: 10.4049/jimmunol.1501521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Skon CN, Lee JY, Anderson KG, Masopust D, Hogquist KA, Jameson SC. Transcriptional downregulation of S1pr1 is required for the establishment of resident memory CD8+ T cells. Nat Immunol. 2013;14:1285–1293. doi: 10.1038/ni.2745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Walsh DA, Borges da Silva H, Beura LK, Peng C, Hamilton SE, Masopust D, Jameson SC. The Functional Requirement for CD69 in Establishment of Resident Memory CD8<sup>+</sup> T Cells Varies with Tissue Location. J Immunol. 2019;203:946–955. doi: 10.4049/jimmunol.1900052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mani V, Bromley SK, Äijö T, Mora-Buch R, Carrizosa E, Warner RD, Hamze M, Sen DR, Chasse AY, Lorant A, Griffith JW, Rahimi RA, McEntee CP, Jeffrey KL, Marangoni F, Travis MA, Lacy-Hulbert A, Luster AD, Mempel TR. 2019. Migratory DCs activate TGF-β to precondition naïve CD8(+) T cells for tissue-resident memory fate. Science 366 [DOI] [PMC free article] [PubMed]
- 36.Mackay LK, Minnich M, Kragten NA, Liao Y, Nota B, Seillet C, Zaid A, Man K, Preston S, Freestone D, Braun A, Wynne-Jones E, Behr FM, Stark R, Pellicci DG, Godfrey DI, Belz GT, Pellegrini M, Gebhardt T, Busslinger M, Shi W, Carbone FR, van Lier RA, Kallies A, van Gisbergen KP. Hobit and Blimp1 instruct a universal transcriptional program of tissue residency in lymphocytes. Science. 2016;352:459–463. doi: 10.1126/science.aad2035. [DOI] [PubMed] [Google Scholar]
- 37.Casey KA, Fraser KA, Schenkel JM, Moran A, Abt MC, Beura LK, Lucas PJ, Artis D, Wherry EJ, Hogquist K, Vezys V, Masopust D. Antigen-independent differentiation and maintenance of effector-like resident memory T cells in tissues. J Immunol. 2012;188:4866–4875. doi: 10.4049/jimmunol.1200402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schenkel JM, Fraser KA, Casey KA, Beura LK, Pauken KE, Vezys V, Masopust D. IL-15-Independent Maintenance of Tissue-Resident and Boosted Effector Memory CD8 T Cells. J Immunol. 2016;196:3920–3926. doi: 10.4049/jimmunol.1502337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mackay LK, Wynne-Jones E, Freestone D, Pellicci DG, Mielke LA, Newman DM, Braun A, Masson F, Kallies A, Belz GT, Carbone FR. T-box Transcription Factors Combine with the Cytokines TGF-β and IL-15 to Control Tissue-Resident Memory T Cell Fate. Immunity. 2015;43:1101–1111. doi: 10.1016/j.immuni.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 40.Holz LE, Prier JE, Freestone D, Steiner TM, English K, Johnson DN, Mollard V, Cozijnsen A, Davey GM, Godfrey DI, Yui K, Mackay LK, Lahoud MH, Caminschi I, McFadden GI, Bertolino P, Fernandez-Ruiz D, Heath WR. CD8(+) T Cell Activation Leads to Constitutive Formation of Liver Tissue-Resident Memory T Cells that Seed a Large and Flexible Niche in the Liver. Cell Rep. 2018;25:68–79.e4. doi: 10.1016/j.celrep.2018.08.094. [DOI] [PubMed] [Google Scholar]
- 41.Hombrink P, Helbig C, Backer RA, Piet B, Oja AE, Stark R, Brasser G, Jongejan A, Jonkers RE, Nota B, Basak O, Clevers HC, Moerland PD, Amsen D, van Lier RA. Programs for the persistence, vigilance and control of human CD8(+) lung-resident memory T cells. Nat Immunol. 2016;17:1467–1478. doi: 10.1038/ni.3589. [DOI] [PubMed] [Google Scholar]
- 42.van der Gracht ETI, Behr FM, Arens R. 2021. Functional Heterogeneity and Therapeutic Targeting of Tissue-Resident Memory T Cells. Cells 10 [DOI] [PMC free article] [PubMed]
- 43.Milner JJ, Toma C, Yu B, Zhang K, Omilusik K, Phan AT, Wang D, Getzler AJ, Nguyen T, Crotty S, Wang W, Pipkin ME, Goldrath AW. Runx3 programs CD8(+) T cell residency in non-lymphoid tissues and tumours. Nature. 2017;552:253–257. doi: 10.1038/nature24993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Behr FM, Chuwonpad A, Stark R, van Gisbergen K. Armed and Ready: Transcriptional Regulation of Tissue-Resident Memory CD8 T Cells. Front Immunol. 2018;9:1770. doi: 10.3389/fimmu.2018.01770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li C, Zhu B, Son YM, Wang Z, Jiang L, Xiang M, Ye Z, Beckermann KE, Wu Y, Jenkins JW, Siska PJ, Vincent BG, Prakash YS, Peikert T, Edelson BT, Taneja R, Kaplan MH, Rathmell JC, Dong H, Hitosugi T, Sun J. The Transcription Factor Bhlhe40 Programs Mitochondrial Regulation of Resident CD8(+) T Cell Fitness and Functionality. Immunity. 2019;51:491–507.e7. doi: 10.1016/j.immuni.2019.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim JH, Han JW, Choi YJ, Rha MS, Koh JY, Kim KH, Kim CG, Lee YJ, Kim AR, Park J, Kim HK, Min BS, Seo SI, Kang M, Park HJ, Han DH, Kim SI, Kim MS, Lee JG, Lee DH, Kim W, Park JY, Park SH, Joo DJ, Shin EC. Functions of human liver CD69(+)CD103(-)CD8(+) T cells depend on HIF-2α activity in healthy and pathologic livers. J Hepatol. 2020;72:1170–1181. doi: 10.1016/j.jhep.2020.01.010. [DOI] [PubMed] [Google Scholar]
- 47.Schödel J, Ratcliffe PJ. Mechanisms of hypoxia signalling: new implications for nephrology. Nat Rev Nephrol. 2019;15:641–659. doi: 10.1038/s41581-019-0182-z. [DOI] [PubMed] [Google Scholar]
- 48.Asada N. Tubular immaturity causes erythropoietin-deficiency anemia of prematurity in preterm neonates. Sci Rep. 2018;8:4448. doi: 10.1038/s41598-018-22791-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pan Y, Tian T, Park CO, Lofftus SY, Mei S, Liu X, Luo C, O'Malley JT, Gehad A, Teague JE, Divito SJ, Fuhlbrigge R, Puigserver P, Krueger JG, Hotamisligil GS, Clark RA, Kupper TS. Survival of tissue-resident memory T cells requires exogenous lipid uptake and metabolism. Nature. 2017;543:252–256. doi: 10.1038/nature21379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Park SL, Zaid A, Hor JL, Christo SN, Prier JE, Davies B, Alexandre YO, Gregory JL, Russell TA, Gebhardt T, Carbone FR, Tscharke DC, Heath WR, Mueller SN, Mackay LK. Local proliferation maintains a stable pool of tissue-resident memory T cells after antiviral recall responses. Nat Immunol. 2018;19:183–191. doi: 10.1038/s41590-017-0027-5. [DOI] [PubMed] [Google Scholar]
- 51.Teijaro JR, Turner D, Pham Q, Wherry EJ, Lefrançois L, Farber DL. Cutting edge: Tissue-retentive lung memory CD4 T cells mediate optimal protection to respiratory virus infection. J Immunol. 2011;187:5510–5514. doi: 10.4049/jimmunol.1102243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol. 2010;7:653–660. doi: 10.1038/nrurol.2010.190. [DOI] [PubMed] [Google Scholar]
- 53.Roberts KB. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011;128:595–610. doi: 10.1542/peds.2011-1330. [DOI] [PubMed] [Google Scholar]
- 54.Ohnishi T, Asada N, Furuichi M, Sekiguchi S, Awazu M, Hori N, Kamimaki I. A novel screening method for pediatric urinary tract infection using ordinary diapers. Sci Rep. 2020;10:19342. doi: 10.1038/s41598-020-76405-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fogo AB, Lusco MA, Najafian B, Alpers CE. AJKD Atlas of Renal Pathology: Cytomegalovirus Infection. Am J Kidney Dis. 2016;68:e35–e36. doi: 10.1053/j.ajkd.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 56.Smith CJ, Caldeira-Dantas S, Turula H, Snyder CM. Murine CMV Infection Induces the Continuous Production of Mucosal Resident T Cells. Cell Rep. 2015;13:1137–1148. doi: 10.1016/j.celrep.2015.09.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Beura LK, Fares-Frederickson NJ, Steinert EM, Scott MC, Thompson EA, Fraser KA, Schenkel JM, Vezys V, Masopust D. CD4(+) resident memory T cells dominate immunosurveillance and orchestrate local recall responses. J Exp Med. 2019;216:1214–1229. doi: 10.1084/jem.20181365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.van Aalderen MC, Heutinck KM, Huisman C, ten Berge IJ. BK virus infection in transplant recipients: clinical manifestations, treatment options and the immune response. Neth J Med. 2012;70:172–183. [PubMed] [Google Scholar]
- 59.van Aalderen MC, Remmerswaal EB, Heutinck KM, Ten Brinke A, Feltkamp MC, van der Weerd NC, van der Pant KA, Bemelman FJ, van Lier RA, Ten Berge IJ. 2016. Clinically Relevant Reactivation of Polyomavirus BK (BKPyV) in HLA-A02-Positive Renal Transplant Recipients Is Associated with Impaired Effector-Memory Differentiation of BKPyV-Specific CD8+ T Cells. PLoS Pathog 12: e1005903 [DOI] [PMC free article] [PubMed]
- 60.van Aalderen MC, Remmerswaal EB, Heutinck KM, ten Brinke A, Pircher H, van Lier RA, ten Berge IJ. Phenotypic and functional characterization of circulating polyomavirus BK VP1-specific CD8+ T cells in healthy adults. J Virol. 2013;87:10263–10272. doi: 10.1128/JVI.01540-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Boyman O, Hefti HP, Conrad C, Nickoloff BJ, Suter M, Nestle FO. Spontaneous development of psoriasis in a new animal model shows an essential role for resident T cells and tumor necrosis factor-alpha. J Exp Med. 2004;199:731–736. doi: 10.1084/jem.20031482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cheuk S, Wikén M, Blomqvist L, Nylén S, Talme T, Ståhle M, Eidsmo L. Epidermal Th22 and Tc17 cells form a localized disease memory in clinically healed psoriasis. J Immunol. 2014;192:3111–3120. doi: 10.4049/jimmunol.1302313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Matos TR, O'Malley JT, Lowry EL, Hamm D, Kirsch IR, Robins HS, Kupper TS, Krueger JG, Clark RA. Clinically resolved psoriatic lesions contain psoriasis-specific IL-17-producing αβ T cell clones. J Clin Invest. 2017;127:4031–4041. doi: 10.1172/JCI93396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Couzi L, Merville P, Deminière C, Moreau JF, Combe C, Pellegrin JL, Viallard JF, Blanco P. Predominance of CD8+ T lymphocytes among periglomerular infiltrating cells and link to the prognosis of class III and class IV lupus nephritis. Arthritis Rheum. 2007;56:2362–2370. doi: 10.1002/art.22654. [DOI] [PubMed] [Google Scholar]
- 65.O'Sullivan KM, Lo CY, Summers SA, Elgass KD, McMillan PJ, Longano A, Ford SL, Gan PY, Kerr PG, Kitching AR, Holdsworth SR. Renal participation of myeloperoxidase in antineutrophil cytoplasmic antibody (ANCA)-associated glomerulonephritis. Kidney Int. 2015;88:1030–1046. doi: 10.1038/ki.2015.202. [DOI] [PubMed] [Google Scholar]
- 66.Masutani K, Akahoshi M, Tsuruya K, Tokumoto M, Ninomiya T, Kohsaka T, Fukuda K, Kanai H, Nakashima H, Otsuka T, Hirakata H. Predominance of Th1 immune response in diffuse proliferative lupus nephritis. Arthritis Rheum. 2001;44:2097–2106. doi: 10.1002/1529-0131(200109)44:9<2097::AID-ART360>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 67.Zhou M, Guo C, Li X, Huang Y, Li M, Zhang T, Zhao S, Wang S, Zhang H, Yang N. 2020. JAK/STAT signaling controls the fate of CD8(+)CD103(+) tissue-resident memory T cell in lupus nephritis. J Autoimmun 109: 102424 [DOI] [PubMed]
- 68.Krebs CF, Paust HJ, Krohn S, Koyro T, Brix SR, Riedel JH, Bartsch P, Wiech T, Meyer-Schwesinger C, Huang J, Fischer N, Busch P, Mittrücker HW, Steinhoff U, Stockinger B, Perez LG, Wenzel UO, Janneck M, Steinmetz OM, Gagliani N, Stahl RAK, Huber S, Turner JE, Panzer U. Autoimmune Renal Disease Is Exacerbated by S1P-Receptor-1-Dependent Intestinal Th17 Cell Migration to the Kidney. Immunity. 2016;45:1078–1092. doi: 10.1016/j.immuni.2016.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tilstra JS, Avery L, Menk AV, Gordon RA, Smita S, Kane LP, Chikina M, Delgoffe GM, Shlomchik MJ. Kidney-infiltrating T cells in murine lupus nephritis are metabolically and functionally exhausted. J Clin Invest. 2018;128:4884–4897. doi: 10.1172/JCI120859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Arazi A, Rao DA, Berthier CC, Davidson A, Liu Y, Hoover PJ, Chicoine A, Eisenhaure TM, Jonsson AH, Li S, Lieb DJ, Zhang F, Slowikowski K, Browne EP, Noma A, Sutherby D, Steelman S, Smilek DE, Tosta P, Apruzzese W, Massarotti E, Dall'Era M, Park M, Kamen DL, Furie RA, Payan-Schober F, Pendergraft WF, 3rd, McInnis EA, Buyon JP, Petri MA, Putterman C, Kalunian KC, Woodle ES, Lederer JA, Hildeman DA, Nusbaum C, Raychaudhuri S, Kretzler M, Anolik JH, Brenner MB, Wofsy D, Hacohen N, Diamond B. The immune cell landscape in kidneys of patients with lupus nephritis. Nat Immunol. 2019;20:902–914. doi: 10.1038/s41590-019-0398-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bertolo M, Baumgart S, Durek P, Peddinghaus A, Mei H, Rose T, Enghard P, Grützkau A. Deep Phenotyping of Urinary Leukocytes by Mass Cytometry Reveals a Leukocyte Signature for Early and Non-Invasive Prediction of Response to Treatment in Active Lupus Nephritis. Front Immunol. 2020;11:256. doi: 10.3389/fimmu.2020.00256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Park SL, Gebhardt T, Mackay LK. Tissue-Resident Memory T Cells in Cancer Immunosurveillance. Trends Immunol. 2019;40:735–747. doi: 10.1016/j.it.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 73.Díaz-Montero CM, Rini BI, Finke JH. The immunology of renal cell carcinoma. Nat Rev Nephrol. 2020;16:721–735. doi: 10.1038/s41581-020-0316-3. [DOI] [PubMed] [Google Scholar]
- 74.Chevrier S, Levine JH, Zanotelli VRT, Silina K, Schulz D, Bacac M, Ries CH, Ailles L, Jewett MAS, Moch H, van den Broek M, Beisel C, Stadler MB, Gedye C, Reis B, Pe'er D, Bodenmiller B. An Immune Atlas of Clear Cell Renal Cell Carcinoma. Cell. 2017;169:736–49.e18. doi: 10.1016/j.cell.2017.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Geissler K, Fornara P, Lautenschläger C, Holzhausen HJ, Seliger B, Riemann D. 2015. Immune signature of tumor infiltrating immune cells in renal cancer. Oncoimmunology 4: e985082 [DOI] [PMC free article] [PubMed]
- 76.Kawashima A, Kanazawa T, Kidani Y, Yoshida T, Hirata M, Nishida K, Nojima S, Yamamoto Y, Kato T, Hatano K, Ujike T, Nagahara A, Fujita K, Morimoto-Okazawa A, Iwahori K, Uemura M, Imamura R, Ohkura N, Morii E, Sakaguchi S, Wada H, Nonomura N. Tumour grade significantly correlates with total dysfunction of tumour tissue-infiltrating lymphocytes in renal cell carcinoma. Sci Rep. 2020;10:6220. doi: 10.1038/s41598-020-63060-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fridman WH, Pagès F, Sautès-Fridman C, Galon J. The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer. 2012;12:298–306. doi: 10.1038/nrc3245. [DOI] [PubMed] [Google Scholar]
- 78.Nakano O, Sato M, Naito Y, Suzuki K, Orikasa S, Aizawa M, Suzuki Y, Shintaku I, Nagura H, Ohtani H. Proliferative activity of intratumoral CD8(+) T-lymphocytes as a prognostic factor in human renal cell carcinoma: clinicopathologic demonstration of antitumor immunity. Cancer Res. 2001;61:5132–5136. [PubMed] [Google Scholar]
- 79.Zhou J, Liu L, Yang T, Lu B. Prognostic and therapeutic value of CD103(+) cells in renal cell carcinoma. Exp Ther Med. 2018;15:4979–4986. doi: 10.3892/etm.2018.6025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Harshman LC, Drake CG, Choueiri TK. PD-1 blockade in renal cell carcinoma: to equilibrium and beyond. Cancer Immunol Res. 2014;2:1132–1141. doi: 10.1158/2326-6066.CIR-14-0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang J, Li X, Wu X, Wang Z, Zhang C, Cao G, Zhang X, Peng F, Yan T. Role of immune checkpoint inhibitor-based therapies for metastatic renal cell carcinoma in the first-line setting: A Bayesian network analysis. EBioMedicine. 2019;47:78–88. doi: 10.1016/j.ebiom.2019.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Park SL, Buzzai A, Rautela J, Hor JL, Hochheiser K, Effern M, McBain N, Wagner T, Edwards J, McConville R, Wilmott JS, Scolyer RA, Tüting T, Palendira U, Gyorki D, Mueller SN, Huntington ND, Bedoui S, Hölzel M, Mackay LK, Waithman J, Gebhardt T. Tissue-resident memory CD8(+) T cells promote melanoma-immune equilibrium in skin. Nature. 2019;565:366–371. doi: 10.1038/s41586-018-0812-9. [DOI] [PubMed] [Google Scholar]
- 83.Malik BT, Byrne KT, Vella JL, Zhang P, Shabaneh TB, Steinberg SM, Molodtsov AK, Bowers JS, Angeles CV, Paulos CM, Huang YH, Turk MJ. 2017. Resident memory T cells in the skin mediate durable immunity to melanoma. Sci Immunol 2 [DOI] [PMC free article] [PubMed]
- 84.Patel SP, Kurzrock R. PD-L1 Expression as a Predictive Biomarker in Cancer Immunotherapy. Mol Cancer Ther. 2015;14:847–856. doi: 10.1158/1535-7163.MCT-14-0983. [DOI] [PubMed] [Google Scholar]
- 85.Lemery S, Keegan P, Pazdur R. First FDA Approval Agnostic of Cancer Site - When a Biomarker Defines the Indication. N Engl J Med. 2017;377:1409–1412. doi: 10.1056/NEJMp1709968. [DOI] [PubMed] [Google Scholar]
- 86.McDermott DF, Huseni MA, Atkins MB, Motzer RJ, Rini BI, Escudier B, Fong L, Joseph RW, Pal SK, Reeves JA, Sznol M, Hainsworth J, Rathmell WK, Stadler WM, Hutson T, Gore ME, Ravaud A, Bracarda S, Suárez C, Danielli R, Gruenwald V, Choueiri TK, Nickles D, Jhunjhunwala S, Piault-Louis E, Thobhani A, Qiu J, Chen DS, Hegde PS, Schiff C, Fine GD, Powles T. Publisher Correction: Clinical activity and molecular correlates of response to atezolizumab alone or in combination with bevacizumab versus sunitinib in renal cell carcinoma. Nat Med. 2018;24:1941. doi: 10.1038/s41591-018-0235-z. [DOI] [PubMed] [Google Scholar]
- 87.Nizard M, Roussel H, Diniz MO, Karaki S, Tran T, Voron T, Dransart E, Sandoval F, Riquet M, Rance B, Marcheteau E, Fabre E, Mandavit M, Terme M, Blanc C, Escudie JB, Gibault L, Barthes FLP, Granier C, Ferreira LCS, Badoual C, Johannes L, Tartour E. Induction of resident memory T cells enhances the efficacy of cancer vaccine. Nat Commun. 2017;8:15221. doi: 10.1038/ncomms15221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Braun DA, Bakouny Z, Hirsch L, Flippot R, Van Allen EM, Wu CJ, Choueiri TK. Beyond conventional immune-checkpoint inhibition - novel immunotherapies for renal cell carcinoma. Nat Rev Clin Oncol. 2021;18:199–214. doi: 10.1038/s41571-020-00455-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Halloran PF. T cell-mediated rejection of kidney transplants: a personal viewpoint. Am J Transplant. 2010;10:1126–1134. doi: 10.1111/j.1600-6143.2010.03053.x. [DOI] [PubMed] [Google Scholar]
- 90.Venner JM, Famulski KS, Badr D, Hidalgo LG, Chang J, Halloran PF. Molecular landscape of T cell-mediated rejection in human kidney transplants: prominence of CTLA4 and PD ligands. Am J Transplant. 2014;14:2565–2576. doi: 10.1111/ajt.12946. [DOI] [PubMed] [Google Scholar]
- 91.Heeger PS, Greenspan NS, Kuhlenschmidt S, Dejelo C, Hricik DE, Schulak JA, Tary-Lehmann M. Pretransplant frequency of donor-specific, IFN-gamma-producing lymphocytes is a manifestation of immunologic memory and correlates with the risk of posttransplant rejection episodes. J Immunol. 1999;163:2267–2275. [PubMed] [Google Scholar]
- 92.Hricik DE, Rodriguez V, Riley J, Bryan K, Tary-Lehmann M, Greenspan N, Dejelo C, Schulak JA, Heeger PS. Enzyme linked immunosorbent spot (ELISPOT) assay for interferon-gamma independently predicts renal function in kidney transplant recipients. Am J Transplant. 2003;3:878–884. doi: 10.1034/j.1600-6143.2003.00132.x. [DOI] [PubMed] [Google Scholar]
- 93.Abou-Daya KI, Tieu R, Zhao D, Rammal R, Sacirbegovic F, Williams AL, Shlomchik WD, Oberbarnscheidt MH, Lakkis FG. 2021. Resident memory T cells form during persistent antigen exposure leading to allograft rejection. Sci Immunol 6 [DOI] [PMC free article] [PubMed]