Abstract
Background
Patients with dementia are frequently hospitalized and may face barriers in post-discharge care.
Objective
To determine whether patients with dementia have an increased risk of adverse outcomes following discharge.
Design
Retrospective cohort study.
Subjects
Medicare beneficiaries hospitalized in 2016.
Main Measures
Co-primary outcomes were mortality and readmission within 30 days of discharge. Multivariable logistic regression models were estimated to assess the risk of each outcome for patients with and without dementia accounting for demographics, comorbidities, frailty, hospitalization factors, and disposition.
Key Results
The cohort included 1,089,109 hospitalizations of which 211,698 (19.3%) were of patients with diagnosed dementia (median (IQR) age 83 (76–89); 61.5% female) and 886,411 were of patients without dementia (median (IQR) age 76 (79–83); 55.0% female). At 30 days following discharge, 5.7% of patients with dementia had died compared to 3.1% of patients without dementia (adjusted odds ratio (aOR) 1.21; 95% CI 1.17 to 1.24). At 30 days following discharge, 17.7% of patients with dementia had been readmitted compared to 13.1% of patients without dementia (aOR 1.02; CI 1.002 to 1.04). Dementia was associated with an increased odds of readmission among patients discharged to the community (aOR 1.07, CI 1.05 to 1.09) but a decreased odds of readmission among patients discharge to nursing facilities (aOR 0.93, CI 0.90 to 0.95). Patients with dementia who were discharged to the community were more likely to be readmitted than those discharged to nursing facilities (18.9% vs 16.0%), and, when readmitted, were more likely to die during the readmission (20.7% vs 4.4%).
Conclusions
Diagnosed dementia was associated with a substantially increased risk of mortality and a modestly increased risk of readmission within 30 days of discharge. Patients with dementia discharged to the community had particularly elevated risk of adverse outcomes indicating possible gaps in post-discharge services and caregiver support.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-022-07549-7.
INTRODUCTION
Over 11% of Medicare beneficiaries have diagnosed dementia, including Alzheimer’s disease- and Alzheimer’s disease-related dementias.1 Older adults with diagnosed dementia have increased rates of hospitalization and post-acute care, resulting in substantially increased Medicare expenditures compared to other older adults.2–5 Those with dementia are also at increased risk of preventable hospitalizations and in-hospital complications including in-hospital death, delirium, functional decline, and adverse drug events.6–9 Cognitive impairment creates barriers in self-care after discharge, limiting patients’ ability to understand and carry out discharge plans and to seek early outpatient care when problems arise. Thus, after hospitalization, older adults with dementia who are discharged home may be at particularly high risk for adverse outcomes.
Prior research examining the association between dementia and post-discharge outcomes has had conflicting findings, which likely reflect the heterogeneity of studied populations.8–10 Prior studies have been single-center or focused on small geographic regions,11,12 or non-US populations.13–15 Additionally, few studies have accounted for geriatric syndromes such as frailty, multi-morbidity, and delirium, which often occur alongside dementia. The most comprehensive study to date, an examination of national discharge data from Japan, found that readmission rates were higher among patients with dementia overall, but varied by index hospitalization diagnosis.15 The generalizability of this study to the USA may be limited, as observed readmission rates were less than half of US readmission rates and rates of discharge to nursing facilities were much lower. Furthermore, the availability of caregiver support and resources for caregivers may differ across countries, and in the USA, caregiver burden is common and contributes to adverse outcomes for patients with dementia.16,17
To inform the development of US initiatives to improve discharge planning and post-discharge care for older adults with dementia, we sought to determine the association between dementia and post-discharge mortality and readmissions by examining a national cohort of Medicare beneficiaries hospitalized in 2016. We hypothesized that patients with dementia would have increased risk of adverse outcomes, even after accounting for multi-morbidity and frailty, and that risks would be the highest among those discharged to the community.
METHODS
This study was determined to be exempt from review by the Beth Israel Deaconess Medical Center Institutional Review Board.
Study Population
We used a 20% national sample of Centers for Medicare & Medicaid Services (CMS) Medicare Provider Analysis and Review files to identify acute care hospitalizations of adults aged 65 years and older between January 1, 2016, and November 30, 2016. We included patients enrolled in Medicare fee-for-service for at least 1 year before hospitalization and at least 30 days after discharge. The unit of observation was the hospitalization; thus, patients could contribute multiple hospitalizations and a hospitalization could be both an index hospitalization and a readmission outcome.
We examined index hospitalizations as defined by the CMS readmission and mortality measures, which include an overall hospitalization category and five sub-cohorts defined using International Classification of Diseases, Tenth Revision to reflect common conditions commonly cared for by different clinical services in hospitals: cardiorespiratory, cardiovascular, neurology, medicine, and surgery/gynecology.18,19 Consistent with CMS measures, we excluded index hospitalizations in which patients died during the index hospitalization, were discharged against medical advice, or were discharged to hospice. We also excluded index hospitalizations for psychiatric diagnoses, rehabilitation, and medical treatment of cancer.
Dementia Diagnosis
We used the CMS Chronic Condition Warehouse algorithm for Alzheimer’s Disease, Related Disorders, or Senile Dementia to identify patients with a dementia diagnosis based upon the presence of one or more dementia diagnosis codes in the 3 years preceding the index hospitalization.20
Outcomes
The primary outcomes were mortality within 30 days of hospital discharge and unplanned hospital readmission within 30 days of hospital discharge. We defined hospital readmissions to include both admissions and observation stays, given evidence suggesting that hospitals may be substituting observation stays for readmissions in response to financial incentives to reduce readmissions and that the distinction between observation stay and admission is often financial rather than clinical.21,22 Readmissions for planned procedures or medical treatments were excluded in accordance with the CMS planned readmission algorithm.19,23
Among patients who were readmitted, we examined discharge diagnoses and subsequent dispositions. Discharge diagnoses were grouped using Agency for Healthcare Research and Quality Clinical Classifications Software (CCS).24 Disposition following readmission was classified as community discharge, facility discharge (including skilled nursing, inpatient rehabilitation, and long-term care facilities), hospital transfer, discharge to hospice, discharge against medical advice, and death during hospitalization.
Covariates
Covariates included patient demographics, comorbidities, frailty, hospitalization factors, and discharge factors. Demographics included age, sex, race/ethnicity, and eligibility for Medicaid. Comorbidities included 50 common chronic conditions, including both chronic diseases and functional impairments, as defined by CMS Chronic Condition Warehouse algorithms. In addition, we included the AHRQ Elixhauser Comorbidity mortality and readmissions indices, which are derived from 29 Elixhauser comorbidities coded on the index hospitalization as being actively managed during hospitalization.25 We used a modified version of the validated claims-based frailty index (CFI), which approximates a standard deficit-accumulation frailty index using diagnosis, procedure, equipment, and device coding.26 We removed the “hereditary and degenerative diseases of the central nervous system” variable from the CFI as it was highly collinear with the primary predictor of dementia. Hospitalization characteristics included state, admission source, specialty cohort, receipt of intensive care unit services, discharge diagnosis (defined by second-level CCS diagnosis categories), performance of major procedures (defined by first-level CCS procedure categories), and presence of delirium (defined by discharge diagnoses using a highly specific but poorly sensitive algorithm27). Discharge factors included discharge on a weekend and discharge to a facility (long-term care, inpatient rehabilitation, or skilled nursing facility).
Statistical Analyses
The primary analyses examined the association between dementia and 30-day mortality and 30-day readmissions in the overall cohort using separate logistic regression models. Multivariable logistic regression models were fitted to estimate odds ratios (ORs) with 95% confidence intervals (CIs) of each outcome among hospitalizations of patients with versus without a dementia diagnosis. Models included the aforementioned covariates to account for differences in characteristics of patients with and without diagnosed dementia and differences in index hospitalization care, and clustered sandwich estimators to account for multiple hospitalizations within patients. The AHRQ Elixhauser Comorbidity mortality index was included in the models estimating 30-day mortality whereas the AHRQ Elixhauser Comorbidity readmissions index was included in the models estimating 30-day readmissions. All analyses were conducted using Stata v.16.1. Statistical tests were 2-sided at a significance level of .05.
We conducted two sets of subgroup analyses defined a priori. First, we examined the primary outcomes in the five specialty cohorts to assess whether the association of dementia with post-discharge outcomes differed by reason for hospitalization. Second, we examined the primary outcomes among patients discharged to the community and those discharged to skilled nursing or inpatient rehabilitation facilities.
Among patients who were readmitted, we used descriptive statistics to explore differences in reasons for readmission and disposition following readmission among patients with and without diagnosed dementia.
Sensitivity Analysis
We conducted two sensitivity analyses. First, we examined unplanned “return-to-hospital” within 30 days of discharge. Return-to-hospital is a combined outcome of readmissions and emergency room visits, which has been proposed as an alternative to readmission measures since it captures visits by patients who lack access to other ambulatory care or are concerned enough to seek emergent care following hospitalization but are not admitted to the hospital.22 Second, we limited our analyses to patients admitted from the community, excluding those transferred from nursing facilities.
RESULTS
The final study cohort consisted of 1,089,109 hospitalizations by 759,437 Medicare beneficiaries (eFigure 1). In the final cohort, 211,698 (19.3%) hospitalizations occurred in patients with diagnosed dementia (Table 1). Compared to patients without dementia, patients with dementia were older (median age 83 years vs 76 years), and a greater proportion were female (61.5% vs 55.0%), Black (12.7% vs 8.6%), Hispanic (6.6% vs 4.6%), and Medicaid eligible (36.4% vs 17.0%). Patients with dementia were more likely to have nearly all chronic conditions. A greater proportion of patients with dementia were moderately or severely frail (24.8% vs 9.7%) and were admitted from nursing facilities (8.7% vs 2.3%). Patients with dementia had a longer median length of stay (4 days vs 3 days) and were more likely to have diagnosed delirium (17.7% vs 6.3%). At discharge, 42.1% of patients with dementia were discharged to skilled nursing facilities compared to 21.6% of patients without dementia.
Table 1.
Characteristics of Hospitalizations of Medicare Beneficiaries with and without Diagnosed Dementia
| Patients with dementia (N=211,698) |
Patients without dementia (N=886,411) |
P | |
|---|---|---|---|
| Demographics | |||
| Age, median (IQR), years | 83 (76–89) | 76 (79–83) | <.001 |
| Female, No. (%) | 130162 (61.5) | 487668 (55.0) | <.001 |
| Race/ethnicity, No. (%) | <.001 | ||
| White | 163800 (77.4) | 736702 (83.1) | |
| Black | 26838 (12.7) | 76606 (8.6) | |
| Asian/Pacific Islander | 4293 (2.0) | 15288 (1.7) | |
| Hispanic | 13974 (6.6) | 41165 (4.6) | |
| Other | 2793 (1.3) | 16650 (1.9) | |
| Medicaid eligible, No. (%) | 76976 (36.4) | 150605 (17.0) | |
| Chronic conditions, No. (%) | |||
| Acute myocardial infarction | 6185 (2.9) | 17147 (1.9) | <.001 |
| Alcohol use disorders | 9182 (4.3) | 24973 (2.8) | <.001 |
| Anemia | 119838 (56.6) | 336700 (38.0) | <.001 |
| Anxiety disorders | 72012 (34.0) | 156022 (17.6) | <.001 |
| Asthma | 22259 (10.5) | 81226 (9.2) | <.001 |
| Atrial fibrillation | 49629 (23.4) | 163464 (18.4) | <.001 |
| Attention-deficit hyperactivity disorder | 3721 (1.8) | 3146 (0.4) | <.001 |
| Benign prostatic hyperplasia | 30563 (14.4) | 92880 (10.5) | <.001 |
| Bipolar disorder | 16437 (7.8) | 17179 (1.9) | <.001 |
| Blindness and visual impairment | 7608 (3.6) | 10410 (1.2) | <.001 |
| Breast cancer | 8861 (4.2) | 37478 (4.2) | .38 |
| Cataract | 36732 (17.4) | 180027 (20.3) | <.001 |
| Chronic kidney disease | 107662 (50.9) | 310144 (35.0) | <.001 |
| Chronic obstructive pulmonary disease | 67456 (31.9) | 212719 (24.0) | <.001 |
| Colorectal cancer | 5165 (2.4) | 20823 (2.3) | .01 |
| Deafness and hearing impairment | 25030 (11.8) | 60478 (6.8) | <.001 |
| Diabetes | 100519 (47.5) | 354668 (40.0) | <.001 |
| Endometrial cancer | 1151 (0.5) | 5118 (0.6) | .07 |
| Epilepsy | 18732 (8.8) | 20701 (2.3) | <.001 |
| Fibromyalgia, chronic pain, and fatigue | 52961 (25.0) | 181107 (20.4) | <.001 |
| Glaucoma | 22138 (10.5) | 99417 (11.2) | <.001 |
| Heart failure | 99353 (46.9) | 267053 (30.1) | <.001 |
| Hip/pelvic fracture | 7836 (3.7) | 9394 (1.1) | <.001 |
| HIV/AIDS | 436 (0.2) | 1522 (0.2) | .001 |
| Hyperlipidemia | 135880 (64.2) | 538921 (60.8) | <.001 |
| Hypertension | 185360 (87.6) | 677425 (76.4) | <.001 |
| Hypothyroidism | 59798 (28.2) | 183322 (20.7) | <.001 |
| Ischemic heart disease | 127229 (60.1) | 419168 (47.3) | <.001 |
| Leukemias and lymphomas | 4514 (2.1) | 23326 (2.6) | <.001 |
| Liver disease | 14225 (6.7) | 54765 (6.2) | <.001 |
| Lung cancer | 3196 (1.5) | 18585 (2.1) | <.001 |
| Migraine and chronic headache | 5779 (2.7) | 21451 (2.4) | <.001 |
| Mobility impairments | 24754 (11.7) | 31834 (3.6) | <.001 |
| Multiple sclerosis and transverse myelitis | 1555 (0.7) | 4338 (0.5) | <.001 |
| Obesity | 37581 (17.8) | 175557 (19.8) | <.001 |
| Opioid use disorder | 6073 (2.9) | 15829 (1.8) | <.001 |
| Osteoporosis | 30448 (14.4) | 78468 (8.9) | <.001 |
| Peripheral vascular disease | 81109 (38.3) | 192917 (21.8) | <.001 |
| Post-traumatic stress disorder | 2008 (0.9) | 5329 (0.6) | <.001 |
| Pressure and chronic ulcers | 41501 (19.6) | 77551 (8.7) | <.001 |
| Prostate cancer | 9444 (4.5) | 41734 (4.7) | <.001 |
| Rheumatoid arthritis/osteoarthritis | 116689 (55.1) | 414225 (46.7) | <.001 |
| Schizophrenia and other psychotic disorders | 36664 (17.3) | 18614 (2.1) | <.001 |
| Spinal cord injury | 2968 (1.4) | 5178 (0.6) | <.001 |
| Stroke/transient ischemic attack | 35007 (16.5) | 54419 (6.1) | <.001 |
| Tobacco use | 22822 (10.8) | 92646 (10.5) | <.001 |
| Traumatic brain injury | 4387 (2.1) | 3136 (0.4) | <.001 |
| Viral hepatitis | 3547 (1.7) | 12389 (1.4) | <.001 |
| Frailty category, No. (%) | <.001 | ||
| Not frail | 6768 (3.2) | 90172 (10.2) | |
| Prefrail | 56310 (26.6) | 444730 (50.2) | |
| Mildly frail | 96062 (45.4) | 265501 (30.0) | |
| Moderately/severely frail | 52558 (24.8) | 86008 (9.7) | |
| Hospitalization factors | |||
| Admission source, No. (%) | <.001 | ||
| Community | 181079 (85.5) | 801601 (90.4) | |
| Hospital transfer | 11717 (5.5) | 62287 (7.0) | |
| Nursing facility | 18327 (8.7) | 20726 (2.3) | |
| Unknown | 575 (0.3) | 1797 (0.2) | |
| Length of stay, median (IQR), days | 4 (3–6) | 3 (2–6) | <.001 |
| Specialty cohort, No. (%) | <.001 | ||
| Medicine | 79412 (37.5) | 335452 (37.8) | |
| Cardiorespiratory | 37109 (17.5) | 141732 (16.0) | |
| Cardiovascular | 17788 (8.4) | 120681 (13.6) | |
| Neurology | 18554 (8.8) | 64904 (7.3) | |
| Surgery/gynecology | 58835 (27.8) | 223642 (25.2) | |
| Intensive care unit, No. (%) | 58741 (27.8) | 247813 (28.0) | .05 |
| Delirium, No. (%) | 37453 (17.7) | 56100 (6.3) | <.001 |
| Discharge factors | |||
| Weekend discharge, No. (%) | 35374 (16.7) | 178666 (20.2) | <.001 |
| Discharge to skilled nursing facility, No. (%) | 89173 (42.1) | 191156 (21.6) | <.001 |
Note: P-values presented for comparison of characteristics of hospitalizations of patients with and without dementia using χ2 tests for categorical variables and t tests for continuous variables
Mortality Following Discharge
At 30 days following discharge, 5.7% of patients with dementia had died compared to 3.1% of patients without dementia (Table 2). After adjustment, patients with dementia had an increased odds of death within 30 days of discharge (OR 1.21; CI 1.17 to 1.24). In subgroup analyses, patients with dementia had higher rates of death in all specialty cohorts and this association persisted in adjusted models, with the highest ORs among patients in the medicine (OR 1.32; 95% CI 1.25 to 1.39) and neurology cohorts (OR 1.33; CI 1.20 to 1.47). Patients with dementia who were discharged to the community had a greater increased odds of death (OR 1.32, CI 1.27 to 1.37) compared to those who were discharged to nursing facilities (OR 1.10, CI 1.06 to 1.14).
Table 2.
Association between Diagnosed Dementia and 30-Day Post-discharge Mortality
| Patients with dementia | Patients without dementia | aOR (95% CI) | |
|---|---|---|---|
| No. died (%) | No. died (%) | ||
| Overall cohort | 12015 (5.7) | 27175 (3.1) | 1.21 (1.17–1.24) |
| Specialty cohorts | |||
| Cardiorespiratory | 2539 (6.8) | 6729 (4.7) | 1.07 (1.01–1.13) |
| Cardiovascular | 802 (4.5) | 2606 (2.2) | 1.20 (1.10–1.33) |
| Medicine | 3563 (4.5) | 6560 (2.0) | 1.32 (1.25–1.39) |
| Neurology | 938 (5.1) | 1781 (2.7) | 1.33 (1.20–1.47) |
| Surgery/gynecology | 4173 (7.1) | 9499 (4.2) | 1.20 (1.14–1.26) |
| Discharge disposition | |||
| Community | 5069 (4.1) | 14485 (2.1) | 1.32 (1.26–1.37) |
| Facility | 6946 (7.8) | 12690 (6.6) | 1.10 (1.06–1.14) |
Notes: Facility discharge includes discharge to skilled nursing facilities, long-term care facilities, and inpatient rehab facilities. Cohorts exclude patients discharged to hospice
Readmission Following Discharge
At 30 days following discharge, 17.7% of patients with dementia had been readmitted compared to 13.1% of patients without dementia (Table 3). After adjustment, patients with dementia had a modestly increased odds of readmission (OR 1.02; CI 1.002 to 1.04). In subgroup analyses, there were modestly increased odds of readmission for patients with dementia following cardiovascular (OR 1.07, CI 1.01 to 1.12) and medicine hospitalizations (1.04, CI 1.01 to 1.07) and no difference following cardiorespiratory, neurology, or surgery/gynecology hospitalizations.
Table 3.
Association between Diagnosed Dementia and 30-Day Hospital Readmissions
| Patients with dementia | Patients without dementia | aOR (95% CI) | |
|---|---|---|---|
| No. readmitted (%) | No. readmitted (%) | ||
| Overall cohort | 37422 (17.7) | 116078 (13.1) | 1.02 (1.002–1.04) |
| Specialty cohorts | |||
| Cardiorespiratory | 7984 (21.5) | 27439 (19.4) | 0.98 (0.95–1.01) |
| Cardiovascular | 3309 (18.6) | 15269 (12.7) | 1.07 (1.01–1.12) |
| Medicine | 11436 (14.4) | 29082 (8.7) | 1.04 (1.01–1.07) |
| Neurology | 2940 (15.8) | 7780 (12.0) | 1.05 (0.996–1.11) |
| Surgery/gynecology | 11753 (20.0) | 36508 (16.3) | 1.01 (0.98–1.04) |
| Discharge disposition | |||
| Community | 23174 (18.9) | 87841 (12.6) | 1.07 (1.05–1.09) |
| Facility | 14248 (16.0) | 28237 (14.8) | 0.93 (0.90–0.95) |
Note: Readmissions exclude planned readmissions and include hospital observation stays. Facility discharge includes discharge to skilled nursing facilities, long-term care facilities, and inpatient rehab facilities
A greater proportion of patients with dementia who were discharged to the community were readmitted compared to those discharged to nursing facilities (18.9% vs 16.0%). Among patients discharged to the community, patients with dementia were more likely to be readmitted within 30 days than those without dementia (18.9% vs 12.6%; OR 1.07, CI 1.05 to 1.09). Among patients discharged to nursing facilities, a greater proportion of patients with dementia were readmitted (16.0% vs 14.8% of patients without dementia), but after adjusting for patient and hospitalization characteristics, patients with dementia had a lower odds of readmission (OR 0.93, CI 0.90 to 0.95).
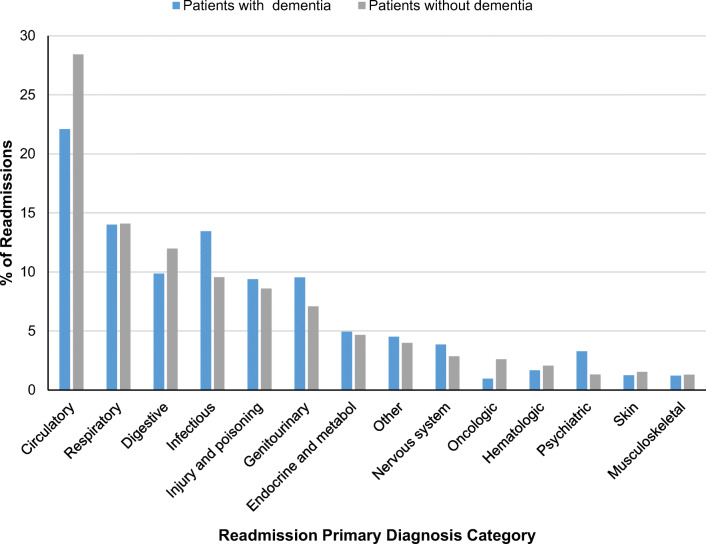
Figure 1 depicts the primary readmission diagnoses of patients with and without dementia who were readmitted within 30 days of index hospital discharge. A greater proportion of patients with dementia were readmitted for infectious, genitourinary, injury-related, and psychiatric diagnoses while fewer were admitted for circulatory system diagnoses. These observed differences were consistent across subgroups defined by the reason for index hospitalization (eFigure 2).
Figure 1.
Primary diagnoses of hospital readmissions among Medicare beneficiaries with and without diagnosed dementia.
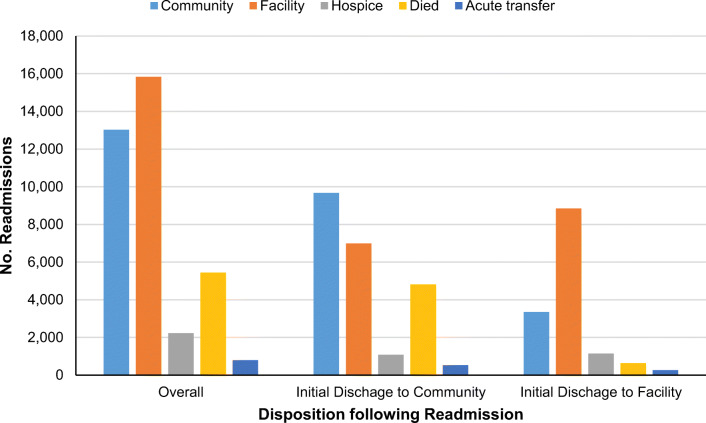
Following discharge, 167,710 (79.2%) patients with dementia were neither readmitted nor died within 30 days, 37,422 (17.7%) of patients with dementia were readmitted, and 6,566 (3.1%) patients died without being readmitted. Figure 2 depicts the disposition of patients with dementia who were readmitted. Among readmitted patients with dementia, 14.5% died during the readmission and 5.9% were discharged to hospice. Death during readmission was more common among patients initially discharged to the community (20.7%) compared to those initially discharged to nursing facilities (4.4%). Among patients initially discharged to the community, 30.2% were subsequently discharged to a nursing facility following readmission.
Figure 2.
Disposition of patients with dementia following unplanned readmissions. Note: Readmissions exclude planned readmissions and include hospital observation stays. 116 readmissions resulted in patients leaving against medical advice not depicted on graph due to low sample size (98 following initial community discharge; 18 following initial facility discharge). Chi-2 test of difference in proportions of patients initially discharged to the community compared to those initially discharged to a facility P<0.001.
Sensitivity Analyses
Analyses examining return-to-hospital for readmission or emergency department visits within 30 days demonstrated similar results to 30-day readmissions, with 26.9% of patients with dementia having a return-to-hospital event compared to 21.2% of patients without dementia (OR 1.05; CI 1.03 to 1.06) (eTable 1).
Analyses restricted to patients hospitalized from the community demonstrated similar results to primary analyses, with an increased risk of mortality, readmission, and return-to-hospital observed among patients with dementia compared to patients without dementia (eTable 2).
DISCUSSION
In this national cohort study of Medicare beneficiaries, diagnosed dementia was associated with a substantially increased risk of post-discharge non-hospice mortality and a modestly increased risk of readmission. Patients with dementia who were discharged to the community had elevated risk of adverse outcomes compared to those discharged to nursing facilities, including a 21% inpatient mortality rate during subsequent readmissions. These findings indicate an urgent need to strengthen and tailor discharge planning, including community and caregiver support services and advanced care planning, for this vulnerable patient population.
Our study builds on prior single-center and disease-specific readmission studies in the USA and internationally which have had conflicting findings on the association between dementia and readmissions.8–10 A key limitation of prior research has been lack of adjustment for geriatric syndromes, such as frailty and delirium, which frequently co-exist with dementia and have been independently associated with adverse post-hospital outcomes.28,29 By applying recently developed claims-based measures of frailty,26 comorbidity,25 and delirium27 to a national sample of Medicare beneficiaries, the current study is able to extend this prior work. Our findings are consistent with a recent national study from Japan which found an elevated risk of readmissions among patients with dementia after controlling for clinical variables, but was only able to assess readmissions of patients to the same hospital as the index hospitalization.15
The observed differences in post-discharge outcomes among patients discharged to the community and those discharged to nursing and rehab facilities have implications for clinicians and policy makers seeking to improve discharge planning. While patients without dementia who were discharged to nursing facilities were more likely to be readmitted than those discharged to the community, likely reflecting higher severity of illness, the converse was true for patients with dementia. This differential finding of patients with dementia who are discharged home being more likely to be readmitted indicates that current processes of care to assess discharge readiness and home support may be poorly suited for assessing home safety for patients with dementia. When coupled with the finding of 21% mortality among readmitted patients with dementia, our results may also suggest a need for earlier advance care planning so that community-based patients nearing the end of life are able to spend their last days at home rather than the hospital, if desired.
Few studies have examined outcomes of patients with dementia discharged to the community. One recent study, not focused on patients with dementia, found that Medicare beneficiaries discharged to home with home health care had higher rates of readmission compared to those discharged to skilled nursing facilities.30 A second study focused on the subgroup of Medicare beneficiaries discharged to skilled nursing facilities found that differences in risk of readmissions among patients with and without dementia were small and varied with the severity of cognitive impairment at the time of skilled nursing facility admission, information not available in the current study.31 A third study, examining Medicare beneficiaries hospitalized in Rhode Island in 2009, observed dementia was associated with a greater risk of readmissions, particularly for those discharged to nursing facilities, but this study did not control for frailty or delirium.32 Together with the current study findings, these data highlight important opportunities to improve care for patients with dementia by focusing efforts to safely triage and support patients who are discharged home.
Self-care after hospitalization requires knowledge, planning, and ability to carry out post-discharge care plans and to identify and address early complications.33 Even among older adults without dementia, understanding of discharge care plans is frequently poor,34,35 and cognitive impairment can pose barriers to completing discharge plans, particularly if caregivers are not involved at the time of discharge.36,37 While not all readmissions are preventable,38 prior research indicates patients with dementia are at high risk of potentially preventable hospitalizations6 and the high inpatient mortality rate among patients with dementia readmitted from home observed in this study highlights the possibility of delays in seeking necessary care. Contributing factors may include insufficient home support, barriers to accessing timely outpatient care,39 and social determinants of health, including neighborhood socioeconomic disadvantage.40,41
Our study indicates that targeted efforts are urgently needed to improve post-discharge outcomes for patients with dementia discharged to the community. We find that patients with dementia were more often readmitted for infectious, genitourinary, and injury-related diagnoses, all of which are often preventable. This builds on prior research demonstrating an increase in potentially preventable hospitalizations of individuals with dementia, particularly those hospitalized from the community, over time.6 Policy efforts to reduce avoidable hospital transfers among nursing home residents with advanced illness, including dementia, have demonstrated early success,42 as have dementia care management programs.43 Successful efforts to reduce post-discharge readmissions and mortality will need to adapt current inpatient and post-discharge ambulatory care delivery to the unique needs of patients with dementia and their caregivers as outlined by the National Academies of Sciences, Engineering, and Medicine.44 Strategies may include developing transitional care management programs45 and quality improvement interventions46 tailored to patients with dementia and to improving payment policies to support comprehensive dementia care,47 family caregiver training,48 and coverage of home equipment.49
Limitations
Our study had several limitations. First, as a study of claims data, we were able to compare only patients with previously diagnosed dementia to those without; thus, individuals with previously undiagnosed dementia or those diagnosed with dementia during hospitalization may have been miscategorized, which would likely have biased our findings towards the null. Second, we were unable to examine patients enrolled in Medicare Advantage or those hospitalized in the Veterans Affairs health system, who may have different patterns of care following hospitalization.50,51 Third, our findings do not generalize to patients hospitalized for medical treatment of cancer or psychiatric diagnoses. Fourth, while we were able to include measures of multi-morbidity, frailty, and hospitalization characteristics, we were unable to examine functional status at discharge, which is associated with adverse post-hospital outcomes.52,53 For this reason, we sought to examine outcomes stratified by discharge disposition as functional impairment is associated with discharge to nursing facilities. Fifth, we were unable to assess caregiver presence or use of home services following discharge, which may impact post-discharge outcomes for patients with dementia.
Conclusions
Among hospitalized Medicare beneficiaries, diagnosed dementia was associated with a substantially increased risk of post-discharge mortality and a modestly increased risk of readmission. Rates of adverse outcomes were uniformly worse among patients discharged to the community compared to those discharged to nursing facilities, indicating important opportunities to improve transitions of care for patients with dementia through improvements in discharge planning, including community and caregiver support services.
Supplementary Information
(DOCX 43 kb)
Sponsor’s Role
The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation or approval of the manuscript; and decision to submit the manuscript for publication.
Author Contribution
Timothy S. Anderson had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Anderson, McCarthy, Marcantonio, and Herzig.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Anderson.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Anderson, Ngo.
Obtained funding: Anderson.
Administrative, technical, or material support: Marcantonio, Herzig, and McCarthy.
Study supervision: Herzig.
Funding
Timothy S. Anderson was supported by grants from the National Institute on Aging (NIA) (L30AG060493 and R03AG064373). Shoshana J. Herzig was supported by a R01HS026215 from the Agency for Healthcare Research and Quality. Edward R. Marcantonio is supported by grants from the NIA (K24AG035075 and R01AG030618). Ellen P. McCarthy is supported by a U54AG063546 that funds NIA Imbedded Pragmatic Alzheimer’s Disease and AD-Related Dementias Clinical Trials Collaboratory (NIA IMPACT Collaboratory). Mara A. Schonberg is supported by a K24AG071906 from the NIA. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declarations
Conflict of Interest
Dr. Anderson reports receiving honoraria from Alosa Health, a nonprofit educational organization with no relationship to any drug or device manufacturers, related to deprescribing education.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centers for Medicare & Medicaid Services. Medicare Chronic Conditions Dashboard. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/CCDashboard. Accessed June 24, 2021.
- 2.Zhao Y, Kuo TC, Weir S, Kramer MS, Ash AS. Healthcare costs and utilization for Medicare beneficiaries with Alzheimer’s. BMC Health Serv Res. 2008;8:108. doi: 10.1186/1472-6963-8-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013;368(14):1326–1334. doi: 10.1056/NEJMsa1204629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phelan EA, Borson S, Grothaus L, Balch S, Larson EB. Association of incident dementia with hospitalizations. JAMA. 2012;307(2):165–172. doi: 10.1001/jama.2011.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feng Z, Coots LA, Kaganova Y, Wiener JM. Hospital and ED use among Medicare beneficiaries with dementia varies by setting and proximity to death. Health Aff (Millwood) 2014;33(4):683–690. doi: 10.1377/hlthaff.2013.1179. [DOI] [PubMed] [Google Scholar]
- 6.Anderson TS, Marcantonio ER, McCarthy EP, Herzig SJ. National trends in potentially preventable hospitalizations of older adults with dementia. J Am Geriatr Soc. 2020;68(10):2240–2248. doi: 10.1111/jgs.16636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shepherd H, Livingston G, Chan J, Sommerlad A. Hospitalisation rates and predictors in people with dementia: a systematic review and meta-analysis. BMC Med. 2019;17(1):130. doi: 10.1186/s12916-019-1369-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ma C, Bao S, Dull P, Wu B, Yu F. Hospital readmission in persons with dementia: a systematic review. Int J Geriatr Psychiatry. 2019;34(8):1170–1184. doi: 10.1002/gps.5140. [DOI] [PubMed] [Google Scholar]
- 9.Rao A, Suliman A, Vuik S, Aylin P, Darzi A. Outcomes of dementia: Systematic review and meta-analysis of hospital administrative database studies. Arch Gerontol Geriatr. 2016;66:198–204. doi: 10.1016/j.archger.2016.06.008. [DOI] [PubMed] [Google Scholar]
- 10.Lehmann J, Michalowsky B, Kaczynski A, Thyrian JR, Schenk NS, Esser A, Zwingmann I, Hoffmann W. The Impact of Hospitalization on Readmission, Institutionalization, and Mortality of People with Dementia: a systematic review and meta-analysis. J Alzheimers Dis. 2018;64(3):735–749. doi: 10.3233/JAD-171128. [DOI] [PubMed] [Google Scholar]
- 11.Daiello LA, Gardner R, Epstein-Lubow G, Butterfield K, Gravenstein S. Association of dementia with early rehospitalization among Medicare beneficiaries. Arch Gerontol Geriatr. 2014;59(1):162–8. doi: 10.1016/j.archger.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 12.Silverstein MD, Qin H, Mercer SQ, Fong J, Haydar Z. Risk factors for 30-day hospital readmission in patients ≥65 years of age. Proc (Bayl Univ Med Cent). 2008;21(4):363–72. doi: 10.1080/08998280.2008.11928429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tropea J, LoGiudice D, Liew D, Gorelik A, Brand C. Poorer outcomes and greater healthcare costs for hospitalised older people with dementia and delirium: a retrospective cohort study. Int J Geriatr Psychiatry. 2017;32(5):539–547. doi: 10.1002/gps.4491. [DOI] [PubMed] [Google Scholar]
- 14.Sganga F, Landi F, Volpato S, Cherubini A, Ruggiero C, Corsonello A, Fabbietti P, Lattanzio F, Gravina EM, Bernabei R, Onder G. Predictors of rehospitalization among older adults: results of the CRIME Study. Geriatr Gerontol Int. 2017;17(10):1588–1592. doi: 10.1111/ggi.12938. [DOI] [PubMed] [Google Scholar]
- 15.Sakata N, Okumura Y, Fushimi K, Nakanishi M, Ogawa A. Dementia and risk of 30-day readmission in older adults after discharge from Acute Care Hospitals. J Am Geriatr Soc. 2018;66(5):871–878. doi: 10.1111/jgs.15282. [DOI] [PubMed] [Google Scholar]
- 16.Callahan CM. Alzheimer’s disease: individuals, dyads, communities, and costs. J Am Geriatr Soc. 2017;65(5):892–895. doi: 10.1111/jgs.14808. [DOI] [PubMed] [Google Scholar]
- 17.Possin KL, Merrilees JJ, Dulaney S, et al. Effect of collaborative dementia care via telephone and internet on quality of life, caregiver well-being, and health care use: the care ecosystem randomized clinical trial. JAMA Intern Med. 2019;179(12):1658–1667. doi: 10.1001/jamainternmed.2019.4101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Medicare & Medicaid Services. Hospital Inpatient Measures: Mortality Measures Methodology. https://qualitynet.cms.gov/inpatient/measures/mortality/methodology. Accessed June 24, 2021.
- 19.Centers for Medicare & Medicaid Services. Hospital Inpatient Measures: Readmission Measures Methodology. https://qualitynet.cms.gov/inpatient/measures/readmission/methodology. Accessed June 24, 2021.
- 20.Centers for Medicare & Medicaid Services. Chronic Conditions Data Warehouse. https://www2.ccwdata.org/web/guest/condition-categories. Accessed June 24, 2021.
- 21.Venkatesh AK, Wang C, Ross JS, et al. Hospital use of observation stays: cross-sectional study of the impact on readmission rates. Med Care. 2016;54(12):1070–1077. doi: 10.1097/MLR.0000000000000601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wadhera RK, Yeh RW, Joynt Maddox KE. The Hospital Readmissions Reduction Program: time for a reboot. N Engl J Med. 2019;380(24):2289–2291. doi: 10.1056/NEJMp1901225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horwitz LI, Grady JN, Cohen DB, Lin Z, Volpe M, Ngo CK, Masica AL, Long T, Wang J, Keenan M, Montague J, Suter LG, Ross JS, Drye EE, Krumholz HM, Bernheim SM. Development and validation of an algorithm to identify planned readmissions from claims data. J Hosp Med. 2015;10(10):670–7. doi: 10.1002/jhm.2416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP): Clinical Classifications Software Refined (CCSR). www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp. Accessed June 24, 2021.
- 25.Moore BJ, White S, Washington R, Coenen N, Elixhauser A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: the AHRQ Elixhauser Comorbidity Index. Med Care. 2017;55(7):698–705. doi: 10.1097/MLR.0000000000000735. [DOI] [PubMed] [Google Scholar]
- 26.Kim DH, Glynn RJ, Avorn J, Lipsitz LA, Rockwood K, Pawar A, Schneeweiss S. Validation of a claims-based frailty index against physical performance and adverse health outcomes in the health and retirement study. J Gerontol A Biol Sci Med Sci. 2019;74(8):1271–1276. doi: 10.1093/gerona/gly197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim DH, Lee J, Kim CA, Huybrechts KF, Bateman BT, Patorno E, Marcantonio ER. Evaluation of algorithms to identify delirium in administrative claims and drug utilization database. Pharmacoepidemiol Drug Saf. 2017;26(8):945–953. doi: 10.1002/pds.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lahue SC, Douglas VC, Kuo T, Conell CA, Liu VX, Josephson SA, Angel C, Brooks KB. Association between inpatient delirium and hospital readmission in patients ≥ 65 years of age: a retrospective cohort study. J. Hosp. Med. 2019;4:201–206. doi: 10.12788/jhm.3130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gilbert T, Neuburger J, Kraindler J, Keeble E, Smith P, Ariti C, Arora S, Street A, Parker S, Roberts HC, Bardsley M, Conroy S. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet. 2018;391(10132):1775–1782. doi: 10.1016/S0140-6736(18)30668-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Werner RM, Coe NB, Qi M, Konetzka RT. Patient outcomes after hospital discharge to home with home health care vs to a skilled nursing facility. JAMA Intern Med. 2019;179(5):617–623. doi: 10.1001/jamainternmed.2018.7998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burke RE, Xu Y, Ritter AZ. Outcomes of post-acute care in skilled nursing facilities in Medicare beneficiaries with and without a diagnosis of dementia. J Am Geriatr Soc. 2021. 10.1111/jgs.17321. [DOI] [PubMed]
- 32.Daiello LA, Gardner R, Epstein-Lubow G, Butterfield K, Gravenstein S. Association of dementia with early rehospitalization among Medicare beneficiaries. Arch Gerontol Geriatr. 2014;59(1):162–8. doi: 10.1016/j.archger.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 33.Horwitz LI. Self-care after hospital discharge: knowledge is not enough. BMJ Qual Saf. 2017;26(1):7–8. doi: 10.1136/bmjqs-2015-005187. [DOI] [PubMed] [Google Scholar]
- 34.Horwitz LI, Moriarty JP, Chen C, Fogerty RL, Brewster UC, Kanade S, Ziaeian B, Jenq GY, Krumholz HM. Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med. 2013;173(18):1715–22. doi: 10.1001/jamainternmed.2013.9318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Greysen SR, Harrison JD, Kripalani S, Vasilevskis E, Robinson E, Metlay J, Schnipper JL, Meltzer D, Sehgal N, Ruhnke GW, Williams MV, Auerbach AD. Understanding patient-centred readmission factors: a multi-site, mixed-methods study. BMJ Qual Saf. 2017;26(1):33–41. doi: 10.1136/bmjqs-2015-004570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Epstein-Lubow G, Baier RR, Butterfield K, Gardner R, Babalola E, Coleman EA, Gravenstein S. Caregiver presence and patient completion of a transitional care intervention. Am J Manag Care. 2014;20(10):e349–444. [PubMed] [Google Scholar]
- 37.Hahn-Goldberg S, Jeffs L, Troup A, Kubba R, Okrainec K. "We are doing it together"; The integral role of caregivers in a patients’ transition home from the medicine unit. PLoS One. 2018;13(5):e0197831. doi: 10.1371/journal.pone.0197831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Auerbach AD, Kripalani S, Vasilevskis EE, Sehgal N, Lindenauer PK, Metlay JP, Fletcher G, Ruhnke GW, Flanders SA, Kim C, Williams MV, Thomas L, Giang V, Herzig SJ, Patel K, Boscardin WJ, Robinson EJ, Schnipper JL. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern Med. 2016;176(4):484–93. doi: 10.1001/jamainternmed.2015.7863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Amjad H, Carmichael D, Austin AM, Chang C, Bynum JPW. Continuity of care and health care utilization in older adults with dementia in fee-for-service medicare. JAMA Intern Med. 2016;176(9):1371–1378. doi: 10.1001/jamainternmed.2016.3553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kind AJ, Jencks S, Brock J, Yu M, Bartels C, Ehlenbach W, Greenberg C, Smith M. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161(11):765–74. doi: 10.7326/M13-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Powell WR, Buckingham WR, Larson JL, et al. Association of neighborhood-level disadvantage with alzheimer disease neuropathology. JAMA Netw Open. 2020;3(6):e207559. doi: 10.1001/jamanetworkopen.2020.7559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McCarthy EP, Ogarek JA, Loomer L, et al. Hospital transfer rates among US nursing home residents with advanced illness before and after initiatives to reduce hospitalizations. JAMA Intern Med. 2020;180(3):385–394. doi: 10.1001/jamainternmed.2019.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jennings LA, Turner M, Keebler C, Burton CH, Romero T, Wenger NS, Reuben DB. The effect of a comprehensive dementia care management program on end-of-life care. J Am Geriatr Soc. 2019;67(3):443–448. doi: 10.1111/jgs.15769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.National Academies of Sciences, Engineering, and Medicine. Meeting the challenge of caring for persons living with dementia and their care partners and caregivers: a way forward. Larson EB, Stroud C, eds. National Academies Press; 2021. [PubMed]
- 45.Bindman AB, Cox DF. Changes in health care costs and mortality associated with transitional care management services after a discharge among medicare beneficiaries. JAMA Intern Med. 2018;178(9):1165–1171. doi: 10.1001/jamainternmed.2018.2572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nuckols TK, Keeler E, Morton S, et al. Economic evaluation of quality improvement interventions designed to prevent hospital readmission: a systematic review and meta-analysis. JAMA Intern Med. 2017;177(7):975–985. doi: 10.1001/jamainternmed.2017.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lees Haggerty K, Epstein-Lubow G, Spragens LH, Stoeckle RJ, Evertson LC, Jennings LA, Reuben DB. Recommendations to improve payment policies for comprehensive dementia care. J Am Geriatr Soc. 2020;68(11):2478–2485. doi: 10.1111/jgs.16807. [DOI] [PubMed] [Google Scholar]
- 48.Burgdorf JG, Fabius CD, Riffin C, Wolff JL. Receipt of posthospitalization care training among medicare beneficiaries’ family caregivers. JAMA Netw Open. 2021;4(3):e211806. doi: 10.1001/jamanetworkopen.2021.1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lam K, Shi Y, Boscardin J, Covinsky KE. Unmet need for equipment to help with bathing and toileting among older US adults. JAMA Intern Med. 2021;181(5):662–670. doi: 10.1001/jamainternmed.2021.0204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Panagiotou OA, Kumar A, Gutman R, Keohane LM, Rivera-Hernandez M, Rahman M, Gozalo PL, Mor V, Trivedi AN. Hospital readmission rates in medicare advantage and traditional medicare: a retrospective population-based analysis. Ann Intern Med. 2019;171(2):99–106. doi: 10.7326/M18-1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nuti SV, Qin L, Rumsfeld JS, Ross JS, Masoudi FA, Normand SL, Murugiah K, Bernheim SM, Suter LG, Krumholz HM. Association of admission to veterans affairs hospitals vs non-veterans affairs hospitals with mortality and readmission rates among older men hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2016;315(6):582–92. doi: 10.1001/jama.2016.0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292(17):2115–2124. doi: 10.1001/jama.292.17.2115. [DOI] [PubMed] [Google Scholar]
- 53.Boyd CM, Landefeld CS, Counsell SR, Palmer RM, Fortinsky RH, Kresevic D, Burant C, Covinsky KE. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr Soc. 2008;56(12):2171–9. doi: 10.1111/j.1532-5415.2008.02023.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 43 kb)