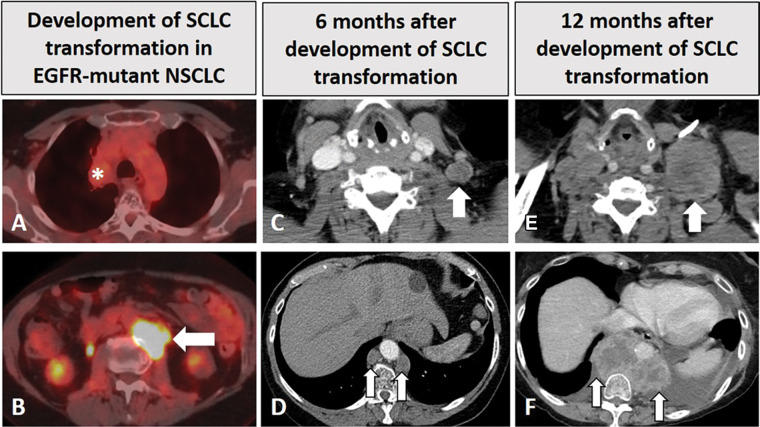
Figure 2:
Images in a 68-year-old woman with EGFR-mutant non–small cell lung cancer (NSCLC) with small cell transformation after epidermal growth facto receptor (EGFR) inhibitor therapy. (A, B) The patient was initially treated with EGFR inhibitor, osimertinib, for her NSCLC with sensitizing EGFR mutation (L858R) and responded well, with a treated non-fluorodeoxyglucose (FDG)–avid primary tumor in the right upper lobe (* in A), as shown on FDG PET/CT scan obtained 2 years after the initiation of osimertinib (A). However, on the same FDG PET/CT scan (B), a new FDG-avid paraspinal mass (arrow in B) was noted. The paraspinal mass demonstrated mixed features of EGFR L858R mutant non-SCLC and SCLC at histologic examination, demonstrating SCLC transformation due to acquired resistance to EGFR inhibitor. The patient was treated with carboplatin plus etoposide. (C, D) Contrast-enhanced chest CT scans obtained 6 months later show further progression, with enlarged left supraclavicular node (arrow in C) and paraspinal nodes (arrows in D). The patient was switched to paclitaxel therapy, while continuing osimertinib. (E, F) Contrast-enhanced CT scans obtained at 12 months demonstrate further progression, with significant further enlargement of the left supraclavicular node (arrow in E) and paraspinal nodes (arrows in F) with heterogeneous CT attenuation and the development of left pleural effusion.