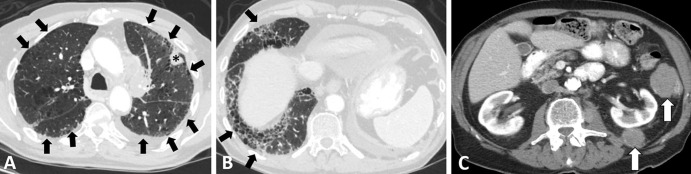
Figure 7:
Images in a 79-year-old man with extensive small cell lung cancer (SCLC) and underling fibrotic interstitial lung disease. The patient was a former smoker and presented with worsening cough and dyspnea on exertion. (A–C) Chest CT scans demonstrate a left upper lobe lesion (* in A) and peritoneal and retroperitoneal deposits (arrows in C) that were biopsied and showed metastatic SCLC. Notably, the clinical record indicated that the annual low-dose CT screening 6 months earlier was negative for cancer. Underlying lungs show fibrotic interstitial lung disease in peripheral and somewhat basilar distribution (arrows in A and B), accompanied by interlobular septal thickening, ground-glass and reticular opacities, traction bronchiectasis, and a few areas suggestive of early honeycombing. The patient was treated with several lines of systemic therapy, including carboplatin plus etoposide and nivolumab; however, he died 6 months after the diagnosis.