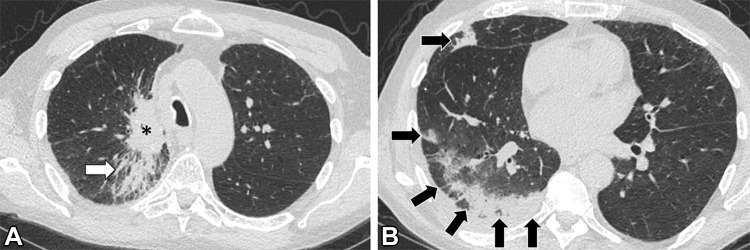
Figure 9:
Images in a 69-year-old man with extensive stage small cell lung cancer (SCLC) treated with first-line atezolizumab plus carboplatin and etoposide. The patient also has a remote history of tracheal squamous cell carcinoma, which had been treated with chemoradiotherapy. (A, B) Chest CT scans obtained 6 weeks after initiation of atezolizumab therapy demonstrate development of peripheral areas of consolidation in the right lung (arrows in B), indicative of immune checkpoint inhibitor–related pneumonitis with an organizing pneumonia pattern. A dominant lung mass from SCLC is noted in the right upper lobe (* in A), with underlying postradiation changes from prior radiation therapy to the tracheal tumor (arrow in A). The patient had increasing shortness of breath but no fever, and results of infectious work-up, including COVID-19, were negative. Atezolizumab was held and the patient was treated with oral corticosteroids.