Abstract
Background
The globalization of healthcare systems, and the aim to lower healthcare costs have all contributed to the growth of telehealth technology in recent years. However, before these systems are put into use, their efficacy should be verified. To the best of our knowledge, this is the first study focusing on the evaluation of functional exercise capacity using the 30-s sit-to-stand (30-s STS) test as a tele-assessment method in patients with type 2 diabetes mellitus (T2DM).
Aims
The purpose of the study is to investigate the level of agreement between tele-assessment and face-to-face assessment of 30-s STS test in patients with T2DM.
Methods
Fifty participants performed two times 30-s STS tests separated by 1 h: a face-to-face and an Internet-connected video call examination (tele-assessment). Two physiotherapists conduct these evaluations; each was blinded to the other. The order of the evaluations was designated at random for each participant and physiotherapist.
Results
There was a good level of agreement between tele-assessment and face-to-face assessment of the 30-s STS test (mean differences = 0.20 ± 0.88, limits of agreement = 1.93 to − 1.53). Excellent interrater reliability was found for scores of the 30-s STS test [ICC = 0.93 (95% CI: 0.88; 0.96)]. In addition, all before and after test parameters show that there was a very good interrater reliability (ρ ≥ 0.75).
Conclusions
This study shows a good level of agreement between tele-assessment and face-to-face assessment of the 30-s STS test. Our study’s findings indicate that tele-assessment is a potential application to determine the level of physical capacity remotely in patients with T2DM.
Keywords: Physical assessment, Tele-assessment, Telehealth, Type 2 diabetes, 30-s sit-to-stand
Introduction
Type 2 diabetes mellitus (T2DM) is caused by hyperglycemia brought on by reduced insulin synthesis, impaired insulin utilization, or both, with symptoms such as thirst, polyuria, and weight loss [1]. Because of the high prevalence and high medical costs worldwide, research is continuing in both the diagnosis and treatment of the disease and important developments are being experienced [2]. Maintaining sufficient glycemic control and lowering cardiovascular risk factors is part of the therapy of T2DM, along with the treatment of complications and related comorbidities [3]. Many systemic complications such as cardiovascular, cognitive, psychological, and neuropathy can occur in T2DM [4]. One of the keys to the management of the disease is maintaining a healthy lifestyle that includes maintaining a healthy weight, eating a balanced diet, quitting smoking, and engaging in physical activity [5].
Glycemic control is enhanced by physical activity, which reduces the risk of cardiovascular disease and also reduces mortality [6]. However, patients with T2DM often do not have adequate physical activity habits that may help glycemic balance [6–8]. Physical activity has psychological benefits as well as physical benefits and reduces depressive symptoms [9, 10]. Therefore, the physical conditions of T2DM patients need to be assessed to recommend individualized exercise programs and follow up on their progression by health professionals [7]. However, few studies have investigated the reliability of the 30-s sit-to-stand (30-s STS) test for assessing functional exercise capacity in the T2DM population [11, 12].
The 30-s STS test involves standing up and sitting down from a regular chair as many times as a person can in 30 s, and its validity and reliability have been proven in patients with T2DM [11, 12]. It is commonly used to assess physical performance in the lower extremities and to provide insight into functional exercise capacity [13–15]. The 30-s STS test has many advantages in that the materials required to perform this test are widely used, easy to use, and inexpensive. It also does not require professional personnel to perform the test. The test is very fast as it requires no more than 1 min per assessment. It is also a type of test used in many studies without a ground effect [16].
Nowadays, new options for clinical evaluation are provided by information and communication technology. In particular, it can benefit from Internet-based systems for the evaluation and follow-up of patients with chronic diseases who reside in distant places or lose their independence. Thus, accessibility to health services increases and the economic burden of the disease decreases [17]. However, scientific evidence is needed before recommending their use. Instead of traditional face-to-face evaluation, tele-assessment methods can be used with video conferencing method with any device with a camera, screen, microphone, speaker, and Internet access. To the best of our knowledge, there is no previous study focusing on the evaluation of the functional exercise capacity of individuals with T2DM as a tele-assessment method has been found. The aim of this study is to investigate the level of agreement between tele-assessment and face-to-face assessment of the 30-s STS test in patients with T2DM.
Methods
Study design and participants
The interrater reliability was tested using a descriptive crossover design. T2DM patients, who consult the Internal Medicine Department of Health Sciences University—İzmir Bozyaka Training and Research Hospital, for routine outpatient follow-up and were diagnosed by an internal diseases specialist were included in this study. Inclusion criteria were having been diagnosed with T2DM by an internal diseases specialist (or endocrinologist), being able to walk independently, having a smartphone and the ability to use it, and having a pulse oximeter device (for O2 saturation measurement) and a blood pressure monitor. Exclusion criteria were having a health problem (orthopedic, neurological, internal, or cardiorespiratory) that prevents standing/walking; acute inflammation; intestinal tumor; cognitive impairment; vision and hearing loss; and/or an orthopedic, vascular, neurological, or psychiatric problem affecting balance.
Assessment procedure
The 30-s STS test was taught once when participants came for the routine control appointment. Participants’ demographic and clinic details (age, gender, educational status, height, body weight, and comorbidities) were recorded after receiving consent for the study. Participants perform two physical tests: a traditional in-person examination (face-to-face) and an Internet-connected video call examination (tele-assessment). Two physiotherapists with an experience of more than 7 years did these evaluations; one physiotherapist always performed the face-to-face assessment while the other always performed the tele-assessment, and each was blinded to the other. The two evaluations were separated by 20 min, and to counterbalance any testing order effects, the order of the evaluations was designated at random for each participant and physiotherapist [18].
Thirty-second STS tests were conducted under the same time frame from 11.00 am to 3.00 pm, Monday to Friday. Participants were informed not to do any vigorous physical activities 3 h before testing and to continue taking their prescription medications. The 30-s STS is a test consisting of getting up from a standard chair (with 45–47 cm seat height) and sitting down, and the participants were instructed to rise up straight and sit down again as many times as they could in 30 s starting from the seated position [13–15].
A smartphone with a built-in microphone and camera and high-speed Internet were used for the tele-assessment. Using the WhatsApp application (WhatsApp Inc., Mountain View, CA), a live video communication was kept running between the patient and the therapist. WhatsApp is an application that has been used frequently in recent years with the coronavirus pandemic and is a promising application as a communication tool between healthcare professionals and patients [19]. When the patient was performed to tele-assessment, he was required to position the smartphone so that all his/her limbs were visible from the camera.
Before and after the tests, dyspnea perception and lower limb fatigue were questioned according to the 10-grade modified Borg scale [20], and peripheral oxygen saturation (SpO2), systolic/diastolic blood pressure, and heart rate were measured and recorded. While the perception of dyspnea and fatigue was questioned in the tele-assessment, oxygen saturation and blood pressure measurements were obtained by the patient by self-measurement. The patient’s devices were used in both tele-assessment and face-to-face assessment to eliminate measurement tool differences.
Statistical analysis
On the recommendation of the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN), a total sample size of 50 participants was selected [21]. The Bland–Altman limits of agreement test were used to investigate the agreement between tele-assessment and face-to-face assessment methods for the 30-s STS test. Additionally, two-way random effect intraclass correlation coefficients (ICC) (ρ) and confidence intervals of the parameters were calculated for the interrater reliability analysis. SPSS Version 21 for Windows (SPSS Inc., Chicago, IL) was used to perform all of the statistical analysis, with a 0.05 α value. The ICC was considered excellent (≥ 0.75), fair to good (0.4–0.75), or poor (≤ 0.4) [22].
Results
Fifty-eight of the patients were assessed for eligibility to participate in the study. Four did not meet the inclusion criteria and four did not join in some of the assessment stages. The study was completed with a total of 50 patients (Fig. 1).
Fig. 1.
Recruitment flowchart
The mean + SD age and BMI of patients were 54.5 ± 6.3 years and 28.8 ± 3.5 kg/m2, respectively. Sixty-two percent of the patients were male and 38% female. Table 1 presents the descriptive characteristics of patients.
Table 1.
Descriptive characteristics of patients
| Parameters | Mean ± SD |
|---|---|
| Gender (% male/female) | 62.0/38.0 |
| Age (years) | 54.5 ± 6.3 |
| BMI (kg/m2) | 28.8 ± 3.5 |
| Educational status, n (%) | |
| Primary school | 3 (6.0) |
| Secondary school | 33 (66.0) |
| High school | 2 (4.0) |
| University | 10 (20.0) |
| Postgraduate | 2 (4.0) |
| 30-s sit-to-stand test score (face-to-face) | 12.4 ± 1.83 |
| 30-s sit-to-stand test score (tele-assessment) | 12.2 ± 1.62 |
| Comorbidity, n (%) | |
| HT | 25 (50.0) |
| COPD | 2 (4.0) |
| CAD | 6 (12.0) |
| HF | 0 |
SD Standart Deviation, BMI Body Mass Index, HT Hypertension, COPD Chronic Obstructive Pulmonary Disease, CAD Coronary Artery Disease, HF Heart Failure
In Fig. 2, the Bland–Altman plot illustrated a good level of agreement between tele-assessment and face-to-face assessment for the 30-s STS, with no evidence of systematic bias. The mean of the differences was 0.20 ± 0.88. The limits of agreement were 1.93 and − 1.53, respectively. Excellent interrater reliability was found for scores of the 30-s STS test [ICC = 0.93 (95% CI: 0.88; 0.96)] (Table 2).
Fig. 2.
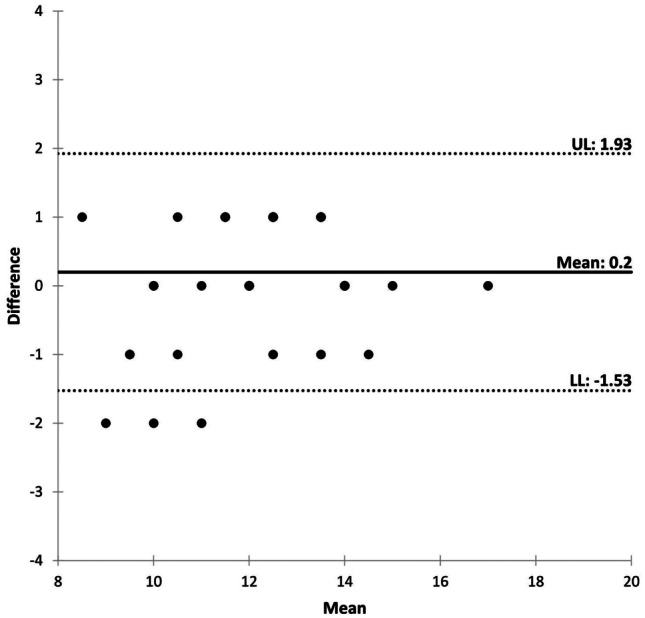
Bland–Altman plot of the difference between tele-assessment and face-to-face assessment for the 30-s sit-to-stand test. The Y axis shows the difference between the two paired measurements and the X axis represents the average of these measures. The solid line represents the mean difference between the face-to-face and tele-assessment. Dotted lines are the upper and lower limits of agreement (UL and LL, respectively)
Table 2.
Interrater reliability between tele-assessment and face-to-face assessment of 30-s sit-to-stand test parameters
| Mean difference between assessments (95% CI) |
Interrater reliability ICC (95% CI) |
|
|---|---|---|
| 30-s sit-to-stand test score (repetitions) | 0.20 (− 0.05, 0.45) | 0.93 (0.88, 0.96) |
| Resting dyspnea (mBorg) | 0.14 (0.03, 0.26) | 0.92 (0.85, 0.95) |
| Resting lower limb fatigue (mBorg) | 0.14 (− 0.001, 0.28) | 0.85 (0.74, 0.92) |
| Resting heart rate (bpm) | 0.66 (− 0.62, 1.94) | 0.75 (0.56, 0.86) |
| Resting systolic blood pressure (mmHg) | 2.16 (− 1.30, 5.62) | 0.89 (0.81, 0.94) |
| Resting diastolic blood pressure (mmHg) | 1.12 (− 1,24, 3.48) | 0.80 (0.64, 0.88) |
| Resting SpO2 (%) | − 0.12 (− 0.36, 0.12) | 0.79 (0.63, 0.88) |
| End-dyspnea (mBorg) | 0.06 (− 0.12, 0.24) | 0.85 (0.74, 0.92) |
| End-lower limb fatigue (mBorg) | 0.04 (− 0.14, .022) | 0.86 (0.76, 0.92) |
| End-heart rate (bpm) | 2.06 (0.68, 3.43) | 0.76 (0.57, 0.86) |
| End-systolic blood pressure (mmHg) | 2.16 (− 1.30, 5.62) | 0.84 (0.72, 0.91) |
| End-diastolic blood pressure (mmHg) | 0.12 (− 1.80, 2.04) | 0.88 (0.79, 0.93) |
| End-SpO2 (%) | − 0.04 (− 0.28, 0.20) | 0.75 (0.57, 0.86) |
CI Confidence Interval, ICC Intraclass Correlation Coefficient, SpO2 Peripheral Oxygen Saturation, mBorg Modified Borg Score
In Table 2, the mean differences between tele-assessment and face-to-face assessment for the 30-s STS parameters and the interrater reliability values are shown. Interrater reliability was deemed “acceptable” if the score was ≥ 0.75 [22]. All parameters show that there was a very good interrater reliability (ρ ≥ 0.75). Additionally, most of the 95% CI were narrow.
Discussion
The main finding of this study is that the 30-s STS test tele-assessment can be successfully used to assess functional exercise capacity in patients with T2DM. Our results show that there is high interrater reliability between tele-assessment and the face-to-face test methods.
The COVID-19 epidemic, the globalization of healthcare systems, and the aim to lower healthcare costs have all contributed to the growth of telehealth technology in recent years [18, 23]. However, before these systems are put into use, their efficacy should be verified against that of the more traditional health systems. Technological developments in the last decade have increased telehealth opportunities and provided greater flexibility in accessing health services [24]. In this study, we used the WhatsApp application, which can be used freely just that it needed an Internet-connected smartphone or tablet, for performing tele-assessment. WhatsApp is seen as a simple, inexpensive, and effective communication tool in the clinical health sector and its use will increase [25]. The security policy of WhatsApp is one of the important issues for its potential widespread usage in patient evaluation. WhatsApp uses end-to-end encryption for its services. It means that data and calls/video calls are encrypted and secured against third parties and wrong hands, even WhatsApp developers and authorities [26].
The 30-s STS test is often used for the evaluation of physical performance in adults because it is a simple and easy-to-use test [27]. The Centers for Disease Control recommend it as one of the tests for fall-risk screening [15]. The first reliability findings of the 30-s STS test were shown by the authors who developed it [28]. They found a high ICC for men and an excellent ICC for women. The 30-s STS reliability has been investigated in various populations. It was found an excellent ICC for people with total hip arthroplasty [29], a high ICC for people with dementia [30], excellent results in people who suffered a stroke [31], and an excellent ICC for people with multiple sclerosis [32]. To the best of our knowledge, only two studies researched on the reliability of the 30-s STS test in people with T2DM [11, 12]. Relative reliability for the 30-s STS test was excellent in both studies (for both, ICC > 0.90). In addition, Ogawa et al. [33] examined the reliability of virtual physical performance assessments in a group consisting of various diseases, and in this study, they found an excellent ICC for the 30-s STS test performed remotely. However, we think that there is a heterogeneous population in the mentioned study and that patients’ self-reporting of the diagnosis was a weakness of the study. In our study, we investigated the level of agreement between tele-assessment and face-to-face assessment of the 30-s STS test in patients physician-diagnosed with T2DM. We found excellent interrater reliability (ICC = 0.93) for the 30-s STS test of T2DM patients.
When tele-assessment studies are investigated, it is shown that different methods are used in various groups [34–37]. In a systematic review, it was shown that the evaluation of some functional and neurodynamic tests with the tele-assessment method is applicable [35]. In a recent study, Güngör et al. [34] showed that functional and core strength-endurance tests assessed using the tele-assessment approach were valid and practicable for assessing the capabilities of healthy young adults. Another recent review emphasized the fact that while tele-assessments are useful for monitoring the progression of neuromuscular illnesses, they still require improvement [38]. In our study, we showed that the 30-s STS test tele-assessment method used in the measurement of functional capacity in patients with type 2 diabetic patients is easy to use, applicable, and reliable.
The validity of the measurement of the vital signs before and after the test are crucial outcomes for the tele-assessment procedure. Kagiyama et al. [39] investigated the feasibility and validity of a tele-assessment in which healthcare providers monitor vital signs remotely. They demonstrated that telemedicine-based self-assessment of vital signs was feasible and reliable; additionally, it is a useful alternative to traditional face-to-face vital sign measurements. In their study, the agreement between tele-assessment and face-to-face assessment was excellent for all parameters. The ICC for systolic (0.92), diastolic blood pressure (0.86), heart rate (0.89), and SpO2 (0.92) were statistically significant [39]. In our study, we also found excellent agreement between tele-assessment and face-to-face assessment for vital signs both before and after the tests.
Strengths and limitations
Being the first study examining the interrater reliability, validity, and feasibility of a 30-s STS tele-assessment test in patients with T2DM, and having a sufficient sample according to COSMIN [21], can be listed as the strengths of our study. We have some limitations in our study. Our study was limited to T2DM who are more familiar with the Internet and be able to use technology. Therefore, we cannot generalize the findings of the study to all T2DM patients. Future research should assess the effectiveness of a complementing home-based treatment centered on functional capacity tele-assessment methods with a minimal clinical difference in light of our findings.
Conclusions
This study shows a good level of agreement between tele-assessment and face-to-face assessment for the 30-s STS test. Additionally, the 30-s STS test tele-assessment to assess functional exercise capacity in patients with T2DM was found to have high interrater reliability. The study’s findings indicate that tele-assessment is a potential application to conduct physical evaluations remotely.
Author contribution
All authors contributed to the study conception and design. Material preparation: Rıdvan Aktan, Hayriye Yılmaz, and İsmail Demir. Data collection: Rıdvan Aktan and Hayriye Yılmaz. Analysis of data: Rıdvan Aktan and Sevgi Özalevli. The first draft of the manuscript was written by Rıdvan Aktan and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Data availability
On request.
Code availability
Not applicable.
Declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the local Ethical Committee of the Health Sciences University Izmir Bozyaka Training and Research Hospital with approval number 2022–33 on 23/02/2022, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.American Diabetes Association. Summary of Revisions: Standards of Medical Care in Diabetes (2021) Diabetes Care 44 (Suppl 1):S4-S6. 10.2337/dc21-Srev [DOI] [PubMed]
- 2.Ogurtsova K, da Rocha Fernandes JD, Huang Y, et al. IDF Diabetes Atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50. doi: 10.1016/j.diabres.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 3.Reyes-García R, Moreno-Pérez Ó, Tejera-Pérez C, et al. Document on a comprehensive approach to type 2 diabetes mellitus. Endocrinol Diabetes Nutr (Engl Ed) 2019;66:443–458. doi: 10.1016/j.endinu.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 4.Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15 (7):539–553. 10.1002/(SICI)1096-9136(199807)15:73.0.CO;2-S [DOI] [PubMed]
- 5.Diabetes Association Of The Republic Of China (Taiwan) (2020) Executive summary of the DAROC clinical practice guidelines for diabetes care- 2018. J Formos Med Assoc 119:577–586. 10.1016/j.jfma.2019.02.016 [DOI] [PubMed]
- 6.Hamasaki H. Daily physical activity and type 2 diabetes: a review. World J Diabetes. 2016;7:243–251. doi: 10.4239/wjd.v7.i12.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duclos M, Oppert JM, Verges B, et al. Physical activity and type 2 diabetes. Recommandations of the SFD (Francophone Diabetes Society) diabetes and physical activity working group. Diabetes Metab. 2013;39:205–216. doi: 10.1016/j.diabet.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 8.López Sánchez GF, Smith L, Raman R, et al. Physical activity behaviour in people with diabetes residing in India: a cross-sectional analysis. Sci Sports. 2019;34(1):e59–e66. doi: 10.1016/j.scispo.2018.08.005. [DOI] [Google Scholar]
- 9.Schram MT, Baan CA, Pouwer F. Depression and quality of life in patients with diabetes: a systematic review from the European depression in diabetes (EDID) research consortium. Curr Diabetes Rev. 2009;5:112–119. doi: 10.2174/157339909788166828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Narita Z, Inagawa T, Stickley A, et al. Physical activity for diabetes-related depression: a systematic review and meta-analysis. J Psychiatr Res. 2019;113:100–107. doi: 10.1016/j.jpsychires.2019.03.014. [DOI] [PubMed] [Google Scholar]
- 11.Alfonso-Rosa RM, Del Pozo-Cruz B, Del Pozo-Cruz J, et al. Test-retest reliability and minimal detectable change scores for fitness assessment in older adults with type 2 diabetes. Rehabil Nurs. 2014;39:260–268. doi: 10.1002/rnj.111. [DOI] [PubMed] [Google Scholar]
- 12.Barrios-Fernández S, Pérez-Gómez J, Galán-Arroyo MDC, et al. Reliability of 30-s Chair Stand Test with and without cognitive task in people with type-2 diabetes mellitus. Int J Environ Res Public Health. 2020;17:1450. doi: 10.3390/ijerph17041450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Millor N, Lecumberri P, Gómez M, et al. An evaluation of the 30-s chair stand test in older adults: frailty detection based on kinematic parameters from a single inertial unit. J Neuroeng Rehabil. 2013;10:86. doi: 10.1186/1743-0003-10-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pinheiro PA, Carneiro JAO, Coqueiro RS, et al. “Chair stand testˮ as simple tool for sarcopenia screening in elderly women. J Nutr Health Aging. 2016;20:56–59. doi: 10.1007/s12603-016-0676-3. [DOI] [PubMed] [Google Scholar]
- 15.Chow RB, Lee A, Kane BG, et al. Effectiveness of the “Timed Up and Go” (TUG) and the Chair test as screening tools for geriatric fall risk assessment in the ED. Am J Emerg Med. 2019;37:457–460. doi: 10.1016/j.ajem.2018.06.015. [DOI] [PubMed] [Google Scholar]
- 16.Domínguez-Muñoz FJ, Carlos-Vivas J, Villafaina S, et al. Association between 30-s Chair Stand-Up Test and anthropometric values, vibration perception threshold, FHSQ, and 15-D in patients with type 2 diabetes mellitus. Biology (Basel) 2021;10:246. doi: 10.3390/biology10030246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bernard M-M, Janson F, Flora PK, et al. Videoconference-based physiotherapy and tele-assessment for homebound older adults: a pilot study. Act Adapt Aging. 2009;33:39–48. doi: 10.1080/01924780902718608. [DOI] [Google Scholar]
- 18.Cabrera-Martos I, Ortiz-Rubio A, Torres-Sánchez I, et al. Agreement between face-to-face and tele-assessment of upper limb functioning in patients with Parkinson disease. PM R. 2019;11:590–596. doi: 10.1002/pmrj.12001. [DOI] [PubMed] [Google Scholar]
- 19.Giordano V, Koch H, Godoy-Santos A, et al. WhatsApp messenger as an adjunctive tool for telemedicine: an overview. Interact J Med Res. 2017;6:e11. doi: 10.2196/ijmr.6214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wilson RC, Jones P. A comparison of the visual analogue scale and modified Borg scale for the measurement of dyspnoea during exercise. Clin Sci. 1989;76:277–282. doi: 10.1042/cs0760277. [DOI] [PubMed] [Google Scholar]
- 21.Mokkink LB, Terwee CB, Knol DL, et al. The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: a clarification of its content. BMC Med Res Methodol. 2010;10:22. doi: 10.1186/1471-2288-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fleiss JL. Design and analysis of clinical experiments. John Wiley & Sons; 2011. [Google Scholar]
- 23.Heredia-Ciuró A, Lazo-Prados A, Blasco-Valls P et al (2022) Agreement between face-to-face and tele-assessment of upper limb disability in lung cancer survivors during COVID-19 era. J Telemed Telecare 1357633x221079543. 10.1177/1357633x221079543 [DOI] [PMC free article] [PubMed]
- 24.Car J, Tan WS, Huang Z, et al. eHealth in the future of medications management: personalisation, monitoring and adherence. BMC Med. 2017;15:73. doi: 10.1186/s12916-017-0838-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mars M, Scott RE. WhatsApp in clinical practice: a literature review. Stud Health Technol Inform. 2016;231:82–90. [PubMed] [Google Scholar]
- 26.WhatsApp LLC (2021) Privacy policy. https://www.whatsapp.com/legal/privacy-policy/?lang=en. Accessed 01 Sept 2022
- 27.Collado-Mateo D, Madeira P, Dominguez-Muñoz FJ, et al. The automatic assessment of strength and mobility in older adults: a test-retest reliability study. Medicina (Kaunas) 2019;55:270. doi: 10.3390/medicina55060270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rikli RE, Jones CJ (2001) Senior fitness test manual. Human Kinetics
- 29.Unver B, Kahraman T, Kalkan S, et al. Test-retest reliability of the 50-foot timed walk and 30-second chair stand test in patients with total hip arthroplasty. Acta Orthop Belg. 2015;81:435–441. [PubMed] [Google Scholar]
- 30.Blankevoort CG, van Heuvelen MJ, Scherder EJ. Reliability of six physical performance tests in older people with dementia. Phys Ther. 2013;93:69–78. doi: 10.2522/ptj.20110164. [DOI] [PubMed] [Google Scholar]
- 31.Lyders Johansen K, Derby Stistrup R, Skibdal Schjøtt C, et al. Absolute and relative reliability of the Timed ‘Up & Go’ Test and ‘30second Chair-Stand’ Test in hospitalised patients with stroke. PLoS ONE. 2016;11:e0165663. doi: 10.1371/journal.pone.0165663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Özkeskin M, Özden F, Ar E et al (2022) The reliability and validity of the 30-second chair stand test and modified four square step test in persons with multiple sclerosis. Physiother Theory Pract 1–7. 10.1080/09593985.2022.2070811 [DOI] [PubMed]
- 33.Ogawa EF, Harris R, Dufour AB, et al. Reliability of virtual physical performance assessments in veterans during the COVID-19 pandemic. Arch Rehabil Res Clin Transl. 2021;3:100146. doi: 10.1016/j.arrct.2021.100146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Güngör F, Ovacık U, Ertan Harputlu Ö et al (2022) Tele-assessment of core performance and functional capacity: reliability, validity, and feasibility in healthy individuals. J Telemed Telecare 1357633x221117335. 10.1177/1357633x221117335 [DOI] [PubMed]
- 35.Mani S, Sharma S, Omar B, et al. Validity and reliability of Internet-based physiotherapy assessment for musculoskeletal disorders: a systematic review. J Telemed Telecare. 2017;23:379–391. doi: 10.1177/1357633x16642369. [DOI] [PubMed] [Google Scholar]
- 36.Palacín-Marín F, Esteban-Moreno B, Olea N, et al. Agreement between telerehabilitation and face-to-face clinical outcome assessments for low back pain in primary care. Spine (Phila Pa 1976) 2013;38:947–952. doi: 10.1097/BRS.0b013e318281a36c. [DOI] [PubMed] [Google Scholar]
- 37.Mani S, Sharma S, Singh DK. Concurrent validity and reliability of telerehabilitation-based physiotherapy assessment of cervical spine in adults with non-specific neck pain. J Telemed Telecare. 2021;27:88–97. doi: 10.1177/1357633x19861802. [DOI] [PubMed] [Google Scholar]
- 38.Spina E, Trojsi F, Tozza S, et al. How to manage with telemedicine people with neuromuscular diseases? Neurol Sci. 2021;42:3553–3559. doi: 10.1007/s10072-021-05396-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kagiyama N, Hiki M, Matsue Y et al (2021) Validation of telemedicine-based self-assessment of vital signs for patients with COVID-19: a pilot study. J Telemed Telecare 1357633X211011825. 10.1177/1357633x211011825 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
On request.
Not applicable.


