Video
Combination of argon plasma coagulation prior to suturing for endoscopic gastroplasty as revisional and primary intervention method, respectively.
Abbreviations: %TBWL, percentage of total body weight loss; APC, argon plasma coagulation; ESG, endoscopic sleeve gastroplasty; OCG, oscillating circles gastroplasty
Background
Endoscopic bariatric therapies provide an effective and minimally invasive approach to obesity that augments the available treatment options beyond surgery, medication, and lifestyle modifications. Endoscopic sleeve gastroplasty (ESG) provides transoral endoscopic gastric volume reduction resulting in a sleeve-like anatomy similar to, but not identical to, that of sleeve gastrectomy. ESG uses full-thickness endoscopic suturing (OverStitch; Apollo Endosurgery, Austin, Tex, USA) to approximate the mucosal surfaces for creation of gastroplasty,1 thus relying on the suture stability to maintain the integrity of the plications. Endoscopic sleeve gastroplasty integrity correlates with better weight loss outcomes over time.2 The expected mean percentage of total body weight loss (TBWL) following ESG is 13.7% ± 6.8%, 15.0% ± 7.7%, and 14.8% ± 8.5% at 6, 12, and 18 months, respectively.3 However, several reports demonstrate evidence of suture dehiscence between 8 months and 2 years after ESG, regardless of the suturing technique, suturing pattern, or number of sutures used.4
Evolving techniques have focused on approximating the submucosal surfaces,5,6 thus relying on the wound healing cascade events of re-epithelization and formation of well-vascularized collagen for enhanced durability of gastroplasty. However, these techniques may be technically challenging, add significant procedural time, and have additional costs. One of these techniques is the oscillating circles gastroplasty (OCG) technique, which uses EMR with band-ligation (Duette; Cook Medical, Limerick, Ireland) and endoscopic suturing (OverStitch; Apollo Endosurgery). The incorporation of the OCG technique adds a mean ± standard deviation of 12 ± 8 minutes to the ESG procedure time, which averages around 65 minutes in our institution.
Argon plasma coagulation (APC) is a common technique used in gastrointestinal endoscopy to induce intentional submucosal tissue injury by thermal ablation of mucosal surfaces.7 The combination of APC prior to endoscopic suturing potentially enhances the durability of the ESG by inducing more fibrosis in the stomach. An example of this application is the transoral outlet reduction procedure, which uses APC in addition to endoscopic suturing.8 To date, one case report of a patient who had undergone ESG with APC prior to suturing has been published. Itani et al9 report promising weight loss results at 6 months’ follow-up (14.5% total weight loss), and a follow-up endoscopy at 6 months revealed enhanced fibrosis along the plications. In this video, we describe the use of APC prior to suturing in revisional and primary ESG, respectively (Video 1, available online at www.giejournal.org).
Case Presentation
A 60-year-old woman with obesity class III (weight: 123 kg, body mass index: 44.9 kg/m2) and history of multiple comorbidities as well as history of abdominal surgeries presented for weight regain of 22 kg from nadir weight post–sleeve gastrectomy 4 years ago. CT imaging of the abdomen and pelvis showed antral dilation of the stomach. Because of her poor surgical candidacy, we opted to perform revisional endoscopic sleeve gastroplasty.
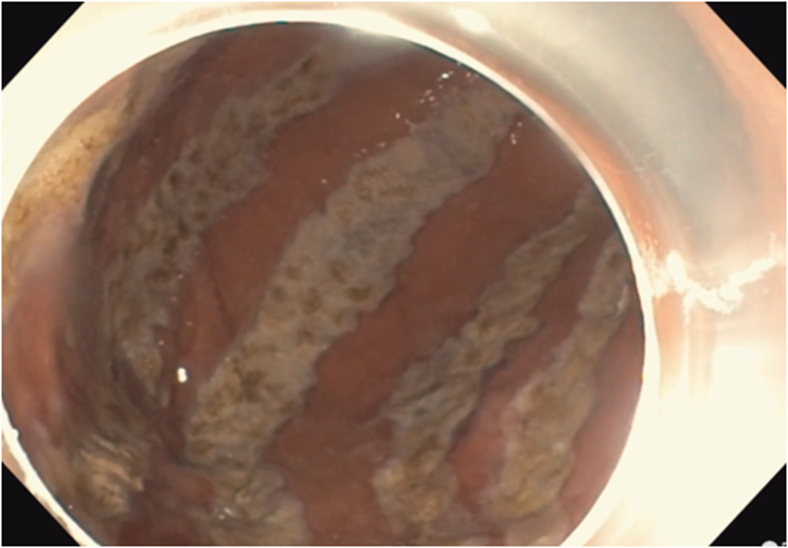
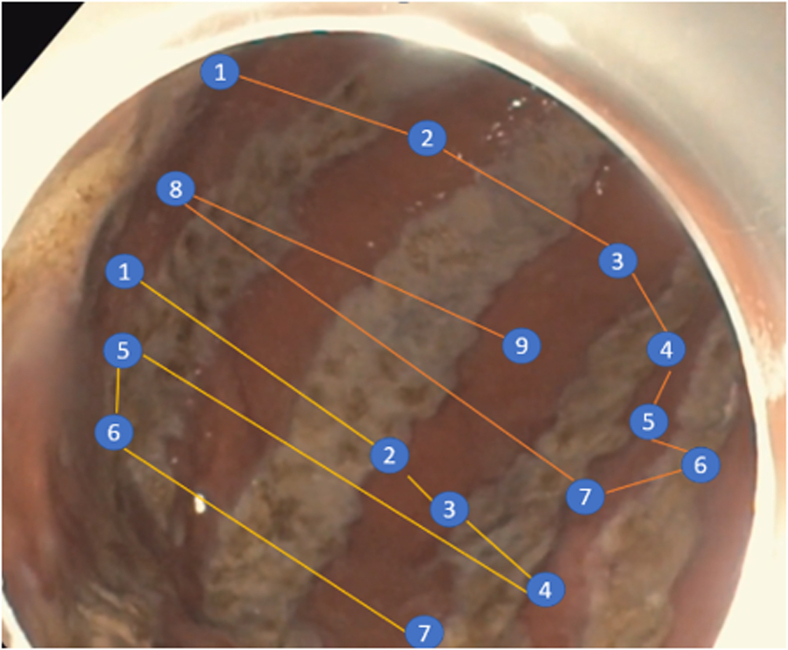
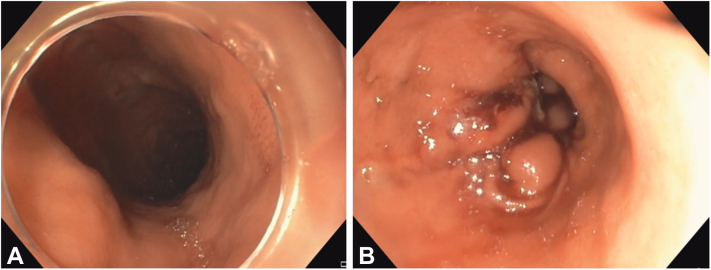
The procedure was performed in an operating room with the patient under general anesthesia with orotracheal intubation. The patient was placed in the left lateral decubitus position, with administration of prophylactic antibiotic (levofloxacin). A diagnostic endoscopy was performed before the procedure for any contraindications of ESG using a double-channel endoscope, Olympus CV 190 (Olympus Medical Systems Corp, Tokyo, Japan), and insufflation with carbon dioxide. The anti-emetic ondansetron was used intra-procedurally. On upper endoscopy, the distal sleeve starting at the level of incisura and antrum was significantly dilated and capacious with a volume of about 600 cc. Thermal ablation using APC at a setting of 60 watts and 1-L flow per minute was used to ablate mucosal surfaces. A total of 6 bands were created (Fig. 1). A full-thickness endoscopic suturing device was then used to approximate the ablated mucosal surfaces and retighten the dilated distal sleeve and antrum. The suturing sequence involved 2 O-shaped sutures at the level of the antrum (Fig. 2). Three additional reinforcing sutures were placed approximate. The final result showed a restricted tubular stomach from the gastroesophageal junction to the distal antrum terminating approximately 3 cm from the pylorus (Fig. 3). The procedure time for APC was 9 minutes. The total procedure time from scope-in to scope-out was 55 minutes. No procedural adverse events occurred. The patient reported no pain (pain score 0 on a scale of 0 to 10) after the procedure.
Figure 1.
Endoscopic view showing argon plasma coagulation markings on anterior wall, greater curvature, and posterior wall.
Figure 2.
O-shaped suture pattern in the revisional endoscopic sleeve gastroplasty.
Figure 3.
Endoscopic view showing the antrum of stomach before (A) and after (B) revisonal endoscopic sleeve gastroplasty.
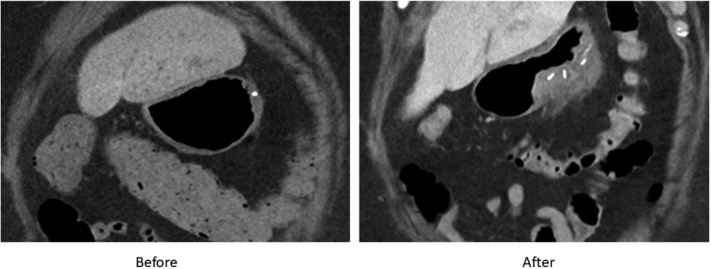
The patient did not use any weight loss over-the-counter products or prescriptions after the procedure. She was placed on dietary modifications and standard moderate intensity lifestyle interventions. A follow-up CT imaging of the abdomen showed successful antral reduction (Fig. 4). A follow-up endoscopy 2 months later showed a normal tubular stomach with intact sutures. In addition, the patient’s weight at 2 months’ follow-up was 115 kg, and percentage of TBWL (%TBWL) was 6.5%. No adverse events were reported.
Figure 4.
CT imaging of the abdomen before and after antral reduction.
In the second case, we describe the same technique for primary ESG in a 59-year-old woman with obesity class III (weight: 96.9 kg, body mass index: 40.4 kg/m2) and multiple comorbidities. Similarly, the procedure was performed in an operating room with the patient under general anesthesia with orotracheal intubation. The patient was placed in the left lateral decubitus position, with administration of prophylactic antibiotics (levofloxacin). A diagnostic endoscopy was performed before the procedure for any contraindications of ESG using a double-channel endoscope, Olympus CV 190 (Olympus Medical Systems Corp), and insufflation with carbon dioxide. The anti-emetic ondansetron was used intra-procedurally. Thermal ablation using APC at a setting of 60 watts and 1-L flow per minute was followed by endoscopic suturing to approximate the ablated mucosal surfaces. The suturing sequence involved 2 O-shaped sutures at the level of the distal stomach followed by 4 additional reinforcing sutures. The final result showed a restricted tubular stomach from the gastroesophageal junction to the distal antrum terminating approximately 3 cm from the pylorus. The total procedure time from scope-in to scope-out was 65 minutes. The procedure time for APC was 13 minutes. The patient reported no pain (pain score 0 on a scale of 0 to 10) after the procedure. The patient did not use any weight loss over-the-counter products or prescriptions after the procedure. She was placed on dietary modifications and standard moderate intensity lifestyle interventions. At 2 months’ follow-up, the patient’s weight was 90.9 kg and %TBWL was 6.1%. No adverse events were reported.
Conclusion
The combination of APC with endoscopic suturing in an ESG procedure is a readily available and reproducible technique that provides promising weight loss effects without adding any significant procedural time. However, further investigations with a larger cohort size and a longer follow-up period would be needed to establish weight loss effects and suture durability before widely adopting in endoscopic sleeve gastroplasties.
Disclosure
Dr Abu Dayyeh is a consultant for Endogenex, Endo-TAGSS, Metamodix, and BFKW; is a consultant for and receives grant/research support from USGI, Cairn Diagnostics, Aspire Bariatrics, and Boston Scientific; has speaker roles with Olympus and Johnson and Johnson; is a speaker for and receives grant/research support from Medtronic and EndoGastric Solutions; and receives research support from Apollo Endosurgery and Spatz Medical. All other authors disclosed no financial relationships.
Footnotes
Ethical Approval
Ethical approval has been waived by the Mayo Institution Board Review.
Supplementary data
Combination of argon plasma coagulation prior to suturing for endoscopic gastroplasty as revisional and primary intervention method, respectively.
References
- 1.Dayyeh B.K.A., Rajan E., Gostout C.J. Endoscopic sleeve gastroplasty: a potential endoscopic alternative to surgical sleeve gastrectomy for treatment of obesity. Gastrointest Endosc. 2013;78:530–535. doi: 10.1016/j.gie.2013.04.197. [DOI] [PubMed] [Google Scholar]
- 2.Pizzicannella M., Lapergola A., Fiorillo C., et al. Does endoscopic sleeve gastroplasty stand the test of time? Objective assessment of endoscopic ESG appearance and its relation to weight loss in a large group of consecutive patients. Surg Endosc. 2020;34:3696–3705. doi: 10.1007/s00464-019-07329-1. [DOI] [PubMed] [Google Scholar]
- 3.Alqahtani A., Al-Darwish A., Mahmoud A.E., et al. Short-term outcomes of endoscopic sleeve gastroplasty in 1000 consecutive patients. Gastrointest Endosc. 2019;89:1132–1138. doi: 10.1016/j.gie.2018.12.012. [DOI] [PubMed] [Google Scholar]
- 4.Runge T.M., Yang J., Fayad L., et al. Anatomical configuration of the stomach post-endoscopic sleeve gastroplasty (ESG): what are the sutures doing? Obes Surg. 2020;30:2056–2060. doi: 10.1007/s11695-019-04311-7. [DOI] [PubMed] [Google Scholar]
- 5.Currie A.C., Glaysher M.A., Blencowe N.S., et al. Systematic review of innovation reporting in endoscopic sleeve gastroplasty. Obes Surg. 2021;31:2962–2978. doi: 10.1007/s11695-021-05355-4. [DOI] [PubMed] [Google Scholar]
- 6.Mahmoud T., Vargas E.J., Ghazi R., et al. The osculating circles gastroplasty: a novel endoscopic submucosal esection enhanced endoluminal suturing for obesity. Gastroenterology. 2021;161:1806–1808.e1. doi: 10.1053/j.gastro.2021.08.059. [DOI] [PubMed] [Google Scholar]
- 7.Manner H., Neugebauer A., Scharpf M., et al. The tissue effect of argon-plasma coagulation with prior submucosal injection (hybrid-APC) versus standard APC: a randomized ex-vivo study. United European Gastroenterol J. 2014;2:383–390. doi: 10.1177/2050640614544315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fayad L., Schweitzer M., Raad M., et al. A real-world, insurance-based algorithm using the two-fold running suture technique for transoral outlet reduction for weight regain and dumping syndrome after Roux-En-Y gastric bypass. Obes Surg. 2019;29:2225–2232. doi: 10.1007/s11695-019-03828-1. [DOI] [PubMed] [Google Scholar]
- 9.Itani M.I., Farha J., Sartoretto A., et al. Endoscopic sleeve gastroplasty with argon plasma coagulation: a novel technique. J Dig Dis. 2020;21:664–667. doi: 10.1111/1751-2980.12939. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Combination of argon plasma coagulation prior to suturing for endoscopic gastroplasty as revisional and primary intervention method, respectively.
Combination of argon plasma coagulation prior to suturing for endoscopic gastroplasty as revisional and primary intervention method, respectively.