Abstract
Objective
Currently, individualized navigation templates are rarely applied in pediatric orthopedic surgery. This study aimed to explore the potential of navigation templates obtained using computer-aided design and three-dimensional (3D) printing to correct lower limb deformities in children by the guided growth technique.
Methods
We prospectively studied 45 children with leg length discrepancy (LLD) or lower limb angular deformities, who underwent guided growth surgery involving 8-plate. In total, 21 and 24 children were included in the navigation template (group A) group and in the traditional surgery (group B) group, respectively. Mimics software was used for designing and printing navigation templates. The operation time, X-ray radiation exposure, damage to cartilage, and postoperative complications were recorded.
Results
The mean operation time in groups A and B were 20.78 and 28.39 min, respectively, and the difference was statistically significant. Compared with group B, the intraoperative exposure of X-rays in group A was reduced by 25% on average. After 9–24 months of follow-up, the deformities were corrected in both groups. No significant differences in the treatment effect were noted between the groups, and no complications occurred.
Conclusions
Using the individualized navigation template in the guided growth technique made the surgical procedure convenient and simple to perform. In addition, the operation time and intraoperative exposure to X-rays were reduced. We consider that 3D printed navigation templates can facilitate the accurate completion of corrective surgeries for lower limb deformities in children, which is worthy of promotion and application.
Keywords: Pediatrics, Technology, Bone Diseases
WHAT IS ALREADY KNOWN ON THIS TOPIC
Leg length discrepancy (LLD) and angular deformities are common lower limb deformities in children.
The tension band plate is commonly used to correct angular deformities and LLD.
Accurate placement of 8-plate and screws can reduce the risk of epiphysial plate injury while ensuring the corrective effect.
WHAT THIS STUDY ADDS
This study applied three-dimensional (3D) printed individualized navigation templates to treat lower limb deformities in children by the guided growth technique.
In 90% of patients with individualized navigation template, 8-plate could be successfully located at once, avoiding repeated adjustments.
Using the individualized navigation template in the guided growth technique had a good corrective effect and reduced the operation time and intraoperative X-ray exposure.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE AND/OR POLICY
The use of individualized navigation template in the guided growth technique made the surgical procedure simple to perform and reduced the incidence of complications.
The medical cost was low because no specific equipment was involved, such as the computer-assisted navigation system.
The individualized navigation templates prepared using computer-aided design and 3D printing technologies have great potential for application in pediatric orthopedic surgery, such as guided growth surgery.
Introduction
Leg length discrepancy (LLD) and angular deformities (including pathologic genu varus or genu valgum) are common lower limb deformities in children.1 2 If such patients are not promptly treated, multiple complications may occur, such as standing imbalance, lameness, stress fractures, and arthritis.3–10 The guided growth technique is a commonly used surgical technique for correcting lower limb deformities in children.11 In 2007, Stevens et al reported the use of tension band plates for guided growth for angular correction; since then, several studies have confirmed the safety of treatment with tension band plates.12–15 Considering that the tension band plate in temporary epiphysiodesis has the advantages of not creating a permanent physeal tether through excessive and prolonged compression across the physis, it differs from staple and screw that exert compression on the physis, so it is commonly used to correct angular deformities and LLD.16 The actual corrective effect is related to the 8-plate and accurate placement and orientation of its screws. The accurate insertion of screws is pivotal for the orthopedic surgeons due to large individual differences and small bone size in children.17 If the position of the 8-plate deviates in the direction of the sagittal or coronal plane, it may lead to implant loosening or even secondary deformities such as rotation deformity.18 Accordingly, X-ray fluoroscopy needs to be performed at each step to constantly verify the position intraoperatively. The epiphysial plate in children cannot withstand repeated penetrating damages, so successful insertion of guided Kirschner wire into the 8-plate for the first time is essential.19 Therefore, how to insert 8-plate screws safely and efficiently is a critical issue that needs to be addressed.
In recent years, with the development of digital medicine, individualized navigation templates prepared using computer-aided design (CAD) and three-dimensional printing (3DP) technologies have been widely employed, for example, in spine surgery, joint surgery, and trauma orthopedics.20–22 However, the application of this technique in pediatric orthopedic surgery has rarely been reported. In our previous study, we used individualized navigation templates for treating pediatric developmental dysplasia of the hip, femoral neck fracture, and cubitus varus.23 The application of surgical navigation templates in guided growth surgery to treat lower limb deformities in children remains rare. The aim of this study was to determine whether navigation templates obtained using a combination of CAD and 3DP could be used to treat lower limb deformities in children by the guided growth technique.
Methods
Patients
From January 2014 to July 2017, all children with LLD or lower limb angular deformities, who underwent guided growth surgery involving 8-plate were selected for the study. Finally, 45 children (27 males and 18 females) with lower limb deformities were included. The mean age was 9.5 years (range 3–13 years; table 1). All patients were randomly divided into the 3D printed combined navigation template group (n=21, group A) and traditional surgery group (n=24, group B). CT was performed on the knees of all patients. All patients had to undergo a comprehensive preoperative examination. In this study, the cause of deformity had been identified preoperatively in all patients (ie, idiopathic or post-trauma deformity). Surgical treatment was performed only for children who had angular deformities of >10° or LLD of between 2.5 and 5 cm. Skeletal development of the wrist was assessed to determine skeletal maturity24; it can be ensured that the skeletal maturation still had an estimated growth period of at least 12 months.25 We excluded children with physiological genu varum or genu valgum, bone metabolic diseases, and lower limb deformities due to infections or tumors.
Table 1.
Comparison of general information between the three-dimensional printed combined navigation template group (group A) and traditional surgery group (group B)
| Age (y) |
Gender | Side | Deformity | Proposed surgical site | Primary surgery | |||||||||
| M | F | L | R | Genu varum | Genu valgum | LLD | Medial distal femur | Lateral distal femur | Medial proximal tibia | Lateral proximal tibia | Yes | No | ||
| Group A (n=21) | 9.43±2.50 | 13 | 8 | 13 | 13 | 3 | 10 | 8 | 18 | 11 | 15 | 11 | 16 | 5 |
| Group B (n=24) | 9.13±2.89 | 11 | 13 | 18 | 12 | 7 | 13 | 4 | 18 | 10 | 11 | 9 | 20 | 4 |
| P value | 0.710 | 0.373 | 0.591 | 0.208 | 0.942 | 0.713 | ||||||||
P values were obtain by analysis of variance for quantitative data and by χ2 test for qualitative data.
F, female; L, left; LLD, leg length discrepancy; M, male; R, right.
Preoperative designing and printing individualized navigation templates
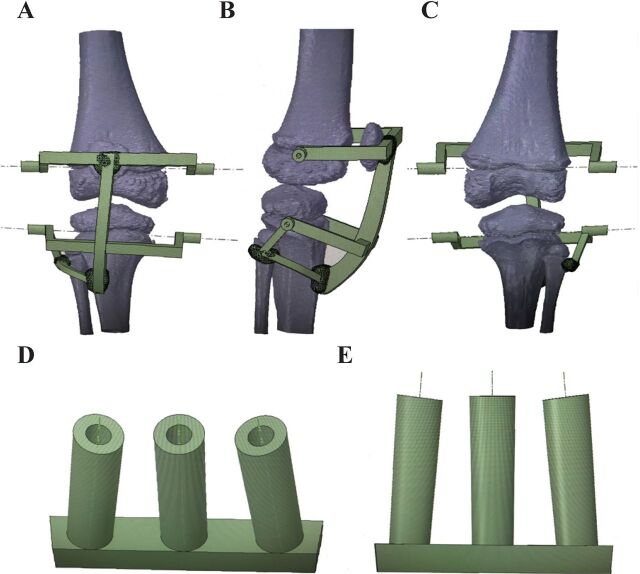
Preoperative CT images were acquired on a 64-MSCT scanner (Philips, Netherlands), with parameters of 120 kV, 160 mA, and 1 mm section thickness. Imaging data were stored in DICOM format. The Mimics software (Materialise, Belgium) was used for designing and printing the skin surface template (assisting in percutaneous puncture the guided pin through 8-plate) and bone surface template (assisting in the accurate insertion of two 8-plate screws). According to the radiographs, differences in the femoral and tibial length, mechanical lateral distal femoral angle (mLDFA), and mechanical medial proximal tibial angle (mMPTA) were measured to determine the placement of 8-plate. When correcting femoral or tibial valgus, the 8-plate was placed on the medial aspect of knee, and the varus deformity was corrected on the lateral aspect correspondingly. When correcting LLD, the 8-plate was placed on both the medial and the lateral sides of the femur and/or tibia. CT data were used to generate the 3D reconstructed knee joint model by using Mimics 17.0 (Materialise NV, Leuven, Belgium). Anatomical data pertaining to the skeletal surface of the knee joint, such as the patella, tibial tuberosity, and fibular head, were extracted. A wing-shaped substrate with the same shape was then established, and the thickness was reversed by 5 mm. The image of the knee joint was rotated (figure 1A) and the navigation hole data for the Kirschner wire were calculated; the Kirschner wire was to be inserted into the middle region of the corresponding growth plate cartilage based on the side view (figure 1B) of the knee. Then, combined the navigation hole data into a skin surface navigation template (figure 1C). After simulating the precise insertion of 8-plate, navigation holes were designed to match the Kirschner wire guide pin and those suitable for two screws at appropriate distances (based on the distance between two holes of 8-plate) from the upper and lower ends of guide pin (figure 1D). The angle between the extension lines of the upper and lower navigation holes was 30°. After the Boolean operation, according to screw length and diameter, cross the Kirschner wire navigation hole, and then trim the boundary to complete the design of bone surface template (figure 1E). The computer measured and recorded the projected screw length and exported data pertaining to the model. Data were then imported into the 3DP device (Fusion Tech, China) in Standard Triangle Language format, and 3D printed combined navigation templates made of medical polylactic acid were eventually obtained and plasma sterilized without causing deformation of navigation templates.
Figure 1.
Designing and printing individualized navigation templates. The skin surface template part of 3DP navigation templates: a front view (A), a side view (B), and a dorsal view (C). The skin surface template part: the main view (D) and front view (E). Figure 1 was illustrated by all authors and its use gained the permission of all authors.
Preoperative preparation, surgical process, and postoperative treatment
Before the operation, a general appearance picture (figure 2A) and anteroposterior full-length radiographs of the legs (figure 2B) were obtained from all patients in the standing position. To keep the pelvis horizontal, blocks of appropriate sizes were inserted under the shorter limb, depending on the degree of LLD. During the surgery, damage to the growth plate cartilage and articular cartilage was avoided as much as possible. Patients in traditional surgery group were scanned using C-arm X-ray intraoperatively. According to the standard operative protocol, a longitudinal incision of approximately 2–3 cm in length was made on the outer side of the femoral condyle, and the skin, subcutaneous tissue, and fascia were then sequentially incised.12 26 Under C-arm X-ray monitoring, the growth plate region was punctured with a thin Kirschner wire. The Kirschner wire was used as a positioning pin, and the positioning hole at the center of the 8-plate was then inserted into it. Drilling the Kirschner wires as the guide pin on the upper and lower navigation holes of the 8-plate. After confirming the position of 8-plate and Kirschner wire using X-ray imaging, the 8-plate was fixed using a hollow bit to insert cannulated screws in the direction of the upper and lower Kirschner wires. The anterior and lateral knee X-rays were then reviewed to confirm accurate positioning of the 8-plate and screws; the guiding and positioning Kirschner wires were removed.
Figure 2.
Application of three-dimensional printed navigation template to treat a 6-year-old boy with leg length discrepancy. (A) A 6-year-old boy deformed leg length discrepancy (LLD) after trauma, and his left lower limb is overgrown by 2.5 cm. (B) Standing anteroposterior (AP) preoperative full-length leg radiographs. (C, D) The skin surface navigation template’s positioning area fitted with the bony landmarks (the patella, tibial tuberosity, and fibular head). (E) Drill with Kirschner wires according to the direction of the preoperative design navigation hole. (F) The previously used Kirschner wire was employed to position the growth plate into the middle navigation hole of the bone surface navigation template. (G) Use C-arm X-ray to verify the Kirschner wire’s place. (H) Full-length leg radiographs after 1 month of follow-up. (I) Full-length leg radiographs after 2 years of follow-up. (J) General appearance after 2 years of follow-up. L, left.
In group A, the positioning area of the skin surface navigation template fitted with the bony landmarks (the patella, tibial tuberosity, and fibular head) (figure 2C, D). While maneuver holding an electric drill with the Kirschner wire according to the direction of the preoperative design navigation hole, the surgeon used their left hand to fix and maintain the stability of the skin surface navigation template (figure 2E). C-arm X-ray subsequently was used to verify whether the Kirschner wire was in place (figure 2F). A longitudinal incision of approximately 2–3 cm in length was made around the Kirschner wire navigation hole, followed by blunt separation to fully expose the surgical field. The bone surface template was used outside the periosteum (figure 2G); the previously used Kirschner wire was employed to position the growth plate into the middle navigation hole of the bone surface navigation template. The Kirschner wires were then drilled according to the navigation holes on both sides of the template. According to preoperative computer measurement results, a hollow screw of an appropriate length was selected and placed along the direction of the upper and lower navigation holes.
The operation time, number of X-rays, damage to growth plate cartilage and articular cartilage, and postoperative complications were recorded. No external fixation was required for the affected limb postoperatively. Patients were encouraged to start walking after the surgery, and they gradually resumed normal activities, while avoiding strenuous exercise and trauma. Follow-ups were performed every 3 months postoperatively, and the degree of deformity correction was evaluated by radiological and clinical examinations (Figure 2H–I). After achieving the correction, a second surgery was planned for implant removal.
Statistical analysis
Statistical analyses were performed using SPSS V.23.0 (SPSS, USA). P values <0.05 were considered statistically significant. Data were expressed as mean ± SD. Independent sample t-test was applied in the difference analysis. Differences between two groups were analyzed by the Student’s t-test and the χ2 test.
Results
Preoperative design and navigation template preparation
The skin surface navigation template was successfully designed based on the knee bony landmarks, and the direction and length of the navigation holes were effectively calculated. According to the different widths of the distal femur and/or proximal tibia in each patient, the appropriate size of the 8-plate and screws was selected. The preoperative design duration for group A was 37–63 min (average, 45.6 min), and all 3D printed combined navigation templates were successfully designed and printed.
Surgical outcomes
In group A, two patients with genu valgum were obese, and it was difficult to accurately locate the skin surface navigation template; so, body surface templates were not used intraoperatively. However, in these two patients, after adjusting the guide pins inserted into the 8-plate, the bone surface navigation template could still be used, and the surgery continued to be simple and accurate to assist the placement of the two screws. In the remaining patients in group B, individualized navigation templates prepared using a combination of CAD and 3DP completely matched the knee bony landmarks intraoperatively. The mean operation times of each 8-plate in the navigation template group and the traditional operation group were 20.78±2.36 and 28.39±2.35 min, respectively. The operation time between two groups showed significant differences (p<0.001).
In comparison with the average of 4.70 times in group B, the number of X-rays in group A was 3.50 times, which was statistically significant (p<0.001, table 2). After 9–24 months (average, 17.1 months) of postoperative follow-up, lower limb deformities were corrected in both groups. If the correction was achieved, another surgery would be planned to remove the 8-plate and screws. There was no significant difference in the treatment effect between two groups, and no complications that include incision infection, loosening of internal fixation, and neurovascular injury occurred.
Table 2.
Comparison of surgery-related information and results between the three-dimensional printed combined navigation template group (group A) and traditional surgery group (group B)
| Operation time | X-ray exposure | Growth plate cartilage or articular cartilage injury | Achieve the treatment goals at the last follow-up | ||
| (min) | (time)* | Yes | Yes | No | |
| Group A | 20.78±2.36 | 3.50±0.65 | 0 | 18 | 3 |
| Group B | 28.39±2.35 | 4.70±0.88 | 3 | 20 | 4 |
| P value | 0.00 | 0.00 | 0.094 | 0.826 | |
Data were presented with mean±SD.
P values were obtain by analysis of variance for quantitative data and by χ2 test for qualitative data.
* Times means the exposure numbers of X-ray.
SD, standard deviation.
Discussion
LLD and angular deformities are common lower limb deformities in children.2 Using the tension band plate in temporary epiphysiodesis is a commonly used treatment method for patients who still show growth potential. This surgical intervention can effectively correct angular deformities or limit excessive growth of the limbs.27 The 8-plate method, which can provide a tension band, is effective in correcting deformities and has a low incidence of postoperative complications; moreover, osteotomy can be avoided.28 29 However, owing to large individual differences and to complex anatomical structures in children, intraoperative errors can easily damage the articular surface and even the growth plate, which poses a challenge to surgeons. Stevens et al found that the tension band plate in temporary epiphysiodesis might cause various complications in clinical applications, such as incision infection, loosening or breakage of the internal fixation, recurrence of deformity, damage of the growth plate, and early fusion of the epiphysial growth plate.12 25 Therefore, to correctly position the guided Kirschner wire into growth plate during the surgery, skillful and experienced surgeons are needed. Due to the complex anatomical structure of growth plate in the distal femur and proximal tibia of children and considering the different degrees of deformity, it is difficult to locate a growth plate by directly using the Kirschner wire as a guided pin intraoperatively.30 During previous surgery, it is necessary to use X-rays repeatedly to adjust the position and angle of the guide pin, particularly when the proximal tibia growth plate is small in size and narrow in height, and its outer edge needs to avoid the fibula. Inserting and withdrawing pins repeatedly can easily damage the surrounding nerves, puncture blood vessels, and cause incision infection; moreover, the pins may penetrate into joints and damage the articular surface, and even cause irreversible damage to the growth plates. In addition, repeated use of X-rays intraoperatively can increase the radiation exposure to patients and surgeons, and excessive exposure during childhood has been reported to increase the risk of tumor incidence. Therefore, there is a need for an auxiliary positioning method that is low cost and easy to popularize, along with strong practicability. The 3D printed combined navigation template produced in this study matched the patients well. The patella, tibial tuberosity, and fibular head are easily accessible surface bony landmarks. Herein with the guidance of the body surface navigation template, first, the most critical step was the accurate insertion of the guided Kirschner wire in the middle hole of the 8-plate, followed by using the guided Kirschner wire as the center to incise the soft tissue. After the guide pin was inserted into the middle hole of the bone surface navigation template and matched with the bone surface, two cannulated screw guide pins were accurately inserted according to the upper and lower holes, and the screw length was precisely controlled. Using the 3DP printed combined navigation template can avoid frequent positioning correction and repeated X-rays; moreover, the template can help control the length of the screw being implanted. Compared with group A, the operation time and number of X-rays in group B were significantly reduced. Another interesting thing is that by comparing the operation time of two groups, it was found that the operation time on the lateral aspect of the proximal tibia was longer than that on the medial aspect of the proximal tibia. In addition, the operation time of the proximal tibia is longer than that of the distal femur. It is because the anatomical structure of proximal tibia is very small, and the thickness of growth plate is thinner than that of the distal femur, so it takes longer to position the Kirschner wire in the growth plate with than at the distal femur. The fibula is located on the outer side of proximal tibia, and it is vital to avoid the obscured fibular head. Therefore, it is tricky to use the Kirschner wire to locate the growth plate on the outer side of proximal tibia. It is often necessary to penetrate the Kirschner wire multiple times to find the best position, which takes a long time. In traditional surgery, to ensure that correct positioning of the 8-plate, avoiding anterior or posterior position, and avoiding secondary torsional deformities, it is pivotal to repeatedly change the patients’ position or turn the C-arm; these steps prolong the operation time and increase the risk of infections. The 3D printed combined navigation template designed in this study as a part of the preoperative design process ensured the accurate positioning of 8-plate without the need for X-rays, making the surgery quite convenient.
As one of the objectives of using the 8-plate by guided growth technique is to slow down, rather than to stunt, the growth of the part, a lag period is unavoidable. Burghardt et al considered that the slower growth rate with 8-plate might be due to the fact that it takes a certain time for the screws to diverge with growth until they are fully engaged with the plate.31 Faster correction may be achieved by using prepositioned screws in an open angle in the 8-plate during implantation. Eltayeby et al found that the opening angle of between 0° and 30° had no effect on the correction rate.32 Take the skeletal age and needs of remaining growth into account, the implant should not be placed in the body for >2 years.33 And based on our clinical experience, the interscrew angle should be 30°. It was difficult to accurately control the angle in group A, so X-rays should be repeatedly performed. On the other hand, using the navigation template could help accurately regulate the angle to 30°. Zhang et al designed an in vivo assisted navigation template for the 8-plate screws with three parallel guided holes34; however, such screws tend to gradually open in the first few months. The hysteretic effect may delay the time for the correction to show an effect, which may cause older children to lose the best correction period. More importantly, they could not overcome the difficulty of inserting the guided Kirschner wire and controlling its position34; thus, X-rays needed to be acquired repeatedly. They only used the bone surface navigation template, and it is difficult to achieve a perfect match on the bone surface because of its small surface contact area.34 Therefore, this navigation template was challenging to achieve precise control of screw placement and thus required repeated puncture positioning, which may increase the risk of radiation exposure and growth plate cartilage or articular cartilage injury. Recently, our research group has conducted extensive research in the field of digital medicine, particularly surgical navigation templates designed using 3DP. In the present study, in group B, an individualized 3D printed combined navigation template was obtained on designing on a computer. The template showed a high degree of matching with surface bony landmarks and fitted tightly. Herein, in 90% patients with the navigation template, the 8-plate could be successfully located at once, avoiding repeated adjustments. The use of navigation template made the surgery more convenient, markedly shortened the operation time and subjectively, was associated with less blood loss. More importantly, accurate positioning of the Kirschner wire considerably improved the surgical results.
The 3DP printed combined navigation template designed in this study had many advantages. The individualized data obtained by computer measurements could determine the insertion position of the guide pin, 8-plate, and screws. This ensured that the 8-plate is located in the middle of the coronal position, reducing the correction of anterior and posterior deformities and ensuring that the screw length does not exceed the midline of the coronal position of the affected limb. Therefore, the possibility of iatrogenic injury to articular cartilage and growth plate cartilage is reduced, the correction results are better, and the incidence of complications is further reduced. Moving on, the navigation template used multiple surface bony landmarks. As long as this template is closely fitted to the corresponding anatomical structure of the bone, precise positioning and orientation can be completed without special experience requirements; this is particularly valuable for young doctors. In addition, the size of the navigation template is small, which eliminates the need of large surgical incision. No specific equipment was involved such as a computer-assisted navigation system, so the medical cost is low. However, this study still has some limitations. First, the skin surface template designed in this study relies on the positioning of surface bony landmarks, and more points and 3D selection of these landmarks should be used to enhance the degree of navigation template fitment and stability. Considering that its use was limited in special cases, such as severely obese patients, we aim to further optimize the design in our future studies. Second, the sample size was small and the follow-up was not long enough. There was no investigation on the correction of the sagittal deformity of the knee joint in children. Finally, although using the navigation template made the surgical process convenient and reduced intraoperative injuries in children, the preoperative time required to design the template is long. With proficiency in technical operations, the time could gradually decrease. And we believe that artificial intelligence can also be used to expedite template designing.
For children with LLD or lower limb angular deformities, CT has high diagnostic value that was required to determine whether there were deformities due to growth plate lesions. Although the radiation dose of performing a single CT is usually higher than that from X-ray, preoperative CT could provide additional advantages, including significantly reducing the number of intraoperative X-rays, making the surgery more convenient, markedly shortening the operation time and improving the surgical results. Therefore, the risk of CT-related radiation dose can be considered small compared with the benefits that accurate diagnosis and treatment can provide. Of course, despite the fact that the benefits of CT exceed the harmful effects of radiation exposure, we should still avoid unnecessary radiation exposure during medical procedures. Moreover, we expect to make individualized navigation templates by using MRI instead of CT, which is also our research direction in future.
To conclude, we successfully used the 3D printed combined navigation template to correct lower limb deformities in children by the guided growth technique. This method was convenient, simplified the surgical process, reduced the operation time, and even reduced the intraoperative X-ray radiation exposure, which is worthy of promotion and application for the children with LLD or lower limb angular deformities.
Footnotes
Contributors: MF: Formal analysis and writing—original draft. YW: Formal analysis and writing—original draft. HP: Data curation. YW: Data curation. PX: Software. YL: Resources. PZ: Funding acquisition, Writing—review and editing, and acting as the guarantor. KT: Funding acquisition and writing—review and editing. All authors finally approved the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: This work was supported by the Science Foundation of Jiangsu Provincial Key Research and Development Program grant number BE2019608.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. Not applicable.
Ethics statements
Patient consent for publication
Consent of figure 2 has been obtained from parent(s)/guardian(s).
Ethics approval
This study involves human participants and was approved by the Ethics Committee of Children’s Hospital of Nanjing Medical University (approval number: 201306279-1). Participants gave informed consent to participate in the study before taking part.
References
- 1. White GR, Mencio GA. Genu valgum in children: diagnostic and therapeutic alternatives. J Am Acad Orthop Surg 1995;3:275–83. 10.5435/00124635-199509000-00003 [DOI] [PubMed] [Google Scholar]
- 2. Wilkins KE. Bowlegs. Pediatr Clin North Am 1986;33:1429–38. 10.1016/S0031-3955(16)36152-1 [DOI] [PubMed] [Google Scholar]
- 3. Gurney B. Leg length discrepancy. Gait Posture 2002;15:195–206. 10.1016/S0966-6362(01)00148-5 [DOI] [PubMed] [Google Scholar]
- 4. Golightly YM, Allen KD, Renner JB, et al. Relationship of limb length inequality with radiographic knee and hip osteoarthritis. Osteoarthritis Cartilage 2007;15:824–9. 10.1016/j.joca.2007.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Harvey WF, Yang M, Cooke TDV, et al. Association of leg-length inequality with knee osteoarthritis: a cohort study. Ann Intern Med 2010;152:287–95. 10.7326/0003-4819-152-5-201003020-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kim C, Nevitt M, Guermazi A, et al. Brief report: leg length inequality and hip osteoarthritis in the multicenter osteoarthritis study and the osteoarthritis initiative. Arthritis Rheumatol 2018;70:1572–6. 10.1002/art.40537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tahririan MA, Mohammadsharifi G. Correction of the knee coronal plane deformity using the screws plus reconstruction plate versus cannulated screws. Orthop Traumatol Surg Res 2020;106:1345–51. 10.1016/j.otsr.2020.04.020 [DOI] [PubMed] [Google Scholar]
- 8. Álvarez-López CA, García-Lorenzo YC. [Relationship between angular deformity and primary osteoarthritis of the knee. Review article]. Acta Ortop Mex 2015;29:232–6. [PubMed] [Google Scholar]
- 9. Felson DT, Niu J, Gross KD, et al. Valgus malalignment is a risk factor for lateral knee osteoarthritis incidence and progression: findings from the multicenter osteoarthritis study and the osteoarthritis initiative. Arthritis Rheum 2013;65:355–62. 10.1002/art.37726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sharma L, Song J, Felson DT, et al. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 2001;286:188–95. 10.1001/jama.286.2.188 [DOI] [PubMed] [Google Scholar]
- 11. Gottliebsen M, Shiguetomi-Medina JM, Rahbek O, et al. Guided growth: mechanism and reversibility of modulation. J Child Orthop 2016;10:471–7. 10.1007/s11832-016-0778-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop 2007;27:253–9. 10.1097/BPO.0b013e31803433a1 [DOI] [PubMed] [Google Scholar]
- 13. Gorman TM, Vanderwerff R, Pond M, et al. Mechanical axis following staple epiphysiodesis for limb-length inequality. J Bone Joint Surg Am 2009;91:2430–9. 10.2106/JBJS.H.00896 [DOI] [PubMed] [Google Scholar]
- 14. Shabtai L, Herzenberg JE. Limits of growth modulation using tension band plates in the lower extremities. J Am Acad Orthop Surg 2016;24:691–701. 10.5435/JAAOS-D-14-00234 [DOI] [PubMed] [Google Scholar]
- 15. Raluy-Collado D, Sanpera I, Frontera-Juan G, et al. Screw length in the guided growth method. Arch Orthop Trauma Surg 2012;132:1711–5. 10.1007/s00402-012-1615-3 [DOI] [PubMed] [Google Scholar]
- 16. Ballal MS, Bruce CE, Nayagam S. Correcting genu varum and genu valgum in children by guided growth: temporary hemiepiphysiodesis using tension band plates. J Bone Joint Surg Br 2010;92:273–6. 10.1302/0301-620X.92B2.22937 [DOI] [PubMed] [Google Scholar]
- 17. Siedhoff M, Ridderbusch K, Breyer S, et al. Temporary epiphyseodesis for limb-length discrepancy. 8- to 15-year follow-up of 34 children. Acta Orthop 2014;85:626–32. 10.3109/17453674.2014.960646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dai Z-Z, Liang Z-P, Li H, et al. Temporary hemiepiphysiodesis using an eight-plate implant for coronal angular deformity around the knee in children aged less than 10 years: efficacy, complications, occurrence of rebound and risk factors. BMC Musculoskelet Disord 2021;22:53. 10.1186/s12891-020-03915-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhao J, Ma Y, Han D, et al. [Application of three-dimensional printing in the operation of distal tibia fracture involving epiphyseal plate injury for teenagers]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2017;31:1195–9. 10.7507/1002-1892.201704103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wu A-M, Lin J-L, Kwan KYH, et al. 3D-printing techniques in spine surgery: the future prospects and current challenges. Expert Rev Med Devices 2018;15:399–401. 10.1080/17434440.2018.1483234 [DOI] [PubMed] [Google Scholar]
- 21. Ni J, Li D, Mao M, et al. A method of accurate bone tunnel placement for anterior cruciate ligament reconstruction based on 3-dimensional printing technology: a cadaveric study. Arthroscopy 2018;34:546–56. 10.1016/j.arthro.2017.08.288 [DOI] [PubMed] [Google Scholar]
- 22. Sun L, Liu H, Xu C, et al. 3D printed navigation template-guided minimally invasive percutaneous plate osteosynthesis for distal femoral fracture: a retrospective cohort study. Injury 2020;51:436–42. 10.1016/j.injury.2019.10.086 [DOI] [PubMed] [Google Scholar]
- 23. Zheng P, Xu P, Yao Q, et al. 3D-Printed navigation template in proximal femoral osteotomy for older children with developmental dysplasia of the hip. Sci Rep 2017;7:44993. 10.1038/srep44993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Acheson RM. A method of assessing skeletal maturity from radiographs; a report from the Oxford child health survey. J Anat 1954;88:498–508. [PMC free article] [PubMed] [Google Scholar]
- 25. Klatt J, Stevens PM. Guided growth for fixed knee flexion deformity. J Pediatr Orthop 2008;28:626–31. 10.1097/BPO.0b013e318183d573 [DOI] [PubMed] [Google Scholar]
- 26. Masquijo JJ, Lanfranchi L, Torres-Gomez A, et al. Guided growth with the tension band plate construct: a prospective comparison of 2 methods of implant placement. J Pediatr Orthop 2015;35:e20–5. 10.1097/BPO.0000000000000263 [DOI] [PubMed] [Google Scholar]
- 27. Stevens PM, Maguire M, Dales MD, et al. Physeal stapling for idiopathic genu valgum. J Pediatr Orthop 1999;19:645–9. 10.1097/01241398-199909000-00018 [DOI] [PubMed] [Google Scholar]
- 28. Burghardt RD, Herzenberg JE, Standard SC, et al. Temporary hemiepiphyseal arrest using a screw and plate device to treat knee and ankle deformities in children: a preliminary report. J Child Orthop 2008;2:187–97. 10.1007/s11832-008-0096-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Burghardt RD, Herzenberg JE. Temporary hemiepiphysiodesis with the eight-Plate for angular deformities: mid-term results. J Orthop Sci 2010;15:699–704. 10.1007/s00776-010-1514-9 [DOI] [PubMed] [Google Scholar]
- 30. Craig JG, Cody DD, Van Holsbeeck M. The distal femoral and proximal tibial growth plates: MR imaging, three-dimensional modeling and estimation of area and volume. Skeletal Radiol 2004;33:337–44. 10.1007/s00256-003-0734-x [DOI] [PubMed] [Google Scholar]
- 31. Burghardt RD, Kanellopoulos AD, Herzenberg JE. Hemiepiphyseal arrest in a porcine model. J Pediatr Orthop 2011;31:e25–9. 10.1097/BPO.0b013e31821a5d04 [DOI] [PubMed] [Google Scholar]
- 32. Eltayeby HH, Iobst CA, Herzenberg JE. Hemiepiphysiodesis using tension band plates: does the initial screw angle influence the rate of correction? J Child Orthop 2019;13:62–6. 10.1302/1863-2548.13.180086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Blount WP, Clarke GR. Control of bone growth by epiphyseal stapling; a preliminary report. J Bone Joint Surg Am 1949;31A:464–78. [PubMed] [Google Scholar]
- 34. Zhang HT, Kong XX, Shi Q. Clinical study on straightening lower limb using rapid prototyping template for guiding implantation of eight shape plate. Chinese Journal of Bone and Joint Injury 2016;31:479–81. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. Not applicable.