Abstract
Health, harms and disease are intimately linked, and their promotion and distribution are determined by the social, political and physical worlds in which people live. Yet, the popular narrative on health is still dominated by a biological model that focuses on a disease-causing ‘pathogen’ or ‘agent’ that leads to pathology which is diagnosable and amenable to intervention at the individual level via measures delivered through the health care and public health systems. This model generally rests on understanding populations as a collection of individuals, with the pattern of disease seen as the sum of a series of risk factors acting on each of them. Too little attention is paid to the ways in which health, harm, disease, causation and risk are conceptualized and used as guiding concepts in research, policy debates and other fora. We often overlook the distribution of health and the regulatory regimes, norms, values and rights that promote or undermine health. By challenging our ways of thinking about health, harms and disease, we can start to appreciate with greater depth the ways in which health can be threatened and what should be seen as harmful, and conversely, opportunities for moving our systems towards promoting and protecting health.
Keywords: commercial determinants of health, and inequities; health promotion; public health; social determinants
Why are some people healthy and others not?
A 1994 book by Canadian authors asked a seemingly simple question: why are some people healthy and others not?1 It recognizes the contribution of science, for example germ theory and understanding of the molecular basis of disease, but also the wider influences on health, often termed ‘upstream’ determinants. Since then, a growing body of research has shed light on the complex nature of disease and its distribution within populations, with the development of multi-causal models, or ‘webs’ of causation.2 Yet, the popular narrative on health is still dominated by a biological model, ‘biomedical individualism’, that focuses on a disease-causing ‘pathogen’ or ‘agent’ (e.g. parasite or cigarette) that leads to pathology which is diagnosable and amenable to intervention at the individual level via measures delivered through the health care and public health systems. This model generally rests on understanding populations as a collection of individuals, with the pattern of disease seen as the sum of a series of risk factors acting on each of them. This leads to messages such as ‘risk factor [e.g. smoking, alcohol, poor diet] causes x deaths per year and costs the economy £y’ or debates about how many deaths occurred ‘from’ or ‘with’ Covid-19.
While greater recognition of the social determinants of health potentially broadens this lens, they are often seen as secondary or ‘distal’ to more ‘proximal’ causes of disease.3 Correspondingly, efforts to address the wider determinants of health or disease tend to drift towards intervening on a limited set of behavioural risk factors often characterized as ‘lifestyles’, typically focusing on changing individual behaviour so as to reduce consumption of whatever is seen as the main ‘cause’ of a disease.4,5 As discussed by others previously, these lines of thinking risk excluding consideration of powerful social, political and commercial determinants of health and disease, foreclosing engagement with why diseases and their outcomes are distributed in the ways that they are,3 and assuming that knowledge of aetiology can be applied directly and uncritically to strategies for prevention.6
Of course, while public health measures should, where possible, be informed by an understanding of the biological causes of disease, there is a danger that a narrow focus on them, and the ‘proximal’ risk factors, and by extension, individual choice, will constrain our scope to engage with the wider determinants of health and disease and, especially, the ‘causes of the causes’.2,3,7,8 Thus, while remarkable advances have been achieved in our understanding of the determinants of health and cause of disease, with much of this taking place during the 50 years since the inception of the UK Faculty of Public Health, in many ways the public’s health is not flourishing, particularly in the case of the most disadvantaged. The experience of the Covid-19 global pandemic, which has stimulated growing support for a transition to healthier, just and sustainable ways of living and governing,9 gives us the opportunity to scrutinize how certain ways of thinking about and explaining health and disease may hinder or enable addressing the public health challenges we face in the 21st century.
The greater recognition of the wider determinants of health, be they social, political, environmental or commercial, has important implications for how we conceptualize, measure and act upon health harms and how we respond to them. Yet too little attention is paid to the ways in which health, harm, disease, causation and risk are conceptualized and used as guiding concepts in research, policy debates and other fora. We often fail to distinguish between the different concepts that exist, sometimes using them interchangeably. Crucially, when we describe and respond to disease burden, we often overlook the distribution of health and the regulatory regimes, norms, values and rights that promote or undermine health.
Revisiting our conceptualizations of health
The WHO understands health to be ‘a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity’.10 Like all definitions that seek to capture complex concepts that are influenced by contextual and historical forces, it may not reflect all perspectives and nuances. However, what it does capture is the critical difference between the causation and presence of disease, and the attainment of health, with many implications for how we understand and therefore address public health harms and threats to health, particularly those that emerge as our social, political, economic, cultural and environmental contexts change over time. It is also important to appreciate this difference as it has implications for fulfilment of human rights for all, with the WHO constitution also stating that ‘[t]he enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition’,10 and these contexts often restrict the ability of members of certain groups to enjoy those rights.11
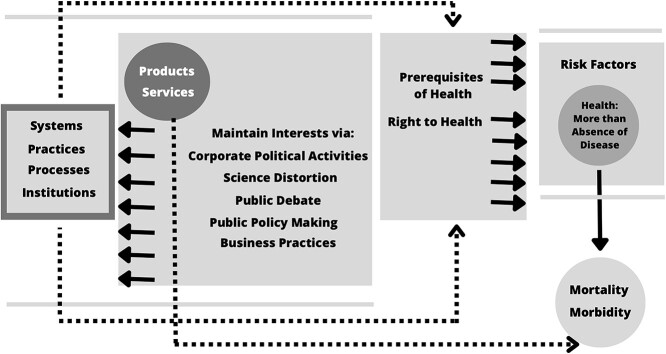
These considerations take on particular importance in the context of emerging trends and forces that have the potential to undermine public health in ways that fall outside of disease-oriented models with their emphasis on proving causation based on characterizing biological mechanisms at the individual level. Furthermore, concepts of disease and causation are often conflated with health and harm, with little attention being directed at how these are distinct, albeit with important connections. Recognizing this difference allows for more consideration to be directed at how harms may contribute to undermining public health in more ways than through the development of disease: there are social, political or other factors, such as corporate lobbying or marketing strategies, that may contribute to mechanisms that have detrimental impacts on health without causing disease in an individual. It also challenges us to define harm and to reflect on the level at which harm should be measured, where it can be seen to be occurring, what are the underlying mechanisms or explanations for its emergence, and how the concept may be (mis)used to maintain the status quo by limiting its meaning. In the case where the threat to health is the development of a particular disease, is the harm confined to the product or causative ‘agent’ associated with that disease, the harmful ‘life-style choice’, the circumstances in which the individual makes a given choice, or should we look for multiple harms interconnecting in ways that ultimately culminate in disease, many with their origins in a complex mix of processes, practices or regulatory systems (Fig. 1)?
Fig. 1.
Representation of the key elements in a complex system of health, harms and disease.
Complex systems of harm
These questions remind us of the political nature of health:12 who is responsible and what should be done to protect and promote health, how are problems that undermine health being defined, and with what implications and for whom? Who should fund and produce the evidence underpinning our understanding of causes of disease, what counts as proof, and who should be seen as responsible for ill-health? These issues are all highly contested, particularly when considerable political and commercial interests are involved. Broadening how we think about health, disease, harms and related concepts such as ‘harmful’ and health threats changes the terrain on which such debates take place and affects where public health must direct its gaze and actions. This also raises questions of governance, and about the norms and values that guide what comes to be understood as constituting ‘proof’ of disease versus harm. What can and should be considered a health harm, and who decides which conceptual models should guide this thinking? Who should be seen as responsible for defining the extent of a harm and what metrics can and should be used? Open and effective engagement with the public, including young people, on these issues will be key to building public understanding and ownership of broader conceptualizations of harm. This in turn may build public support for the kinds of policies needed to prevent diverse forms of harm and to promote health and equity.
Harm often lies at the centre of highly sensitive political and commercial issues—the impacts of lead, asbestos, tobacco, alcohol, agrochemicals, for example—with the ‘harms’ associated with these issues being, in some contexts, mostly conceptualized through an exposure-disease conceptual model, often appropriately. But do the harms extend beyond the corresponding diseases? In all these cases, it can be argued that the disease burden associated with the product in question goes far beyond the individual most obviously affected, such as the smoker who gets lung cancer. To take that example, there is a complex system, involving a wide range of processes, each facilitated or constrained by, for example, regulatory contexts that encouraged that individual to take up smoking and obtain cigarettes. Thus, tobacco companies engage in employment practices that may harm the farmers who harvest tobacco,13 they engage in lobbying to undermine health policies more generally, they employ tax evasion that reduces the availability of funds for health care14 and they act corruptly,15 undermining the rule of law that is necessary to safeguard health. Thus, the spectrum of harms associated with a proximal risk factor for a particular disease can be extensive and is often influenced by the actions of those driving the harm as they act to protect their commercial interests. It is thus apparent that the overall toll of harm incurred cannot be explained or mitigated by understanding the biological causal mechanisms alone. In cases such as this, it is crucial to have an understanding of the many ways in which those whose interests are threatened by regulating to prevent harm and protect workers and the public act to block or delay change. Along a similar line of thinking, Robert Proctor, leading tobacco industry historian, explains that "[n]o causes are themselves uncaused, however, which means that when we think about what causes lung cancer or even smoking, we should think not just in terms of how individuals `decide' to start smoking, but rather in terms of larger, more weblike threads of causation. We have to look at the cigarette epidemic and therefore lung cancer as facilitated by long causal chains of a sociopolitical, technical, molecular and agricultural nature.16 More generally, the efforts of certain industries to distort science, public debate and public policymaking have contributed to delays and lost opportunities to prevent disease or damage to the environment, and to promote health, that go far beyond their particular product and have profound consequences for people and planet. Furthermore, can societies that function is such a way as to value and incentivize this form of multidimensional harm in the pursuit of profit, disproportionately harming those who benefit the least, ever be regarded as healthy societies? A body cannot thrive in part only, just as a society cannot flourish based on practices and systems that lack compassion and are harmful to some of its members.16,17
Harm thus can be understood as more than causes and presence of disease or risk factors that increase the likelihood of disease. Indeed, understandings of harm from other fields, such as law or philosophy, where, for example loss of privacy or agency is are understood as forms of harm, may help when conceptualizing harms to health beyond the presence of disease. The meanings we assign to concepts such as harm should also reflect the experiences of the individuals, families and communities that are harmed, and definitions adopted by those in positions of power or those with vested interests should be open to challenge. The concept can be extended to include the forces that determine why disease and risk is occurring to whom and in what form and those which compromise the attainment of health, through, for example, undermining people’s continued access to, and enjoyment of, the pre-requisites to health. Harms may thus include practices and policies that shape determinants of health and disease in ways that go beyond the individual relationship between disease and its proximal determinants. By adopting a broader view, we can encompass the effects of harmful systems and practices: what should be seen as the harm, what is harmful and where among the process and practices of the social world is harm seen to lie? This then forces us to confront how decision-making processes that are not open to scrutiny or scientific processes that have lost their integrity, for example, can be seen as harmful.
Relatedly, harm may arise from unquestioningly adhering to a pursuit of a narrow model of causation when studying different social phenomena. A wider perspective than that employed in the natural and biological sciences can thus provide valuable insights about the ways that harm can arise and be perpetuated. An understanding of how regulatory agencies, for example, are vulnerable to corporate capture or how their structures constrain them from acting in the interests of the public even when evidence of harm emerges is essential. Building on this further, the ways in which the concept of ‘causation’ and the closely related one of ‘uncertainty’ can be manipulated, misunderstood or misrepresented to protect commercial interests and the consequences this has for public policymaking can be seen as harmful practices in and of themselves.18–23
By charting the differences and connections between causes of disease and health harms, we can start to understand with greater depth the ways in which health can be threatened and what should be seen as harmful, and conversely, opportunities for moving our systems towards promoting and protecting health. This also focuses attention on who benefits from health harming systems or practices, revealing the conflicts of interest that can arise and the need for systems that facilitate engagement with and handling of opposing interests as opposed to concealing them, for example, behind a smokescreen of activities that fall within the concept of Corporate Social Responsibility (CSR). Similarly, there are other harms that warrant more attention including understanding the mechanisms through which public health practices and policies may themselves be harmful, such as embracing CSR efforts promoted by industry and adopting framing and interventions that serve to reinforce the dominant narrative based on individualizing understandings of health, emphasizing personal responsibility and ‘free choice’. These will support efforts by some corporate actors to shift blame onto individuals and allow them to absolve themselves of responsibility for the harms caused by their practices or products. Such framings are potentially harmful in and of themselves24 and can be strengthened by focusing on disease causation at the individual level as the sole mechanism of harm.
Reflecting on our engagement with emerging harms
Of equal importance is how we engage with emerging harms—harms are not static, but evolve with changes in social norms, technology and the environment, for example. Two key examples are commercialized gambling and social media, both of which are unprecedented in their nature and scale. Both are driven by highly profitable commercialized industries that can interact with citizens in multiple ways at all times of the day with products of their own design, generally unimpeded by robust safety checks or consideration of citizens’ rights or agency.25,26 Commercial data gathered by these industries on the impacts of their products and practices are used to promote further use and engagement. When considered in this way, arguments that use of a certain gambling or social media product have not been proven to cause a given disease or that harm arises from ‘misuse’ of these products deflects from the wider harms that they create whereby their business models undermine people’s potential for ‘enjoyment of the highest attainable standard of health’.
In these examples and others, the companies involved reject regulatory measures because of a lack of ‘proof’ that they cause harm at the individual level. Yet, the potential for harm, when defined more widely, is apparent from basic reasoning, given how many gambling products and social media platforms impact, often by design, on many pre-requisites for health, including financial resources, relationships, education, employment and housing. These are all areas where the causal chain between exposure, for example home or job loss, and disease is complex and difficult to establish with precision, as well as their ability to promote research subject to conflicts of interest and to undermine the integrity of policymaking. In these cases, there may never be definitive proof, to the standard often demanded in the health field, that a given product in a certain context over a defined time period causes more harm than benefit. Furthermore, definitive proof or accumulation of specific forms of evidence should not be unquestioningly viewed as pre-requisites to acting to prevent harms,27 and demands by vested interests for methodical perfection can be employed to delay or block efforts to prevent harm.28
Further examples include climate change and biodiversity loss, two of the greatest threats to health in the 21st century. While the mechanisms through which these crises impact on health are broad, there is recognition that they undermine the systems and resources that are needed for health to be achieved by all. These mechanisms are far more complex than can be captured by a focus on proving causation between a single exposure and a disease outcome. Even a broader approach, linking extreme weather events or famine to health outcomes, fails to capture the entire range of harms arising from the actions of those most responsible. Climate change and biodiversity loss are profoundly complex issues with diverse perspectives on causes and solutions but limiting our view of what is harmful undermines efforts to address these critical issues. Indeed, the 6th report of working group III of the Intergovernmental Panel on Climate Change describes the ways in which corporate agents attempt to undermine climate change mitigation efforts, from the creation of doubt and targeting lobbying to shifting of responsibility onto individuals and limiting understanding of mitigation through narrow framings that focus on consumer choice and consumption.29 Understanding the harms that can arise from these activities and how they can be countered is critical to addressing climate change, with the activities of the pesticide and other industries being of similar concern in the context of biodiversity loss.
A commitment to challenging our own thinking
It is essential that we remain committed to developing innovative, and dynamic ways of conceptualizing disease, health, causation and harm. This involves recognizing the limits of models that we do use, including the need to ‘avoid the trap of conflating scientific assumptions with reality’ or the ‘individualistic fallacy’, the assumption that individual-level data are sufficient to explain group-level phenomena.2 Of equal importance is a commitment to asking whose interests are served by adopting certain ways of understanding an issue. This is not to suggest that detailed understandings of disease and causation are not critical to advancing our understanding of threats to health, and it is not intended to set us on a path of perpetual inertia that hinders innovation and progress by designating everything as harmful. Opening the dynamic and complex relationships between health, disease, harms, mechanisms and effects, and finally individuals and populations offers opportunities to avoid (re)producing processes and practices and wider social and political systems that hinder the flourishing of people and planet, particularly among those who are already exposed to and suffering from existing harms. History has often shown that what has been labelled as the route to progress and liberation, with little scrutiny of unknowns, uncertainties and vested interests, can ultimately set us back from a health or environmental perspective and/or lock in years of harm or instability.
Health, harms and disease are intimately linked, and their promotion and distribution are determined by the social, political and physical worlds in which people live and work. The complexity of the relationships and intersections of these forces and their outcomes is not to be underestimated but should equally not be ignored. Instead, it calls for ongoing engagement with and scrutiny of how we conceptualize health and explain threats to its realization by everyone. Limiting our thinking constitutes a harm when it obscures evidence on what influences disease and health and maintains ignorance as to what is shaping health in the 21st century and what is needed to ensure everyone flourishes now and over the next 50 years of the Faculty and beyond.
May CI van Schalkwyk,
Marco Zenone,
Nason Maani,
Mark Petticrew,
Martin McKee,
Contributor Information
May C I van Schalkwyk, Faculty of Public Health and Policy, London School of Hygiene and Tropical Medicine, London WC1H 9SH, UK.
Marco Zenone, Faculty of Public Health and Policy, London School of Hygiene and Tropical Medicine, London WC1H 9SH, UK.
Nason Maani, Faculty of Public Health and Policy, London School of Hygiene and Tropical Medicine, London WC1H 9SH, UK.
Mark Petticrew, Faculty of Public Health and Policy, London School of Hygiene and Tropical Medicine, London WC1H 9SH, UK.
Martin McKee, Faculty of Public Health and Policy, London School of Hygiene and Tropical Medicine, London WC1H 9SH, UK.
Funding
MvS is funded by a National Institute for Health Research Doctoral Fellowship (Ref NIHR300156) and is supported by the National Institute for Health Research ARC North Thames. The views expressed in this publication are those of the author(s) and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care. MP and NM are members of the SPECTRUM consortium which is funded by the UK Prevention Research Partnership (UKPRP), a consortium of UK funders [UKRI Research Councils: Medical Research Council (MRC), Engineering and Physical Sciences Research Council (EPSRC), Economic and Social Research Council (ESRC) and Natural Environment Research Council (NERC); British Heart Foundation, Cancer Research UK, Wellcome and The Health Foundation; Government: Scottish Government Chief Scientist Office, Health and Care Research Wales, National Institute of Health Research (NIHR) and Public Health Agency (NI)].
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1. Evans RG, Barer ML, Marmor TR. Why Are Some People Healthy and Others Not? The Determinants of the Health of Populations (1st ed.). Routledge, New York, 1994. [Google Scholar]
- 2. Krieger N. Epidemiology and the web of causation: has anyone seen the spider? Soc Sci Med 1994;39(7):887–903. [DOI] [PubMed] [Google Scholar]
- 3. Krieger N. Proximal, distal, and the politics of causation: what’s level got to do with it? Am J Public Health 2008;98(2):221–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Glasgow S, Schrecker T. The double burden of neoliberalism? Noncommunicable disease policies and the global political economy of risk. Health Place 2015;34:279–86. [DOI] [PubMed] [Google Scholar]
- 5. Popay J, Whitehead M, Hunter DJ. Injustice is killing people on a large scale—but what is to be done about it? J Public Health 2010;32(2):148–9. [DOI] [PubMed] [Google Scholar]
- 6. Kelly MP, Russo F. Causal narratives in public health: the difference between mechanisms of aetiology and mechanisms of prevention in non-communicable diseases. Sociol Health Illn 2018;40(1):82–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rose G. Sick individuals and sick populations. Int J Epidemiol 2001;30(3):427–32 discussion 33-4. [DOI] [PubMed] [Google Scholar]
- 8. Maani N, van Schalkwyk MC, Petticrew M, Galea S. The commercial determinants of three contemporary national crises: how corporate practices intersect with the COVID-19 pandemic, economic downturn, and racial inequity. Milbank Q 2021;99(2):503–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. van Schalkwyk MC, Maani N, Cohen J et al. Our postpandemic world: what will it take to build a better future for people and planet? Milbank Q 2021;99(2):467–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organization . forty-ninth edition (including amendments adopted up to 31 May 2019). Geneva: World Health Organization; 2020. [Google Scholar]
- 11. Krieger N. ENOUGH: COVID-19, structural racism, police brutality, plutocracy, climate change—and time for health justice, democratic governance, and an equitable, sustainable future. Am J Public Health 2020;110(11):1620–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bambra C, Fox D, Scott-Samuel A. Towards a politics of health. Health Promot Int 2005;20(2):187–93. [DOI] [PubMed] [Google Scholar]
- 13. Lecours N, Almeida GE, Abdallah JM, Novotny TE. Environmental health impacts of tobacco farming: a review of the literature. Tob Control 2012;21(2):191–6. [DOI] [PubMed] [Google Scholar]
- 14. Guindon GE, Driezen P, Chaloupka FJ, Fong GT. Cigarette tax avoidance and evasion: findings from the International Tobacco Control Policy Evaluation (ITC) Project. Tob Control 2014;23(suppl 1):i13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shah A, Eminson K, Bogdanovica I, Britton J. The relation between tobacco tax structure and corruption in European Union Member States. Int J Environ Res Public Health 2019;16(16). doi: 10.3390/ijerph16162842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Galea S. Compassion in a time of COVID-19. The Lancet 2020;395(10241):1897–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Abdalla SM, Maani N, Ettman CK, Galea S. Claiming health as a public good in the post-COVID-19 era. Development 2020;63(2):200–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zenone M, Silva D, Smith J, Lee K. How does the British Soft Drink Association respond to media research reporting on the health consequences of sugary drinks? Glob Health 2021;17(1):72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cassidy R. Vicious Games: Capitalism and gambling. London: Pluto Press, 2020. [Google Scholar]
- 20. Proctor RN. Golden Holocaust: Origins of the Cigarette Catastrophe and the Case for Abolition. Berkeley: University of California Press, 2011. [Google Scholar]
- 21. Oreskes N, Conway EM. Merchants of Doubt: How a Handful of Scientists Obscured the Truth on Issues from Tobacco Smoke to Global Warming. New York, NY2010: Bloomsbury Publishing, 2011. [Google Scholar]
- 22. Bergman Å, Becher G, Blumberg B et al. Manufacturing doubt about endocrine disrupter science – A rebuttal of industry-sponsored critical comments on the UNEP/WHO report “State of the Science of Endocrine Disrupting Chemicals 2012”. Regul Toxicol Pharmacol 2015;73(3):1007–17. [DOI] [PubMed] [Google Scholar]
- 23. Goldberg RF, Vandenberg LN. The science of spin: targeted strategies to manufacture doubt with detrimental effects on environmental and public health. Environ Health 2021;20(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Maani N, van Schalkwyk MC, Petticrew M, Buse K. The pollution of health discourse and the need for effective counter-framing. BMJ 2022;377:1128. [DOI] [PubMed] [Google Scholar]
- 25. van Schalkwyk MCI, Petticrew M, Cassidy R et al. A public health approach to gambling regulation: countering powerful influences. Lancet Public Health 2021;6(8):e614–9. [DOI] [PubMed] [Google Scholar]
- 26. Zenone M, Kenworthy N, Maani N. The social media industry as a commercial determinant of health. Int J Health Policy Manag 2022. doi: 10.34172/ijhpm.2022.6840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Schrecker T. Can health equity survive epidemiology? Standards of proof and social determinants of health. Prev Med 2013;57(6):741–4. [DOI] [PubMed] [Google Scholar]
- 28. Hatchard JL, Evans-Reeves KA, Ulucanlar S et al. How do corporations use evidence in public health policy making? The case of standardised tobacco packaging. The Lancet 2013;382:S42. [Google Scholar]
- 29. Intergovernmental Panel on Climate Change . Climate Change 2022 Mitigation of Climate Change, 2022.