FIGURE 3.
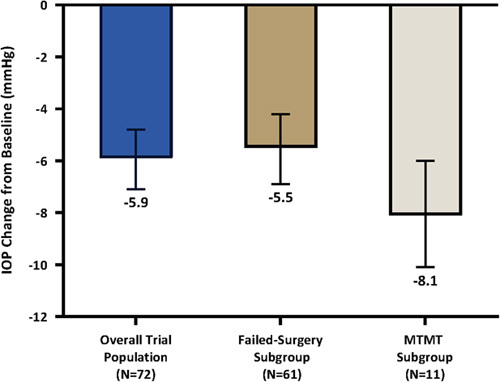
IOP change from baseline effectiveness endpoint: 12-month diurnal IOP change from baseline. Data from intent-to-treat population in all groups. Multiple imputation was used for 1 patient with missing data at month 12. Vertical lines represent 95% CI. The following imputation methods were used for the 12-month mean diurnal intraocular pressure: (1) For patients with hypotony associated with clinically significant findings, cyclodialysis cleft, and/or no stents visible, the worst postoperative IOP on the same or greater number of OHT medication classes as baseline was used. If a patient was on fewer OHT medication classes than baseline, then the baseline IOP was used. (2) For patients with loss of light perception, the observed 12-month MDIOP was used. (3) For patients with IOP-related secondary surgical interventions, the worst postoperative IOP before secondary surgical intervention on the same or greater number of OHT medication classes as baseline was used. If a patient was on fewer OHT medication classes than baseline, then the baseline IOP was used. (4) For patients on more OHT medication classes than at baseline, the worst postoperative IOP on the same or greater number of OHT medication classes as baseline was used. IOP indicates intraocular pressure; MTMT, maximum tolerated medical therapy; OHT, ocular hypotensive.
