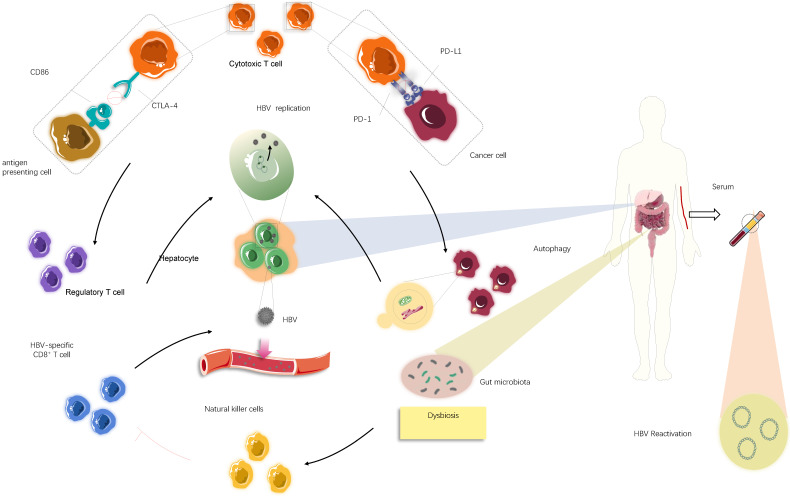
Fig 3.
The underlying mechanism causing HBV reactivation induced by immune checkpoint inhibitors (ICIs). Overall, HBV reactivation has been reported to occur in approximately 4.1% of patients with advanced tumour undergoing ICIs therapies (i.e., anti-PD-1/PD-L1 and anti-CTLA-4 therapies), manifested by the re-detected HBV DNA levels in serum samples. In individuals ever infected with HBV, blockade of PD-1/PD-L1 axis could stimulate autophagic activities of cancer cells, which might be involved in further HBV replication. Apart from that, suppression of CTLA-4 may lead to increase in the frequency of regulatory T cells, thereby creating a context for HBV survival and expansion. In addition to these immediate impacts of immunological systems on HBV fate, most likely dysbiosis of gut microbiota, partly mediated by ICIs treatments, serves an immunological role by activating natural killer cells and in turn driving the exhaustion of HBV-specific T cells, consequently facilitating the release of latent HBV from damaged hepatocyte into circulation.