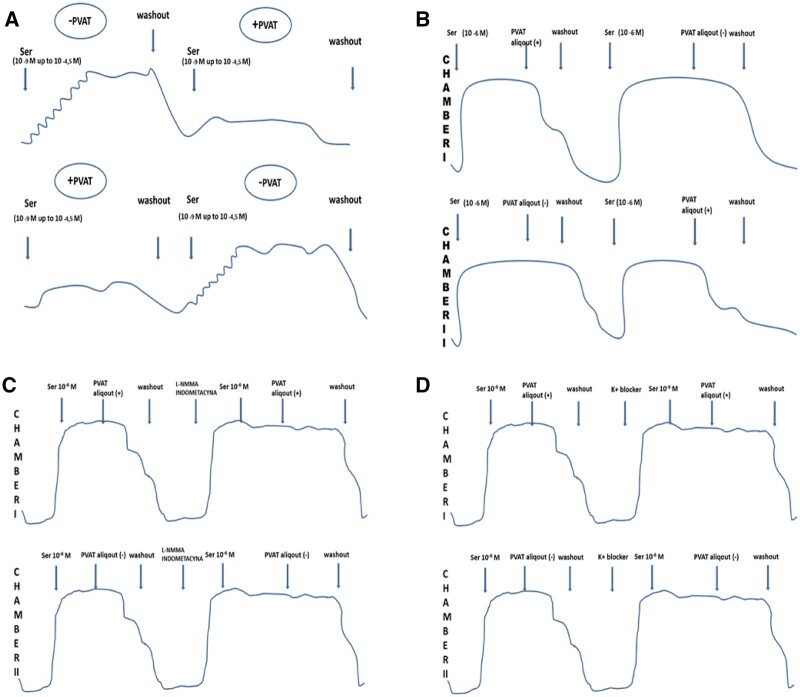
Figure 1:
(A) One segment was incubated with perivascular adipose tissue and the other without perivascular adipose tissue. First, both arterial rings were gradually contracted with serotonin starting from 10−9 M and rising in negative logarithm half-molar cumulative steps up to 10−4.5 M to establish the concentration-effect relationship in the presence/absence of perivascular adipose tissue. After washout and transfer of loose perivascular adipose tissue, the concentration-response curves with the same contractile factor were reconstructed. (B) Both arterial rings were precontracted with a single dose of 10−6 M serotonin. The perivascular adipose tissue tissue was floating freely in the solution during the experiment, presumably releasing adipocyte-derived relaxing factor into the bath. Having achieved a plateau of the contraction to serotonin, the 5-ml perivascular adipose tissue aliquot was added to 1 arterial segment with another one serving as a control. Various levels of relaxation were observed after adding the perivascular adipose tissue aliquot. (C) After washout and a stabilization period, we added NG-monomethyl-l-arginine to the first 5 specimens and indomethacin to the next 5 specimens. After incubation, we observed the contraction of 1 arterial segment in response to a single, submaximal dose of serotonin and then some relaxation associated with the perivascular adipose tissue aliquot. (D) After washout and the stabilization period, we added potassium channel blockers. After incubation, we observed the contraction of 1 arterial segment with a single, submaximal dose of serotonin and then some relaxation/contraction associated with the 5-ml perivascular adipose tissue aliquot. INDO: indomethacin; K+ blocker: potassium channel blocker; l-NMMA: NG-monomethyl-l-arginine; PVAT: perivascular adipose tissue; PVAT aliquot: Krebs–Henseleit solution with incubated PVAT; Ser: serotonine.