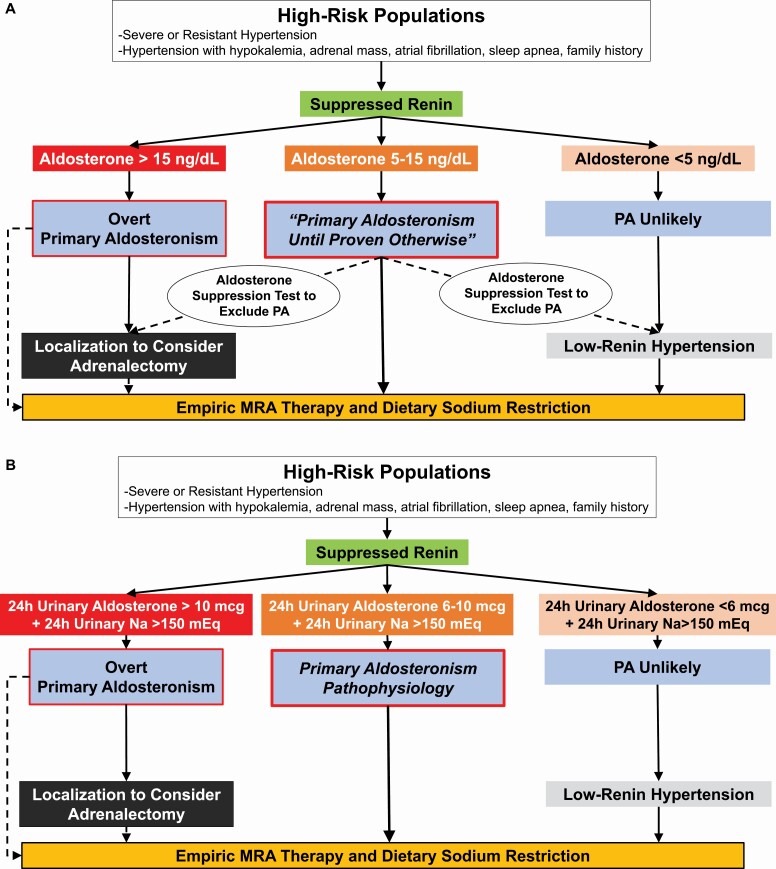
Figure 4.
(a) Pragmatic diagnostic approach for all clinicians. High-risk populations are those with a high pretest probability for having PA. In the context of a suppressed renin, a plasma aldosterone >15 ng/dl essentially confirms the diagnosis of overt PA and clinicians can proceed to localization or empiric MR antagonist therapy. In a high-risk patient with a suppressed renin and a very low aldosterone concentration, <5 ng/dl, PA is unlikely; however, MR antagonist therapy should still be considered as an effective treatment for low-renin hypertension. For all other high-risk patients (suppressed renin and aldosterone 5–15 ng/dl), the diagnostic mindset should be that this is “PA until proven otherwise.” Several options are available, including empiric initiation of MR antagonist therapy and dietary sodium restriction, or an aldosterone suppression test (including a 24-hour urine collection to measure aldosterone and sodium excretion) to exclude the possibility of PA or increase confidence in the diagnosis prior to pursuing localization and possible adrenalectomy. (b) Enhanced diagnostic approach for specialist clinicians. When available, specialists may opt to test high-risk populations with a suppressed renin with a 24-hour urine collection to gain a better integrated assessment of aldosterone production. This can be performed on an ad libitum diet since many patients may already be consuming sufficient dietary sodium, or after dietary sodium loading to ensure a high-sodium balance. Ideally, the desired 24-hour urinary sodium balance should be greater than 150 mEq/24 hours (reflective of a dietary intake of ~3.5 g of sodium per day). A 24-hour urinary aldosterone excretion rate of >10 mcg in this context likely confirms PA, whereas values between 6 and 10 mcg are suggestive of PA pathophysiology that is likely to still respond to targeted therapy. Twenty-four-hour urinary aldosterone excretion rates less than 6 mcg suggest PA is unlikely, but MR antagonist therapy may still be beneficial for low-renin hypertension. Abbreviations: MR, mineralocorticoid receptor; PA, primary aldosteronism.