Abstract
Introduction and importance
To summarize the clinical manifestations and treatment of bilateral persistent first intersegmental artery (PFIA) in a patient with posterior subluxation of atlantoaxial joint.
Case presentation
A-85-year-old woman with a two-months history of aggravating of gait disturbance and finger clumsiness was referred to our hospital. Magnetic resonance imaging revealed posterior subluxation of the atlantoaxial joint and spinal cord compression at C1 level. Three-dimensional computed tomography angiography (CTA) of cervical spine showed bilateral PFIA and left side high-riding VA. Because of the high risk of vertebral artery injury with posterior arch resection and lateral mass screw insertion due to the presence of PFIA, as well as the bony fragility of the cervical spine and the fact that the posterior atlantoaxial subluxation was reduced in the flexed position, the posterior occipito-thoracic fixation without posterior arch resection in the mildly flexed cervical position was underwent. The postoperative course was uneventful and her neurological symptoms improved gradually after surgery.
Clinical discussion
PFIA is a very rare condition representing between 0.01 % and 1.8 %. Most patients with this condition have a unilateral persistent segmental artery, but in a small minority of cases it occurs bilaterally. It may be more difficult to resect of posterior arch or insert the C1 lateral mass screw in cases of PFIA.
Conclusion
The best way to avoid IVAI may be careful examining the abnormal running of VA preoperatively especially on 3D-CT of cervical spine with arteriography and not to choose a technique with a high risk of VA injury.
Keywords: Bilateral persistent first intersegmental artery, High riding vertebral artery, Iatrogenic vertebral artery injury, Atlantoaxial subluxation, Occipitothoracic fixation, Cervical spondylotic myelopathy
Highlights
-
•
We summarize the clinical manifestations and treatment of bilateral persistent intersegmental artery in a patient with posterior atlantoaxial subluxation after subaxial cervical laminoplasty.
-
•
Occipitothoracic fixation without resection of posterior arch of C2 was underwent uneventfully.
-
•
The abnormal running of vertebral artery preoperatively especially on 3-dimentional CT should be carefully examined.
1. Introduction
Recent advances in instrumentation enable us to safely and effectively manage the atlantoaxial instability. However, upper cervical instrumentation can result in iatrogenic vertebral artery (VA) which may cause cerebellar and/or brain stem infarction and death by exsanguination [1], [2], [3], [4]. Surgeons should completely understand the relationship between the VA and osseous structures at the craniovertebral junction especially in existence of anomalous course to decrease the risk of VA injury during the surgical procedures.
Several types of anomalous course of VA at the craniovertebral junction are well documented. There are two main types of anomalous course, one is intraosseous running abnormalities, such as high-riding VA (HRVA; located too medially, too posteriorly, and/or too high at C2 isthmus), and the other is extraosseous running abnormalities, such as fenestration and persistent first intersegmental artery (PFIA) [5], [6], [7]. PFIA is a very rare condition representing between 0.01 % and 1.8 % [5], [6], [7], [8]. We report a case of bilateral PFIA accompanied with left HRVA in a patient with posterior atlantoaxial subluxation following subaxial laminoplasty.
2. Case report
A-85-year-old woman with a two-months history of aggravating of gait disturbance and finger clumsiness was referred to our hospital. She had a medical history of hypertension and no contributory family history. The patient underwent C3–7 laminoplasty for subaxial cervical spondylotic myelopathy with finger clumsiness and gait disturbance two years before the visit. Neurological examination revealed some weakness in her upper and lower extremities and normal sensation. Deep tendon reflexes of biceps brachii, patellar and Achilles tendon were hyperreflexia. Bilateral scapulohumeral reflexes, Hoffman and Babinski reflexes were positive. The Japanese Orthopedic Association (JOA) score for cervical myelopathy was 8 points.
Lateral radiograph of cervical spine on neutral position showed that posterior subluxation of atlantoaxial joint associated with os odontoideum (Fig. 1). The subluxation of atlantoaxial joint was reduced in cervical flexion. T2-weighted magnetic resonance imaging (MRI) revealed posterior subluxation of the atlantoaxial joint and spinal cord compression at C1 level (Fig. 2). Three-dimensional computed tomography angiography (CTA) of cervical spine showed bilateral vertebral arteries running just below the C2 pedicle (PFIA) and left reconstructed parasagittal image on CTA revealed left side HRVA (Fig. 3).
Fig. 1.

Lateral radiograph of cervical spine on neutral position showed that posterior subluxation of atlantoaxial joint associated with os odontoideum.
Fig. 2.
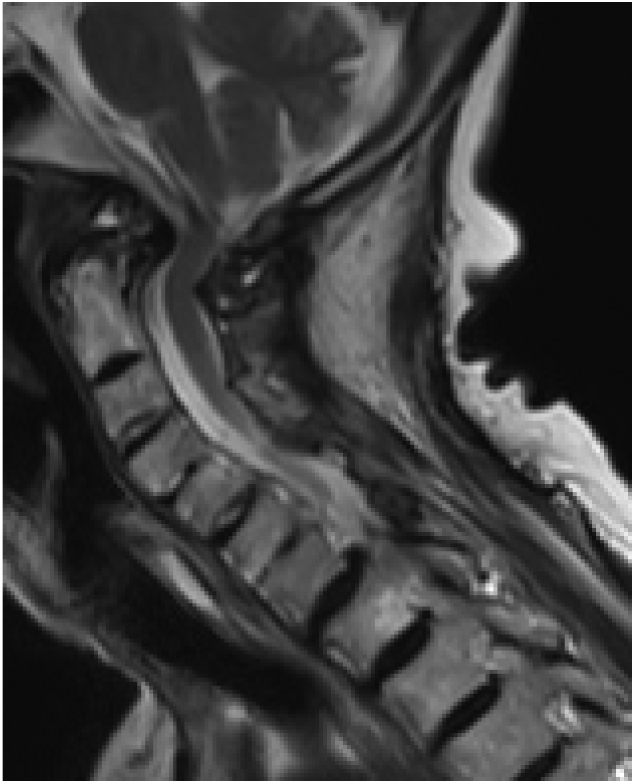
T2-weighted MR image of the cervical spine revealed posterior subluxation of the atlantoaxial joint and spinal cord compression at C1–2.
Fig. 3.
A, Posterior view on three-dimensional CTA showing bilateral persistent first intersegmental artery (black arrow). B, Left reconstructed parasaggital image on CTA revealing high riding VA (white arrow).
The placement of lateral mass screws of axis and posterior arch resection were judged to carry an extremely high risk of vertebral artery injury because of bilateral vertebral arteries running just below and inner the C2 pedicle. The C2 anchor was considered to allow placement of a pedicle screw only on the right side because of abnormal intraosseous running of the left vertebral artery at C2 vertebra (HRVA). Furthermore, radiographs revealed that the whole cervical spine was severely osteoporotic. Based on the above, it was considered that the upper thoracic spine rather than the cervical spine was appropriate for the lowest instrumented vertebrae. A posterior occipitothoracic fixation with mild cervical flexion with the caudal anchor being in the thoracic spine was scheduled.
The operation was started under general anaesthesia in the supine position with head elevated mildly and the cervical spine in a mildly flexed position under fluoroscopically confirmation.
A median longitudinal skin incision was made from the external occipital protuberance to Th5, and the paraspinal muscles were dissected to expose the occipital bone and laminae. Three screws were placed in the median occipital bone, pedicle screws on the right C2 and on Th1 ∼ Th4 bilaterally, then connected to a rod. After cortical bone stripping from the occipital bone to the thoracic spine, the iliac and local bones were grafted (operated by H.S.) (Fig. 4). The operation time was 5 h and 7 min, the estimated blood loss was 650 ml and no transfusion was required.
Fig. 4.

Postoperativel lateral radiograph of cervical spine on neutral position showed the occipitothoracic fixation (O-T4) with mild cervical flexion.
The tracheal tube was extubated in the operating room, and the patient did not complain of respiratory distress. The patient had anorexia for 10 days postoperatively and was referred to otolaryngology department to check for suspected dysphagia. Swallowing function evaluation and laryngoscopic examination showed no dysphagia. The O—C2 angle on the lateral radiograph of the cervical spine decreased from 19° preoperatively to 0° at 2 weeks postoperatively, and the anterior-posterior diameter of the pharynx at C3 level on cervical X-p decreased from 17.9 mm to 13.3 mm respectively. The appetite improved from 2 weeks postoperatively. At 3 weeks post-operatively, she was able to walk with a cane and was discharged from hospital. The MRI taken three months postoperatively confirmed adequate spinal cord decompression at C1 level (Fig. 5).
Fig. 5.

The MRI taken three months postoperatively confirmed adequate spinal cord decompression at C1 level.
Her neurological symptoms improved gradually after surgery. She was awkward in eating with chopsticks, writing and buttoning preoperatively, but she could do them smoothly and walk with forward gaze postoperatively. Her JOA score increased from 8 points preoperatively to 15 points at the one-year follow-up.
3. Discussion
PFIA is a very rare condition representing between 0.01 % and 1.8 % [5], [6], [7], [8]. Most patients with this condition have a unilateral PFIA, but in a small minority of cases it occurs bilaterally [9]. It may be more difficult to insert the C1 lateral mass screw in cases of PFIA, which is an anatomically abnormal vertebral artery running caudal to the C1 lateral mass, than in cases where it runs cephalad.
Iatrogenic vertebral artery injury (IVAI) during cervical spine surgery is an extremely rare complication, but can result in massive bleeding, cerebellar or brain stem infarction and intraoperative death by exsanguination [1], [2], [3], [4]. Overall incidence of iatrogenic vertebral artery injury in cervical spine surgery is reported to be 0.07–0.14 % [2], [4], [10]. Among intraoperative vertebral artery injuries in cervical spine surgery, incidence of IVAI of posterior surgery at the C1 and C2 levels are indeed 34.5–53.4 % [2], [4], [10]. In multicenter studies, Lee reported the incidence rate of IVAI was 1.35 % (7/518cases) in C1, C2 posterior screw fixation [4]. The reported mean estimated blood loss of IVAI during posterior cervical spine surgery was 770–2410 ml (range: 100-8000 ml) [4], [10], [11]. Some of the cases reported by Neo have bled more than 8500 ml [10].
Hong reported the deep groove on the inner aspect of the C1 posterior arch where the aberrant V3 segment courses into the spinal canal in cases of a PFIA or fenestrated VA [9]. When the vertebral arteries run just below and inner the bilateral C1 pedicles (PFIA), as in this case, the risk of IVAI may be extremely high during laminectomy of posterior C1 arch or insertion of lateral mass screw of C1. Aota reported a case of vertebral artery injury due to the tapper tip being displaced headward during tapping at the time of C1 lateral mass screw insertion [12]. If the PFIA is presented, the C1 lateral mass screw insertion should be avoided. Carmody reported a good postoperative result of bilateral PFIA in a patient with odontoid fracture operated with C1 posterior arch screw [13]. Kashiro underwent C1–2 posterior fixation with transarticular screws in a case of axial subluxation with PFIA utilizing the spinal navigation system [14]. The operation performed in the above two cases are technically demanding and require a spinal navigation system which is not permanently available in usual facilities. The best way to avoid IVAI may be careful examining the abnormal running of VA preoperatively especially on 3D-CT of cervical spine with arteriography and not to choose a technique with a high risk of VA injury.
Postoperative dyspnea and/or dysphagia after occipitocervical or occipitothoracic fusion are rare but can result in life threating [15]. Occipitocervical fusion in a cervical flexed position has been reported to cause postoperative dysphagia and breathing problems [16], [17]. Miyata reported a 40 % decrease in the anterior-posterior diameter of the pharynx when the O—C2 angle decreased by 10° after O—C2 fusion compared to preoperatively, resulting in dyspnea and dysphagia [18].
In this case, in addition to the original os odontoideum, the cervical protrusion caused by intervertebral fusion and paraspinal muscle atrophy after subaxial laminoplasty seems to have concentrated mechanical stress on the upper cervical spine, resulting in the posterior atlantoaxial subluxation. The posterior atlantoaxial subluxation was reduced in cervical flexion. Because of the high risk of vertebral artery injury with posterior arch resection and lateral mass screw insertion due to the presence of PFIA, as well as the bony fragility of the cervical spine and the fact that the posterior atlantoaxial subluxation was reduced in the flexed position, the posterior occipitothoracic fixation without posterior arch resection in the mildly flexed cervical position was underwent. Although the O—C2 angle on the lateral radiograph of the cervical spine decreased from 19° preoperatively to 0° at 2 weeks postoperatively, and the anterior-posterior diameter of the pharynx at C3 level on the lateral radiograph of the cervical spine decreased from 17.9 mm to 13.3 mm respectively, she did not suffer from dysphagia or breathing disturbance and showed considerable neurological improvement.
This case has been reported in line with the SCARE 2020 criteria [19].
4. Conclusion
The best way to avoid IVAI may be careful examining the abnormal running of VA preoperatively especially on 3D-CT of cervical spine with arteriography and not to choose a technique with a high risk of VA injury.
Sources of funding
No source of funding.
Ethical approval
This paper as a case report, therefore does not require ethics approval.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Hisashi Serikyaku: operator, manuscript drafting, writing, literature search.
Shoichiro Higa: Colleague who assisted in the operation.
Tetsuya Yara: Colleague who assisted in the operation.
Registration of research studies
None.
Guarantor
Hisashi Serikyaku.
Provenance and peer review
Not commissioned, externally peer-review.
Declaration of competing interest
This work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Sources of support that require acknowledgement: The manuscript submitted does not contain information about medical device(s)/drug(s). No funds were received in support of this work. No relevant financial activities outside the submitted work.
References
- 1.Maughan P.H., Elhadi A.M., Martirosyan N.L., et al. Multimodality management of vertebral artery injury susutained during cervical or craniocervical surgery. Oper. Neurosurg. 2013;73:271–282. doi: 10.1227/01.neu.0000431468.74591.5f. [DOI] [PubMed] [Google Scholar]
- 2.Lunardini D.J., Eskander M.S., Even J.L., et al. Vertebral artery injuries in cervical spine surgery. Spine J. 2014;14:1520–1525. doi: 10.1016/j.spinee.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 3.Hsu W.K., Kannan A., Mai T.S., et al. Epidemiology and outcomes of vertebral artery injury in 16582 cervical spine surgery patients: an AO spine North America multicenter study. AO Spine. 2017;7:21S–27S. doi: 10.1177/2192568216686753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee C.H., Hong J.T., Kang D.H., et al. Epidemiology of iatrogenic vertebral artery injury in cervical spine surgery:21 multicenter studies. World Neurosurg. 2019;126:e1050–e1054. doi: 10.1016/j.wneu.2019.03.042. [DOI] [PubMed] [Google Scholar]
- 5.Yamazaki M., Okawa A., Furuya T., et al. Anomalous vertebral arteries in the extra- and intraosseous regions of the craniovertebral junction visualized by 3-dimensional computed tomographic angiography. Spine. 2012;37:E1389–E1397. doi: 10.1097/BRS.0b013e31826a0c9f. [DOI] [PubMed] [Google Scholar]
- 6.Wakao N., Takeuchi M., Nishimura M., et al. Vertebral artery variation and osseous anomaly at the C1–2 level diagnosed by 3D CT angiography in normal subjects. Neuroradiology. 2014;56:843–849. doi: 10.1007/s00234-014-1399-y. [DOI] [PubMed] [Google Scholar]
- 7.O’Donnell C.M., Child Z.A., Anderson P.A., et al. Vertebral artery anomalies at the craniovertebral junction in the US population. Spine. 2014;39:E1053–E1057. doi: 10.1097/BRS.0000000000000447. [DOI] [PubMed] [Google Scholar]
- 8.Zhang H., Chai W., Wang S., et al. Persistent first intersegmental artery(PFIA) visualized by three-dimensional computed tomography angiography in chinese population. Int. J. Surg. 2018;52:233–236. doi: 10.1016/j.ijsu.2018.02.038. [DOI] [PubMed] [Google Scholar]
- 9.Hong J.T., Lee S.W., Son B.C., et al. Analysis of anatomical variations of bone and vascular structures around the posterior atlantal arch using threedimensional computed tomography angiography. J. Neurosurg. Spine. 2008;8:230–236. doi: 10.3171/SPI/2008/8/3/230. [DOI] [PubMed] [Google Scholar]
- 10.Neo M., Fujibayashi S., Miyata M., et al. Vertebral artery injury during cervical spine surgery. Spine. 2008;33:779–785. doi: 10.1097/BRS.0b013e31816957a7. [DOI] [PubMed] [Google Scholar]
- 11.Madawi A.A., Casey A.T.H., Solanki G.A., et al. Radiological and anatomical evaluation of the atlantoaxial transarticular screw fixation technique. J. Neurosurg. 1997;86:961–968. doi: 10.3171/jns.1997.86.6.0961. [DOI] [PubMed] [Google Scholar]
- 12.Aota Y., Honda A., Uesugi M., et al. Vertebral artery injury in C-1 lateral mass screw fixation. J. Neurosurg. Spine. 2006;5:554. doi: 10.3171/spi.2006.5.6.554. [DOI] [PubMed] [Google Scholar]
- 13.Carmody M.A., Martin M.D., Wolfla C.E. Persistent first intersegmental vertebral artery in association with type 2 odontoid fracture:surgical treatment utilizing a novel C1 posterior arch screw:case report. Neurosurgery. 2010;67:E210–E213. doi: 10.1227/01.NEU.0000370012.34424.30. [DOI] [PubMed] [Google Scholar]
- 14.Kashiro H., Wada K., Yui M., et al. Atlantoaxial fixation in a patient with bilateral persistent first intersegmental vertebral artery anomaly using an o-arm navigation system: a case report. SSRR. 2019;3:196–198. doi: 10.22603/ssrr.2018-0065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matsuyama Y., Kawakami N., Yoshihira H., et al. Log-term results of occipitothoracic fusion surgery in RA patients with destruction of the cervical spine. J. Spinal Disord. Tech. 2005;18:S101–S106. doi: 10.1097/01.bsd.0000127700.29969.e6. [DOI] [PubMed] [Google Scholar]
- 16.Yoshida M., Neo M., Fujibayashi S., et al. Upper-airway obstruction after short posterior occipitocervical fusion in a flexed position. Spine. 2007;32:E267–E270. doi: 10.1097/01.brs.0000259977.69726.6f. [DOI] [PubMed] [Google Scholar]
- 17.Tagawa T., Akeda K., Asanuma Y., et al. Upper airway obstruction associated with flexed cervical position after posterior occipitocervical fusion. J. Anesth. 2011;25:120–122. doi: 10.1007/s00540-010-1069-0. [DOI] [PubMed] [Google Scholar]
- 18.Miyata M., Neo M., Fujibayashi S., et al. O-C2 angle as apredictor of dyspnea and/or dysphagia after occipitocervical fusion. Spine. 2009;34:184–188. doi: 10.1097/BRS.0b013e31818ff64e. [DOI] [PubMed] [Google Scholar]
- 19.Franchi T., Agha R.A., Sohrabi C. Guideline: updating consensus surgical case report (SCARE) guidelines. Int. J. Surg. 2020;2020(84):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]



