Abstract
Background
COVID-19 has created a burden on the healthcare system globally. Severe COVID-19 is linked with high hospital mortality. Data regarding 30-day in-hospital mortality and its factors has not been explored in southwestern Uganda.
Methods
We carried out a retrospective, single-center cohort study, and included all in-patients with laboratory-confirmed, radiological, or clinical severe COVID-19 admitted between April 2020 and September 2021 at Mbarara Regional Referral Hospital (MRRH). Demographic, laboratory, treatment, and clinical outcome data were extracted from patients’ files. These data were described comparing survivors and non-survivors. We used logistic regression to explore the factors associated with 30-day in-hospital mortality.
Results
Of the 283 patients with severe COVID-19 admitted at MRRH COVID-19 unit, 58.1% were male. The mean age ± standard deviation (SD) was 61±17.4 years; there were no differences in mean age between survivors and non-survivors (59 ± 17.2 versus 64.4 ±17.3, respectively, p=0.24) The median length of hospital stay was 7 (IQR 3–10) days (non-survivors had a shorter median length of stay 5 (IQR 2–9) days compared to the survivors; 8 (IQR 5–11) days, p<0.001. The most frequent comorbidities were hypertension (30.5%) and diabetes mellitus (30%). The overall 30-day in-hospital mortality was 134 of 279 (48%) mortality rate of 47,350×105 with a standard error of 2.99%. The factors associated with 30-day in-hospital mortality were age: 65 years and above (aOR, 3.88; 95% CI, 1.24–11.70; P =0.020) a neutrophil to lymphocyte ratio above 5 (aOR, 4.83; 95% CI, 1.53–15.28; P =0.007) and oxygen requirement ≥15L/min (aOR, 15.80; 95% CI, 5.17–48.25; P <0.001).
Conclusion
We found a high 30-day in-hospital mortality among patients with severe forms of COVID-19. The identified factors could help clinicians to identify patients with poor prognosis at an early stage of admission.
Keywords: severe, COVID-19, 30-day in hospital mortality
Introduction
The year 2020 will always be remembered as the “COVID-19” (Coronavirus disease 2019) year. COVID-19 is a viral infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and is currently the world leading cause of mortality from a single infectious agent.1 The novel coronavirus is a strain that had not been previously identified in humans2 but, has since caused a huge healthcare burden in both developed and less-developed countries.3
A study in Wuhan that analyzed patients hospitalized with COVID-19 pneumonia revealed older age, presence of comorbidities like cardiovascular diseases, symptoms like dyspnea, fatigue and headache, high white cell counts, elevated creatinine, d-dimers, and hypoxia as the main risk factors associated with mortality.4
In Uganda, there have been slightly above 167,000 cases with 3626 deaths.5 Previous reports show that persons older than 65 years had significantly higher COVID-19 mortality rates compared to younger individuals, and men carried a higher risk of death from the same when compared to women.6 A study conducted at the national referral hospital in Uganda which involved hospitalized COVID-19 patients who mostly had severe and critical diseases found that more than one-third of the patients died of the illness. Overall, 174 (37%) patients died. Predictors of all-cause in-hospital mortality were as follows; age ≥50 years, oxygen saturation at admission of ≥92% and admission pulse rate of ≥100 beats per minute. The risk of death was 1.4-fold higher in female participants compared with their male counterparts.7
Patients admitted with severe COVID-19 have high risk of death especially in a low-resource setting like Mbarara. This is mostly due to the limited human resource, lack of equipment, inadequate consumables among others and competition from other infectious diseases like Tuberculosis, HIV and Malaria.8
Despite the several publications that have emerged on COVID-19, data from Mbarara Regional Referral Hospital regarding the factors associated with mortality in this special category of patients had not been explored. Most studies examining the factors associated with mortality in patients with severe COVID-19 were done mostly in high-income countries with majority of the studies stating parameters like interleukin (IL) −6 levels, troponins which are not readily available in resource limited settings like Mbarara.
A clear understanding of the predictors of mortality in our setting leads to interventions that target modifiable factors to reduce mortality in our weak healthcare system. In this study, our main goal is to determine the 30-day in-hospital mortality and its associated factors among patients admitted with severe COVID-19.
Methodology
We retrospectively retrieved data from files of patients with severe forms of COVID-19 that had been admitted between April 2020 and September 2021 at Mbarara regional referral hospital (MRRH). Mbarara Regional Referral Hospital is in Mbarara City, which is approximately 260 kilometres from Kampala, the capital city. It has a bed capacity of 350 and serves south-western -Uganda and neighbouring countries of Democratic Republic of Congo, Tanzania and Rwanda. The hospital additionally serves as the teaching hospital for Mbarara University of Science and Technology (MUST) the second oldest medical school in Uganda. This hospital was south-western Uganda’s COVID-19 treatment centre of excellence. The COVID-19 treatment unit has a high dependency unit and an Intensive Care Unit to support people with severe COVID-19 disease. The treatment team comprises of specialist physicians, anaesthesiologists, critical care nurses, physiotherapists, and registered nurses. All COVID-19 diagnostics and adjunct laboratory tests were done at the hospital.
COVID-19 was defined by either having laboratory confirmation, clinical or radiological diagnosis according to the WHO 2020 definition.9 Patients were considered to have severe COVID-19 disease if they had SpO2 <90% on room air at sea level, a respiratory rate of >30 breaths/min, PaO2/FiO2 <300 mm Hg, or lung infiltrates (ground glass opacities) >50%9 Acute respiratory distress syndrome (ARDS) was defined as having worsening respiratory distress despite receiving maximum oxygen flow rate using a face mask with a reservoir bag.10
Patients transferred to another treatment unit or discharged against medical advice were excluded. Data extracted from the patients’ files included socio-demographics, clinical parameters, underlying comorbidities, laboratory values, 30-day in-hospital mortality and treatment received according to the Uganda national treatment guidelines for COVID–19 that included oxygen therapy, IV ceftriaxone and azithromycin, vitamin D3, IV fluids, anticoagulation and assisted ventilation according to the degree of severity.10 This study was approved by the Mbarara University of Science and Technology Research and Ethics Committee (Ref; MUREC 1/7) Mbarara Regional Referral Hospital administration. All methods in this study were carried out in accordance with relevant guidelines and regulations and the declaration of Helsinki was fully followed in the conduct of this study.
Statistical Analysis
Data were entered and stored in a web-based data analysis application, REDCap (Vanderbilt University, Nashville, NT, USA). Statistical analyses were carried out in STATA (STATA Corp, College Station, Texas, USA version 16). Descriptive statistics of eligible participants were reported as medians with interquartile ranges stratified by clinical outcomes (died versus survived). Statistical significance tests included t-tests, nonparametric tests, or chi-square tests as appropriate. Logistic regression was used and considered a p value of <0.05 as significant.
Results
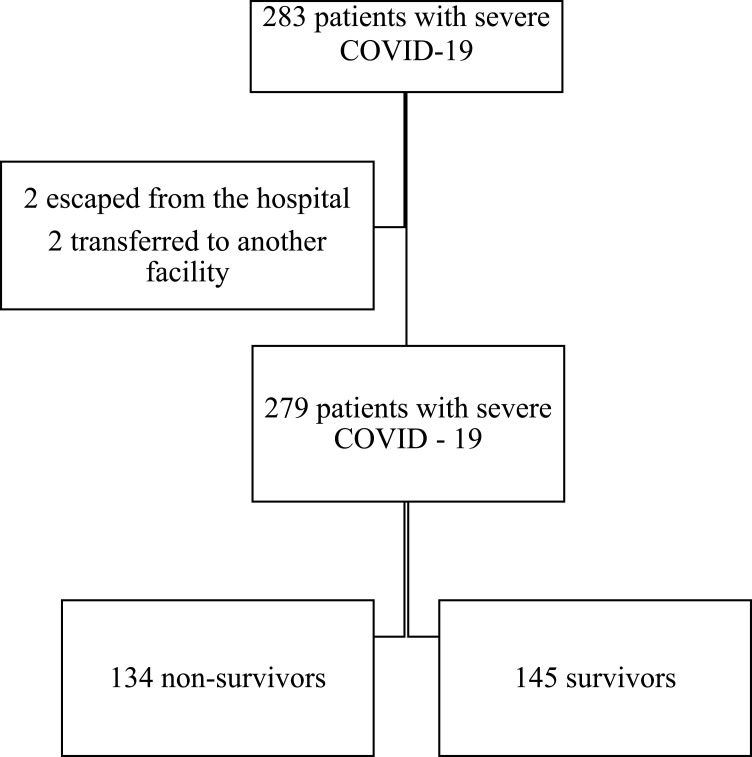
Between March 2020 and September 2021, a total of 283 patients with severe COVID-19 were admitted at MRRH COVID-19 treatment unit. Four patients were excluded; two were discharged against medical advice and the other two were transferred to another facility before 30 days of hospitalisation as shown in Figure 1.
Figure 1.
Study flow of patients.
Of the 279 patients enrolled, majority 162 (58.1%) were male, the mean age ± standard deviation (SD) was 61±17.4 years. There was no noticeable mean difference in age between those who survived (59±17.2) (n years ± SD) and those who did not survive 64.4±17.3 (n years ± SD) to the 30-day mark p=0.243. The overall median (interquartile range (IQR)) length of hospital stay was 7 (IQR 3–10) days. Non-survivors had a shorter median length of stay 5 (IQR 2–9) days compared to the survivors 8 (IQR 5–11) days, p<0.001. The most common comorbidities were Hypertension (30.5%) and diabetes (30%). Other comorbidities were; chronic liver disease, chronic cardiac disease and chronic kidney disease. The details of the patients’ baseline characteristics are shown in Table 1.
Table 1.
Demographic Characteristics of Study Patients at Admission
| Characteristic | N | Overall | Survivors | Non-Survivors | P-value | ||
|---|---|---|---|---|---|---|---|
| N | N | ||||||
| Men n (%) | 279 | 162 (58.1) | 145 | 89 (61.4) | 134 | 73 (54.5) | 0.243 |
| Age, mean (± SD) -years- | 279 | 61 (17.4) | 145 | 59 (17.2) | 134 | 64.4 (17.3) | 0.243 |
| Smoking, n (%) | 133 | 30 (22.6) | 81 | 20 (24.7) | 52 | 10 (19.2) | 0.426 |
| Length of hospital stay median (IQR) | 278 | 7 (3,10) | 144 | 8 (5,11) | 134 | 5 (2,9) | <0.001 |
| Obesity, n (%) | 279 | 9 (3.2) | 145 | 4 (44.5) | 135 | 5 (55.6) | 0.646 |
| Diabetes, n (%) | 279 | 83 (30) | 145 | 39 (47) | 135 | 44 (53) | 0.278 |
| Hypertension, n (%) | 279 | 85 (30.5) | 145 | 41 (28.3) | 135 | 44 (32.8) | 0.408 |
| Chronic lung disease, n (%) | 278 | 7 (2.5) | 145 | 5 (3.4) | 133 | 2 (1.5) | 0.278 |
| HIV, n (%) | 130 | 14 (10.8) | 77 | 7 (9.1) | 53 | 7 (13.2) | 0.457 |
| Others, n (%) | 279 | 26 (9.3) | 145 | 9 (6.2) | 134 | 17 (12.7) | 0.781 |
Note: (Bolded text indicates the significant findings).
Abbreviations: HIV, Human Immunodeficiency disease; IQR, Interquartile Range; SD, Standard deviation.
Signs and Symptoms at Admission
The overall median oxygen saturation was 81% (IQR, 67–87) with non survivors having a lower median compared to the survivors (76% (IQR, 55–85) versus 85% (IQR, 75–88), P<0.001). Cough and shortness of breath where the most common presenting complaints at admission (86% and 75% respectively), followed by fever (43%) with more survivors presenting with fever 72 (57.7%) compared to the non survivors 48 (35.8%), p=0.02). As shown in Table 2.
Table 2.
Signs and Symptoms of Participants at Admission
| Characteristics | N | Overall | Survivors | Non-Survivors | P-value | ||
|---|---|---|---|---|---|---|---|
| N | N | ||||||
| 269 | 91 (34.0) | 141 | 95 (19) | 128 | 99 (17) | 0.968 | |
| Systolic pressure, mean (± SD)-mmHg | 271 | 126 (22) | 139 | 126 (21) | 132 | 126 (23) | 0.466 |
| Respiratory rate, mean (SD) -bpm- | 163 | 31 (8) | 85 | 30 (9) | 78 | 32 (6) | 0.914 |
| Axillary temperature mean (± SD) –℃ | 134 | 37.4 (1.3) | 78 | 37.3 (1.3) | 56 | 37.4 (1.2) | 0.634 |
| Oxygen saturation on room air, median (IQR) | 274 | 81 (67, 87) | 144 | 85 (75, 88) | 130 | 76 (55, 85) | <0.001 |
| Fever, n (%) | 279 | 120 (43) | 145 | 72 (57.7) | 134 | 48 (35.8) | 0.02 |
| Cough, n (%) | 279 | 240 (86) | 145 | 129 (89) | 134 | 111 (82.9) | 0.14 |
| Headache, n (%) | 279 | 35 (12.5) | 145 | 20 (13.8) | 134 | 15 (11.2) | 0.513 |
| Dyspnea, n (%) | 279 | 210 (75.3) | 145 | 109 (75.2) | 134 | 101 (75.4) | 0.969 |
| Chest pain, n (%) | 279 | 101 (36.3) | 145 | 54 (37.2) | 134 | 47 (35.1) | 0.707 |
| Fatigue, n (%) | 279 | 79 (28.3) | 145 | 37 (25.5) | 134 | 42 (31.3) | 0.281 |
| Altered level of consciousness, n (%) | 279 | 22 (7.9) | 145 | 8 (5.5) | 134 | 14 (10.5) | 0.127 |
Note: (Bolded text indicates the significant findings).
Abbreviations: IQR, Interquartile Range; SD, Standard deviation; C, degree Celsius; bpm, breath per minute; mmHg, millimeters of mercury.
Laboratory Parameters at Admission
Non-survivors presented with a higher median creatinine 1.2 (IQR, 1.0–1.8) compared to survivors 1.1 (IQR, 0.9–1.3) (p=0.017), reduced platelet count (p=0.386) and high absolute neutrophil count (p=0.0278). A high neutrophil lymphocyte ratio was found in those who did not survive to hospital discharge 7.3 (IQR, 3.0–10.1) versus 6.0 (IQR, I 4.2–9.4). The laboratory parameters are shown in Table 3.
Table 3.
Laboratory Values at Admission
| Characteristic | N | Overall | Survivors | Non Surviors | P-value | ||
|---|---|---|---|---|---|---|---|
| N | N | ||||||
| Creatinine, median (IQR) -mg/dl- | 152 | 1.2 (0.9,1.6) | 73 | 1.1 (0.9, 1.3) | 79 | 1.2 (1.0, 1.8) | 0.017 |
| AST, median (IQR) -U/L- | 51 | 55.9 (33.0,99.6) | 27 | 42.3 (38.3,71.0) | 24 | 66.3 (39.5, 112) | 0.51 |
| CRP, median (IQR) -mg/dl- | 83 | 117 (48,200) | 33 | 95.3 (48, 182.5) | 50 | 143.0 (48, 200) | 0.27 |
| Leukocytes, median (IQR) −10^3/ µL - | 189 | 8.2 (6.0,115) | 93 | 7.4 (5.8, 11.0) | 96 | 8.9 (6.0, 12.59) | 0.094 |
| Hemoglobin, mean (± SD) -g/dl- | 186 | 13.5 (2.5) | 90 | 13.6 (2.3) | 96 | 13.4 (2.7) | 0.317 |
| Platelets, median (IQR) µL | 165 | 191 (150,269) | 85 | 216 (167, 275) | 80 | 214 (140, 251) | 0.0386 |
| Absolute lymphocyte count, median (IQR)-10^3/ µL | 175 | 1.1 (4.4,11.4) | 85 | 1.1 (0.7, 1.6) | 90 | 1.0 (0.7, 1.6) | 0.676 |
| Absolute neutrophil count, median (IQR)-10^3/ µL | 175 | 6.7 (4.4,11.4) | 75 | 6.0 (4.2, 9.4) | 84 | 7.7 (4.9, 12.4) | 0.0278 |
| Neutrophil-lymphocyte ratio, median (IQR) 10^3/µL | 174 | 5.5 (1.9,10.5) | 85 | 4.0 (1.3, 8.6) | 89 | 7.3 (3.0, 10.1) | 0.001 |
| RBS at Admission median,(IQR) mmol/L | 94 | 11.5 (6.8,17.0) | 46 | 11.2 (6.4,15.6) | 48 | 12.0 (6.9,17.2) | 0.782 |
| D-dimer, median (IQR) -ng/mL | 109 | 1.65 (0.7,3.6) | 52 | 1.9 (0.5, 4.52) | 57 | 1.5 (1.0, 2.66) | 0.971 |
Note: (Bolded text indicates the significant findings).
Abbreviations: IQR, Interquartile Range; SD, Standard deviation; CRP, C-reactive protein; ng/mL, Nanograms per milliliter; RBS, Random Blood Sugar; g/dl, gram/deciliter; mg/dl, milligrams per deciliter; mmol/L, millimoles per liter; AST, Aspartate Transaminase.
The 30-Day in-Hospital Mortality Rate and Associated Factors
The overall 30-day in-hospital mortality rate in patients admitted with severe COVID-19 was (134 of 279) 48%, mortality rate of 47,350×105 with a standard error of 2.99%. The factors associated with the 30-day in-hospital mortality were old age (65 years and above) (aOR, 3.88; 95% CI, 1.24–11.70; P =0.020) a neutrophil to lymphocyte ratio ≥ 6 (aOR, 4.83; 95% CI, 1.53–15.28; P =0.007) and oxygen requirements ≥ 15 liters per (aOR, 15.80; 95% CI, 5.17–48.25); P <0.001The detail of the univariate and multivariate analyses are shown in Table 4.
Table 4.
Risk Factors Associated with 30-Day in-Hospital Mortality
| Variable | Unadjusted Estimate | Adjusted Estimate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | aOR | 95% CI | P value | |
| Age≥65 years | 1.87 | 1.12–3.0 | 0.01 | 3.88 | 1.24–11.70 | 0.020 |
| Fever | 0.56 | 0.35–0.91 | 0.020 | 0.63 | 0.22–1.82 | 0.393 |
| Male gender | 0.75 | 0.48–1.21 | 0.244 | |||
| Diabetes | 1.33 | 0.79–2.22 | 0.277 | 1.21 | 0.34–3.05 | 0.965 |
| Hypertension | 1.24 | 0.74–2.06 | 0.409 | |||
| Smoking | 0.72 | 0.36–1.71 | 0.467 | |||
| Obesity | 1.36 | 0.36–5.12 | 0.647 | |||
| Oxygen saturation < 80% | 3.3 | 2.00–5.4 | < 0.001 | 1.63 | 0.53–5.03 | 0.398 |
| Neutrophil Lymphocyte ratio ≥6 | 3.02 | 1.62–5.62 | <0.001 | 4.83 | 1.53–15.28 | 0.007 |
| Creatinine≥1.5 mg/dl | 2.31 | 1.1–4.86 | 0.27 | |||
| Maximum oxygen requirement during hospitalization ≥15L/min | 12.58 | 6.95–22.74 | <0.001 | 15.80 | 5.17–48.25 | <0.001 |
| ARDS | 4.61 | 2.55–8.35 | <0.001 | 2.22 | 0.66–7.44 | 0.225 |
Notes: Adjusted by age, male gender, fever, NLR, ARDS, Oxygen saturation < 80%, Creatinine≥1.5, DM. (Bolded text indicates the significant findings).
Abbreviations: OR, odds ratio; aOR, adjusted Odds ratio; CI, confidence interval; NLR, Neutrophil Lymphocyte ratio; ARDS, Acute Respiratory Distress Syndrome; DM, Diabetes Mellitus.
Discussion
The main finding of this study was that the 30-day in-hospital mortality in patients admitted with severe COVID-19 at Mbarara Regional referral hospital was high. Almost half of the patients admitted with severe COVID-19 pneumonia died in hospital within 30 days of admission. This is high compared to that reported from our national referral hospital and from another regional referral hospital in northern Uganda (34% and 4.8%, respectively).7,11 The difference in mortality is attributed to the patient population included in the two studies. Our study included adult patients with severe COVID –19 hypoxia defined by oxygen saturation less than 90%. The other studies included patients with less severe forms of COVID –19. Another large prospective and multicenter study done in Africa, reported a very high mortality in severely ill COVID-19 patients (48.2%), striking a significant similarity with our findings and it is higher than the average of the reported global mortality (31.5%).12
On multivariate logistic regression, the odds of death during hospitalization were higher among patients who were aged ≥ 65 years which is in agreement with findings in other studies.4,12 The most possible explanation is that old age is associated with reduced T and B cell function leading to unchecked viral replication as well as increased production of pro-inflammatory cytokines responsible for the increased mortality.13
A Neutrophil to Lymphocyte (NLR) ratio of ≥6 was associated with higher odds of death compared to a ratio less than 6. This was similar to findings from previous studies that reported that the cut-off value of 5.94 and above had 3.9 higher odds of death during hospitalization.14
An elevation in the NLR is due to direct attack of the virus on CD4+ T-cells which are important in the recruitment of other lymphocytes to fight the infection.15 Further studies have elucidated that lymphocytes are involved in the regulation of the inflammatory response and a decrease in their number may give raise to high inflammatory states that are associated with poor outcomes.16
Much as diabetes and hypertension have been described as independent risk factors of death in previous studies,17 in this study the two comorbidities were not associated with 30-day in-hospital mortality. This agrees with that previously reported in New York in which diabetes and hypertension were not associated with in-hospital mortality in critically ill COVID-19 patients. A Ugandan cohort also did not find any significant association of diabetes and hypertension with mortality in severe COVID-19 patients.4,18
Patients whose oxygen requirement during hospitalisation was ≥15 litres /min had higher odds of death compared to those who required less. This is because these patients were more hypoxic and hence more likely to die, agreeing with data reporting that hypoxemia is significantly associated with in-hospital mortality in patients with severe COVID-19.19
Limitations
The retrospective nature of our study and the small sample size is a major limitation; we had missing data in some of the key variables and some of the laboratory parameters that have been associated with mortality like interleukin 6 and cardiac troponins were not measured.
Conclusion
Severe COVID-19 has a high 30-day in-hospital mortality. Age ≥65 years, NLR ≥6 and maximum oxygen requirement during hospitalization ≥15L/min were the factors associated with mortality during hospitalization. More studies are needed to explain why people with the above characteristics are at risk of death.
Acknowledgments
We thank the study team, hospital administration and the clinicians and nurses who accepted to part of this study.
Abbreviations
BP, Blood pressure; CD, Cluster of Differentiation; CI, Confidence interval; aOR, Adjusted Odds Ratio; OR, Odds Ratio; COVID –19, Corona Virus Disease 2019; CVD, Cardiovascular disease; DBP, Diastolic blood pressure; HTN, Hypertension; ICU, Intensive Care Unit; MRRH, Mbarara regional referral hospital; NLR, Neutrophil to lymphocyte Ratio; SBP, Systolic blood pressure; WHO, World Health Organization.
Data Sharing Statement
The datasets used during this study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
This study was approved by the Mbarara University of Science and Technology’s faculty review board and institutional ethics review board. A waiver for consent was sought from the necessary boards. All methods in this study were carried out in accordance with relevant guidelines and regulations.
Consent to Publish
All authors consented to publish this work.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
- 1.Figure WHOJGF. Global excess deaths associated with COVID-19: January 2020–December 2021; 2022.
- 2.Wan Y, Shang J, Graham R, Baric RS, Li FJ. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol. 2020;94(7):e00127–e00120. doi: 10.1128/JVI.00127-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walker PG, Whittaker C, Watson OJ, et al. The impact of COVID-19 and strategies for mitigation and suppression in low-and middle-income countries. Science. 2020;369(6502):413–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Du R-H, Liang L-R, Yang C-Q, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J. 2020;55(5):2000524. doi: 10.1183/13993003.00524-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organisation. Uganda situation; 2022. Available from: https://covid19.who.int/region/afro/country/ug. Accessed December 1, 2022.
- 6.Yanez ND, Weiss NS, Romand J-A, Treggiari MM. COVID-19 mortality risk for older men and women. BMC Public Health. 2020;20(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bongomin F, Fleischer B, Olum R, et al. High mortality during the second wave of the coronavirus disease 2019 (COVID-19) pandemic in Uganda: experience from a national referral COVID-19 treatment unit. Open Forum Infect Dis. 2021;8(11):ofab530. doi: 10.1093/ofid/ofab530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alene KA, Elagali A, Barth DD, et al. Spatial codistribution of HIV, tuberculosis and malaria in Ethiopia. BMJ Global Health. 2022;7(2):e007599. doi: 10.1136/bmjgh-2021-007599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organisation. HO R&D blueprint novel coronavirus. Contract No.: January 21, 2020; 2020.
- 10.Ministry of Health. Uganda National guidelines for clinical management of COVID-19. Contract No.: April,2020; 2020.
- 11.Baguma S, Okot C, Alema NO, et al. Factors associated with mortality among the COVID-19 patients treated at Gulu Regional Referral Hospital: a retrospective study. Front Public Health. 2022;10. doi: 10.3389/fpubh.2022.841906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biccard BM, Gopalan PD, Miller M, et al. Patient care and clinical outcomes for patients with COVID-19 infection admitted to African high-care or intensive care units (ACCCOS): a multicentre, prospective, observational cohort study. Lancet. 2021;397(10288):1885–1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Opal SM, Girard TD, Ely EW. The immunopathogenesis of sepsis in elderly patients. Clin Infect Dis. 2005;41(Supplement_7):S504–S512. doi: 10.1086/432007 [DOI] [PubMed] [Google Scholar]
- 14.Yildiz H, Castanares-Zapatero D, Pierman G, et al. Validation of neutrophil-to-lymphocyte ratio cut-off value associated with high in-hospital mortality in COVID-19 patients. Int J Gen Med. 2021;14:5111. doi: 10.2147/IJGM.S326666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.King AH, Mehkri O, Rajendram P, Wang X, Vachharajani V, Duggal A. A high neutrophil-lymphocyte ratio is associated with increased morbidity and mortality in patients with Coronavirus Disease 2019. Crit Care Explorat. 2021;3(5). doi: 10.1097/CCE.0000000000000444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heffernan DS, Monaghan SF, Thakkar RK, Machan JT, Cioffi WG, Ayala A. Failure to normalize lymphopenia following trauma is associated with increased mortality, independent of the leukocytosis pattern. Crit Care. 2012;16(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehraeen E, Karimi A, Barzegary A, et al. Predictors of mortality in patients with COVID-19-a systematic review. Eur J Integrat Med. 2020;40:101226. doi: 10.1016/j.eujim.2020.101226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cummings MJ, Baldwin MR, Abrams D, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. 2020;395(10239):1763–1770. doi: 10.1016/S0140-6736(20)31189-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mansab F, Donnelly H, Kussner A, Neil J, Bhatti S, Goyal DK. Oxygen and mortality in COVID-19 pneumonia: a comparative analysis of supplemental oxygen policies and health outcomes across 26 countries. Front Public Health. 2021;9. doi: 10.3389/fpubh.2021.580585 [DOI] [PMC free article] [PubMed] [Google Scholar]