Abstract
Benign paroxysmal positional vertigo (BPPV) is a widely recognized vestibular disorder which occurs with short periods of paroxysmal vertigo produced in specific positions. This investigation targets contrasting the adequacy of two unique moves utilized in the management of posterior canal BPPV (PC-BPPV). One is traditional procedure, Epley repositioning maneuver (ERM) and another is Gans Repositioning maneuver (GRM). To compare the efficacy of maneuvers on vertigo and dizziness for people with posterior canal BPPV using Dix hallpike test, Vertigo Analogue Scale (VAS) and Dizziness Handicap Inventory (DHI), 100 people will be recruited confirming to eligibility criteria for this two group (ERM group and GRM group) participant and assessor blinded randomized control study. After Participants will be randomly assigned to either group, the respective maneuver will be performed one or two times until the symptoms resolve. Post maneuver instructions will be demonstrated to each subject nicely. Then, family history will be taken using a questionnaire. Outcomes will be taken once after giving maneuver and then, once after 1 month of treatment. Main outcome variables include VAS, DHI, and Dix hallpike test negativity. If the results indicate that Gans Manoeuvre is equivalent to Epley manoeuvre, then in older and postural compromised BPPV patients who has cervical related neck stiffness and pain or any other disorder, where Epley manoeuvre can not be given as it involves neck extension and rotation, Gans manoeuvre can be given. Trial registration: Clinical Trials Registry (CTRI/2019/10/021681). October 16, 2019.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12070-021-02762-y.
Keywords: Randomized controlled trial, Rehabilitation, Vertigo
Introduction
Vertigo is the sensation of self-motion (of head/body) when no self-motion is occurring and in case of Benign Paroxysmal Positional Vertigo (BPPV), it mostly comes with head movement with respect to gravity. BPPV occurs when there is displacement of otoconia from its fixed position (utricular macula) to floating in semi-circular canals. Posterior canal BPPV (PC-BPPV) is most frequent among the three canals. There are repeated and short periods of vertigo with movement especially on changing the position of head like on turning in bed. Vertigo duration is typically less than 1 min. Nausea and upbeating rotational nystagmus beating towards the involved ear semicircular canal are also associated with vertigo [1, 2]. Dix- hallpike test is the test used to diagnose the PC-BPPV and the side of ear involved. In this, the assessor turns the patient’s head 45 degree towards the ear tested and then taking him to supine position with head extended up to 20 degree. Examiner can either put a pillow below the patient’s upper back or hang his head off the bed giving hands’ support to maintain hyperextension of neck. Test is positive if patient has subjective vertigo with latency of few seconds and paroxysmal, up beating rotatory nystagmus towards the involved ear. An up-beating, rotary nystagmus is specific for posterior canal BPPV due to its connection to the inferior rectus and superior oblique extraocular muscles [3, 4].
Epley Canalith Repositioning (ECR) is the maneuver used for treating posterior canal BPPV since long time. BPPV is basic in mature age; these patients have comorbid factors like cervical spondylosis, vertebra-basilar insufficiency, low back pain, obesity. These elements are supposed to be considered during performing diagnostic as well as treatment maneuvers. Side-lying test is utilized as a legitimate option for surveying BPPV rather than Dix–Hallpike test (DH) as an analytic test in patients with comorbid factors [5]. Hyperextension of the neck is contraindicated for patients with cervical related disorders; however, this position is very important in Epley. Gans Repositioning Manuever (GRM) has been designed to manage such patients. The GRM consolidates the side-lying move as its primary position with no hyper-extension of neck [6]. As per the National Ambulatory Medical Care Survey, if lifetime occurrence of BPPV is thought of, then 7% out of 17% cases of BPPV from 42% of the total population with dizziness, will have BPPV eventually in life [7]. One study revealed almost 5% of BPPV patients had close family members who additionally experienced BPPV [8].
As per the updated 2008 guideline from the American Academy of Otolaryngology-Head and Neck Surgery Foundation evidence -based recommendations to the BPPV, the quality of care and outcomes for BPPV should be improved by improving the accurate and efficient diagnosis of BPPV, reducing the inappropriate use of vestibular suppressant medications, decreasing the iapropriate use of ancillary testing such as radiographic imaging, and increasing the use of appropriate therapeutic reposting manoeuvres. To fulfil the purpose of this guideline, there is a strong need to search the accurate diagnosis as well as the most effective canalith repositioning maneuvers that suits every age group population [9]. This study will be aimed at discovering the equality of Gans Repositioning Manoeuvre (GM) to Epley Manoeuvre (EM) in the management of posterior canal BPPV so that GM can also be used as an effective treatment manoeuvre for patients with posterior canal BPPV. Second objective is to find out any familial likelihood in the occurrence of BPPV.
Materials and Methods
Design and Registration
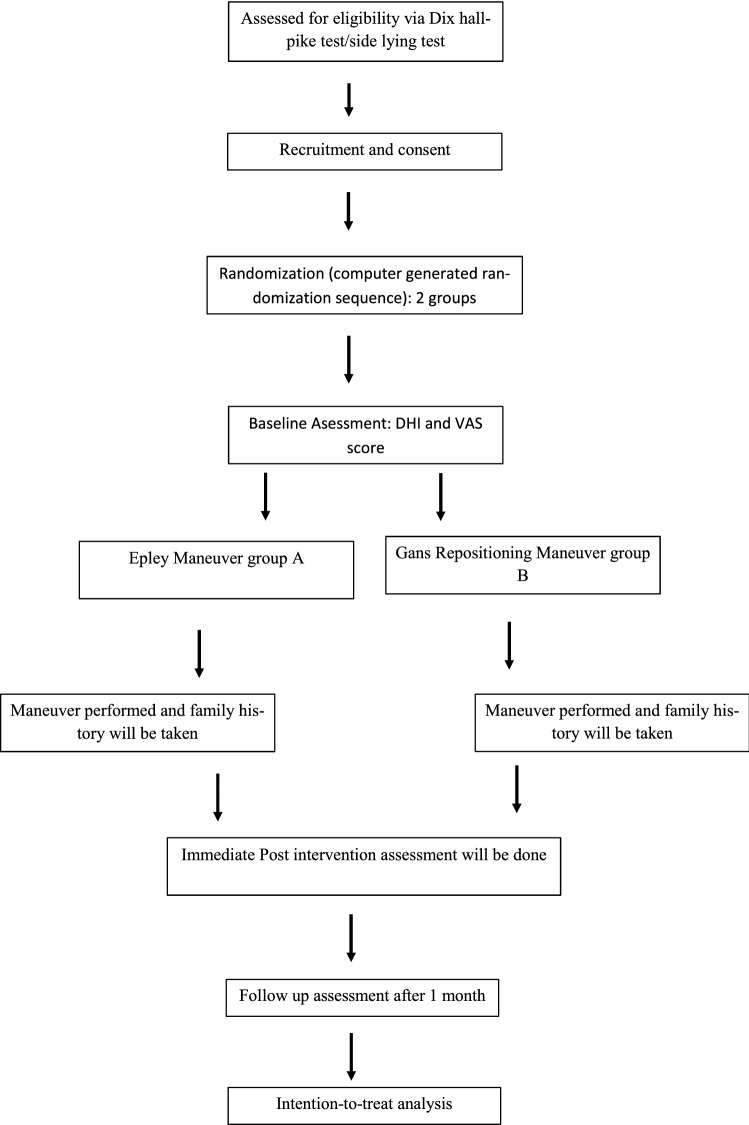
This study will be double blind (assessor and participant) randomized controlled trial (RCT). Figure 1 explains the procedure of the study.
Fig. 1.
Procedure of the study
Study Setting and Participants
Study will be conducted in Neurology department, Institute of Medical Sciences, Banaras Hindu University, Varanasi, India. Sample size is determined based on a pilot study done on 20 patients with PC-BPPV. Each group having 10 subjects, depending on the results, sample size was calculated to be 60 patients. Considering the loss to follow-up, total 100 patients, 50 in each group will be recruited in this study, based on the following inclusion and exclusion criteria. Special attention will be paid to the similarity in various parameters of both groups. We will be including all age group patients who has BPPV and also giving them one of both the manoeuvres irrespective of their age. This is to clarify and prove that Gans repositioning manoeuvre can be performed over all age group patients just like Epley manoeuvre. We will take into consideration the familial occurrences of the problem also by taking family history with the help of a questionnaire (Fig. 2).
Fig. 2.
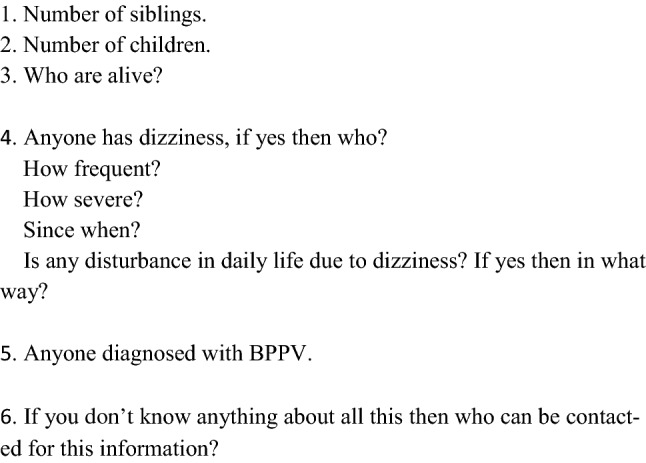
Patient history about family
Inclusion Criteria
Diagnosed unilateral or bilateral PC-BPPV with the help of symptoms and a positive Dix-Hallpke (DH) test or positive side-lying test whichever patient is able to perform.
The Dix-Hallpike test will be considered positive if vertigo and nystagmus (up-beating, rotary towards affected ear) develops and stays for below 1 min, at a latency of few seconds.
Patients shall have normal Central Nervous System examination.
Age 18 and above.
Participants should have the ability to follow verbal instructions.
Exclusion Criteria
Patients with vestibular neuritis, labyrinthine diseases and systemic disease.
Patients with other canal BPPV.
Patients taking any drugs currently causing dizziness, drowsiness and light headedness.
Patients consuming anti-vertigo medications.
Procedures
Informed consent (Appendix 1(Online Supplementary material)) will be obtained from each patient. Patients will be selected randomly to Epley group and Gans group as per the treatment maneuvers they will undergo. Before the recruitment, a blinded investigator will create a simple randomization sequence with the help of computer, held in sealed, opaque, and consecutively numbered envelopes and then assign participants in either group. In this way, participants will be blinded to the treatment procedure they will undergo. Therapists who will perform the manoeuvre will not be blinded to treatment allocation. The data analysts and the intervention outcome assessors will be blinded to the allocation of participants and treatment maneuver.
A questionnaire called Dizziness Handicap Inventory (DHI) [10, 11] (Appendix 2(Online Supplementary material)), negative D-H Test and Vertigo Analogue Scale (VAS) [12] (Appendix 3(Online Supplementary material)) score will be used for the efficacy of treatment modality. We will do the Dix hallpike test before the application of either maneuver. Maneuvers will be performed to both the groups. Maneuvers will be repeated until the nystagmus and vertigo becomes absent on Dix-Hallpike test or side-lying test.
Epley Repositioning Maneuver (ERM) [1, 2]
Patient is sitting on the bed with legs extended.
He turns the head 45 degrees to the involved side.
He lies on bed in supine position with head turned and neck extended up to 20 degrees.
He then turns his head 90 degrees to the other side (normal side).
He turns the whole body along with head to another 90 degrees on the same side, into the bed. His face is downward now.
Finally, the patient is seated straight.
Patient has to hold each position for 30 s to 1 min.
Gans-repositioning Maneuver (GRM) [6]
Patient is sitting on the edge of bed.
He turns his head 45 degree towards normal side, and lie down sideways on involved side.
He turns his whole body to the opposite side into the bed. Face in downward position.
He moves his head side to side two to three times.
Sit upright with head straight.
Post-maneuver instructions will be given in both verbal and written form2:
Avoid neck bending for the next 24 h (wear cervical collor).
Sleep in a semi-inclined position of 30 to 40 degree for 2 days.
Avoid lying on the treated/affected side.
Adherence monitoring to the post-maneuver instructions will not be done.
Immediately after 20 min of performing the maneuvers, post maneuver assessments of both groups will be conducted by the blinded assessor. Follow-up visits will be advised after 1 month of intervention.
Familial Incidence
All patients’ relatives will be interviewed and examined directly. Patients’ relatives showing BPPV symptoms but having negative Dix–Hallpike test will be excluded. In the questionnaire [13], we will ask the patients about their first degree family members whether any of them is diagnosed with BPPV by doctors or have vertigo. If any relative comes with similar symptoms, we will call them and test them personally to find if they have BPPV.
Primary Outcome Measures
Effectiveness of Epley and Gans Maneuvers will be determined on the basis of resolution or improvement in vertigo and nystagmus that we will come to know by testing them with dix hallpike test. Presence (yes) and absence (no) will be the two probable outcomes.
Secondary Outcome Measures
We will also score Visual Analog Scale (VAS) from 0 to 10 where 0 indicates no subjective vertigo, and scoring of 10 indicates the severe vertigo. The VAS is a reliable indicator of the magnitude of vertigo [12]. Dix hallpike Inventory questionnaire (DHI) is a 25 item scale, scores range from 0 to 100, measuring the functional, emotional and physical effects of dizziness and imbalance [10, 11]. There is no data reporting the adverse events of these maneuvers except persistence of vertigo that too when repositioning maneuvers are unsuccessful or BPPV recur. Still, we will conduct the adverse events monitoring on the third day of manoeuvre by making a phone call to the patient.
Data Analysis
Data analysis will be done using SPSS latest version, once data collection completes. Demographic characteristics of the participants will be determined through descriptive data analysis with means and standard deviations. A two-tailed analysis, with a 0.05 significance level and 95% confidence intervals will be considered. Intention-to-treat principle including all participants, who received either maneuver, will be applied for the analysis of research data. improvement difference between the groups will be conducted by using Two-way repeated measures analysis of variance (ANOVA); treatment measures will be named as inter-group variables. The scoring of each participant at baseline and after treatment will be recorded and listed, and the mean estimation of both groups will be determined. At that point, values of sum of squares of deviation from mean, degree of freedom, and mean square will be calculated.
Discussion
According to researches, BPPV is the commonest reasons for dizziness. Its yearly frequency has been accounted to be 64 cases for each 100,000 populaces [4]. If this study proves in future that Gans maneuver will as effective as Epley maneuver in treating patients with PC-BPPV, then it will be most beneficial for such patients of BPPV who are suffering from cervical related disorders like stenosis, scoliosis, restricted mobility, radiculopathy, postural dysfunction, osteoporosis, and also spinal cord injuries like conditions as they cannot even undergo the treatment maneuver.
Three studies are conducted on this hybrid approach. M. Wanees et al. investigated the effect of Gans Repositioning maneuver (GRM) with and without post maneuver instructions and found no difference, they had very small sample size [14]. A. Richard et al. examined the difference between GRM and Semont liberatory maneuver (SLM) [6]. Alia Saberi et al. conducted the study to find out the difference between GRM and ERM in 73 patients with 1 week follow-up [15]. As they mentioned in their result that longer time follow-up can be done in future to examine the reversibility of symptoms or recurrence of vertigo and in our study, we will follow the patients after 1 month. Their sample size was also smaller. The results obtained from the data gathered once the study is completed, will be of great clinical significance in the field of medical research. Vertigo patients will get immediate relief after giving manoeuvre without any supportive therapy that is going to add not only scientific but also economical, social and individual value to this project. Also, if we find that Gans Manoeuvre is equivalent to Epley manoeuvre, in older and postural compromised BPPV patients who has cervical related neck stiffness and pain or any other disorder, where Epley manoeuvre can not be given as it involves neck extension and rotation, Gans manoeuvre can be given. This will also make people and practitioners more aware about this new technique of treatment for BPPV.
Conclusion
Epley manoeuvre has been widely used for the treatment of posterior canal BPPV and has become particularly popular. The complication that has been seen highly after giving Epley manoeuvre, is cervical pain. This problem can be avoided if we use Gans manoeuvre instead of Epley manoeuvre for PC-BPPV. In this study, as we will take similar patients in both groups on factors like age, gender, duration of symptoms and history of BPPV. Therefore, the results of this study will be generalised to all age groups and both genders. If the Gans manoeuvre is equivalent to Epley manoeuvre according to the results of the study, then in old patients and patients with cervical and lumbar problems, Gans manoeuvre as treatment, will clearly be more suitable considering its lesser complications.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Indian Council of Medical Research, New Delhi.
Funding
No funding required.
Declarations
Conflict of interest
No conflict of interest.
Ethical Approval
The study is registered at the Clinical Trials Registry (CTRI/2019/10/021681) on October 16, 2019 and is also approved by the Institutional ethical committee of Institute of Medical Sciences, Banaras Hindu University, Varanasi-UP, India.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Deepika Joshi, Email: drdeepikajoshi73@gmail.com.
Vyom Gyanpuri, Email: vyom.physio@gmail.com.
Abhishek Pathak, Email: abhishekpathakaiims@gmail.com.
Rameshwar Nath Chaurasia, Email: goforrameshwar@gmail.com.
Vishwambhar Singh, Email: singhvishwambhar@gmail.com.
Neetu Rani Dhiman, Email: gyanpurineetu@gmail.com.
References
- 1.Mandala M (2017) Bedside examination of the vestibular and ocular motor system-level 2: how to diagnose and treat BPPV. In: 3rd congress of the European academy of neurology 2017, 24–27 June
- 2.Argaet EC, Bradshaw AP, Welgampola MS. Benign Positional Vertigo, its diagnosis, treatment and mimics. Clin Neurophysiol Pract. 2019;4:97–111. doi: 10.1016/j.cnp.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dix MR, Hallpike CS. Pathology, symptomatology and diagnosis of certain disorders of the vestibular system. Proc R Soc Med. 1952;45:341–354. doi: 10.1177/003591575204500604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zainun Z, Zakaria MN, Sidek D, Ismail Z. Determivation of sensitivity & specificity of Dix Hallpike test (DHT) in peripheral vestibular disordered subjects. Int Med J. 2013;20(2):1–2. [Google Scholar]
- 5.Cohen HS. Side-Lying as an alternative to the Dix-Hallpike test of the posterior canal. Otolo Neurotol. 2004;25:130–134. doi: 10.1097/00129492-200403000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Roberts RA, Gans RE, Montaudo RL. Efficacy of a new treatment maneuver for posterior canal benign paroxysmal positional vertigo. J Am Acad Audiol. 2006;17:598–604. doi: 10.3766/jaaa.17.8.6. [DOI] [PubMed] [Google Scholar]
- 7. Nelson C, Mclemore T (1988) The national ambulatory medical care survey, 1975–81 and 1985 trend. Vital Health Stat 93:1–50 [PubMed]
- 8.Mizukoshi K, Watanabe Y, Shojaku H, Okubo J, Watanabe I. Epidemiological studies on benign paroxysmal positional vertigo in Japan. Acta Otolaryngol Stockh Suppl. 1988;447:67–72. doi: 10.3109/00016488809102859. [DOI] [PubMed] [Google Scholar]
- 9.Bhattacharyya Neil, et al. Clinical practice guideline: benign paroxysmal positional vertigo (update) Otolaryngol Head Neck Surg. 2017;156(3):S1–S47. doi: 10.1177/0194599816689667. [DOI] [PubMed] [Google Scholar]
- 10.Jacobson GP, Newman CW. The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1990;116:424–427. doi: 10.1001/archotol.1990.01870040046011. [DOI] [PubMed] [Google Scholar]
- 11.Yorke A, Ward I, Vora S, Combs S, Keller-Johnson T. Measurement characteristics and clinical utility of the Dizziness Handicap Inventory among individuals with vestibular disorders. Arch Phys Med Rehabil. 2013;94:2313–2314. doi: 10.1016/j.apmr.2013.07.007. [DOI] [Google Scholar]
- 12.Dannenbaum E, Chilingaryan G, Fung J. Visual vertigo analogue scale: an assessment questionnaire for visual vertigo. J Vestib Res. 2011;21(3):153–159. doi: 10.3233/VES-2011-0412. [DOI] [PubMed] [Google Scholar]
- 13.Martin G, Ayyagari S, Khattar V. The familial incidence of benign paroxysmal positional vertigo. J Otolaryngol. 1998;118:774–777. doi: 10.1080/00016489850182422. [DOI] [PubMed] [Google Scholar]
- 14.Badawy WMA, Gad El-Mawla EK, Chedid AEF, Mustafa AHA. Effect of a hybrid maneuver in treating posterior canal benign paroxysmal positional vertigo. J Am Acad Audiol. 2015;26:138–144. doi: 10.3766/jaaa.26.2.4. [DOI] [PubMed] [Google Scholar]
- 15.Saberi A, Nemati S, Sabnan S, Mollahoseini F, Kazemnejad E. A safe-repositioning maneuver for the management of benign paroxysmal positional vertigo: gans versus Epley maneuver; a randomized comparative clinical trial. Eur Archives Otorhinolaryngol. 2016;274(8):2973–2979. doi: 10.1007/s00405-016-4235-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.