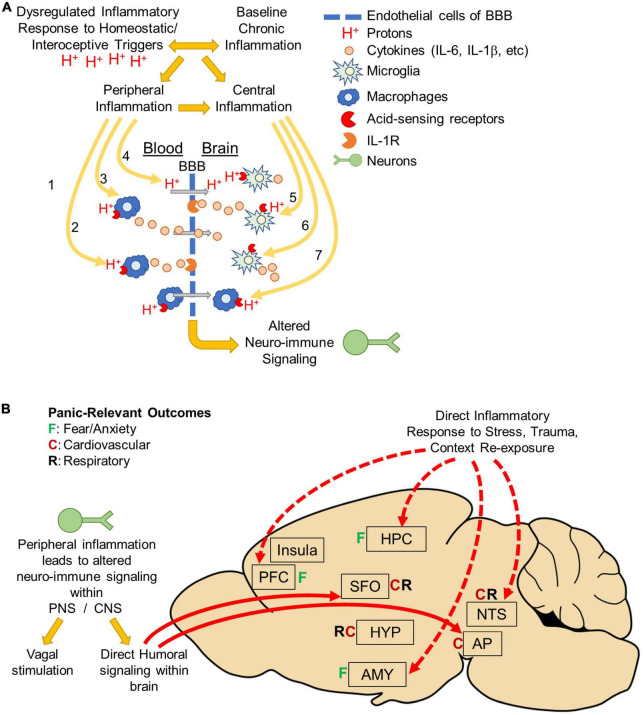
FIGURE 2.
Body to brain signaling: Mechanisms of acidosis evoked peripheral and central inflammation: (A) panic disorder is associated with dysregulated inflammatory responses to homeostatic/interoceptive triggers like acidosis. Panic disorder is also associated with baseline chronic inflammation. Regardless of which inflammatory response occurs initially, either can facilitate the development of the other and result in peripheral and central inflammation. Acidosis could lead to altered neuroimmune signaling through a variety of mechanisms. In the periphery, acidosis may activate acid-sensing receptors on peripheral macrophages. This could lead to either (1) macrophage infiltration across the blood brain barrier (BBB), (2) cytokine release that activates cytokine receptors on endothelial cells, or (3) release of cytokines that cross the BBB. Peripheral acidosis could acidify the brain via protons (H+) that cross the BBB and activate acid-sensing receptors on microglia. Alternatively, acidosis could occur directly within the brain (5) activating acid-sensing receptors on microglia resulting in cytokine release and activation of cytokine receptors on endothelial cells or (6) directly on neurons or other cell types. It is also possible that acidosis could activate acid-sensing receptors on peripheral macrophages that have previously infiltrated the brain, possibly as a result of prior trauma or other risk factor (disease, etc.). Ultimately, Inflammation within the brain is thought to drive emotional, behavioral and physiological responses that occur during panic attacks and increase vulnerability to develop panic disorder. (B) Peripheral inflammation can alter neuronal activity either by neuro-immune signaling occurring either in the periphery or directly in brain. In the periphery, neuro-immune signaling could result in vagal stimulation that terminates in the nucleus tractus solitarius (NTS) and mediates cardiovascular and respiratory responses. There could also be direct humoral signaling within circumventricular organs the subfornical organ (SFO) or Area Postrema (AP). These areas are known to project directly to fear, respiratory and cardiovascular regulatory areas throughout the brain. Alternatively, inflammation could occur directly in the brain in response to stress (interoceptive/homeostatic or exteroceptive), trauma, or panic context re-exposure. Many studies have shown increased inflammation in fear-associated regions prefrontal cortex (PFC), hippocampus (HPC), amygdala (AMY) or the NTS. Inflammation in these areas could affect neuronal activity and drive the emotional, behavioral and physiological responses associated with panic disorder pathology.