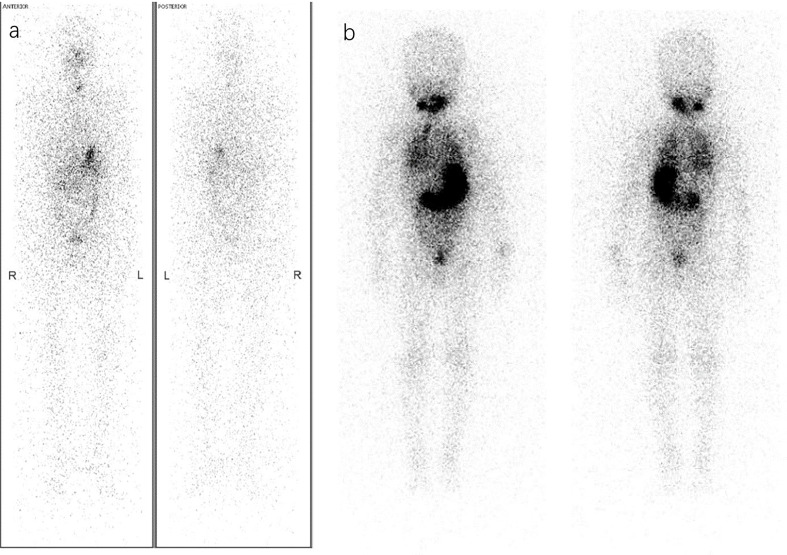
Figure 1.
Different RAT considerations via Dx-WBS. (A) A 36-year-old woman was diagnosed with PTC (pT1bN1bM0, ATA intermediate-risk) by pathology after thyroidectomy and lymph node dissection. Considering both the postoperative disease status of ps-Tg<0.04 ng/ml and A-Tg 111 IU/ml with a decreasing trend and Dx-WBS findings that did not indicate suspicious concealed lesions, she may not benefit from RAT. Therefore, she received TSH suppression therapy instead of RAT. (B) A 4-year-old boy under thyroidectomy was confirmed pathologically to have PTC (pT1aN1aM0, ATA low-risk) in 2008. Surprisingly, Dx-WBS revealed wide uptake of 131I in the lungs, whereas preoperative CT did not. Through 3 times of 60 mCi RAI, he obtained and has maintained an excellent response (ER) in recent years (1st RAT: TSH >150 μIU/mL, Tg 91 ng/ml, A-Tg 13.25 IU/ml; 2nd RAT: TSH >150 μIU/mL, Tg 9.4 ng/ml, A-Tg 10 IU/ml; 3rd RAT: TSH >150 μIU/mL, Tg 3.4 ng/ml, A-Tg 10 IU/ml; the latest follow-up: TSH 0.244 μIU/mL, Tg<0.04 ng/ml, A-Tg 15 IU/ml).