Abstract
This article examines policy innovation, emergence of innovative health technology and its implication for a health system. The complexity of policy innovation implementation resulting from mixing public health resolution and economic interest will trigger the emergence of innovative health technology, which implies a health system improvement. The findings revealed that: First, policy innovation based on a science-mix category created the complexity of policy enforcement, affected the scale and speed of COVID-19 transmissions, and triggered the emergence of health innovative technology. Second, despite policy innovation in early COVID-19, handling was relatively less successful due to restricting factors in policy implementation but provided a new market for the emergence of innovative health technology. Third, the emergence of innovative health technology has strengthened health system preparedness during the pandemic, and provide an opportunity to re-examine the strengths and deficiencies of an entire health system for better health care.
Keywords: Policy innovation, Emergence, Innovative health technology, Health system, System dynamics
1. Introduction
1.1. Background
COVID-19 has attacked almost all countries in the world. For countries affected by this virus there is no choice but to unite against an invisible enemy. Each country has its own experience in conquering COVID-19. In Italy, where the pandemic turned into a disaster, a major contributing factor to COVID-19 disaster was the decision-making process at many levels of government [1]. China revealed that the most critical factors in stopping a pandemic were early recognition of infected individuals, carriers and contacts, and rapid implementation of quarantine measures with an organized, pro-active and unified strategy at a national level. Delays resulted in significantly higher death tolls [2]. Vietnam was characterized by a rapid response, clear leadership, a multi-sectoral approach, and supported by clinical care and a public health response [3]. Thailand managed the COVID-19 pandemic by implementing real-time application technologies by using a bottom-up approach, resulting in people taking greater control of their own health, improving efficiency and reduction of demand on health resources [4]. Rapid response and high reliance on technology have been a common characteristic of countries that have successfully managed COVID-19 such as Israel, Singapore and Korea [5]. While, Indonesia faced governance challenges in dealing with the early COVID-19, which was exacerbated by political nuances in pandemic handling, ignorance of science, limited economic capacity, and an inadequate health service system [6].
Science and knowledge gained from these experiences produced a high level of confidence, and had applicability to specific places, times, society, and events. Those documented experiences in peer reviewed journals became knowledge sources to broaden insights in policy making. Beside documents, the main source of knowledge for policy making is people, including internal colleagues, external contacts, and their contacts. External contact comprises individuals who are scientific professional representatives or membership in professional organizations [7]. In the case of COVID-19 handling, France valued the science-based evidence by appointing group of scientists as an advisory board to help manage the crisis. However, in situations where decision makers face radical uncertainty, sticking to conventional approaches might jeopardize the science-policy interface [8]. In handling COVID-19, Indonesian government did not fully put science first in early COVID-19 handling [9,10]. Indonesia used a “science-mix category” in designing its COVID-19 handling policy.
The definition of a science-mix category in this study is public health resolution mix with economic interests in designing the COVID-19 handling policy. The implementation of health protocols is balanced with the continuity of socio-economic activity, where the application of health protocol for all people (including washing hand, social distancing and wearing mask) is balanced with controlling people mobility and crowding in socio-economic activity. Indonesia government can be categorized as implementing policy innovation in early COVID-19 (see literature review), which was driven by the exponentially rising rates of COVID-19. The mixture of public health resolution mix with economic interests created the complexity of policy implementation without clear priorization, which caused an increasing rate of COVID-19 infection, and a higher level of concern to seek a quick solution. In short, the complexity of policy innovation implementation had an impact on emergence of innovative technology for a quick solution to the COVID-19 pandemic.
The Indonesian policy innovation that put into effect science-mix policy instruments distinct from the general policy measure (lockdown), was a Large Scale Social Restriction (LSSR). The LSSR is stricter than social distancing (SD) guidelines, but not lockdown, because it gave opportunity for people to move outside their home for fulfilling essential needs. The LSSR belongs to the authority of central government, which receives and approves regional administration (city, district and province) proposals for the LSSR. A LSSR proposal must be based on epidemiology, threat magnitude, effectiveness, supporting resources and operational, technical, political, economic, socio-cultural, defense and security considerations [11]. Indonesia applied SD from March, 15 to April 10, 2020, followed by LSSR from April 10 to May 31, 2020. We define this period as early COVID-19, since then Indonesia has entered a new normal phase from June 1, 2020 up to present.
Policy innovation based on science mix category was designed and enforced by policy makers to conquer COVID-19. As a matter of fact COVID-19 case numbers were around twenty eight thousand in the period early COVID-19, then rose to around 1.5 million by the end of March 31, 2021, ten months later. To sum up the complexity of the pandemic, we cite the famous Steve Jobs’ quote:“You can not understand what happening today without understanding what came before”. In the context of acquiring a deep understanding of past events, we conducted the system dynamics modelling of early COVID-19 handling in Indonesia. The model explained the patterns of problematic behaviors caused primarily by the design of feedback structure inside the system, thus we understand how and why the system of early COVID-19 handling really worked. This is the first model of system dynamics on early COVID-19 handling, while the most recent scientific work on COVID-19 modelling by Ref. [12] focused on a future scenario of COVID-19.
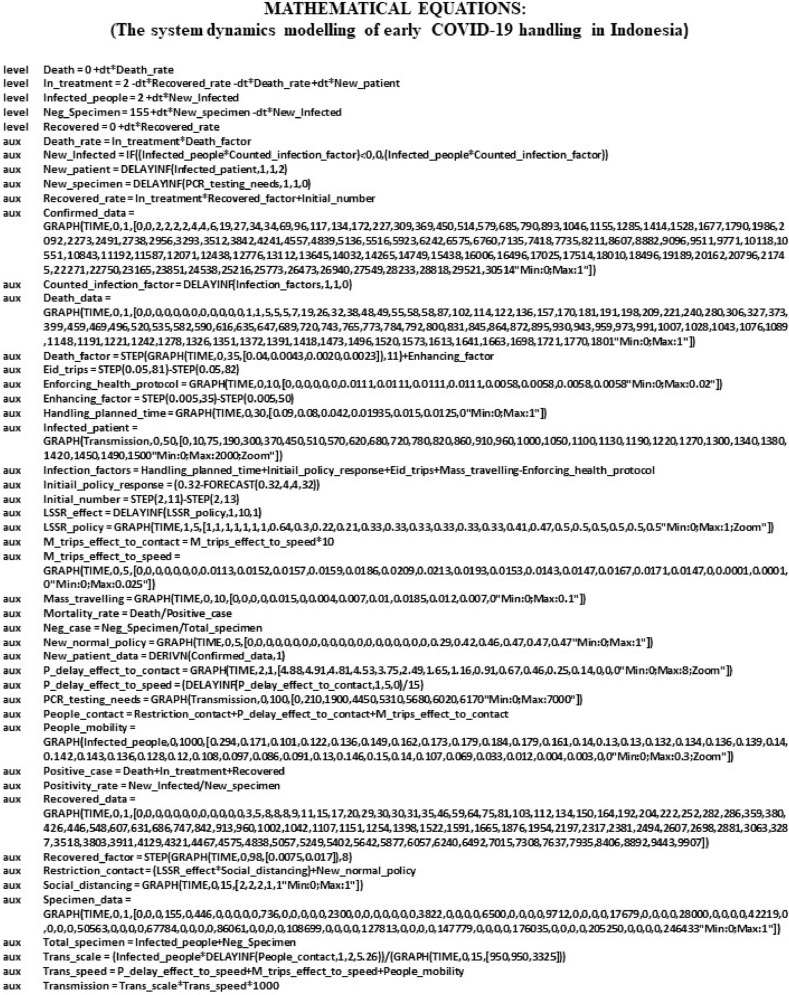
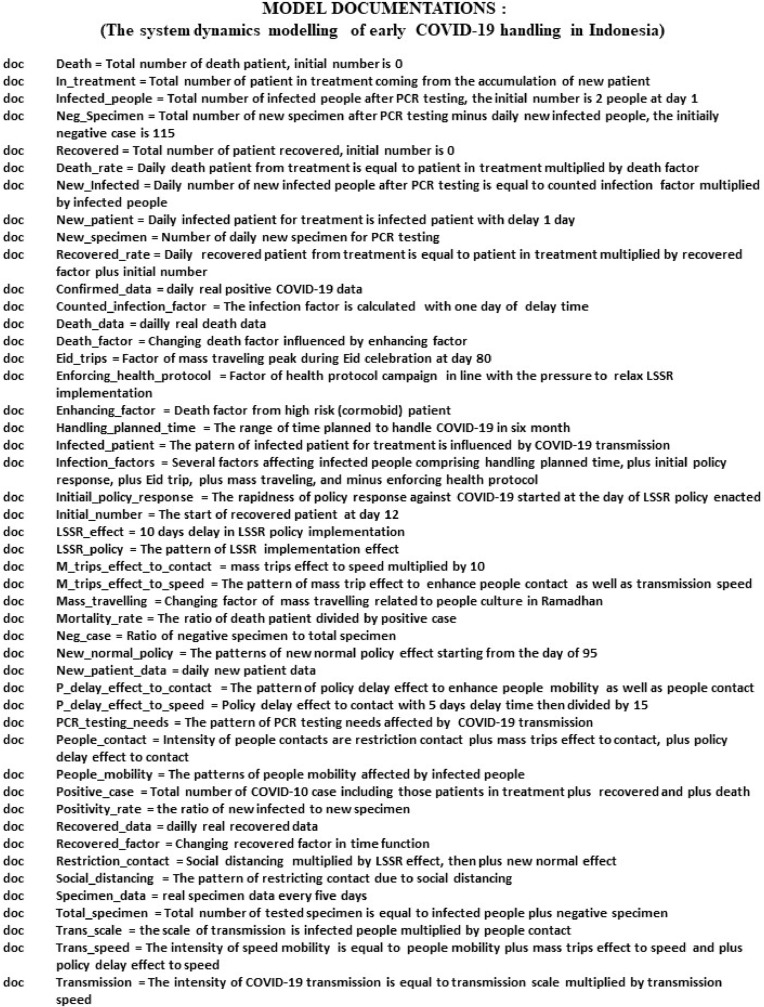
Theoretically, this study had three contributory values: First, the original framework for seeing the whole picture of early COVID-19 handling (Fig. 1 ), which was formulated into an original model of system dynamics (Fig. 2 ). Second, revealing the emergence of innovative health technology driven by complexity of crisis that needs quick solutions, will enrich the concept of [13] that technological emergence is a cyclic process in highly creative scientific networks. Third, understanding the reality of a policy innovation dynamic in the past contributed to enrich historically sensitive policy making model in policy science [14].
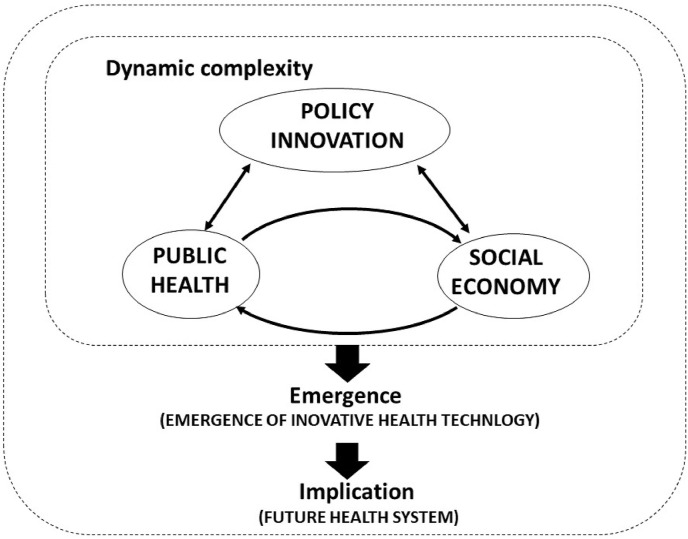
Fig. 1.
Dynamic complexity and emergence of innovative health technology.
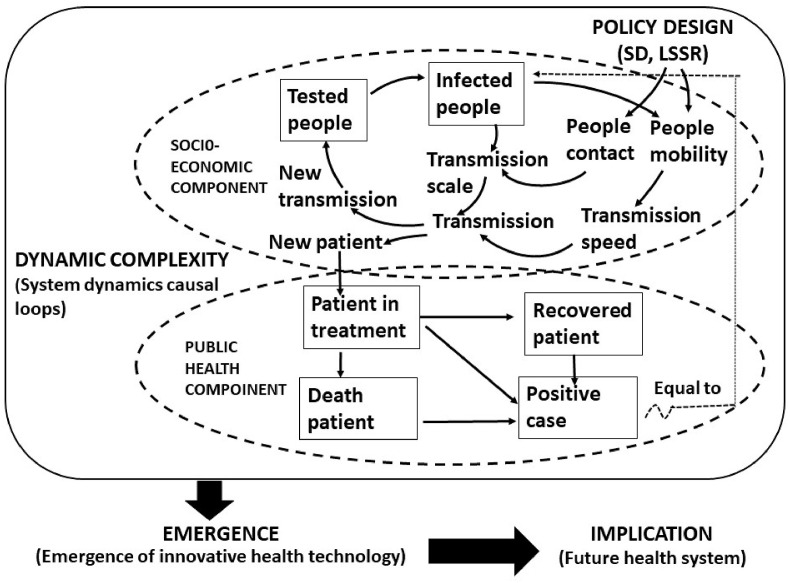
Fig. 2.
System dynamics model of policy design, socio-economic and public health.
1.2. Objective of study
The objectives of study are: i) to understand the events behind the dynamic curves in early COVID-19 handling, where the curves was drawn with computer simulation by using system dynamics modelling, and; ii) to carry out policy analysis with computer simulation to explain the policy innovation effectiveness during early COVID-19 handling. The key questions are: i) How effective were the early COVID-19 handling policy instruments by social distancing (SD) and largescale social restriction (LSSR)?; ii). How science-mix category affected policy related events behind dynamic curves of early transmission of COVID-19?; iii) What were the impacts of policy innovation implementation on the emergence of innovative health technology?; and iv) What important lessons were learnt from model intervention by computer simulation for future epidemic/pandemic handling and health system improvement?
1.3. Methodology
1.3.1. System dynamics modelling
Methodology of study was the application of system dynamics modelling for understanding past policy implementation and learning for future policy improvement [15]. The modelling in system dynamics are as follows: First, model building was enriched from the method of “from story to structure” [16]. The model was constructed from data/evidence behaviour to be a original model or “from real data to model”. The evidence was documented [17]. Systematization of evidence was formulated into five dynamic patterns of events: i. the exponentially rapid increase of COVID-19's cases; ii. gradual increase in government policy responses; iii. gradual expansion in the scope of LSSR enforcement; iv.gradual extension in the control of people mobility; and v. the gradual relaxation of prolonged LSSR enforcement. The structure of the model behind these dynamic patterns was constructed (section 3) based on conceptual framework (section 2).
Second, computer simulation used Powersim software. The simulation results as graphical events behind the dynamics patterns are described in section 4. Policy analysis was conducted by computer simulation to find policy leverage and policy correction for solving the sources of policy failures, then discussion on simulation results were condensed into the lessons learnt from the success and failure of informing policy with science-mix category as revealed in section 5.
1.3.2. Data types and sources
Two types of data were used: first, quantitative data included number of positive cases, number of patients in treatment, number of patient deaths, number of recovered patients, and number of people tested by PCR. For documentation of data types (Appendix 3). Second, qualitative information related to: the story of early spatial distribution of COVID-19, changing patterns of government policy response to COVID-19, leadership attitude on early COVID-19, policy resistance to early COVID-19; and the difficulty of reaching consensus in early COVID-19.
Data source of study were the daily statistics published by Infeksi EmerGing department, Official update information media on emerging infectious disease, Ministry of Health, Indonesia [18]. For qualitative data sources, the study used media mainstream news on early COVID-19, namely, the Jakarta Post, CNN Indonesia, Kompas, Media Indonesia and Antaranews. Data period for analysis was limited in the three months of early COVID-19 between day 1 (first case detected) to day 94 (closing of LSSR and entering the new normal phase).
1.3.3. Validated model
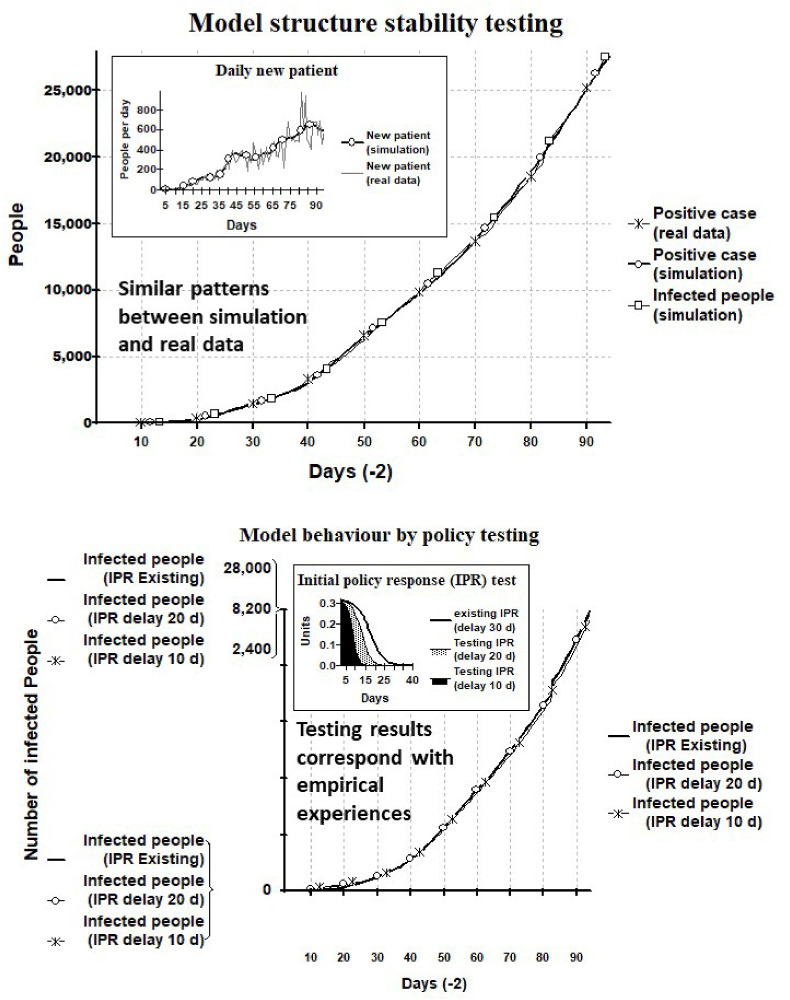
Validated model passed four orderly stages. The order of testing from one to four is decisive, if test fails at one stage then model construction must start from the beginning [19].
First, empirical structure test by comparing model equations against knowledge from the real system being modelled. The model was constructed from real data/evidence through understanding the dynamics patterns of evidence, where the model structure (section 3) and equations (appendix 2) was formulated from the dynamic patterns of evidence.
Second, theoretical structure test by comparing model equations against generalized knowledge on the system, that exist in the literature. Theoretical structure of first loop is the interplay between infected people and people contact [20], and the second loop is interplay between infected people and people mobility [21], (section 2.2.2).
Third, stability of structure test by modifying model parameter, which generated similar patterns of model simulation behaviors against the patterns of real data behaviors. The stability of structure test was confirmed by similar patterns among the confirmed case (real data), positive case (simulation) and infected people (simulation) (Appendix 1).
Fourth, patterns of prediction behaviors test by policy testing, which produced a logical results or corresponded with the behaviors of the real system. Prediction behaviors was tested by Initial Policy Response (IPR) parameter (section 5.2). The simulation results were in correspondence with the empirical experience on the success of very rapid response in COVID-19's handling, as proven by Vietnam and Taiwan (section 5.4 and Appendix 1).
1.3.4. How the model worked
The model worked through computer simulation that mimics real systems. The model can explain how and why the patterns of non-linearity on system behaviors occur, caused primarily by the design of feedback structure inside the system [22]. In this study, the feedback structure was based on the policy innovation perspective, where different perspectives result in different designs of the feedback structure and produce different patterns of system behaviors as well.
2. Literature review and conceptual framework
2.1. Literature review
2.1.1. Policy innovation and dynamic complexity
Policy innovation is policy change from status quo to innovation, where change can be on the aims of policy, the means of policy and both aims and means of policies [23]. Innovation in the goals of management not only inspire but also serve as the magnetic stone in managing the innovation program [24]. The extension of health policy goals from a public health aspect by the inclusion of socio-economic and political aspects, is a policy innovation. Implementing policy innovation by mixed policy instruments in early COVID-19 as a new experiment maybe less successful, because innovation failure increases when we seek to do something we have not been done before [25]. Factors that impact on the success of policy innovation and its development are: approach, method and tools of policy design [26].
Policy innovation for health is driven by the exponentially rising rates of chronic disease (and infectious disease such as COVID-19, added by authors), obesity, and mental health problems indicate that we need to shift course and apply a radically new mind-set to health and health policy [27]. Informing policy with science-mix category combining public health with socio-economic and political interests in policy making is collaborative policy making. The weakness of collaborative policy making is the failure to establish a common ground for public problem-solving [28]. Collaborative policy making by informing policy with science is related to science-policy interface, dealing with the relationship between scientists and other actors in the policy process, which allows for exchanges, co-evolution, and joint construction of knowledge with the aim of enriching decision-making [29]. On communicating science advice [30], stated that improving the science-policy interface through dialog by having conversations rather than talking at one-another; a two-way approach for better information sharing. In investigating the use of research results in policy making, it is important to understand the context and consider the political and economic drivers of decisions making [31]. Political and cultural forces are usually far more important for decision-making [32]. In short, we comprehend that policy innovation implies dynamic complexity in policy implementation.
The dynamic complexity in policy implementation caused worsening COVID-19 transmission and triggered the emergence of innovative health technology. The theoretical relationship between complexity and creative emergence refer to the concepts of [33]. The dynamic complexity in policy implementation can be understood by using system thinking. In the context of pandemic crisis, as non-linear interactions between healthy and infected people, which is invisible and silent due to asymptomatic carriers of the virus, the unfolding crisis needs using complexity thinking or application of system thinking to complex systems [34]. The systemically scientific methods of dealing with complexity of quantification and modeling at both a basic and more advanced level, and considering both theory and application, was explained by Ref. [35]. Quantitative modelling for understanding dynamic complexity by using system dynamics method was used by the founder of system dynamics [15,36,37].
2.1.2. Emergence of innovative health technology and implication for health system
Seven clusters of rapid-response COVID-19 innovations were categorized [38]. The clusters of innovative technology are medical equipment and protectives innovations. Medical equipment describes innovations for equipment used in hospitals, mainly centering around the production of ventilators for intensive care units. Protectives describes the production of protective gear such as face masks, hand sanitizers, and visors. For research on technological innovation in fighting COVID-19 [39], and health care innovation [40]. Health innovation through scientific research on COVID-19 was to create vaccines, health devices and innovative products, which are crucial for vaccination, disease prevention, early detection, as well as the patient-centered treatment [41]. Developing countries' vaccine manufacturers’ network members (including Indonesia) were in progressing in the R&D of COVID-19 vaccines and their capacities in the manufacturing, fill-finish and distribution of vaccines. Currently, 19 network members engaged in the R&D of COVID-19 vaccines, using six principal technology platforms [42].
The success of policy implementation in detection, prevention and response of COVID-19 outbreaks are determined by the health system preparedness for emerging infectious diseases (EID) [43]. Ministry of Health provided technical guidance on health system preparedness for COVID-handling [44]. For the acceleration of COVID-19 handling, the health system preparedness in Indonesia was coordinated by task force for the acceleration of COVID-19 handling to prepare and strengthen health resource capacity in hospitals, laboratories, and other health facilities. The task force coordinated and provided guidelines on the basic flow and mechanism of risk mitigation in the community and COVID-19 handling in health facilities [45]. The health system preparedness depends on the availability and capacity of: i) material resources and structures elements including works force, infrastructure and medical supply, surveillance and communication mechanism, and ii) human and institutional elements including governance, and trust [42]. The health system preparedness is the key to execute a rapid response and successful managing COVID-19 [5].
COVID-19 caused massive changes to people's lives but offered an opportunity to re-examine the strengths and deficiencies of our health care system. The emergence of innovative health technology relates to various contexts. In the context of COVID-19, the emergence of virtual innovations during the covid-19 pandemic is for a better tomorrow in health care [46], telemedicine set to transform healthcare in a post-COVID-19 world [47]. In the context of health management, transforming the health care prioritizing cost reduction and improved patient outcomes have altered medical device innovation and market regulations [48]. In the context of health governance, implementing evidence-based health innovations will inform health system planners and evaluators, especially on effective and sustainable implementing evidence-based health innovations for health reforms [49,50]. In the context of health administration, the dynamic processes of responding to the needs of health society will be critical [51]. In short, the emergence of innovative health technology has implications for health system management and governance.
The summary of reviewed literature were the basis for the theoretical foundations for the construction of our framework and model structure (Section 3, 2.2), which consists of: i) policy innovation in policy objectives including for health and economic goals is essentially collaborative policies by converging health resolution and economic interests, while the implementation of collaborative policies based on public health, economic and political considerations lead to dynamic complexity in realizing policy objective; and ii) the dynamic complexity in COVID-19 handling system under the less preparedness of health system drive the emergence of innovative health technology for quick solutions of urgent problems related to rapid rising COVID-19 infections.
2.2. Conceptual framework
On the basis of the literature review we: i. formulated the core ideas or whole picture that the dynamic complexity of policy innovation lead to the emergence of innovative technology during early COVID-19 handling, which implied the improvement of the health system, and; ii. constructed the framework of policy innovation effectiveness resulting from the interaction between public health resolution and economic interest during early COVID-19 handling (Fig. 1).
The interaction among four key concepts are as follows: i. Policy innovation role. The policy innovation should function as determinant factors to drive both in balancing between public health resolution and economic interest, the balance between easing economic suppression at the cost of worsening COVID-19 and tightening public health resolution at the cost of more economic suppression; ii. Interplay between public health resolution and economic interest. The public health resolution is the prerequisite for economic activity, an increase in people infected by COVID-19 suppresses economic activity and social contact, the lower the economic activity suppressed by COVID-19, the more intense the search for public health resolution by invented innovative health technology; iii. Emergent innovative health technology from dynamic complexity. The emergence of innovative health technology is unplanned creativity in form of emergent technology innovation as a quick response to the serious public health problem triggered by COVID-19; and iv. Implication for health system. the emergence of innovative health technology implies not only to a strengthened health system preparedness during the covid-19, but also offers an important opportunity to re-examine the strengths and deficiencies of entire health system for a better health care.
3. Model structure
3.1. Model components
The model structure has three components: policy design, socio-economy, and public health.
3.1.1. Policy design
Policy design and implementation were the use of policy instruments including social distancing and physical distancing (SD), and large scale social restriction (LSSR). Policy design implementation was mixing the interests from various policy stakeholders in health and social-economic sectors. The mixture of interests in governing public health problem led to policy action without clear priorization [52]. The government priority is a balance between COVID-19 handling and economy recovery. Indonesia has been applying both brake and gas pedal for the balancing between manageable health risk and continuous economic activities [53]. The policy action based on science-mix category created the complexity of early COVID-19 handling in Indonesia.
3.1.2. Socio-economic components
i. People contact was the intensity of close contact coming from people interaction which was controlled by SD and LSSR to stop the spread of infectious diseases; ii. People mobility was the intensity of people movement, which was controlled to stop the spread of infectious diseases and influenced by people's social and economic condition; iii. Transmission scale was the magnitude of spreading infectious diseases depended on close contacts between people; iv. Transmission speed was the rate of spreading infectious diseases depended on people mobility; v. Transmission was the multiplication of transmission scale and speed as the potency of people infected by COVID-19 transmission; vi. New patient was the rate of newly positive COVID-19 cases; vii. New transmission was the rate of new people needed to be tested as COVID-19 suspects; viii. Tested people was the number of testing people (with polymerace chain reaction - PCR) whether infected or negative with COVID-19; and ix. Infected people was the number of people with positive COVID-19 or positivity rate.
3.1.3. Public health components
i. Patient in treatment was the number of positive COVID-19 under medical treatment; ii. Patient death was the number of patient deaths caused by positive COVID19; iii. was the number of patient recovered from positive COVID-19; and iv. Positive case was the sum of patient in treatment plus death patient and plus recovered patient, which was equal to infected people in the element of socio-economic component.
3.2. Model structure
Model structure is the interaction three components: policy, socio-economy, and public health. Dealing with the complexity of socio-economic components determined the success of an operating public health component. First, the social economic component consists of two main elements, namely the number of tested people and the number of infected people. These two elements were determined by policy implementation on SD and LSSR, which were influenced by people's socio-economic condition. Second, the public health component consisted of three patient elements, namely patient in treatment, recovered patient and dead patient. The sum of these three elements was called total number of positive cases. Third, the linkage between socio-economic and public health components is bridged by the number of new patients in treatment, where new patient was determined by COVID-19 transmission, which was defined as the multiplication between the transmission scale and the transmission speed (Fig. 2).
The first loop is the interplay between infected people and people contact [20]. An increase in the number of infected people provided information on the increase of transmission scale. The increase of transmission scale contributed to the increase of COVID-19 transmission. It leads to increase the new transmission and it will again increase the number of tested people as COVID-19 suspects. Such a positive feedback loop process results in the exponential increase in the number of infected people. The second loop is the interplay between infected people and people mobility [21]. An increase in the number of infected people provided information on the increase of people mobility. The increase of people mobility leads to increased transmission speed. The increase of transmission speed contributed to the increase of COVID-19 transmission, which lead to increase the new transmission and again increase the number of tested people as COVID-19 suspects. Such a positive feedback loop process will force the first loop toward exponentially increase in the number of infected people.
The two positive feedback loops can be changed into negative feedback loop by using control measures through policy implementation. Consequently, the exponential increase in the number of infected people will shift into a parabolic curve. First, the control of transmission scale was done by minimizing people contact by applying SD and LSSR. The delay in the application of SD and LSSR will contribute to the increase of COVID-19 transmission. Second, the control of transmission speed is determined by managing people mobility, which is influenced by the socio-economic condition of the people. The difficulties of economic condition in urban areas due to the implementation of LSSR pushed people mobility back to their hometown in rural areas. Then, the social needs for family gathering in Ramadhan and Eid celebration also pulled the increase of people mobility back to their hometown in rural areas.
4. Simulation results
4.1. The effectiveness of policy instrument to control COVID-19
The main policy instrument to control COVID-19 is LSSR. The effectiveness of LSSR policy to handle COVID-19 is explained by the way LSSR policy works. The LSSR policy was enforced on day 31 or one month after COVID-19's outbreak. There were four events related to LSSR policy enforcement: prior to, during, prolong, and before closing LSSR implementation.
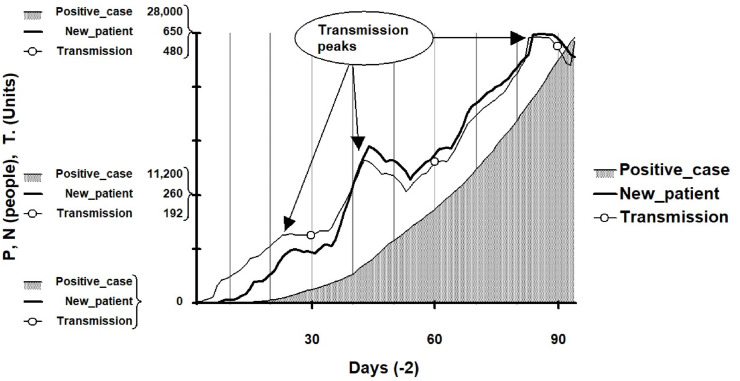
The increase of positive COVID-19 or raising the number of new patient per day was caused by the following transmission events. First, prior to LSSR, the number of positive COVID-19 increased exponentially from day 2 to day 28. Such a rapid increase of new patient, which was caused by the increasing trend of transmission that reached the first peak at day 25. It reflected the restriction guidelines on social distancing and physical distancing were less effective. Second, during the preparation of LSSR implementation, the number of positive cases continued to increase from day 28 to day 38. Third, during the period of LSSR implementation, the rapid increase of transmission occurred by fluctuating between day 38 and day 94. There were two peaks during this period, the first peak was at day 40 and the second peak at day 80. The 1st LSSR succeeded to suppress transmission between day 40 to day 52. The transmission continued increase during the prolonged enforcement of the 2nd and 3rd LSSR. The second peak at around one thousand new patients occurred at day 80. Fourth, before closing the 3rd LSSR, the transmission was slightly suppressed from day 80 to day 94. From day 95, Indonesia had entered the phase of new normal or enforcing LSSR in transition (Fig. 3 ).
Fig. 3.
Patterns of transmission and positive case in early COVID-19.
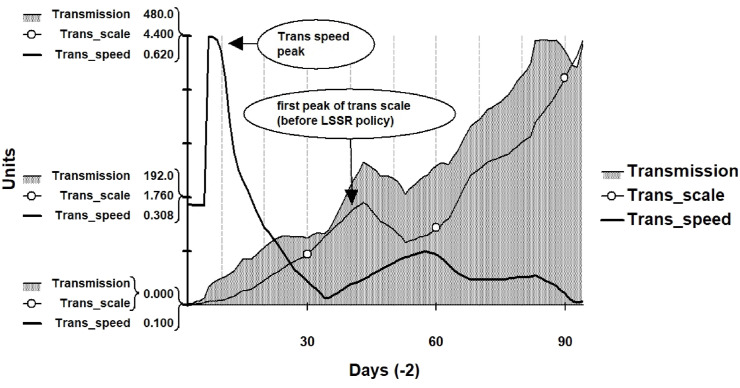
The patterns of dynamic transmission were formed by two elements: transmission speed and transmission scale as shown by two interesting sets of evidence.
Firstly, prior to LSSR enforcement there were two peaks. The first peak of rapid increase in transmission around day 10 was caused more by transmission speed rather than transmission scale. The very rapid increase of transmission speed occurred from day 2 to day 15. It was the golden time of Indonesian government of lost opportunity to stop the transmission speed. The second peak of rapid increase in transmission around day 40 was caused more by transmission scale rather than transmission speed. The very rapid increase of transmission scale occurred between days 35–40. It was the initial time of great efforts in fund and resources for LSSR preparation that must be spent to suppress the transmission scale.
Secondly, during LSSR enforcement, the rapid increase of COVID-19 transmission was caused by both rapid increase of transmission scale and transmission speed as well, where the fluctuating increase of transmission was caused more by transmission speed rather than transmission scale. It infers that Covid-19 transmission was caused by mutual enforcing between transmission speed and transmission scale, failure to stop the transmission speed at initial time of COVID-19 outbreak led to transmission scale expansion to anywhere inside Indonesian territory (Fig. 4 ).
Fig. 4.
The transmission scale and speed in early COVID-19.
Based on evidence of dynamic curves (Fig. 3, Fig. 4), our findings revealed that the effectiveness of LSSR policy intervention to handle COVID-19 depends on three factors: the rapidness of LSSR intervention time, strictly controlled transmission speed, and consistent control of transmission scale. The delay in LSSR intervention time, less control of transmission speed, and less consistent control of transmission scale had constrained the achievement of effective LSSR policy intervention to handle COVID-19. The discussion of why these happened is found in Section 6.1.
4.2. Policy related events behind dynamic curve of COVID-19 transmission
The science-mix category converges interests from various policy stakeholders (in health and social-economic sector). Such processes influence the ways of setting policy responses and affect the instruments for implementing policy decision. The science-mix category created policy dynamic at implementation stage that finally affects the COVID-19 transmission speed and the transmission scale as well.
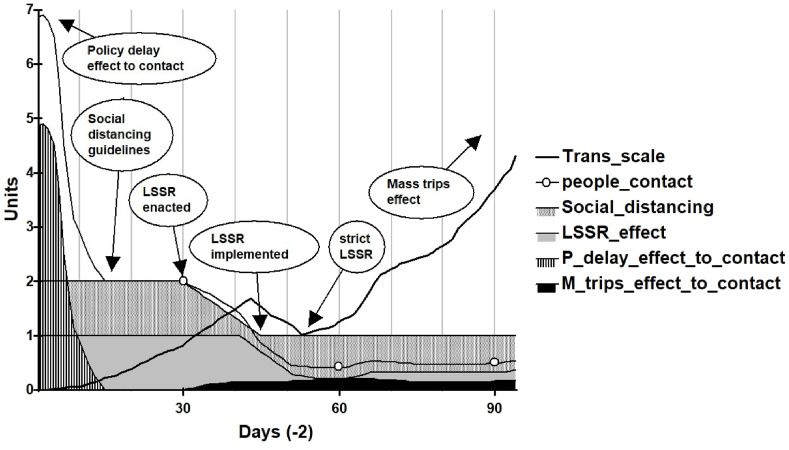
4.2.1. Transmission scale curve
This study revealed that the adoption of science-mix category during pandemic outbreak delayed policy enforcement and affected the consistent control of transmission scale. The dynamic patterns are as follows:
First, the transmission scale had increased exponentially from the day 1 to day 28. The exponential increase of transmission scale was caused by: i) public campaign on social restriction including social and physical restrictions was less effective between day 15 to day 28; and ii) LSSR enacted at day 28 meant that policy delay for one month after day 1 since COVID-19 was detected. Why this happened is elaborated in Section 5. The consequence of LSSR policy delay was greater effort to fund and resources to meet policy targets with the delayed response.
Second, the transmission scale continued to increase rapidly during the period of LSSR preparedness between day 28 and day 38. The rapid increase was the co-incidence with mass traveling going back early to hometown prior to Ramadhan. Strict LSSR policy implementation succeeded to initially suppress the transmission scale from day 40 to day 52, but it continued to increase afterwards. The re-increase of the transmission scale was caused by the mass traveling effect, which was related to three mobility factors: i) going out of economic pressure in urban areas for low income of daily workers; ii) social needs for family gathering in Ramadhan; and iii) local traveling and seasonal crowding before Eid celebration that caused citizens to disobey LSSR rules (Fig. 5 ).
Fig. 5.
Policy related events behind transmission scale in early COVID-19.
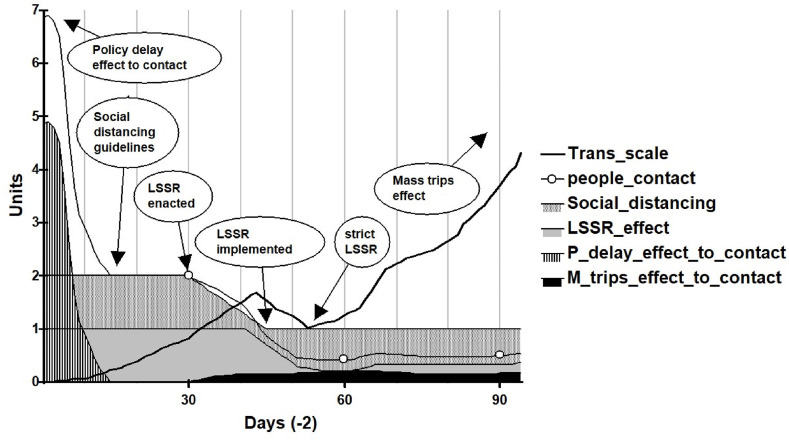
4.2.2. Transmission speed curve
The application of science-mix category during pandemic outbreak caused a delay in policy enforcement and finally affecting COVID-19 transmission speed. Between the first case identified, there was five days of delay time for transmission speed to spread. The transmission speed increased abruptly between day 7 to day 15 and determined that COVID-19 was allowed spreading extensively without significant government intervention. In the next two weeks (days 15–30), the government took steps to campaign for social distancing and physical distancing. Even though the campaigns of work from home (WFH) had reduced people mobility and transmission speed as well, the initial transmission speed of COVID-19 between day 7 to day15 had spread to several other areas, and the COVID-19 epicenter shifted to the dense population region of Jakarta Province.
The transmission speed had been successfully reduced by LSSR policy preparedness between day 28 and day 38. The LSSR policy preparedness caused economic difficulties for daily low-income people, which caused the wave of mass traveling out of Jakarta. The LSSR implementation between the day 38 and day 94 was co-incidental with returning to hometown earlier before Eid and doing Ramadhan's fasting at hometown. Initially, the LSSR policy was successful, but later it became less successful because of increasing people mobility in several cities and districts of hometown destinations, mainly on Java Island. After Eid celebration, the transmission speed was suppressed by the strict control of people mobility and new normal preparation as well. In short, transmission speed followed people mobility (Fig. 6 ).
Fig. 6.
Policy related events behind transmission speed in early COVID-19.
5. Discussion
5.1. Restricting factors
The computer simulation results revealed the policy dynamic behind the dynamic curves. The Indonesian policy on COVID-19 handling, which was driven by a policy mix perspective, must be agreed by health, social economic and political stake holders. Moreover, policy on COVID-19 handling operates in complex environments, it was an abnormal situation in which many factors were also operating and tightly specified causal analysis of policy effects should be tested before implementing, was simply not possible to undertake [54]. The following explanation discusses the three restricting factors coming from that complex environment, namely: i) the perception of COVID-19 as an insignificant problem; ii) policy resistance; and iii) the difficulty of reaching consensus.
First, dealing with COVID-19 was an attitude problem, the COVID-19 was perceived as an insignificant problem and consequently that led to symptomatic solutions and caused fundamental problems. This attitude caused the lack of anticipation that resulted in less preparedness when COVID-19 was identified as having entered Indonesian territory. The overconfident attitude of the government was found in various statements of the government elite or state actors. Initially by discrediting the study results of a scientist from the Harvard T. H. Chan School of Public Health who said the presence of the corona virus in Indonesia was detected [55]. Furthermore, it became a high-level joke by a top Minister who said that Indonesia is the only major country in Asia that has not been touched by the corona case [56]. A government Minister expressed ‘jokingly’ by saying COVID-19 virus does not enter Indonesia because of ‘cats rice’ [57]. Meanwhile, the top decision maker said that wild horse milk can counter corona virus [58]. These denials of severe problems contribute to the failure of government policy innovation [59]. Moreover, the traditional knowledge cannot stand up against the scientific knowledge which is often ignored [32].
These government official's statements of underestimating the presence of COVID-19, resulted in some delays in decision making. The delay of decision making to respond to COVID-19 was shown by the government's first decision on the guidelines of Social Distancing two weeks after the first case identified on March 2, 2020. Furthermore, later on March 31, 2020, the government enacted the LSSR. For the regions, which implemented LSSR, they closed public facilities, transportation, markets, restaurants and access from both air and land, except for food supply and medicines. The delays of decision making resulted in the government's less preparedness to face the spread of the virus raising exponentially with an unexpected speed and scale. The less preparedness of government had an impact on the limited supply of medical equipment at all levels, especially at the provincial and district levels. This condition made it difficult for medical workers to provide medical services when COVID-19 came to their regions. The medical workers' difficulties emerged in many provinces as medical supplies become depleted [60].
Second, policy resistance arising from complex environmental responses make matters worse [61]. Policy resistance can be seen from the community's response to government guidelines for social restrictions. Government guidelines for applying social distance and physical distance were ignored by most people. The ignorance of people made the situation worse, which was shown by the exponential increase in COVID-19 cases. The ignorance response by some public elements to government guidance happened in various socio-cultural activities such as mass preaching, mass prayer, weddings, which can increase the risk of COVID-19 transmission through social and physical relations among people who were gathered. The crowd appeared at various public facilities, such as restaurants, markets, supermarkets, houses of worship, and wedding venues. The resistance was also inherent to: i) the social living consideration that requires the culture of high discipline for LSSR implementation, where such culture has not fully established in Indonesian society; and ii) people's economic activities consideration, especially small to medium enterprises (SMEs), was greatly affected by the implementation of LSSR. Such socio-economic and cultural forces are more influential than health consideration and usually far more important for decision-making [32].
The first region implementing the LSSR was the Jakarta province on April 10, 2020. The Jakarta provincial government distributed social assistance to low-income people expecting them to stay at home during the LSSR period. However, the response of low-income people and street vendor in the informal sector preferred returning to the village rather than survive without income in the city. The exodus of going back to hometown coincided with the approaching of fasting and Eid moments, where family gatherings during Ramadhan fasting and Eid celebration are cultural traditions long rooted in society. Government efforts to control mass trips to hometown ranging from appealing to banning were less successful. It was estimated that around 500 thousand passenger cars left Jakarta in the context of Ramadhan and Eid [62]. As a result of mass trips to hometown, the spread of COVID-19 increased in various regions outside Jakarta province. The worsening problems due to unexpected social responses were difficult to be controlled by the government. Increasing number of cases in the regions, due to the presence of back to hometown travelers, was expected to provide lessons for the public to comply with government regulations, but it was less successful.
Third, the difficulty of reaching consensus in policy implementation. In the perspective of policy mix in health science plus social and economic aspects, the characteristics of policy needs to accommodate stakeholder interest, which were coming from health care, economic activities, social life of the community, pressure groups and others in and outside of government. Forrester [37] argued that “there are no decision makers with the power and courage to reverse ingrained policies that would be directly contradicted to public expectations”. For example, in line with the LSSR implementation, the decision of the Jakarta administration closed the inter-city bus terminal, but it was then canceled by the transportation ministry. Finally, the closure was done again after the COVID-19 transmission increased rapidly. Furthermore, the decision to ban people returning to hometown was finally allowed by the reasons of easing transportation for emergency purposes and limited traveling for special sectors under LSSR regulation as well. The difficulty of reaching consensus also occurred in the implementation of economic policies that did not synergize with health policies to stop the spread of COVID-19 entering the Indonesian territory. For example, it was a wicked problem where the government was still opening international flight routes from China, encouraging foreign tourist visits, and even promoting ticket cutting to increase the attractiveness of the tourist industry; economic solution caused the health problem.
Hudson, Hunter & Peckham [28] stated that the weakness of collaborative policy-making is the failure to establish a common ground for public problem-solving. The more consensual the design process the less the likelihood of disagreements at the implementation stages. Difficulties in reaching consensus also occurred in the preparation of a new normal. Controversy arose over the timing of the new normal implementation. The government's desire to implement new normal at the beginning of June together when the curve of COVID-19 infections was not trending down. The government was faced with a policy priority between the interests of health, economics, and both. To combine these two options, the health protocol must be followed with discipline and the reopening of economic activity gradually launched depending on the success of the health protocols. The government's suggestion to live “peaceful with the corona” was responded by a respectful community member who said “that the coronas do not want to make peace”. In order to start opening economic activities, the government simulated the easing of LSSR by reopening access to transportation, malls and markets under disciplined health protocol. The enforcement of discipline supported by security measures to occur with full obedience to health protocols. The simulation of LSSR easing in the context new normal preparation was done before new normal implementation on June 5, 2020.
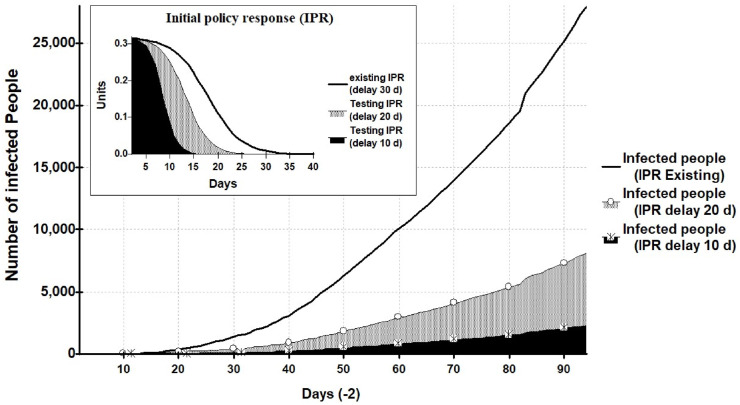
5.2. Counter intuitive policy response
The first restricting factor was the attitude of overconfidence by thinking there was no virus, when the virus was out there. The attitude is basically under government control, but the debate between health science and economic interests delayed a fundamental solution, which finally came with a moderate solution (policy-mix with delay time). For our analysis, we called it a “compromised policy-mix”, intuitively agreed by policy makers but one year later this policy was recognized by a high government official as a careless step [63]. For the future of infectious disease handling policy, government needs to avoid overconfidence and making preparation to combat the coming wicked problem. A rapid initial response without delay on emerging diseases is just as vital as early detection to avoid a largescale pandemic [43]. Rapid initial response without delay will curtail the time of controlling a pandemic, and effective control will stop local transmission amplification.
A computer simulation of “counter intuitive policy response” was based on the logic of system principles [15,36]. We found that effective and rapid policy response in controlling of emerging diseases were represented by initial value and initial time. The rapidly initial response without delay in our model was initial policy response (IPR). The simulation results (between day 1–94) showed that: i) the LSSR policy was enforced with one month IPR delay after COVID-19's outbreak, the existing positive case was 28,000 infected people; ii) if the IPR delay is reduced by ten days or LSSR policy is implemented within 20 days of first case identified, the possibly positive case would be less than 10,000 infected people; and iii) if the IPR delay is reduced by twenty days or LSSR policy is implemented within 10 days of first case identified, the possibly positive case would be less than 3000 infected people (Fig. 7 ).
Fig. 7.
Counter intuitive policy effect to possible reduction of infected people.
5.3. Residual policy instrument
Two restricting factors, namely policy resistance and the difficulty of reaching consensus, both proven to be not easily controlled by government. The adoption of new normal life has been taking place when the curve on the addition of new cases of COVID-19 had not steadily decreased. The new normal life has been carrying out simultaneously for the benefit of health and economy, by enforcing highly disciplined health protocols, along with the gradual reopening of economic activities. The policy analysis, through computer simulation, revealed that the effective enforcement of highly disciplined health protocols must be directed to lowering two restricting factors: policy resistance and difficulty of reaching consensus. If government succeed to enforce highly disciplined health protocols, there is an expectation to see a gradually drop in new cases of COVID-19 in the new normal period [64].
The success of enforcing a highly disciplined health protocol will be determined by the successful executing systemic control of policy implementation in all socio-economic activities. The comprehensive monitoring tool needs to be applied sustainably at all levels. The application of monitoring tools must be capable of correcting irregularities in enforcing highly disciplined health protocols. The participation of all parties collectively was crucial, including public health, economic activities, social life, pressure groups and stakeholders inside and outside the government bureaucracy, religious leaders, and various levels of community leaders down to the grass roots level of society [64]. There will be uncertainty until the vaccination for all people has occurred, and difficult to maintain the same policy instrument (strict LSSR) causing a serious impact on social economic condition, except under the COVID-19 emergency risk. The remaining policy instrument, as a preventive measure by enforcing highly disciplined health protocols with sustainably comprehensive monitoring, is called a residual policy instrument for COVID-19 handling.
5.4. Lessons learnt
The important lessons learned from model intervention using computer simulation is a counter intuitive policy response, where rapid initial policy response is the point of leverage for the success of infectious disease handling policy. The shorter the delay, the greater the chance of success to reduce the number of infected people and the shorter the time of infectious disease handling. The empirical experience on the success of very rapid response in COVID-19's handling was proven by Vietnam [3,65] and Taiwan [5]. By the end of March 2021, total cases in Vietnam were only 2591, and Taiwan only had 1022 cases of COVID-19, while Indonesia has reached 1.5 million cases (Source: [66].
Other important lessons learned from the findings are: i) raising the effectiveness of LSSR policy intervention to handle future epidemic or pandemic depends on strict control of both transmission speed and transmission scale; ii) designing and informing policy with a science-mix category should be formulated by consensus in advance and guarantee its consistent implementation for effectiveness of future LSSR policy intervention [67]. The strategy of policy formulation by consensus should be taken through dialog by having conversation rather than talking at one-another [30]; and. iii) The participation of all parties collectively were crucial until vaccination for all people completed because it will be difficult to maintain the main policy instrument (LSSR). The remaining policy instrument, as a preventive measure by enforcing highly disciplined health protocols, was the sustainable comprehensive monitoring at grassroot level.
6. Emergence of innovative health technology and implication for health system
The complexity of policy innovation implementation resulting from mixing between public health resolution and economic interest will trigger the emergence of innovative health technology, which implies health system improvement.
Health technology innovation had been emerging during the period of LSSR implementation. Indonesia had been building innovation capability through scientific research, technology development and innovation solution to deal with COVID-19. It was initiated by the consortium of research and innovation on COVID-19. The consortium has produced 55 technology products, nine of which became superior innovative technology products [68]. There is one innovative technology product (the brand is Genose) has been widely used for COVID19 detection. This superior Indonesian-made COVID-19 breath analyzer sensitivity is comparable to Rapid Test- Polymerase Chain Reaction or RT-PCR [69]. All products are the result of R&D cooperation between the government, academia and domestic industry. Indonesia also has been building innovation capability in basic research for vaccine invention to be used for curing COVID-19 by vaccination. It is hoped that the vaccine developed by the Eijkman Biomolecular Research Institute will be produced by the state-owned biomedical company Biofarma Indonesia in March 2021 [70]. Biofarma Indonesia is one of the global manufacturers engagements in the COVID-19 vaccine research, development and supply [71].
The emergence innovative health technology should not only strengthen health system preparedness during the covid-19, but more importantly it also offers an opportunity to re-examine the strengths and deficiencies of entire health system for better health care in future. The policy implication of those findings for health system and health innovation are: First, the rapid initial policy response as the point of leverage for the successful stopping of infectious disease outbreaks, it required the health system to function. Furthermore, the preparedness of health system elements to function well requires continuous upgrading of health material resources and structures as well as health human resources and institutional change. Second, in the context of enhancing innovation capability in health sector, emerging health innovations in medical supply equipment, devices, drug development and vaccine based on R&D investment needs to be consistently supported by the government. The national research and innovation priority should allocate sufficient resources, advanced facilities and funds for health technology research and bridging the innovation to be commercialized through mass production by the industrial sector.
7. Conclusion
The conclusion is the complexity of policy innovation implementation resulting from mixing between public health resolution and economic interest will trigger the emergence of innovative health technology, which implies health system improvement. The findings revealed that: First, policy innovation based on a science-mix category created the complexity of policy enforcement, affected the scale and speed of COVID-19 transmissions, and triggered the emergence of innovative health technology (i. e. Genose). Second, despite policy innovation in early COVID-19 handling it was relatively less successful due to restricting factors in policy implementation but provided a new market for emergence of innovative health technology. Third, less effectivity of large-scale social restriction (LSSR) policy intervention to handle COVID-19 in Indonesia because of constraints to execute against: the rapidness of LSSR intervention time, strict control of transmission speed, and consistent control of transmission scale.
Limitation of study was the methodology of system dynamics, which was intended to explain the patterns of problematic behaviors caused primarily by the design of feedback structure inside the system. In this study, the feedback structure was based on the perspective of policy innovation, where different perspectives lead to different designs of the feedback structure. Other system dynamic models based on different perspective (for further study) are possible so long as the models are designed to understand why the patterns of problematic behaviors occurred.
Policy insight from the study revealed
First, the rapidness of LSSR intervention time was the point of leverage to curtail the time of controlling pandemic, and effective control by enforcing counter intuitive policy response would stop local transmission amplification. This finding was in line with the empirical experience on the success of very rapid response in COVID-19's handling, as proven by Vietnam and Taiwan. Second, the health system preparedness is the key to execute a rapid response and successful managing COVID-19. Third, the emergence of innovative health technology had strengthened health system preparedness during the covid-19. But more importantly it should provide an opportunity to re-examine the strengths and deficiencies of entire health system for a better health care.
Scientific contributions of this study were
First, the original framework for seeing the whole picture of early COVID-19 handling, which was formulated into original model of system dynamics. Second, revealing the emergence of innovative health technology was driven by complexity of crisis which needed quick solutions and will enrich the concept of Burmaoglu, Sartenaer, & Porter [13] on technological emergence as a cyclic process in highly creative scientific networks. Third, understanding the reality of a policy innovation dynamic in the past contributed to enrich historically sensitive policy making model in policy science [14]. The practical contribution of the study was the feedback for policy makers to raise the effectivity of epidemic or pandemic handling in future, upgrade the health system, and increase in health technology innovation capability.
Notes
-
1.
Authors declare no conflict of interest in writing this article. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
-
2.
Numeric data generated by computer simulation in this article will be made available by authors upon request.
-
3.
All authors had equal contribution to this article and had responsibility to this publication
Authors’ statement
Authors express gratitude to the very constructive reviewers' suggestion to make this article eligible for publication in TIS.
Authors thank very much indeed for the excellent reviewers' comments and suggestion on analytical framework (Fig. 1) and model (Fig. 2).
- The most important suggestion by reviewers has substantially elevated the scientific value of this article by putting clear statement on:
- First, the framework (Section 2.1) contains four concepts: i. . Policy innovation role, ii. Interplay between public health resolution and economic interest, iii. Emergence of innovative health technology from dynamic complexity. iv. Implication for health system.
- Second, the basic thesis of this article is: The complexity of policy innovation implementation resulting from mixing between public health resolution and economic interest will trigger the emergence of innovative health technology, which implies health system improvement.
Acknowledgement
Authors indebted to Dr. Noel Taylor Moore, the English editor of the article.
Appendix 1. System dynamics model validation for COVID-19 handling in Indonesia
Appendix 2.
Appendix 3.
References
- 1.Pisano G.P., Sadun R., Zanini M. March 27). Lessons from Italy's response to Coronavirus. Harv. Bus. Rev. 2020 https://hbr.org/2020/03/lessons-from Italys-response-to-coronavirus [Google Scholar]
- 2.Peng F., Tu L., Yan Y., Hu P., Wang R., Hu Q., Cao F., Jiang T., Sun J., Xu G., Chang C. Management and treatment of VOVID-19: the Chinese experience. Can. J. Cardiol. 2020:1–16. doi: 10.1016/j.cjca.2020.04.010. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ha B.T.T., Quang L.N., Mirzoev T., Tai N.T., Thai P.Q., Dinh P.C. Combating the COVID-19 epidemic: experiences from Vietnam. Int. J. Environ. Res. Publ. Health. 2020;(17):3125. doi: 10.3390/ijerph17093125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Intawong K., Olson D., Chariyalertsak S. Application technology to fight the COVID-19 pandemic: lessons learned in Thailand. Biochem. Biophys. Res. Commun. 2020;xxx(xxxx) doi: 10.1016/j.bbrc.2020.10.097. xxx (article in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salvador-Carulla L., Rosenberg S., Mendoza J., Tabatabaei-Jafari H. Rapid response to crisis: health system lessons from the active period of COVID-19. Health Pol. Technol. 2020 doi: 10.1016/j.hlpt.2020.08.011. xxx (xxxx) xxx (article inpress) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mas’udi W., Winanti P.S. In: (2020). COVID-19 Handling Governance in Indonesia (Chapter 1. Mas’udi W., Winanti P.S., editors. Gajahmada University Press; Yogyakarta: 2020. COVID-19: from health crisis to governance crisis; pp. 3–15. (In Indonesian) [Google Scholar]
- 7.Maybin J. Palgrave Macmillan; New York: 2016. Producing Health Policy: Knowledge and Knowing in Government Policy Work; p. 141. [Google Scholar]
- 8.Moatti J.-P. Thelancet.com/public-health; 2020. The French Response to COVID-19: Intrinsic Difficulties at the Interface of Science, Public Health, and Policy; p. e255. 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Savirani A., Prasongko D. In: COVID-19 Handling Governance in Indonesia (Chapter 14. Mas’udi W., Winanti P.S., editors. Gajahmada University Press; Yogyakarta: 2020. Power, science, and governance in the response to COVID-19 pandemic; pp. 255–273. (2020) (In Indonesian) [Google Scholar]
- 10.Jakarta Post . 2020, April 8. Science First. The Jakarta Post/editorial.https://www.thejakartapost.com/academia/2020/04/08/jokowi-vs-the-scientists.html [Google Scholar]
- 11.State Secretariat Ministry – RI . The State Secretariat Ministry – RI; Jakarta: 2018. Law Number 6, 2018 Concerning Health Quarantine (Article 59, Concerning LSSR; Article 11, Paragraph 1, Concerning the Health Quarantine Implementation) [Google Scholar]
- 12.Salman A.M., Ahmed I., Mohd M.H., Jamiluddin M.S., Dheyab M.A. Scenario analysis of COVID-19 transmission dynamics in Malaysia with the possibility of reinfection and limited medical resources scenarios. Comput. Biol. Med. 2021;(133):104372. doi: 10.1016/j.compbiomed.2021.104372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burmaoglu S., Sartenaer O., Porter P. Conceptual definition of technology emergence: a long journey from philosophy of science to science policy. Technol. Soc. 2019;(59):101126. [Google Scholar]
- 14.Howlett M., Rayner J. Understanding the historical turn in the policy sciences: a critique of stochastic, narrative, path dependency and process-sequencing models of policy-making over time. Pol. Sci. 2006;(39):1–18. [Google Scholar]
- 15.Forrester J.W. Pegasus communication (reprint); Massachusetts: 1990. Principles of System; pp. 4-1–4-17. [Google Scholar]
- 16.Kim D.H., Anderson V. Pegasus communications; Waltham, Massachusetts: 1998. Systems Archetype Basics: from Story to Structure; pp. 1–208. [Google Scholar]
- 17.Aminullah E. Kompas.id (in Indonesian); 2020, May 5. The Dynamics of Policy Response to Covid-19.https://www.kompas.id/baca/opini/2020/05/05/dinamika-tangterhadap-covid-19/ [Google Scholar]
- 18.Infeksi emerging . 2020. Current Situation of Coronavirus Disease Development. Infeksi Emerging.https://infeksiemerging.kemkes.go.id/ [Google Scholar]
- 19.Barlas Y. Formal aspects of model validity and validation in system dynamics. Syst. Dynam. Rev. 1996;12(3):183–210. [Google Scholar]
- 20.Kwok K.O., Tang A., Wei V.W.I., Park W.H., Yeoh E.K., Riley S. Epidemic models of contact tracing: systematic review of transmission studies of severe acute respiratory syndrome and Middle East respiratory syndrome. Comput. Struct. Biotechnol. J. 2019;(17):186–194. doi: 10.1016/j.csbj.2019.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maeno Y. Detecting a trend change in cross-border epidemic transmission. Physica A. 2016;(457):73–81. doi: 10.1016/j.physa.2016.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kunc M., Morecroft J.D.W., Brailsford S. Special issue on advances in system dynamics modelling from the perspective of other simulation methods. J. Simulat. 2018;12(2):87–89. [Google Scholar]
- 23.Paz B., Fontaine G. A Causal mechanism of policy innovation the reform of Colombia's oil-rents management system. Open Ed. J. 2018:2–19. Columbia: Universidad de los Andes. Revista de Estudios Sociales. [Google Scholar]
- 24.Euchner J. Building a culture of innovation. Res. Technol. Manag. 2016;59(6):10–11. [Google Scholar]
- 25.Wills I. Springer Nature; Switzerland AG: 2019. Thomas Edison: Success and Innovation through Failure; pp. 246–247. [Google Scholar]
- 26.Ryan A. BII+E (The brookfield institute for innovation + entrepreneurship); Toronto: 2018. (2018). Exploring Policy Innovation: Tools, Techniques + Approaches; p. 3. Introduction, in BII+E. [Google Scholar]
- 27.Kickbusch I. In: Policy Innovation for Health. Kickbusch I., editor. Springer Science+Business Media; 2009. Policy innovation for health; pp. 1–21. 2009. [Google Scholar]
- 28.Hudson B., Hunter D., Peckham P. Policy failure and the policy-implementation gap: can policy support programs help? Pol. Des. Pract. 2019;2(1):1–14. [Google Scholar]
- 29.Den Hove S. van. A rationale for science–policy interfaces. Futures. 2007;(39):807–826. [Google Scholar]
- 30.Young J., Waylen K., Sarkki S., Albon S., Bainbridge I., Balian E., Davidson J., Edwards D., Fairley R., Margerison C., Cracken D., Owen R., Quine C., Stewart-Roper C., Thompson D., Tinch R., Van den Hove S., Watt A. Improving the science-policy dialogue to meet the challenges of biodiversity conservation: having conversations rather than talking at one-another. Biodivers. Conserv. 2014;(23):387–404. [Google Scholar]
- 31.Newman K., Capillo A., Famurewa A., Nath C., Siyanbola W. International Network for the Availability of scientific Publications (INASP); Oxford: 2013. What Is the Evidence on Evidence‐informed Policy Making? Lessons from the International Conference on Evidence‐informed Policy Making; pp. 1–18. [Google Scholar]
- 32.Grundmann R., Stehr N. Cambridge University Press; New York: 2012. The Power of Scientific Knowledge from Research to Public Policy; pp. 179–194. [Google Scholar]
- 33.Kreps D. Palgrave Macmillan; Hampshire: 2015. Complexity, and Creative Emergence; pp. 211–233. [Google Scholar]
- 34.Saurin T.A. A complexity thinking account of the COVID-19 pandemic: implications for systems-oriented safety management. Saf. Sci. 2021;134:105087. [Google Scholar]
- 35.Flood R.L., Carson E.R. Plenum Press; New York: 1988. Dealing with Complexity: an Introduction to the Theory and Application of Systems Science; pp. 205–266. [Google Scholar]
- 36.Forrester J.W. Counterintuitive behavior of social systems. Technol. Rev. 1971;73(3):52–68. [Google Scholar]
- 37.Forrester J.W. System Dynamics-A personal view of the fifty years. Syst. Dynam. Rev. 2007;23(2/3):345–358. [Google Scholar]
- 38.Dahlke J., Bogner K., Becker M., Schlaile M.P., Pyka A., Ebersberger B. Crisis-driven innovation and fundamental human needs: a typological framework of rapid-response COVID-19 innovations. Technol. Forecast. Soc. Change. 2021;169:120799. doi: 10.1016/j.techfore.2021.120799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lai L., Sato R., Ouchi K., Landman A.B., Zhang H.M. Digital health innovation to integrate palliative care during the COVID-19 pandemic. AJEM (Am. J. Emerg. Med.) 2020;xxx(xxxx):xxx. doi: 10.1016/j.ajem.2020.08.008. (article in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee D., Choi B. Policies and innovations to battle Covid-19 – a case study of South Korea. Health Pol. Technol. 2020;xxx(xxxx):xxx. doi: 10.1016/j.hlpt.2020.08.010. (article in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Setiati S., Azwar M.K. COVID-19 and Indonesia. Acta Medicana Indonesia –Indones. J. Intern. Med. 2020;52(1):84–89. [PubMed] [Google Scholar]
- 42.Palagyi A., Marais B.J., Abimbola S., Topp S.M., McBryde E.S., Negin J. Health system preparedness for emerging infectious diseases: a synthesis of the literature. Global Publ. Health. 2019;14(12):1847–1868. doi: 10.1080/17441692.2019.1614645. [DOI] [PubMed] [Google Scholar]
- 43.WHO . WHO; Geneva: 2018. Managing Epidemics: Key Facts about Major Deadly Diseases; p. 30. [Google Scholar]
- 44.Ministry of Health . Ministry of Health, Director General of Disease Prevention and Control; Jakarta: 2020. Guidelines for the Preparedness to Novel Coronavirus Infection (2019-nCoV) pp. 10–65. (P2P) [Google Scholar]
- 45.TFACH . The task force for acceleration of covid-19 handling (TFACH); Jakarta: 2020. Guidelines for Rapid Medical and Public Health Handling on COVID-19 in Indonesia; pp. 8–38. [Google Scholar]
- 46.Kumar A., Patel D.R., Nissen S.E., Desai M.Y. Never let a crisis go to waste: implementing virtual innovations during the COVID-19 pandemic for a better tomorrow in health care. JACC Case Rep. 2020;2(9):1376–1378. doi: 10.1016/j.jaccas.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Iyengar K., Mabrouk A., Jain V.K., Venkatesan A., Vaishya R. Learning opportunities from COVID-19 and future effects on health care system. Diabetes Metabo. Syndrome: Clin. Res. Rev. 2020;14:9. doi: 10.1016/j.dsx.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kesavan B.S.P., Christopher J. Impact of health care reform on technology and innovation. Hand Clin. 2020;36(2):255–262. doi: 10.1016/j.hcl.2020.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Leonard E., Kock I., Bam W. Evidence-based health innovations in low- and middle-income countries: a systematic literature review. Eval. Progr. Plann. 2020;(82):101832. doi: 10.1016/j.evalprogplan.2020.101832. [DOI] [PubMed] [Google Scholar]
- 50.Cinaroglu S., Baser O. The relationship between medical innovation and health expenditure before and after health reform. Health Pol. Technol. 2018;7(4):379–387. [Google Scholar]
- 51.Kickbusch I. Innovation in health policy: responding to the health society. Gac. Sanit. 2007;21(4):338–342. doi: 10.1157/13108509. [DOI] [PubMed] [Google Scholar]
- 52.Conversation . The Conversation/Tarahita, D.; 2020, May 20. Amid COVID-19, Indonesia Should Stop Prioritizing the Economy: Lessons from Other Countries.https://theconversation.com/amid-covid-19-indonesia-should-stop-prioritising-the-economylessons-from-other-countries-138546 [Google Scholar]
- 53.Antaranews . Antaranews (in Indonesian); 2020, July 29. Endeavoring for a Balance between COVID-19 Handling, Economy Recovery.https://en.antaranews.com/news/153258/endeavoring-for-a-balance-between-covid-19-handlingeconomy-recovery [Google Scholar]
- 54.Nathan R.P. the Rockefeller institute press; New York: 2000. Social Science in Government, the Role of Policy Researchers; p. 197. [Google Scholar]
- 55.Jakarta Post . The Jakarta post/Cahya, G.H.; 2020, February 15. ‘It's Meant to Help’: Harvard Professor Responds after Government Dismisses Study on Undetected Coronavirus Cases.https://www.thejakartapost.com/news/2020/02/14/its-meant-to-help-harvardprofessor-responds-after-government-dismisses-study-on-undetected-coronavirus-cases.html [Google Scholar]
- 56.CNN Indonesia . CNN Indonesia (in Indonesian); 2020, February 7. Mahfud: RI Is the Only Major Country in Asia Not Affected by Corona.https://www.cnnindonesia.com/nasional/20200207194915-20-472750/mahfud-ri-satu-satunyanegara-besar-di-asia-tak-kena-corona [Google Scholar]
- 57.Antaranews . Antaranews (in Indonesian); 2020, February 17. Budi Karya: COVID-19 Virus Does Not Enter Indonesia Because of “cats Rice”.https://www.antaranews.com/berita/1302390/budi-karya-virus-covid-19-tidak-masuk-indonesiakarena-nasi-kucing [Google Scholar]
- 58.CNN Indonesia . CNN Indonesia/Setyawan, F.E. (in Indonesian); 2020, March 11. Jokes Vice President call Wild Horse Milk Can Counter Corona Virus.https://www.cnnindonesia.com/nasional/20200311170241-20-482556/canda-wapres-sebut-susukuda-liar-bisa-tangkal-virus-corona [Google Scholar]
- 59.Howlett M. Why are policy innovations rare and so often negative? Blame avoidance and problem denial in climate change policy-making. Global Environ. Change. 2014;(29):395–403. [Google Scholar]
- 60.Jakarta Post . The Jakarta Post/Fachriansyah; 2020, March 22. COVID-19: Inadequate Medical Supplies Take Toll on Lives of Indonesian Medical Workers.https://www.thejakartapost.com/news/2020/03/22/covid-19-inadequate-medicalsupplies-take-toll-on-lives-of-indonesian-medical-workers.html R, Gunawan, A. and Hasani, A. [Google Scholar]
- 61.Ghaffarzadegan N., Lyneis J., Richardson G.P. How small system dynamics models can help the public policy process. Syst. Dynam. Rev. 2011;27(1):22–44. [Google Scholar]
- 62.CNN Indonesia . CNN Indonesia (in Indonesian); 2020, May 24. 465 Thousand Vehicles Get Out of Jakarta since May 17, 2020.https://www.cnnindonesia.com/nasional/20200524160912-20-506491/465-ribu-kendaraankeluar-dari-jakarta-sejak-17-mei-2020 [Google Scholar]
- 63.Kompas . Kompas/Deti Mega Purnamasari (in Indonesian); 2021, April 20. Muhadjir Acknowledges that the Government Was Careless at the Beginning of the Covid-19 Pandemic.https://nasional.kompas.com/read/2021/04/20/13572641/muhadjir-akui-pemerintah-teledor-saat-awal-pandemi-covid-19 [Google Scholar]
- 64.Aminullah E. Kompas.id (in Indonesian); 2020, July 13. COVID-19, Needs Sustainable Monitoring at Downstream.https://kompas.id/baca/opini/2020/07/13/covid-19-perlu-pemantauan-berkelanjutan-di-hilir/ [Google Scholar]
- 65.Than H.M., Nong V.M., Nguyen C.T., Tran N.H.T., Do C.D., Pham T.N. Management of mild cases of COVID-19 in low resource countries: an experience in Vietnam. J. Microbiol. Immunol. Infect. 2020 doi: 10.1016/j.jmii.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.HU CSSE COVID-19 Data, https://github.com/CSSEGISandData/COVID-19.
- 67.Engen N.V., Steijn B., Tummers L. Do consistent government policies lead to greater meaningfulness and legitimacy on the front line? Publ. Adm. 2019;(97):97–115. [Google Scholar]
- 68.Kompas . Kompas/Uly, Y. A. (in Indonesian); 2020, May 20. Handling Covid-19, Jokowi and Kemenristek Launched 55 Innovative Products.https://www.kompas.com/sains/read/2020/05/20/170200723/tangani-covid-19-jokowi-dan-kemenristek-luncurkan-55-produk-inovasi [Google Scholar]
- 69.Conversation . The Conversation/Tarahita, D.; 2021, March 20. Indonesian-made-covid-19-breathalyser-sensitivity-comparable-to-RT-PCR.https://theconversation.com/indonesian-made-covid-19-breathalyser-sensitivity-comparable-to-rt-pcr-155497 [Google Scholar]
- 70.Media Indonesia . Media Indonesia/Putri Rosmalia Octaviyani; 2020, June 26. Eijkman Prepares Red and White Vaccine.https://m.mediaindonesia.com/read/detail/323489-lawan-covid-19-eijkman-siapkanvaksin-merah-putih P. S., (in Indonesian) [Google Scholar]
- 71.Pagliusi S., Jarrett S., Hayman B., Kreysa U., Prasad S.D., Reers M., Thai P.H., Wu K., Zhang Y.T., Baek Y.O., Kumar A., Evtushenko A., Jadhav S., Meng W., Dat D.T., Huang W., Desai S. Emerging manufacturers engagements in the COVID-19 vaccine research, development and supply. Vaccines. 2020;(38):5418–5423. doi: 10.1016/j.vaccine.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]