Figure 3 |. Effects of glucocorticoids on inflammation.
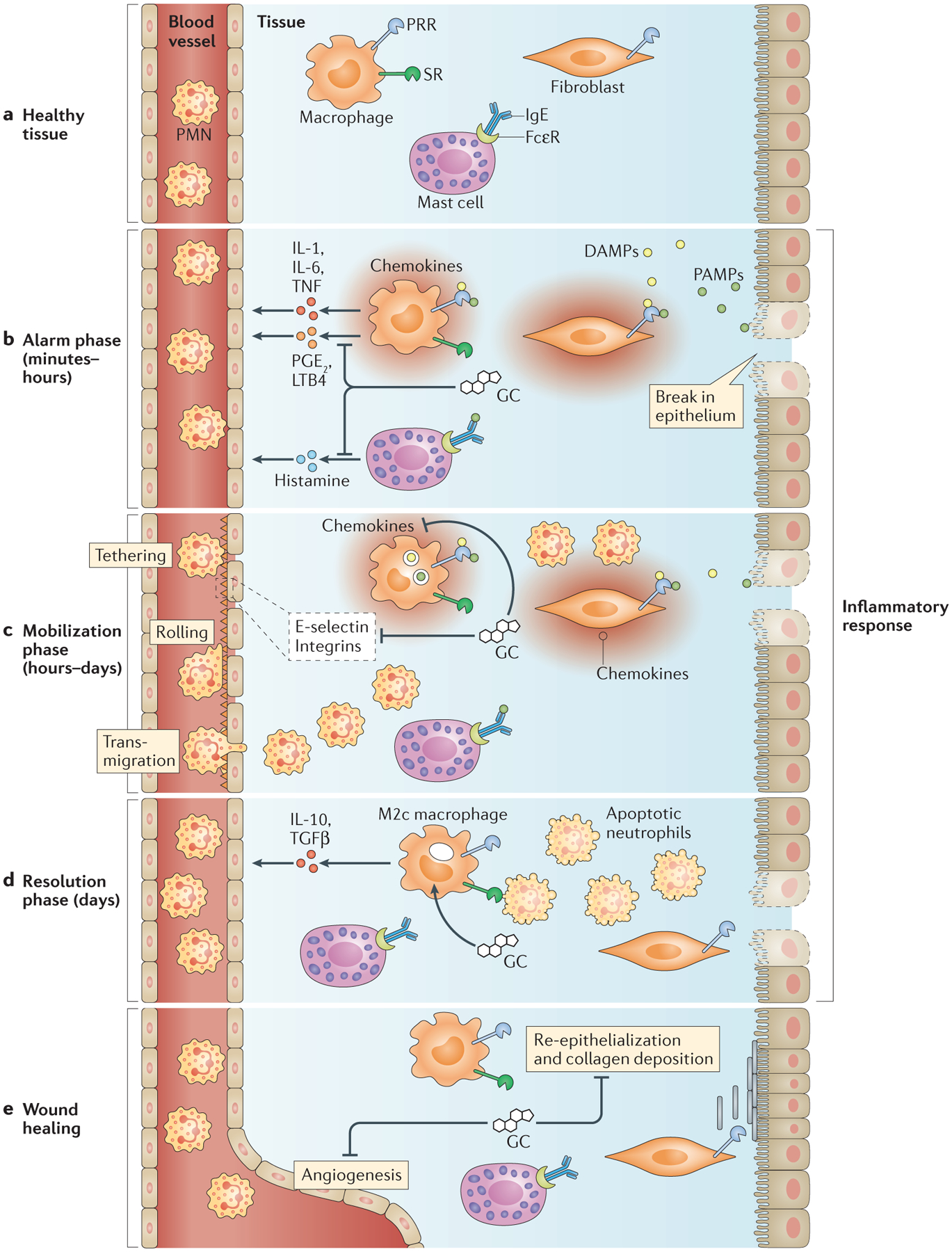
a | In healthy tissue, tissue-resident macrophages, fibroblasts and stromal cells express pattern recognition receptors (PRRs) and scavenger receptors (SRs). Mast cells bind soluble IgE via Fcε receptors (FcεRs). b | During the alarm phase of inflammation, pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs) trigger PRR signalling, which induces the production of inflammatory mediators, including cytokines, prostaglandin E2 (PGE2) and leukotriene B4 (LTB4). Antigens bind FcεR-bound IgE on mast cells to induce histamine release. Glucocorticoids (GCs) dampen signalling through PRRs, FcεRs and cytokine receptors. c | During the mobilization phase of inflammation, inflammatory mediators induce the display of adhesion molecules — including E-selectin, chemokines and integrins — on the vascular endothelium to recruit leukocytes, especially polymorphonuclear leukocytes (PMNs), into the tissue. Extravasating leukocytes follow chemokine gradients towards inflammatory sites. GCs inhibit the expression of E-selectin, chemokines and integrins to reduce leukocyte recruitment. d | During the resolution phase of inflammation, GCs promote the differentiation of alternatively activated ‘M2c’ macrophages, which clear apoptotic PMNs and secrete anti-inflammatory factors. e | The resolution of inflammation triggers wound healing, which is characterized by re-epithelialization, collagen deposition and angiogenesis. As GCs inhibit these processes, optimal wound healing probably depends on reduced glucocorticoid production. IL, interleukin; TGFβ, transforming growth factor-β; TNF, tumour necrosis factor.
