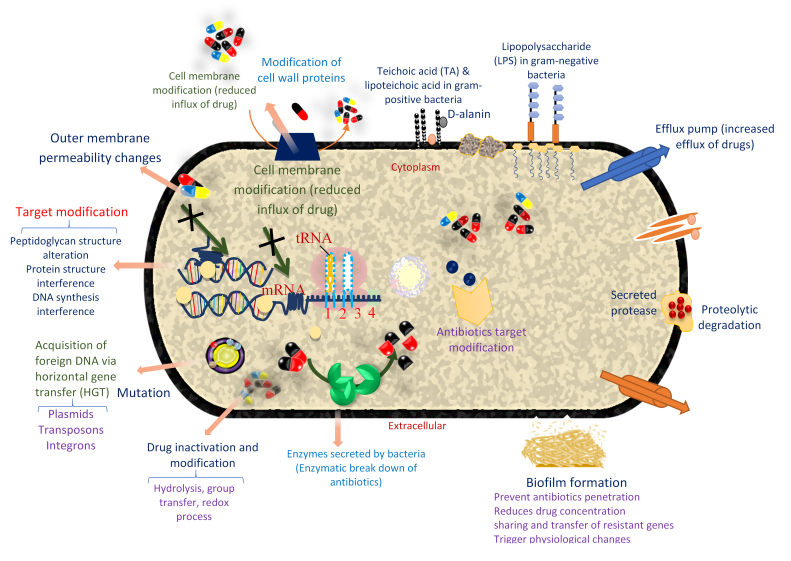
Figure 3.
Mechanism of bacteria resistance to antibiotics and AMP. Resistance to antibiotics is generally due to cell membrane modification, target modification, enzymatic breakdown of antibiotics, drug inactivation and modification, mutation, and acquisition of foreign DNA via HGT and biofilm formation. Some of these resistance mechanisms in antibiotics are shared by AMP. Specifically, in AMP, resistance is due to extracellular protease-mediated degradation, altered cell surface changes, repulsion of AMP through changes in the cell wall and membrane surface changes, biofilm formation, modification of host cellular processes, and LPS modification. There is also AMP sequestration/inactivation and AMP-induced gene induction/downregulation. Inactivation of some genes can also lead to loss of LPS production and reduction in the binding of AMP. The anionic feature of bacterial cell membrane makes them a good binding site for cationic AMP. Therefore, teichoic acid modification reduces the negative charge in the bacterial cell membrane. Resistance to AMP is also due to the active efflux of AMPs. D-alanine alteration of teichoic and lipoteichoic acids in gram-positive bacteria is another AMP resistance mechanism in some bacteria. Moreover, some pathogens, especially the gram-negatives known for the presence of diverse polysaccharides such as K. pneumonia, resist peptides by forming capsular polysaccharides [23,165].