Abstract
Acid attacks are on the rise, and they cause extensive and deep burns, especially on the face. The treatments used to improve the aesthetic, functional and social impact of non-acid scars do not always prove useful for acid scars. This article reports the case of a woman with an extended, mature, acid facial scar, caused by sulfuric acid assault, treated with a recent new procedure that combines the application of vacuum and electromagnetic fields. Before and after the treatment, the aesthetic appearance, and motor function of the face and neck were evaluated, as well as the level of hydration, the amount of sebum, the elasticity, and the pH of the skin. The improvements highlighted after the treatment of the aesthetic and functional characteristics of the face and neck, and of the physical parameters of the skin seemed to indicate that this particular treatment induces tissue regeneration, even in the nerve component. However, it is evident that the rehabilitation pathways of facial wounds and scars must be personalized, and must include continuous psychological support for the patient.
Keywords: acid attack, burn, scar, V-EMF, regenerative treatment
1. Introduction
The data on the increase in the number of chemical attacks are alarming [1,2,3,4,5]. Mortality associated with these actions is very high [4,5,6,7,8], and, considering that the victim is often attacked in the face, the sequelae completely destroy her/his life because the damage is aesthetic, functional and social [9,10,11,12,13,14,15,16,17].
Among the acids most used to perform the attacks is sulfuric acid, which on the skin has a double action, both chemical and thermal, due to its properties [4,7,18,19]. The effects of prolonged and massive exposure to this acid, if the victim survives, are both disfiguring and dysfunctional [4,5,7,8,20,21,22] due to the long healing times of the wounds and the fact that numerous reconstructive surgeries are often necessary [7,23,24].
There are numerous more or less invasive treatments aimed at improving residual aesthetic stigmatizations and facial dysfunctions (Table 1, [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43]), but an optimal treatment has not yet been identified [44,45]. In fact, although many interventions appear promising, sometimes the results reported in the literature are conflicting [32,33,34,35], or interventions suitable for some types of scars are not effective for others [29,43,44,45]. This may depend on the extreme variability of individual situations, for each of which a personalized medical-surgical-rehabilitation path should be identified.
Table 1.
Most common scar treatments.
| Invasiveness | Type | References |
|---|---|---|
| Non-invasive | Silicone sheet coating | [25] |
| Topical treatment | [26,27] | |
| Application of mesenchymal stem cells in tissue scaffolds | [28] | |
| Minimally invasive | Corticosteroid injection | [29] |
| (principally injectable therapies) | Botox injection | [30] |
| Mesenchymal stem cells injection (principally obtained from fat grafting) |
[31,32,33] | |
| Hyaluronic acid filler | [34,35] | |
| Invasive | Cryotherapy (generally applied after surgical excision) |
[36] |
| Others (more/less invasive) | Laser - minimally invasive—non-ablative - invasive—ablative |
[37,38,39] |
| Shock wave therapy | [40] | |
| Radiofrequencies application | [41] | |
| Microneedling | [42] | |
| Dermabrasion (combined with regenerative agents) | [43] |
In this report we present the case of a woman with a mature scar, extending to the whole face, caused by a sulfuric acid attack and treated with a new recent multi-technique procedure. The latter is a form of therapy, generally used for small scars [46], which combines the application of vacuum and electromagnetic fields (V-EMF).
V-EMF Treatment
In V-EMF therapy, a medium frequency electromagnetic field is applied in a vacuum regime, directly to the affected area. The waves used are radio waves with a frequency range of 450–2000 kHz (the frequency range generally used in resistive-capacitive diathermy is 450–1200 kHz). Energy is transferred to the tissues in a capacitive way, by means of a single metal electrode, suitably shielded by insulating material. The second conductive plate of the capacitor is given by the body tissue, and this implies that the electromagnetic charge is concentrated near the isolated electrode, i.e., in the superficial tissues [47,48,49].
From the biomedical point of view, an endogenous diathermic effect and a magneto-mechanical effect are simultaneously induced on the treated tissues. The thermal effect is due to the transformation of the kinetic energy of the ions, which move due to electromagnetic waves, into heat (Joule effect) [50,51,52]. The magneto-mechanical effect is linked to the piezoelectricity of some tissues, i.e., to their ability to mechanically alter their structure following a magnetic stress [53,54].
The first effect determines an increase in metabolic reactions. There is an increase in microcirculation, with a consequent increase in the number of gaseous exchanges between blood and tissues. The catabolic products are drained more quickly and the diapedesis of granulocytes, macrophages, and of the cells involved in inflammatory and reparative processes increases. In addition, the “cell killing” effect of senescent and damaged cells occurs [48,49,55,56,57,58]. The rise in temperature extends deeper [48,49,55], although the actual amount progressively decreases as it deepens from the surface of the skin [47,58]. However, this involves an overall analgesic effect [47,49,56,59], and consequently a well-being after therapy, with muscle relaxation, an increase in muscle flexibility [60,61], a reduction in pain associated with movements, and an increase in the elasticity of the connective tissue [49,56,61,62].
The second effect occurs mainly at the level of connective tissue, which is the body tissue with the most significant piezoelectric characteristics. The structural deformation of this tissue favours the resolution of fibrotic states, and the rebalancing of the extracellular matrix [63,64].
The combination of the two effects improves the repair of all involved tissues, and wound healing. We can speak of a real regenerative effect, given that there is an overall tissue regeneration [49,58,59], including that of the neural component [65,66,67,68].
The application of electromagnetic waves in a vacuum regime (100–150 millibar) amplifies the effects that these waves induce on the tissues. In particular, the vacuum appears to play a fundamental role in the restructuring of the extracellular matrix, since the induced mechanical stimulus activates the endothelial cells, the fibroblasts and the cutaneous myofibroblasts [69,70].
2. Materials and Methods
2.1. Case
We present the case of a 63-year-old female, attacked with sulfuric acid on 28 May 2012 and hospitalized from 28 May 2012 to 2017 at the Cardarelli Hospital in Naples, Italy. Here she underwent 27 surgeries for the reconstruction of the face and neck, through autologous skin grafts taken from different parts of the body, and 3 autologous lipofilling procedures. After the surgeries, she did not use an elastic compression mask at home. From the event, the patient has been followed from a psychological point of view by the Association “Women for Women Against Violence”.
After 10 years from the attack, on the face and neck, she visually showed retraction of the skin and marked dyschromia. Evident were the flattening of the nose, presumably due to the retraction of the peri-labial tissue, and the deformation of the neck, with the absence of the typical right-angled conformation of the platysma and the presence of a diagonal line shape.
Face and neck showed hardening and thickening of the skin surface, and loss of sensation, with absence of both slight tactile perception and pinching.
From a functional point of view, the deformation of the nose involved the reduction of the nasal rostrums, resulting in the need to breathe through the mouth. The deformation of the neck reduced its motility. The rotational movement of the head appeared limited and sometimes painful on the side opposite to that of rotation. The retraction of the skin tissue at the level of the face induced traction of the lower lip with consequent involuntary opening of the mouth, in case of extension of the head.
2.2. Methods
The patient underwent V-EMF treatment, that was delivered according to the Biodermogenesi® method, using the Bi-one® LifeTouchTherapy device (Expo Italia Srl, Florence, Italy), and with the protocol already detailed in Veronese et al. [46]. Specifically, the subject underwent a cycle of 12 sessions, lasting 25 min each, with the frequency of one session a week, in the period April–May 2022. The vacuum was applied at 100–150 millibars. The frequency used for the generation of the EMF varied between 0.5 and 2 MHz, i.e., the supplied power was on average 4 W. The variability was linked to an automatic self-regulation system of the device, linked to an automatic feedback control of the quantity of energy absorbed by the skin. This amount is, in turn, related to the thickness of the treated skin.
A neutral alcohol-based cleanser was used on the skin before starting the procedure. Before each session, the operator identified the main fibrous excerpts present by palpation. In an initial phase lasting about 15 min, the handpiece was applied to the fibrotic excerpts, first parallel to their progression (10 min), to obtain a progressive softening action, and subsequently (5 min), tangentially. In the remaining 10 min, the handpiece was passed over the whole face and neck, to generalize the action.
Before the first treatment session (T0) and a week after the last session (T1) the level of hydration, the quantity of sebum, the elasticity, and the pH of the skin were measured at the level of the center of the forehead, of the left and right cheekbones, and in the center of the chin. To make the measurements the Skin Plus® device (Lemi s.r.l., Casalbuttano and Uniti, Italy) was used. Measurement was performed 2 times per test type and per location. The value obtained from the first survey was considered valid if confirmed by a second survey, with a tolerance of 5%. In the presence of greater differences, the average of the 2 measured values was taken.
At T0 and T1, photographs of the forehead, middle third of the face, nose in profile, and lower third of the face were taken for a qualitative evaluation of the effects of the treatment. A Nikon D500 camera was used, at a distance of 1 m from the patient, with artificial light.
3. Results
The level of hydration, the amount of sebum, the elasticity, and the pH of the skin recorded at T0 and T1 are shown in Table 2. For all tests and all sites, the 2 measurements taken differed by 2–3%. Therefore, the first value detected was considered valid.
Table 2.
Skin parameters.
| Forehead | Right Cheekbone | Left Cheekbone | Chin | |||||
|---|---|---|---|---|---|---|---|---|
| T0 | T1 | T0 | T1 | T0 | T1 | T0 | T1 | |
| Hydration Level | 12 | 18 * | 32 | 46 | 35 | 86 | 34 | 73 |
| normal value | >44/100 | |||||||
| Sebum Quantity | 27 | 43 ** | 25 | 65 ** | 27 | 70 ** | 29 | 63 ** |
| normal value | <40/100 | |||||||
| Skin Elasticity | 18 | 48 | 16 | 45 | 16 | 44 | 15 | 63 ** |
| normal value | >20/50 | |||||||
| Skin pH | 3.7 | 4.9 | 3.6 | 5.0 | 3.6 | 4.8 | 3.2 | 4.9 |
| normal range | 4.1–5.8 | |||||||
* increase below normal levels; ** increase above normal levels.
After the treatment, 2 of the 4 tested parameters did not normalize in the forehead area. The level of skin hydration remained practically unchanged, while the amount of sebum produced exceeded the upper limit of the norm. The latter data was common to all the facial areas considered.
In the cheek there was an increase above the normal range of skin elasticity. Therefore, even for the cheek 2 out of 4 parameters did not normalize.
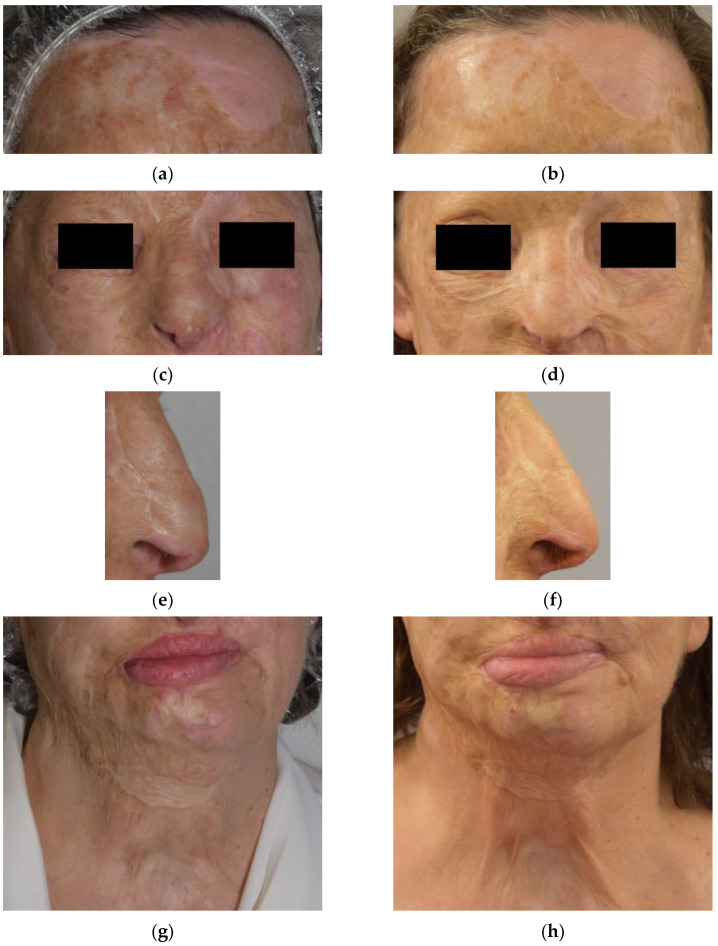
On the surface, the skin appeared less tight. Some scar furrows appeared smooth. On palpation, the fibrotic tissue mainly present in the nose, chin and neck was softer and less adherent. The structure of the nose and the lower middle third of the face were particularly reshaped, presenting a more natural conformation. The photographic comparison at T0 and T1 is shown in Figure 1.
Figure 1.
Photographs just before, and 1 week after the V-EMF treatment of the forehead (a,b), middle third of the face (c,d), nose (e,f), and lower third of the face (g,h).
Finally, it should be noted that during the single treatment sessions the subject did not report any discomfort. No side effects or pain were reported during treatment and at T1.
4. Discussion
In cases of acid assault, the face is generally the most affected part of the body [3,4,5]. The first necessity when a patient arrives at the hospital with this type of injury is always to save her/his life. Only when the survival of the subject has been guaranteed is it possible to intervene to try to preserve all the functions of the face (primarily the visual one), promote rapid healing, and minimize visual stigmatization [19,71].
The precocity of treatments seems to indicate a better functional and aesthetic wound healing, with the formation of less extensive and shallow scars [24,72,73]. Unfortunately, timeliness is not always possible, as in the case described in this study, where healing times were very long. In addition, there are people who have old scars and/or who have not benefited from the various treatments performed [44,45]. In these cases, a long time passes after the initial injury. Thus, a treatment may, instead of promoting regeneration (as in the proliferative/modulating phase of healing), cause a resumption of an inflammatory process. This process may ultimately culminate in a major proliferative phase, but first by inducing a major distress phase in the treated subject.
The V-EMF procedure has the advantage of being completely non-invasive and the results obtained with the treatment of small scars are highly encouraging [46]. The application of this treatment on an extensive scar like that of the case described, although not a bet, did not guarantee the results obtained. The latter are extremely interesting, especially from a functional point of view. It should be noted that even the aesthetic results achieved are not trivial. For instance, the regeneration of the nose is evident, both in the skin and in the redefinition of the nasal rostrums (Figure 1c–f).
The reappearance of tactile sensitivity and the improvement of cranio-cervical motility further highlight the regeneration of the tissues damaged by the burn, a regeneration that also includes the neural components. Furthermore, the changes in skin characteristics after treatment (Table 2) demonstrate the regeneration of the skin texture and the normalization of many of its properties. The authors believe that the fact that sebum production increases beyond normal levels underscores the skin’s strong natural response to treatment. And, therefore, it is not seen as a negative datum. The greater elasticity of the cheek could be linked to the greater amount of adipose tissue generally present in this area.
Given the results obtained, in the absence of any discomfort, it can be concluded that the procedure did not reactivate a situation of pain and inflammation, but a tissue regenerative activation was directly induced. This is particularly interesting also considering the age of the treated subject, an age in which the regenerative capacity in general, and of the face in particular, can be the subject of discussion.
In the literature there are not many analyses relating to this technique for the treatment of scars, given that it was recently introduced. In the two works that describe it [46,74], for ethical reasons, no invasive analyzes (e.g., biopsy analysis) were performed to evaluate the effectiveness of the method. The outcomes of the various treatments were evaluated by non-invasive measurements and were considered satisfactory in both studies. Nevertheless, in three studies V-EMF therapy was applied to stretch marks, often referred to as atrophic scars [75,76,77]. Two of these studies also reported histological evaluations of biopsies taken after the treatments [76,77]. These evaluations highlighted a tissue reorganization with restoration of the original volume. A neoformation of collagen shoots and elastin fibers was observed, with restructuring of the basement membrane, and of the extracellular matrix underlying the striae. Although the degree of tissue degeneration linked to chemical burn scars is undoubtedly not comparable to the structural alteration linked to the presence of a stretch mark, the reported observations highlight a regenerative reaction in the tissue treated with V-EMF therapy. This is certainly an important fact.
Studies in the literature described different types of treatment for burn cases, with excellent results for some aspects and absent or negative results for others [31,35,37,40,41]. One wonders if the combination of several different treatments can be significant for the full aesthetic and functional recovery, and for the improvement of all aspects of the quality of life of burned subjects. For this particular category of patients, it seems not only useful, but necessary to define a personalized therapeutic path. V-EMF treatment, which is a multi-technique procedure, appears to respect this principle. Perhaps in these particular subjects, with extensive and deep burn scars and the presence of painful fibrotic shoots, it may be necessary for patients to undergo multiple cycles of V-EMF therapy, to progressively resolve/improve their pathological state.
Finally, it is essential not to forget the fact that people with scars due to acid attacks are first of all victims, which must be followed from a psychological point of view, even during treatments, given the strong emotional impact that aesthetic-functional recovery can have [78,79,80].
5. Conclusions
Undoubtedly, the application of V-EMF treatment to a greater number of subjects is necessary to confirm the results obtained for the subject of this report. Considering this case, it can be concluded that V-EMF therapy appears to be beneficial for mature and widespread scars in burn outcomes. It is very promising that both aesthetic and functional recovery have been observed.
Acknowledgments
The authors wish to express their gratitude to Expo Italia Srl, which promoted the RigeneraDerma 2022 initiative, aimed at donating 500 Biodermogenesi® treatments to women who have scars caused by violence, and who cannot bear the economic burden of the therapies. The authors also wish to thank the Association “Women for Women Against Violence” for the incessant activity carried out against undeclared violence, hidden in the home, and for the constant support to the victims.
Author Contributions
Conceptualization, S.V., B.B., A.M.M. and A.S.; methodology, S.V., B.B. and A.M.M.; formal analysis, S.V. and A.S.; investigation, B.B. and A.M.M.; data curation, S.V., B.B. and A.M.M.; writing—original draft preparation, S.V. and A.S.; writing—review and editing, S.V., B.B., A.M.M. and A.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. Ethical review and approval were waived for this study, because the treatment and analyzes performed are within the standard of care for individuals with the described disease.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
All the data used for this study are present in the text.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rasouli H.R., Ebrahimi A., Motamedi M.H.K. Raising awareness against acid attacks. Lancet. 2015;385:772–773. doi: 10.1016/S0140-6736(15)60435-4. [DOI] [PubMed] [Google Scholar]
- 2.Ahmed F., Maroof H., Ahmed N., Sheridan R. Acid attacks: A new public health pandemic in the west? Int. J. Surg. 2017;48:32–33. doi: 10.1016/j.ijsu.2017.09.073. [DOI] [PubMed] [Google Scholar]
- 3.Mannan A., Ghani S., Clarke A., Butler P.E. Cases of chemical assault worldwide: A literature review. Burns. 2007;33:149–154. doi: 10.1016/j.burns.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 4.Karunadasa K.P., Perera C., Kanagaratnum V., Wijerathne U.P., Samarasingha I., Kannangara C.K. Burns due to Acid Assaults in Sri Lanka. J. Burn Care Res. 2010;31:781–785. doi: 10.1097/BCR.0b013e3181eed228. [DOI] [PubMed] [Google Scholar]
- 5.Peck M.D. Epidemiology of burns throughout the World. Part II: Intentional burns in adults. Burns. 2012;38:630–637. doi: 10.1016/j.burns.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 6.Herndon D. Total Burn Care. 5th ed. Elsevier Saunders; New York, NY, USA: 2017. [Google Scholar]
- 7.Micheau P., Lauwers F., Vath S.B., Seilha T.C., Dumurgier C., Joly B. Brûlures caustiques. Étude clinique à propos de 24 observations de brûlures par acide sulfurique au Cambodge [Caustic burns. Clinical study of 24 patients with sulfuric acid burns in Cambodia] Ann. Chir. Plast. Esthet. 2004;49:239–254. doi: 10.1016/j.anplas.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Behera C., Rani A., Pradhan M., Dikshit P.C. Fatal corrosive attack: A study of 13 cases from central Delhi, India. Am. J. Forensic Med. Pathol. 2014;35:109–112. doi: 10.1097/PAF.0000000000000071. [DOI] [PubMed] [Google Scholar]
- 9.Van Loey N.E.E., Van Son M.J.M. Psychopathology and psychological problems in patients with burn scars: Epidemiology and management. Am. J. Clin. Dermatol. 2003;4:245–272. doi: 10.2165/00128071-200304040-00004. [DOI] [PubMed] [Google Scholar]
- 10.Yu B.-H., Dimsdale J.E. Posttraumatic stress disorder in patients with burn injuries. J. Burn Care Rehabil. 1999;20:426–433. doi: 10.1097/00004630-199909000-00017. discussion 422–425. [DOI] [PubMed] [Google Scholar]
- 11.Lodha P., Shah B., Karia S., De Sousa A. Post-Traumatic Stress Disorder (Ptsd) following burn injuries: A comprehensive clinical review. Ann. Burn. Fire Disasters. 2020;33:276–287. [PMC free article] [PubMed] [Google Scholar]
- 12.De Sousa A., Sonavane S., Kurvey A. Psychological issues in adult burn patients. Delhi Psychiatry J. 2013;16:24–33. [Google Scholar]
- 13.Öster C., Sveen J. The psychiatric sequelae of burn injury. Gen. Hosp. Psychiatry. 2014;36:516–522. doi: 10.1016/j.genhosppsych.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 14.Tebble N.J., Adams R., Thomas D.W., Price P. Anxiety and self-consciousness in patients with facial lacerations one week and six months later. Br. J. Oral Maxillofac. Surg. 2006;44:520–525. doi: 10.1016/j.bjoms.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 15.Van den Elzen M.E., Versnel S.L., Hovius S.E., Passchier J., Duivenvoorden H.J., Mathijssen I.M. Adults with congenital or acquired facial disfigurement: Impact of appearance on social functioning. J. Cranio-Maxillofac. Surg. 2012;40:777–782. doi: 10.1016/j.jcms.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 16.Hoogewerf C.J., van Baar M.E., Middelkoop E., van Loey N.E. Impact of facial burns: Relationship between depressive symptoms, self-esteem and scar severity. Gen. Hosp. Psychiatry. 2014;36:271–276. doi: 10.1016/j.genhosppsych.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 17.Ziolkowski N., Kitto S.C., Jeong D., Zuccaro J., Adams-Webber T., Miroshnychenko A., Fish J.S. Psychosocial and quality of life impact of scars in the surgical, traumatic and burn populations: A scoping review protocol. BMJ Open. 2019;9:e021289. doi: 10.1136/bmjopen-2017-021289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lewis C.J., Al-Mousawi A., Jha A., Allison K.P. Is it time for a change in the approach to chemical burns? The role of Diphoterine® in the management of cutaneous and ocular chemical injuries. J. Plast. Reconstr. Aesthetic Surg. 2017;70:563–567. doi: 10.1016/j.bjps.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 19.Gnaneswaran N., Perera E., Perera M., Sawhney R. Cutaneous chemical burns: Assessment and early management. Aust. Fam. Physician. 2015;44:135–139. [PubMed] [Google Scholar]
- 20.Press B. Thermal, electrical and chemical injuries. In: Sherrel J., Aston M.D., editors. Grabb and Smiths’ Plastic Surgery. 5th ed. Raven Press; New York, NY, USA: 1997. pp. 161–189. [Google Scholar]
- 21.Yeong E.K., Chen M.T., Mann R., Lin T.-W., Engrav L.H. Facial mutilation after an assault with chemicals: 15 cases and literature review. J. Burn Care Rehabil. 1997;18:234–237. doi: 10.1097/00004630-199705000-00010. [DOI] [PubMed] [Google Scholar]
- 22.Matshes E.W., Taylor K.A., Rao V.J. Sulfuric acid injury. Am. J. Forensic Med. Pathol. 2008;29:340–345. doi: 10.1097/PAF.0b013e3181847e3d. [DOI] [PubMed] [Google Scholar]
- 23.Akhtar S., Kanungo S., Khurram M.F., Ahmad I. Epidemiology and outcome of chemical burn patients admitted in Burn Unit of JNMC Hospital, Aligarh Muslim University, Aligarh, Uttar Pradesh, India: A 5-year experience. J. Fam. Med. Prim. Care. 2015;4:106–109. doi: 10.4103/2249-4863.152265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Das K.K., Olga L., Peck M., Morselli P.G., Salek A.J. Management of acid burns: Experience from Bangladesh. Burns. 2015;41:484–492. doi: 10.1016/j.burns.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 25.Hsu K.-C., Luan C.-W., Tsai Y.-W. Review of silicone gel sheeting and silicone gel for the prevention of hypertrophic scars and keloids. Wounds A Compend. Clin. Res. Pract. 2017;29:154–158. [PubMed] [Google Scholar]
- 26.Tran B., Wu J.J., Ratner D., Han G. Topical scar treatment products for wounds: A systematic review. Dermatol. Surg. 2020;46:1564–1571. doi: 10.1097/DSS.0000000000002712. [DOI] [PubMed] [Google Scholar]
- 27.Shin J.Y., Yun S.-K., Roh S.-G., Lee N.-H., Yang K.-M. Efficacy of 2 representative topical agents to prevent keloid recurrence after surgical excision. J. Oral Maxillofac. Surg. 2017;75:401.e1–401.e6. doi: 10.1016/j.joms.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 28.Li Z., Wang H., Yang B., Sun Y., Huo R. Three-dimensional graphene foams loaded with bone marrow derived mesenchymal stem cells promote skin wound healing with reduced scarring. Mater. Sci. Eng. C. 2015;57:181–188. doi: 10.1016/j.msec.2015.07.062. [DOI] [PubMed] [Google Scholar]
- 29.Kant S.B., van den Kerckhove E., Colla C., Tuinder S., van der Hulst R.R.W.J., de Grzymala A.A.P. A new treatment of hypertrophic and keloid scars with combined triamcinolone and verapamil: A retrospective study. Eur. J. Plast. Surg. 2018;41:69–80. doi: 10.1007/s00238-017-1322-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sohrabi C., Goutos I. The use of botulinum toxin in keloid scar management: A literature review. Scars Burn. Health. 2020;6:2059513120926628. doi: 10.1177/2059513120926628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krastev T.K., Schop S.J., Hommes J., Piatkowski A., van der Hulst R.R.W.J. Autologous fat transfer to treat fibrosis and scar-related conditions: A systematic review and meta-analysis. J. Plast. Reconstr. Aesthetic Surg. 2020;73:2033–2048. doi: 10.1016/j.bjps.2020.08.023. [DOI] [PubMed] [Google Scholar]
- 32.Klinger M., Klinger F., Caviggioli F., Maione L., Catania B., Veronesi A., Giannasi S., Bandi V., Giaccone M., Siliprandi M., et al. Fat Grafting for treatment of facial scars. Clin. Plast. Surg. 2020;47:131–138. doi: 10.1016/j.cps.2019.09.002. [DOI] [PubMed] [Google Scholar]
- 33.To K., Crowley C., Lim S.-K., Khan W.S. Autologous adipose tissue grafting for the management of the painful scar. Cytotherapy. 2019;21:1151–1160. doi: 10.1016/j.jcyt.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 34.Grablowitz D., Ivezic-Schoenfeld Z., Federspiel I.G., Gehl B., Kopera D., Prinz M. Long-term effectiveness of a hyaluronic acid soft tissue filler in patients with facial lipoatrophy, morphological asymmetry, or debilitating scars. J. Cosmet. Dermatol. 2020;19:2536–2541. doi: 10.1111/jocd.13454. [DOI] [PubMed] [Google Scholar]
- 35.Riccio M., Marchesini A., Senesi L., Skrami E., Gesuita R., De Francesco F. Managing pathologic scars by injecting auto-cross-linked hyaluronic acid: A preliminary prospective clinical study. Aesthetic Plast. Surg. 2019;43:480–489. doi: 10.1007/s00266-018-01303-3. [DOI] [PubMed] [Google Scholar]
- 36.Van Leeuwen M.C.E., Van Der Wal M.B.A., Bulstra A.-E.J., Galindo-Garre F., Molier J., Van Zuijlen P.P.M., Van Leeuwen P.A.M., Niessen F.B. Intralesional cryotherapy for treatment of keloid scars: A prospective study. Plast. Reconstr. Surg. 2015;135:580–589. doi: 10.1097/PRS.0000000000000911. [DOI] [PubMed] [Google Scholar]
- 37.Peng W., Zhang X., Kong X., Shi K. The efficacy and safety of fractional CO2 laser therapy in the treatment of burn scars: A meta-analysis. Burns. 2021;47:1469–1477. doi: 10.1016/j.burns.2021.08.010. [DOI] [PubMed] [Google Scholar]
- 38.Meynköhn A., Fischer S., Neuss C., Willkomm L.M., Kneser U., Kotsougiani-Fischer D. Fractional ablative carbon dioxide laser treatment of facial scars: Improvement of patients’ quality of life, scar quality, and cosmesis. J. Cosmet. Dermatol. 2021;20:2132–2140. doi: 10.1111/jocd.13850. [DOI] [PubMed] [Google Scholar]
- 39.Taudorf E.H., Danielsen P.L., Paulsen I.F., Togsverd-Bo K., Dierickx C., Paasch U., Haedersdal M. Non-ablative fractional laser provides long-term improvement of mature burn scars-A randomized controlled trial with histological assessment. Lasers Surg. Med. 2015;47:141–147. doi: 10.1002/lsm.22289. [DOI] [PubMed] [Google Scholar]
- 40.Moortgat P., Anthonissen M., Van Daele U., Vanhullebusch T., Maertens K., De Cuyper L., Lafaire C., Meirte J. The effects of shock wave therapy applied on hypertrophic burn scars: A randomised controlled trial. Scars Burn. Health. 2020;6:2059513120975624. doi: 10.1177/2059513120975624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang S., Mi J., Li Q., Jin R., Dong J. Fractional microplasma radiofrequency technology for non-hypertrophic post-burn scars in Asians: A prospective study of 95 patients. Lasers Surg. Med. 2017;49:563–569. doi: 10.1002/lsm.22640. [DOI] [PubMed] [Google Scholar]
- 42.Juhasz M.L.W., Cohen J.L. Microneedling for the treatment of scars: An update for clinicians. Clin. Cosmet. Investig. Dermatol. 2020;13:997–1003. doi: 10.2147/CCID.S267192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yu P.-X., Diao W.-Q., Qi Z.-L., Cai J.-L. Effect of dermabrasion and ReCell® on large superficial facial scars caused by burn, trauma and acnes. Chin. Med. Sci. J. 2016;31:173–179. doi: 10.1016/S1001-9294(16)30047-5. [DOI] [PubMed] [Google Scholar]
- 44.Barone N., Safran T., Vorstenbosch J., Davison P.G., Cugno S., Murphy A.M. Current advances in hypertrophic scar and keloid management. Semin. Plast. Surg. 2021;35:145–152. doi: 10.1055/s-0041-1731461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Berman B., Maderal A., Raphael B. Keloids and hypertrophic scars: Pathophysiology, classification, and treatment. Dermatol. Surg. 2017;43:S3–S18. doi: 10.1097/DSS.0000000000000819. [DOI] [PubMed] [Google Scholar]
- 46.Veronese S., Beatini A., Urbani C., Lanza E., Paz O.M., Saussaye Y., Lomuto M., Sbarbati A. V-EMF treatment of facial scar: First results. J. Tissue Viability. 2022 doi: 10.1016/j.jtv.2022.07.006. [DOI] [PubMed] [Google Scholar]
- 47.Coccetta C.A., Sale P., Ferrara P.E., Specchia A., Maccauro G., Ferriero G., Ronconi G. Effects of capacitive and resistive electric transfer therapy in patients with knee osteoarthritis: A randomized controlled trial. Int. J. Rehabil. Res. 2019;42:106–111. doi: 10.1097/MRR.0000000000000324. [DOI] [PubMed] [Google Scholar]
- 48.De Sousa-De Sousa L., Tebar Sanchez C., Maté-Muñoz J.L., Hernández-Lougedo J., Barba M., Lozano-Estevan M.D.C., Garnacho-Castaño M.V., García-Fernández P. Application of capacitive-resistive electric transfer in physiotherapeutic clinical practice and sports. Int. J. Environ. Res. Public Health. 2021;18:12446. doi: 10.3390/ijerph182312446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nadler S.F., Weingand K., Kruse R.J. The physiologic basis and clinical applications of cryotherapy and thermotherapy for the pain practitioner. Pain Physician. 2004;7:395–399. doi: 10.36076/ppj.2004/7/395. [DOI] [PubMed] [Google Scholar]
- 50.Xuan X. Joule heating in electrokinetic flow. Electrophoresis. 2008;29:33–43. doi: 10.1002/elps.200700302. [DOI] [PubMed] [Google Scholar]
- 51.Song L., Yu L., Brumme C., Shaw R., Zhang C., Xuan X. Joule heating effects on electrokinetic flows with conductivity gradients. Electrophoresis. 2021;42:967–974. doi: 10.1002/elps.202000264. [DOI] [PubMed] [Google Scholar]
- 52.Tang G.Y., Yang C., Chai J.C., Gong H.Q. Joule heating effect on electroosmotic flow and mass species transport in a microcapillary. Int. J. Heat Mass Transf. 2004;47:215–227. doi: 10.1016/j.ijheatmasstransfer.2003.07.006. [DOI] [Google Scholar]
- 53.Kim D., Han S.A., Kim J.H., Lee J.-H., Kim S.-W., Lee S.-W. Biomolecular piezoelectric materials: From amino acids to living tissues. Adv. Mater. 2020;32:e1906989. doi: 10.1002/adma.201906989. [DOI] [PubMed] [Google Scholar]
- 54.Lay R., Deijs G.S., Malmström J. The intrinsic piezoelectric properties of materials—A review with a focus on biological materials. RSC Adv. 2021;11:30657–30673. doi: 10.1039/D1RA03557F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hawamdeh M. The effectiveness of capacitive resistive diathermy (Tecartherapy®) in acute and chronic musculoskeletal lesions and pathologies. Eur. J. Sci. Res. 2014;118:336–340. [Google Scholar]
- 56.Malanga G.A., Yan N., Stark J. Mechanisms and efficacy of heat and cold therapies for musculoskeletal injury. Postgrad. Med. 2015;127:57–65. doi: 10.1080/00325481.2015.992719. [DOI] [PubMed] [Google Scholar]
- 57.Mace T.A., Zhong L., Kokolus K.M., Repasky E.A. Effector CD8+T cell IFN-γproduction and cytotoxicity are enhanced by mild hyperthermia. Int. J. Hyperth. 2012;28:9–18. doi: 10.3109/02656736.2011.616182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tashiro Y., Hasegawa S., Yokota Y., Nishiguchi S., Fukutani N., Shirooka H., Tasaka S., Matsushita T., Matsubara K., Nakayama Y., et al. Effect of Capacitive and Resistive electric transfer on haemoglobin saturation and tissue temperature. Int. J. Hyperth. 2017;33:696–702. doi: 10.1080/02656736.2017.1289252. [DOI] [PubMed] [Google Scholar]
- 59.Shields N., Gormley J., O’Hare N. Short-wave diathermy: Current clinical and safety practices. Physiother. Res. Int. 2002;7:191–202. doi: 10.1002/pri.259. [DOI] [PubMed] [Google Scholar]
- 60.Yokota Y., Sonoda T., Tashiro Y., Suzuki Y., Kajiwara Y., Zeidan H., Nakayama Y., Kawagoe M., Shimoura K., Tatsumi M., et al. Effect of Capacitive and Resistive electric transfer on changes in muscle flexibility and lumbopelvic alignment after fatiguing exercise. J. Phys. Ther. Sci. 2018;30:719–725. doi: 10.1589/jpts.30.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bito T., Tashiro Y., Suzuki Y., Kajiwara Y., Zeidan H., Kawagoe M., Sonoda T., Nakayama Y., Yokota Y., Shimoura K., et al. Acute effects of capacitive and resistive electric transfer (CRet) on the Achilles tendon. Electromagn. Biol. Med. 2019;38:48–54. doi: 10.1080/15368378.2019.1567525. [DOI] [PubMed] [Google Scholar]
- 62.Raeisi M., Mohammadi H.K., Heshmatipour M., Tarrahi M.J., Taheri N. Effect of transfer energy capacitive and resistive therapy on shoulder pain, disability, and range of motion in patients with adhesive capsulitis: A study protocol for a randomized controlled trial. J. Chiropr. Med. 2022 doi: 10.1016/j.jcm.2022.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nair M., Calahorra Y., Kar-Narayan S., Best S.M., Cameron R.E. Self-assembly of collagen bundles and enhanced piezoelectricity induced by chemical crosslinking. Nanoscale. 2019;11:15120–15130. doi: 10.1039/C9NR04750F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Farahani R.M., Kloth L.C. The hypothesis of ‘biophysical matrix contraction’: Wound contraction revisited. Int. Wound J. 2008;5:477–482. doi: 10.1111/j.1742-481X.2007.00402.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Beck-Broichsitter B.E., Lamia A., Geuna S., Fregnan F., Smeets R., Becker S.T., Sinis N. Does pulsed magnetic field therapy influence nerve regeneration in the median nerve model of the rat? BioMed Res. Int. 2014;2014:401760. doi: 10.1155/2014/401760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gunay I., Mert T. Pulsed magnetic fields enhance the rate of recovery of damaged nerve excitability. Bioelectromagnetics. 2011;32:200–208. doi: 10.1002/bem.20629. [DOI] [PubMed] [Google Scholar]
- 67.Mert T., Günay I., Gocmen C., Kaya M., Polat S. Regenerative effects of pulsed magnetic field on injured peripheral nerves. Altern. Ther. Health Med. 2006;12:42–49. [PubMed] [Google Scholar]
- 68.Haastert-Talini K., Grothe C. Electrical stimulation for promoting peripheral nerve regeneration. Int. Rev. Neurobiol. 2013;109:111–124. doi: 10.1016/b978-0-12-420045-6.00005-5. [DOI] [PubMed] [Google Scholar]
- 69.Meirte J., Moortgat P., Anthonissen M., Maertens K., Lafaire C., De Cuyper L., Hubens G., Van Daele U. Short-term effects of vacuum massage on epidermal and dermal thickness and density in burn scars: An experimental study. Burn. Trauma. 2016;4:27. doi: 10.1186/s41038-016-0052-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Moortgat P., Anthonissen M., Meirte J., Van Daele U., Maertens K. The physical and physiological effects of vacuum massage on the different skin layers: A current status of the literature. Burn. Trauma. 2016;4:34. doi: 10.1186/s41038-016-0053-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chai H., Chaudhari N., Kornhaber R., Cuttle L., Fear M., Wood F., Martin L. Chemical burn to the skin: A systematic review of first aid impacts on clinical outcomes. Burns. 2022;48:1527–1543. doi: 10.1016/j.burns.2022.05.006. [DOI] [PubMed] [Google Scholar]
- 72.Claytor R.B., Sheck C.G., Chopra V. Microneedling outcomes in early post-surgical scars. Plast. Reconstr. Surg. 2022;150:557e–561e. doi: 10.1097/PRS.0000000000009466. [DOI] [PubMed] [Google Scholar]
- 73.De Oliveira G.V., Gold M.H. Silicone sheets and new gels to treat hypertrophic scars and keloids: A short review. Dermatol. Ther. 2020;33:e13705. doi: 10.1111/dth.13705. [DOI] [PubMed] [Google Scholar]
- 74.Nicoletti G., Perugini P., Bellino S., Capra P., Malovini A., Jaber O., Tresoldi M., Faga A. Scar remodeling with the association of monopolar capacitive radiofrequency, electric stimulation, and negative pressure. Photomed. Laser Surg. 2017;35:246–258. doi: 10.1089/pho.2016.4180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Alberti G., Laura S. Treatment of stretch marks aged more than twenty years with the synergy of electromagnetic field and vacuum. Clinical case studies and subsequent follow-up. Aesthetic Med. 2019;5:14–21. [Google Scholar]
- 76.Scarano A., Sbarbati A., Amore R., Iorio E.L., Ferraro G., Lorusso F., Amuso D. A New Treatment for stretch marks and skin ptosis with electromagnetic fields and negative pressure: A clinical and histological study. J. Cutan. Aesthet. Surg. 2021;14:222–228. doi: 10.4103/JCAS.JCAS_122_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bacci P.A., Alberti G., Amuso D., Artigiani A., Benitez Roig V., Di Nardo V., Garcia-Gimenez V., Greco D., Laura S., Pagano M., et al. The synergy between vacuum and electromagnetic fields in the treatment of striae distensae: Retrospective study on 917 patients with clinical and histological case records. J. Appl. Cosmetol. 2021;39:43–54. [Google Scholar]
- 78.Curtis K., Kennedy B., Lam M.K., Mitchell R.J., Black D., Burns B., White L., Loudfoot A., D’Amato A., Dinh M., et al. Cause, treatment costs and 12-month functional outcomes of children with major injury in NSW, Australia. Injury. 2020;51:2066–2075. doi: 10.1016/j.injury.2020.04.030. [DOI] [PubMed] [Google Scholar]
- 79.Baker C.P., Russell W.J., Meyer W., III, Blakeney P. Physical and psychologic rehabilitation outcomes for young adults burned as children. Arch. Phys. Med. Rehabil. 2007;88((Suppl. 2)):S57–S64. doi: 10.1016/j.apmr.2007.09.014. [DOI] [PubMed] [Google Scholar]
- 80.Blakeney P.E., Rosenberg L., Rosenberg M., Faber A.W. Psychosocial care of persons with severe burns. Burns. 2008;34:433–440. doi: 10.1016/j.burns.2007.08.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data used for this study are present in the text.